Abstract
Osteoporotic fractures are a major public health concern, particularly among the aging population, as they significantly contribute to morbidity, mortality, and reduced quality of life. While cardiovascular health (CVH) has traditionally been linked to cardiovascular disease outcomes, emerging evidence suggests it may also influence bone health. This study investigates the association between CVH, as measured by the Life’s Essential 8 (LE8) score, and the prevalence of osteoporotic fractures in U.S. adults. This cross-sectional study utilized data from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018. A total of 17,606 adults aged 20 and above were included in the analysis after excluding participants with missing data on CVH or osteoporotic fractures. CVH was assessed using the LE8 score, which incorporates eight modifiable cardiovascular health metrics: diet, physical activity, tobacco use, sleep, body mass index (BMI), lipid levels, blood glucose, and blood pressure. The primary outcome, osteoporotic fractures, was identified through self-reported data confirmed by a physician. Weighted multivariate logistic regression models were used to estimate the association between CVH and the prevalence of osteoporotic fractures, adjusting for demographic and health-related covariates. Participants with higher CVH scores had a lower prevalence of osteoporotic fractures. In the fully adjusted model, each 1-point increase in the LE8 score was associated with a 1% reduction in the odds of osteoporotic fractures (OR = 0.99, 95% CI: 0.98–0.99). Compared to participants with low CVH levels, those with moderate CVH had a 22% lower odds of osteoporotic fractures (OR = 0.78, 95% CI 0.70–0.87), and those with high CVH had a 34% lower odds (OR = 0.66, 95% CI 0.56–0.79). A significant linear trend was observed across different CVH levels (P for trend < 0.001). Subgroup analyses revealed that the inverse relationship between CVH and osteoporotic fractures was consistent across different demographic and health-related subgroups. This study highlights a significant inverse association between cardiovascular health and osteoporotic fractures in U.S. adults. These findings suggest that maintaining a high level of cardiovascular health, as measured by the LE8 score, may be important in reducing the risk of osteoporotic fractures. Public health strategies that integrate cardiovascular and bone health interventions may enhance overall health outcomes and reduce the societal burden of both cardiovascular diseases and osteoporosis.
Similar content being viewed by others
Introduction
Osteoporotic fractures, particularly those affecting the hip, spine, and wrist, represent a significant public health issue, especially among the aging population. These fractures contribute substantially to increased morbidity, mortality, and reduced quality of life in affected individuals. Globally, osteoporosis results in over 8.9 million fractures annually, translating to an osteoporotic fracture occurring approximately every three seconds1. In the United States, an estimated 10 million people are diagnosed with osteoporosis, and approximately 2 million osteoporotic fractures occur each year2,3. The substantial clinical and economic burden posed by these fractures underlines the urgent need for effective prevention and management strategies4.
Cardiovascular health (CVH), as defined by the American Heart Association (AHA), encompasses a set of modifiable risk factors that are critical to both cardiovascular and overall health outcomes. The Life’s Essential 8 (LE8) score integrates these factors—diet, physical activity, tobacco use, sleep, body mass index (BMI), lipid levels, blood glucose, and blood pressure—providing a comprehensive measure of CVH5,6. Previous research has consistently demonstrated that maintaining optimal CVH is associated with lower risks of cardiovascular diseases (CVDs), which remain the leading cause of death worldwide7. Additionally, emerging evidence suggests that the risk factors affecting cardiovascular health may also have implications for bone health and the risk of osteoporotic fractures8,9.
Several studies have explored the relationships between individual cardiovascular risk factors and bone health outcomes. For instance, hypertension, diabetes, and hyperlipidemia have been implicated in increased bone loss and fracture risk, potentially due to shared inflammatory pathways and metabolic processes that affect both the cardiovascular system and bone tissue10,11. Lifestyle factors that are critical for maintaining cardiovascular health, such as physical activity and a healthy diet, are also known to play key roles in supporting bone density and reducing fracture risk12,13.
