Abstract
In this study, we investigated the effect of severe dysphagia on the overall survival of patients who underwent PEG. A cohort of patients who underwent PEG between April 2016 and April 2021 was retrospectively analyzed. The Hyodo–Komagane score was used to evaluate swallowing via endoscopy. Patients with a Hyodo–Komagane score ≤ 8 were defined as having moderate dysphagia, whereas those with a score ≥ 9 were defined as having severe dysphagia. The primary outcome was overall survival. The prognostic factors were identified using multivariate analysis with the Cox proportional hazards model. Values of p < 0.05 were considered statistically significant. Among the 107 patients, 60 (56.1%) were classified into the moderate dysphagia group and 47 (43.9%) into the severe dysphagia group. The median follow-up period was 16.7 months. The overall survival was significantly worse in the severe group than in the moderate group (p < 0.0001). A multivariate analysis revealed that severe dysphagia was an independent poor prognostic factor (hazard ratio, 2.956; 95% confidence interval, 1.592–5.489; p < 0.001). Aspiration-related pneumonia was most common causes of death after PEG. Severe dysphagia was identified as an independent poor prognostic factor for survival in patients who underwent PEG.
Similar content being viewed by others
Introduction
Percutaneous endoscopic gastrostomy (PEG), introduced by Gauderer et al. in 1980, is widely used as an enteral feeding access for artificial nutrition1. PEG for mid- to long-term nutritional management is superior to nasogastric tube feeding in terms of patient tolerability and social acceptance2,3,4. Furthermore, PEG reportedly causes gastroesophageal reflux disease and aspiration pneumonia less frequently than nasogastric tube feeding, and the effectiveness of nutritional intervention with PEG is superior to that of nasogastric tube4,5. Therefore, when nutritional intake is inadequate and artificial enteral nutrition is required for more than 2 or 3 weeks, nutritional support should be provided through gastrostomy6.
The impact of dysphagia on their long-term prognosis after PEG is unclear. Subclinical aspiration can occur even in patients who do not orally consume food, and high dysphagia severity is correlated with an increased risk of developing aspiration pneumonia. In Japan, evaluation of swallowing function is recommended before PEG is performed. Therefore, this study may help determine patient prognosis after PEG based on the severity of dysphagia. If the prognosis is poor, severe dysphagia may not be an ideal indication for PEG.
In this study, we aimed to investigate the association between the severity of dysphagia and post-PEG survival. We hypothesized that severe dysphagia is a poor prognostic factor for post-PEG survival. If it is established that severe dysphagia is associated with significantly shorter survival after PEG, this information will be crucial in determining whether PEG should be performed.
Materials and methods
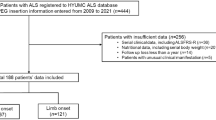
Study participants
Patients who underwent PEG for enteral nutritional access at Omi Medical Center between April 2016 and April 2021 were eligible for the study. All patients who underwent endoscopy for the evaluation of swallowing function before and after PEG were included, and those who did not undergo endoscopy or whose swallowing function could not be evaluated were excluded. This study included only patients who did not orally consume food after PEG.
All experimental protocols described in this study were approved by the Institutional Ethical Review Committee of Omi Medical Center (authorization number:2023-0046). The study adhered to the ethical guidelines of the Japan Ministry of Health, Labour and Welfare for Medical and Health Research Involving Human Subjects and conformed to the principles outlined in the Declaration of Helsinki. The opt-out recruitment method was used, which allowed the patients to decline participation. Informed consent was obtained from all participants.
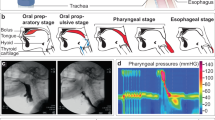
Definition of dysphagia
The Hyodo–Komagane scoring method was used to endoscopically evaluate swallowing function (Table 1)7,8. A higher Hyodo–Komagane score indicated a more severe decline in swallowing function. Since oral intake was considered challenging at a score ≥ 97,8, patients with a Hyodo–Komagane score ≤ 8 were categorized into the moderate dysphagia group, whereas those with a score ≥ 9 were classified into the severe dysphagia group.
Outcome
The primary outcome was overall survival (OS) after PEG, which was defined as the time from the date of PEG administration to the date of death. Patients who were not followed up at the hospital were investigated by hospital staff to confirm whether the patients were alive or dead. Patients for whom survival status was unclear were also excluded.
Statistical analyses
Fisher’s exact test was used to compare patient demographics between the two groups, and the log-rank test was used to compare OS and generate Kaplan–Meier survival curves. We performed a multivariate analysis to identify independent poor prognostic factors and incorporated variables with values of p < 0.15 from the univariate analysis obtained using the Cox proportional hazards regression model. All statistical analyses were performed using EZR software (Saitama Medical Center, Jichi Medical University, Japan). Values of p < 0.05 were considered statistically significant.
Covariates
The variables used for prognostic comparison included the severity of dysphagia, sex, age, body mass index, serum albumin, total cholesterol (TC), total lymphocyte count (TLC), C-reactive protein (CRP), Controlling Nutritional Status (CONUT) score, performance status, Mini Nutritional Assessment Short-Form score, and comorbidities. For each cut-off value, we used values that were previously reported as being related to prognosis9,10,11,12.