This study aims to expand upon this growing body of literature by examining the association between cardiovascular health, as measured by the LE8 score, and the risk of osteoporotic fractures. By utilizing data from the National Health and Nutrition Examination Survey (NHANES), this study seeks to clarify the extent to which comprehensive cardiovascular health influences bone health, potentially informing integrated strategies for preventing both cardiovascular disease and osteoporosis.
Methods
Study population
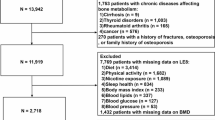
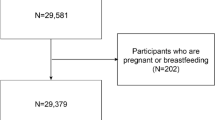
This research draws on data from a cross-sectional study utilizing the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018. Conducted by the National Center for Health Statistics, NHANES critically evaluates the health and nutritional status of the U.S. population, utilizing advanced multi-stage, probability-based sampling to capture a representative sample of the nation14,15. The integrity of the program is upheld by approvals from the National Center for Health Statistics (NCHS) Research Ethics Review Board, with all participants giving informed consent16. For our analysis, we specifically targeted 17,606 adults aged 20 and above, from the initial pool of NHANES 2005–2018 cycle, we excluded those with missing or incomplete information on LE8 measurement (N = 10,730), participants with missing information on osteoporotic fractures (N = 11,321), participants during pregnant or breastfeeding (N = 92), resulting in a final sample of 17,606 participants for analysis (Fig. 1).
Study variables
The outcomes of this study were osteoporotic fracture, which were collected through personal interviews and reported by a doctor. The NHANES interviews were completed by trained interviewers in participants’ homes using the Computer-Assisted Personal Interview system17.
Cardiovascular health is evaluated through the LE8 score, which includes diet (aligned with the Dietary Approaches to Stop Hypertension (DASH) guidelines), physical activity, tobacco use, sleep, body mass index (BMI), lipid levels excluding high-density lipoprotein (HDL), blood glucose, and blood pressure. Standard surveys collect lifestyle data, while physical and biochemical measurements are taken following standardized methods. BMI is calculated as weight in kilograms divided by height in meters squared. Blood pressure is averaged from initial readings, non-HDL cholesterol is obtained by subtracting HDL from total cholesterol, and glycated hemoglobin is determined by liquid chromatography (detailed calculation see Table S1). The LE8 score ranges from 0 to 100, with an aggregate score derived from these components, categorizing CVH into high, moderate, or low according to American Heart Association benchmarks18,19. The choice of covariates in this research was determined by their potential impact on the relationship between CVH and osteoporotic fracture.
Selected covariates included demographic and health-related factors such as age, race, educational levels, the ratio of family income to poverty (PIR) and diabetes status. These factors were selected for their known importance in epidemiological studies and their ability to confound the relationships being examined in our analysis6.
Statistical analysis
All analyses were performed using the statistical software R, version 4.3.0, with a predetermined significance threshold set at a P-value of less than 0.05 for all two-tailed tests. To compensate for any incomplete data, we utilized the mice package to perform multiple imputation using chained equations with ten imputation sets. Additionally, we conducted sensitivity analyses using the complete-case dataset (excluding participants with missing data) to assess the robustness of our findings without imputation.
The LE 8 score was used to stratify cardiovascular health into three categories: low (scores below 50), intermediate (scores between 50 and 79), and high (scores 80 or above). The association between cardiovascular health and osteoporotic fractures was investigated through weighted multivariate logistic regression models. The model 1 did not adjust for additional variables; the model 2 accounted for age and ethnicity, and the third model further incorporated educational background and PIR. In addition to analyzing the overall LE8 score, we conducted further analysis to assess the sensitivity of the individual components of the LE8 score to osteoporotic fracture outcomes. Each component of the LE8 score, including diet, physical activity, tobacco/nicotine exposure, sleep, body mass index (BMI), blood lipids, blood glucose, and blood pressure, was evaluated separately using weighted multivariate logistic regression models. Tests for linear trends across three categories of cardiovascular health metrics scores were performed by modeling the median value within each category as a continuous variable. To explore potential non-linear relationships between CVH and osteoporotic fractures, we employed smooth curve fitting techniques using generalized additive models (GAMs). The smoothness of the curve is determined by a smoothing parameter, which controls the trade-off between the model’s fit and its complexity. We assessed the appropriateness of the curve using the generalized cross-validation score as a criterion for selecting the smoothing parameter21,22,23. Interaction tests were conducted to assess whether the association between CVH and osteoporotic fractures differed across various subgroups (age, sex, education level, PIR, diabetes). For this purpose, we introduced interaction terms into our logistic regression models, which represent the product of CVH scores and subgroup identifiers.
Results
Baseline characteristics
A total of 17,606 adult participants with a mean age of (50.2 ± 17.9) years were enrolled in this study, with 50.1% male and 49.9% female participants. A total of 2,161 participants (12.3%) were diagnosed with osteoporotic fracture.The mean and standard deviation of LE8 score were 61.8 (14.7). Notably, 21.5% of participants had low levels of CVH (LE8 < 50), 66.3% had moderate levels of CVH (50 ≤ LE8 < 80), and 12.2% had high levels of CVH (LE8 ≥ 80). Participants with higher CVH scores had a lower prevalence of osteoporotic fractures and diabetes compared with those with lower CVH scores. In addition, participants with higher CVH scores were younger, more likely to be female, and had higher socioeconomic status (education level and PIR) (P < 0.01) (Table 1).
Association between CVH and osteoporotic fractures
Table 2 demonstrates the association between CVH and osteoporotic fractures. In all models, there was a significant inverse association between CVH and the odds of osteoporotic fractures prevalence (P < 0.001). In the fully adjusted model with all covariates adjusted, each unit increase in LE8 score was associated with a 1% lower in the odds of osteoporotic fractures prevalence [OR = 0.99, 95%CI: 0.98–0.99]. This association remained significant in the complete-case analysis without MI (OR = 0.98, 95% CI: 0.96–0.99, P < 0.001), as shown in Table S2.
In addition, compared to participants with low CVH levels, those with moderate CVH levels had a 22% lower odds of osteoporotic fractures prevalence [OR = 0.78, 95% CI: 0.70–0.87], while participants with high CVH levels had a 34% lower odds of osteoporotic fractures prevalence [OR = 0.66, 95% CI: 0.56–0.79]. The linear trend across CVH levels was significant (P for trend < 0.001), consistent in both imputed and complete-case analyses. The result of smoothed curve fitting further corroborated the inverse association between the LE8 score and osteoporotic fractures (Fig. 2).
The results of the sensitivity analysis for the individual LE8 components are shown in Table S3. Several LE8 subscores were significantly associated with osteoporotic fractures. For example, higher DASH diet scores were associated with a 4% lower risk of fractures in the fully adjusted model (OR = 0.96, 95% CI: 0.93–0.99, P < 0.001), while higher physical activity scores were associated with a 5% lower risk of fractures (OR = 0.95, 95% CI: 0.92–0.98, P < 0.001). Tobacco/nicotine exposure, BMI, and blood pressure scores also demonstrated significant inverse associations with osteoporotic fractures. In contrast, the sleep health score showed a weaker association, with significance only in certain models (P = 0.042 in Model 1 and P = 0.008 in Model 2 but not significant in Model 3). Blood glucose and blood lipid scores showed marginal or non-significant associations in the fully adjusted model.
Subgroup analyses
Table 3 shows the association between CVH and osteoporotic fractures in different populations. Differences in the relationship between participants of different sexes, ages, and educational levels, PIR, and diabetes subgroups were small and were in essentially the same direction, maintaining an inverse correlation (all P for interaction > 0.05).