Results
Patient demographics
Patient demographics are summarized in Table 1. Among the 107 patients, 60 (56.1%) were categorized into the moderate dysphagia group and 47 (43.9%) into the severe dysphagia group. The median Hyodo-Komagane score was 7.62 (IQR 5.5–10). The proportion of male patients was significantly higher (p < 0.001) and the median TC level was significantly lower (p = 0.005) in the severe dysphagia group than in the moderate dysphagia group. In the background, the proportion of traumatic brain injury was statistically significantly higher (p < 0.05) in the severe dysphagia group.(Table 2).
Comparison of overall survival
The median follow-up period was 16.7 (interquartile range [IQR], 5.2–30.2) months. The OS was significantly worse in the severe dysphagia group than in the moderate dysphagia group (p < 0.0001) (Fig. 1). The median survival time was 23.8 (IQR, 11.9–40.0) months for the moderate dysphagia group and 7.7 (IQR, 3.7–19.5) months for the severe dysphagia group. The 1-year survival rates in the moderate and severe dysphagia groups were 76.7% and 36.2%, respectively. In the group with obvious disease (moderate dysphagia n = 38, severe dysphagia n = 37), the prognosis was statistically significantly worse in the severe dysphagia group than in the moderate dysphagia group (p < 0.001) (Fig. 2). The median survival time was 26.4 (IQR, 18.7–41.7) months for the moderate dysphagia group and 8.1 (IQR, 4.6–21.5) months for the severe dysphagia group. In the group with physical function decline due to aging or dementia (moderate dysphagia n = 22, severe dysphagia n = 10), the prognosis was statistically significantly worse in the severe dysphagia group than in the moderate group (p < 0.05) (Fig. 3). The median survival time was 15.9 (IQR, 5.1–36.1) months for the moderate group and 7.7 (IQR, 2.9–12.4) months for the severe group.
Prognostic factors for overall survival
The results of the analysis of the prognostic factors related to OS after PEG are presented in Table 3. The univariate analysis revealed that severe dysphagia (p < 0.001), male sex (p = 0.002), TC < 160 mg/dL (p = 0.007), TLC < 1200 cells/mm2 (p = 0.011), and CONUT score ≥ 5 (p = 0.002) were significant poor prognostic factors associated with OS after PEG. The multivariate analysis revealed that severe dysphagia was an independent poor prognostic factor (hazard ratio, 2.956; 95% confidence interval, 1.592–5.489, p < 0.001).
Comparison of cause of death
Table 4 compares the causes of death between the groups. During the observation period, 39 of the 60 patients (65.0%) in the moderate dysphagia group and 42 of the 47 patients (89.4%) in the severe dysphagia group died. Among the 81 patients who died after PEG, aspiration-related pneumonia was the most common cause (57 [70.4%]). Aspiration-related pneumonia was considerly more common in the severe dysphagia group than in the moderate dysphagia group (61.7% vs. 46.7%, respectively; p = 0.172), though the defference was not statistically significant.
Discussion
In this study, we investigated the relationship between the severity of dysphagia and OS after PEG. Severe dysphagia was identified as a poor prognostic factor for OS in patients after PEG. Several new findings emerged from this study. First, severe dysphagia was identified as an independent poor prognostic factor for OS in patients after PEG. Second, the comparison of the moderate and severe dysphagia groups revealed no differences in background disease or nutritional status except for traumatic brain injury and sex. Third, aspiration-related pneumonia, the most common cause of death, was more common in the severe dysphagia group than in the moderate dysphagia group. To our knowledge, this is the first study to demonstrate that severe dysphagia is a poor prognostic factor for OS in patients after PEG.
The multivariate analysis based on the Cox proportional hazards model revealed that severe dysphagia, defined as a Hyodo–Komagane score ≥ 9, was an independent poor prognostic factor for OS in patients after PEG. In the present study, prognosis after PEG was poor with a shorter survival in the severe dysphagia group than in the moderate dysphagia group. Regarding the association between dysphagia and prognosis, Patel et al. reported that, among 88 million adult hospitalized patients aged ≥ 45 years, 2.7 million with dysphagia had a 1.7 times higher hospitalization mortality rate13, and Light et al. suggested that a history of aspiration pneumonia is a poor prognostic factor in post-PEG patients10. These studies suggest that the degree of dysphagia may influence prognosis, which is consistent with our findings.
The comparison of the moderate and severe dysphagia groups demonstrated no differences in background disease, nutritional status, or other factors except for traumatic brain injury and sex. This indicates that no significant differences exist in the prognostically relevant indices for PEG except for the severity of dysphagia. Several studies have suggested that serum albumin14,15,16,17, TLC17,18, TC19, and CRP levels are prognostic factors for OS after PEG17. Lang et al. investigated 30- or 60-day survival rates after PEG in 502 patients and found that a serum albumin level < 3.0 g/dL is a significant risk factor for early death11. In this study, despite evaluating prognosis using cut-off values from previous studies, the multivariate analysis revealed that a Hyodo–Komagane score ≥ 9 was the poorest prognostic factor for OS among other factors in patients who underwent PEG.