Discussion
In this cross-sectional study involving 17,606 U.S. adults, we found a significant inverse association between CVH, as assessed by the LE8 score, and the prevalence of osteoporotic fractures. Specifically, each 1-point increase in the LE8 score was associated with a 1% reduction in the odds of osteoporotic fractures. Participants with moderate CVH had a 22% lower prevalence of osteoporotic fractures, while those with high CVH had a 34% lower prevalence, compared to participants with low CVH. These results persisted even after adjusting for various demographic, socioeconomic, and health-related covariates. Furthermore, the association exhibited a clear linear trend, and the smoothed curve fitting confirmed a robust inverse relationship between the LE8 score and osteoporotic fractures. In addition to our primary findings, we conducted a sensitivity analysis to examine the differential impact of individual components of the LE8 score on osteoporotic fractures. This analysis revealed that specific components, such as physical activity, diet, and tobacco/nicotine exposure, had a more pronounced association with fracture risk. These findings further emphasize the critical role of healthy lifestyle behaviors in both cardiovascular and bone health. While components like sleep health and blood glucose showed weaker or marginal associations, their contributions to overall cardiovascular health should not be overlooked. This underscores the need for a holistic approach in managing multiple health factors to optimize bone health and reduce fracture risk. These findings suggest that maintaining optimal cardiovascular health could play a critical role in reducing the risk of osteoporotic fractures.
Comparison with previous studies
The relationship between cardiovascular health and bone health has been increasingly recognized in recent years, though the exact mechanisms remain an area of active research. Previous studies have primarily focused on specific cardiovascular risk factors and their associations with bone density and fracture risk. For instance, hypertension has been identified as a risk factor for osteoporosis and fractures, possibly due to its effects on calcium excretion and bone mineral metabolism. Elevated blood pressure can lead to increased urinary calcium loss, which in turn may contribute to decreased bone mineral density (BMD) and increased fracture risk20,21. Diabetes, another critical cardiovascular risk factor, has also been extensively studied in relation to bone health. Research indicates that both type 1 and type 2 diabetes are associated with an increased risk of fractures, despite the higher BMD often observed in individuals with type 2 diabetes22. The paradox of higher BMD yet increased fracture risk in diabetes may be explained by factors such as poor bone quality, alterations in collagen properties, and impaired bone remodeling due to advanced glycation end products23.
Lipid metabolism disorders, such as hyperlipidemia, have similarly been implicated in bone health. High cholesterol levels may promote bone resorption through inflammatory pathways, negatively impacting bone density24. In a study using the NHANES dataset, researchers found that higher levels of total cholesterol were associated with lower BMD and an increased risk of fractures25. Furthermore, dyslipidemia may accelerate atherosclerosis, which has been linked to reduced bone perfusion and subsequent bone loss26.
What differentiates our study from these earlier works is the use of a comprehensive cardiovascular health metric—the LE8 score—instead of focusing on individual risk factors. The LE8 score integrates multiple modifiable cardiovascular risk factors, offering a more holistic approach to understanding the relationship between cardiovascular health and osteoporotic fractures. Physical activity, a key component of the LE8 score, likely plays a crucial role in reducing fracture risk. Regular exercise not only improves cardiovascular health but also strengthens bones by applying mechanical stress, which stimulates bone formation and enhances bone density27. Our findings underscore that not only do individual risk factors matter, but the overall state of cardiovascular health plays a crucial role in bone health outcomes. By examining cardiovascular health in its entirety, our study contributes to a growing body of literature suggesting that strategies aimed at improving overall cardiovascular health could be effective in reducing the risk of osteoporotic fractures18,28. This comprehensive approach aligns with recent research emphasizing the interconnectedness of systemic health, whereby conditions like osteoporosis and cardiovascular diseases share common risk factors and potentially overlapping pathophysiological mechanisms8.
While it is well-documented that women are more susceptible to fractures due to hormonal changes and post-menopausal characteristics, our study did not observe significant gender differences in the association between cardiovascular health and osteoporotic fractures. One possible explanation is that the protective effects of cardiovascular health, as reflected by the LE8 score, may be similarly beneficial for both men and women29. Physical activity and other healthy lifestyle factors included in the LE8 score, such as a balanced diet and non-smoking status, are known to benefit bone health irrespective of gender30. These shared lifestyle factors could have minimized the potential gender-specific differences in fracture risk31. Additionally, the lack of significant differences could be attributed to limitations related to sample size or statistical power. Although our study included a large cohort, detecting subtle gender-specific differences may require even larger sample sizes or more detailed subgroup analyses. Further research with larger cohorts is warranted to explore whether gender plays a modifying role in the relationship between cardiovascular health and osteoporotic fractures.
Potential biological mechanisms
The inverse relationship between CVH and osteoporotic fractures observed in this study can be attributed to several potential biological mechanisms that connect cardiovascular and bone health. One of the primary links between these two systems is inflammation. Chronic low-grade inflammation, commonly associated with poor cardiovascular health, has been shown to negatively impact bone metabolism. Pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) are known to promote bone resorption by activating osteoclasts, the cells responsible for bone breakdown32,33. These cytokines are often elevated in individuals with cardiovascular risk factors, such as obesity, hypertension, and diabetes, creating an environment conducive to both vascular and bone tissue degradation34.
Oxidative stress, another key factor in cardiovascular disease, also plays a significant role in bone health. Reactive oxygen species (ROS), which are elevated in conditions such as hypertension and diabetes, can lead to increased bone resorption and decreased bone formation. Oxidative stress impairs osteoblast function (the cells responsible for bone formation) and promotes osteoclast activity, thereby disrupting the balance between bone formation and resorption35. This imbalance can weaken bone structure, making it more susceptible to fractures.
Furthermore, vascular health is intimately connected with bone health. Adequate blood supply is essential for maintaining healthy bone tissue, and compromised vascular health, as seen in atherosclerosis, can lead to reduced bone perfusion and subsequent bone loss36. Vascular calcification, a hallmark of advanced cardiovascular disease, may also be associated with decreased bone density through shared mechanisms of mineral metabolism37. For example, both bone and vascular tissue rely on similar regulatory pathways for calcium and phosphate balance, and disturbances in these pathways can lead to both vascular calcification and bone loss38.
Another potential mechanism linking cardiovascular health and bone health is the role of lifestyle factors. Physical activity, which is a key component of both cardiovascular and bone health, directly influences bone density by applying mechanical stress to bone tissue, thereby stimulating bone formation39. Similarly, a healthy diet rich in nutrients like calcium, vitamin D, and omega-3 fatty acids supports both cardiovascular and bone health by reducing inflammation, improving lipid profiles, and promoting bone mineralization40. Conversely, unhealthy behaviors such as smoking and excessive alcohol consumption, both of which are detrimental to cardiovascular health, are also well-known risk factors for bone loss and fractures41. These lifestyle factors further reinforce the interconnectedness of cardiovascular and bone health, highlighting the importance of comprehensive health strategies that address multiple risk factors simultaneously.
Finally, metabolic factors such as insulin resistance and dyslipidemia, commonly seen in metabolic syndrome, can affect both cardiovascular and bone health. Insulin resistance, a key feature of type 2 diabetes, has been associated with impaired bone formation and increased bone fragility42. Additionally, abnormal lipid metabolism, characterized by elevated levels of LDL cholesterol and triglycerides, may contribute to bone loss by promoting systemic inflammation and endothelial dysfunction43. These metabolic disturbances create a complex network of interactions that impact both the cardiovascular system and the skeletal system, further explaining the observed association between CVH and osteoporotic fractures in our study.
Strengths and limitations
This study has several strengths. First, the use of a large, nationally representative sample from NHANES ensures that our findings are generalizable to the broader U.S. adult population17. Second, the comprehensive nature of the LE8 score allows for an integrated assessment of multiple cardiovascular risk factors, providing a more holistic view of cardiovascular health’s impact on bone health.
However, there are also limitations to consider. The cross-sectional design of this study precludes the ability to infer causality, meaning we cannot establish whether improved cardiovascular health directly reduces the risk of osteoporotic fractures over time. Longitudinal studies are needed to confirm the directionality of this association. Additionally, our study relies on self-reported data for osteoporotic fractures, which may introduce recall bias and potentially affect the accuracy of the outcomes. While we adjusted for various confounders, residual confounding due to unmeasured factors, such as genetic predisposition or specific dietary patterns, could still influence our results. Future research should aim to incorporate more objective measures of both cardiovascular health and bone health, and explore potential mediating effects of novel biomarkers and genetic factors.
Conclusion
In conclusion, this study demonstrates a significant inverse association between cardiovascular health and the prevalence of osteoporotic fractures in U.S. adults. Our findings suggest that maintaining a high level of cardiovascular health, as measured by the LE8 score, may play a key role in reducing the risk of osteoporotic fractures. The sensitivity analysis of individual LE8 components highlights the importance of promoting specific health behaviors, particularly physical activity and a healthy diet, to enhance bone health. These results underscore the importance of integrated public health strategies that target both cardiovascular and bone health to improve overall health outcomes and reduce the burden of both cardiovascular diseases and osteoporosis.
Data availability
Survey data from this study are accessible globally to researchers and data users via the internet at https://www.cdc.gov/nchs/nhanes/.
Abbreviations
- BMD:
-
Bone mineral density
- CVH:
-
Cardiovascular health
- LE8:
-
Life’s Essential 8
- NHANES:
-
National Health and Nutrition Examination Survey
- CVD:
-
Cardiovascular disease
- PCOS:
-
Polycystic ovary syndrome
- NCHS:
-
National Center for Health Statistics
- BMI:
-
Body mass index
- HDL-C:
-
High-density lipoprotein cholesterol
- PIR:
-
Income-to-poverty ratio
- GAMs:
-
Generalized additive models
- DASH:
-
Dietary Approaches to Stop Hypertension
References
Cummings, S. R. & Melton, L. J. Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319), 1761–1767 (2002).
Looker, A. C. et al. Prevalence of low femoral bone density in older US adults from NHANES III. J. Bone Min. Res. 12(11), 1761–1768 (1997).
Burge, R. et al. Incidence and economic burden of osteoporosis‐related fractures in the United States, 2005–2025. J. Bone Min. Res. 22(3), 465–475 (2007).
Siris, E. S. et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch. Intern. Med. 164(10), 1108–1112 (2004).
Lloyd-Jones, D. M. et al. Life’s essential 8: Updating and enhancing the American Heart Association’s construct of cardiovascular health: A presidential advisory from the American Heart Association. Circulation 146(5), e18–e43 (2022).
Xie, R. et al. Associations of ethylene oxide exposure and Life’s Essential 8. Environ. Sci. Pollut Res. Int. (2023).
Update, A. S. Heart disease and stroke statistics–2017 update. Circulation 135, e146–e603 (2017).
Farhat, G. et al. The association of bone mineral density measures with incident cardiovascular disease in older adults. Osteoporos. Int. 18, 999–1008 (2007).
Lampropoulos, C. E., Papaioannou, I. & D’cruz, D. P. Osteoporosis—a risk factor for cardiovascular disease? Nat. Rev. Rheumatol. 8(10), 587–598 (2012).
Javed, F. et al. Association of hypertension and bone mineral density in an elderly African American female population. J. Natl. Med. Assoc. 104(3–4), 172–178 (2012).
Whitney, C. et al. Are cardiovascular disease and osteoporosis directly linked? Sports Med. 34, 779–807 (2004).
Gregg, E. W., Cauley, J. A., Seeley, D. G., Ensrud, K. E. & Bauer, D. C. Physical activity and osteoporotic fracture risk in older women. Ann. Intern. Med. 129(2), 81–88 (1998).
Lanham-New, S. A. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment: Symposium on ‘diet and bone health’. Proc. Nutr. Soc. 67(2):163–176. (2008).
Xie, R. et al. Association between SII and hepatic steatosis and liver fibrosis: A population-based study. Front. Immunol. 13, 925690 (2022).
Xie, R. & Liu, M. Relationship between non-alcoholic fatty liver disease and degree of hepatic steatosis and bone Mineral Density. Front. Endocrinol. (Lausanne) 13, 857110 (2022).
Xie, R. et al. Dietary inflammatory potential and biological aging among US adults: A population-based study. Aging Clin. Exp. Res. 35(6), 1273–1281 (2023).
Xie, R. et al. Race and gender differences in the associations between cadmium exposure and bone mineral density in US adults. Biol. Trace Elem. Res. 201(9), 4254–4261 (2023).
Ma, H. et al. Cardiovascular health and life expectancy among adults in the United States. Circulation 147(15), 1137–1146 (2023).
Mahemuti, N. et al. Urinary albumin-to-creatinine ratio in normal range, cardiovascular health, and all-cause mortality. JAMA Netw. Open. 6(12), e2348333 (2023).
Sprini, D., Rini, G. B., Di Stefano, L., Cianferotti, L. & Napoli, N. Correlation between osteoporosis and cardiovascular disease. Clin. Cases Mineral. Bone Metab. 11(2), 117 (2014).
Ye, Z., Lu, H. & Liu, P. Association between essential hypertension and bone mineral density: A systematic review and meta-analysis. Oncotarget 8(40), 68916 (2017).
Vestergaard, P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos. Int. 18, 427–444 (2007).
Martínez, S. B., Cenarruzabeitia, N. V., San Martin, J. E. & Canelas, A. C. The diabetic paradox: Bone mineral density and fracture in type 2 diabetes. Endocrinología Y Nutrición (Engl. Edn). 63(9), 495–501 (2016).
Delitala, A. P., Fanciulli, G., Maioli, M. & Delitala, G. Subclinical hypothyroidism, lipid metabolism and cardiovascular disease. Eur. J. Intern. Med. 38, 17–24 (2017).
Ilić, K., Obradović, N. & Vujasinović-Stupar, N. The relationship among hypertension, antihypertensive medications, and osteoporosis: A narrative review. Calcif. Tissue Int. 92, 217–227 (2013).
Hamerman, D. Osteoporosis and atherosclerosis: Biological linkages and the emergence of dual-purpose therapies. QJM 98(7), 467–484 (2005).
Bloomfield, S. A., Little, K., Nelson, M. & Yingling, V. American college of sports medicine position stand: Physical activity and bone health. Med. Sci. Sports Exerc. 195(9131/04), 3611 (2004).
He, S. et al. Association between cardiovascular health and abdominal aortic calcification: Analyses of NHANES 2013–2014. Int. J. Cardiol. 403, 131878 (2024).
Khosla, S., Melton, L. J. III & Riggs, B. L. Estrogen and the male skeleton. J. Clin. Endocrinol. Metab. 87(4), 1443–1450 (2002).
Guadalupe-Grau, A., Fuentes, T., Guerra, B. & Calbet, J. A. Exercise and bone mass in adults. Sports Med. 39, 439–468 (2009).
Mukamal, K., Robbins, J., Cauley, J., Kern, L. & Siscovick, D. Alcohol consumption, bone density, and hip fracture among older adults: The cardiovascular health study. Osteoporos. Int. 18, 593–602 (2007).
Redlich, K. & Smolen, J. S. Inflammatory bone loss: Pathogenesis and therapeutic intervention. Nat. Rev. Drug Discov. 11(3), 234–250 (2012).
Grimble, R. F. Inflammatory response in the elderly. Curr. Opin. Clin. Nutr. Metab. Care 6(1), 21–29 (2003).
Pertynska-Marczewska, M. & Merhi, Z. Relationship of advanced glycation end products with cardiovascular disease in menopausal women. Reprod. Sci. 22(7), 774–782 (2015).
Almeida, M., Han, L., Ambrogini, E., Bartell, S. M. & Manolagas, S. C. Oxidative stress stimulates apoptosis and activates NF-κB in osteoblastic cells via a PKCβ/p66shc signaling cascade: Counter regulation by estrogens or androgens. Mol. Endocrinol. 24(10), 2030–2037 (2010).
Persy, V. & D’Haese, P. Vascular calcification and bone disease: the calcification paradox. Trends Mol. Med. 15(9), 405–416 (2009).
Danilevicius, C., Lopes, J. & Pereira, R. M. R. Bone metabolism and vascular calcification. Braz. J. Med. Biol. Res. 40, 435–442 (2007).
Zaidi, M. Skeletal remodeling in health and disease. Nat. Med. 13(7), 791–801 (2007).
Frost, H. M. Bone mass and the mechanostat: A proposal. Anat. Rec. 219(1), 1–9 (1987).
Cashman, K. D. Diet, nutrition, and bone health. J. Nutr. 137(11), 2507S–2512S (2007).
Kanis, J. A. Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359(9321), 1929–1936 (2002).
Li, G-F. et al. The paradox of bone mineral density and fracture risk in type 2 diabetes. Endocrine. 1–4 (2024).
Kersten, S. New insights into angiopoietin-like proteins in lipid metabolism and cardiovascular disease risk. Curr. Opin. Lipidol. 30(3), 205–211 (2019).
Acknowledgements
Our gratitude extends to every participant involved in this study.
Funding
This research was supported by the National Key Research and Development Project (2018YFE0114500), the National Natural Science Foundation of China (82073653 and 81803313), the Outstanding Youth Scientist Fund Project of Hunan Province (2022JJ10087), the Hunan Provincial Science and Technology Talent Support Project (2020TJ-N07), the Key Research and Development Program of Hunan Province (2018SK2063), the Open Project from NHC Key Laboratory of Birth Defect for Research and Prevention (KF202006), the Natural Science Foundation of Hunan Province (2018JJ2551 and 2022JJ40207), the Hunan Provincial Health Commission General Guidance Program (Grant No. 202104071421), the Hunan Province Clinical Medical Technology Innovation Guidance Project (Grant No. 2021SK51910), and the Regional Joint Fund of the Hunan Provincial Natural Science Foundation (Grant No. 2023JJ50160).
Author information
Authors and Affiliations
Contributions
The study was conceptualized by JO and JQ. Data collection, analysis, and initial drafting were undertaken by JO, TW, RL, MS, XR and JW. Manuscript revisions were carried out by JO, TW, and JQ. Contributions from all authors were integral, and they have given approval for the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and informed consent
The National Center for Health Statistics of the Center for Disease Control and Prevention Institutional Review Board approved the protocol. The research programme complied with the basic elements of the Declaration of Helsinki. All participants signed an informed consent form while participating in NHANES.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ou, J., Wang, T., Lei, R. et al. Association between cardiovascular health and osteoporotic fractures: a national population-based study. Sci Rep 15, 3844 (2025). https://doi.org/10.1038/s41598-025-88020-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88020-5
Keywords
This article is cited by
-
The intersection of osteoporosis and cardiovascular disease in pathogenesis and treatment
Discover Medicine (2026)
-
Application of machine learning algorithms in osteoporosis analysis based on cardiovascular health assessed by life’s essential 8: a cross-sectional study
Journal of Health, Population and Nutrition (2025)