Aspiration-related pneumonia, the most common cause of death after PEG (70.4%), was more common in the severe dysphagia group than in the moderate group. Although there was no statistically significant difference in the frequency of aspiration pneumonia when comparing the causes of death in the groups with moderate and severe dysphagia, it is clear that aspiration is a common cause of death in both groups, and in the group with severe dysphagia, there is a possibility of death due to aspiration occurring at an earlier stage after PEG. The severity of dysphagia reflects the severity of the background disease and the severity of the general condition, which affects survival after PEG. A meta-analysis by Kondwani et al. demonstrated that 42% of patients developed dysphagia following stroke, with a 4.08-fold increased risk of pneumonia and a 4.07-fold increased mortality rate20. The present study demonstrated that the majority of patients had post-stroke dysphagia.
In this study, Hyodo–Komagane score was an objective measure of dysphagia, exhibiting a clear correlation with a poor prognosis. Swallowing function should be evaluated before PEG is performed, and endoscopy is highly useful because it is easy to perform. During endoscopic swallowing function evaluations, an objective rather than subjective judgment should be made. Based on the results of this study, it is imperative that clinicians communicate to patients or their families that a score ≥ 9 indicates a poor prognosis despite PEG.
This study had several limitations. First, it was a single-center retrospective study; therefore, further multicenter prospective studies are required to validate the generalizability of its results. Second, its sample size was relatively small. However, despite the small sample size, we demonstrated that severe dysphagia is an important prognostic factor among patients who undergo PEG. This is the first study to demonstrate that severe dysphagia is an independent poor prognostic factor for OS in patients after PEG, which is of high clinical value. In patients with severe dysphagia after PEG, improving swallowing function is often challenging and associated with a poor prognosis. These results suggest that patients with severe dysphagia should be informed that long-term survival may be difficult before deciding whether to undergo PEG. Aspiration prevention surgery should be considered as a treatment option for patients with severe dysphagia who strongly desire to continue oral intake even if they are unable to speak or who want to avoid death due to aspiration as much as possible. Even if the patient has severe dysphagia, if they are in a lot of pain from a nasogastric tube, it is not wrong to perform PEG to improve their quality of life. If a patient with severe dysphagia does not complain of any pain due to nasogastric tube, it may be acceptable to continue feeding via a nasogastric tube without PEG, which may cause complications and postoperative pain, or to choose peripheral infusion.
Conclusion
In this study, patients with severe dysphagia experienced significantly shorter survival after PEG than that of patients with moderate dysphagia. The multivariate analysis revealed that severe dysphagia was an independent poor prognostic factor for OS in patients after PEG.
Data availability
Sequence data that support the findings of this study have been deposited in figshare.10.6084/m9.figshare.25679520.
References
Gauderer, M. W. L., Ponsky, J. L. & Izant, R. J. Gastrostomy without laparotomy: A percutaneous endoscopic technique. J. Pediatr. Surg. 15, 872–875 (1980).
Nenad, V., Aida, S., Srdjan, G. & Rusmir, M. Percutaneous endoscopic gastrostomy: Retrospective analysis of 7-year clinical experience. Acta Inf. Med. 20, 235–237 (2012).
Nicholson, F. B., Korman, M. G. & Richardson, M. A. Percutaneous endoscopic gastrostomy: A review of indications, complications and outcome. J. Gastroenterol. Hepatol. 15, 21–25 (2000).
Park, R. H. et al. Randomised comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurological dysphagia. BMJ 304, 1406–1409 (1992).
Norton, B., Homer-Ward, M., Donnelly, M. T., Long, R. G. & Holmes, G. K. T. A randomized prospective comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding after acute dysphagic stroke. BMJ 312, 13–16 (1996).
Löser, C. et al. ESPEN guidelines on artificial enteral nutrition-percutaneous endoscopic gastrostomy (PEG). Clin. Nutr. 24, 848–861 (2005).
Sakamoto, T. et al. Determination of the cut-off score of an endoscopic scoring method to predict whether elderly patients with dysphagia can eat pureed diets. World J. Gastrointest. Endosc. 8, 288–294 (2016).
Chiba, Y. et al. Predictive value of the Hyodo score in endoscopic evaluation of aspiration during swallowing. Auris Nasus Larynx. 45, 1214–1220 (2018).
Stefano, V., Szannne, G. L., Maria-Chiara, C., Tamara, B. H. & Jack, M. G. The value of serum albumin and high-density lipoprotein cholesterol in defining mortality risk in older persons with low serum cholesterol. J. Am. Geriatr. Soc. 49, 1142–1147 (2002).
Light, V. L., Slezak, F. A., Porter, J. A., Gerson, L. W. & McCord, G. Predictive factors for early mortality after percutaneous endoscopic gastrostomy. Gastrointest. Endosc. 42, 330–335 (1995).
Lang, A. et al. Risk factors for mortality in patients undergoing percutaneous endoscopic gastrostomy. Endoscopy 36, 522–526 (2004).
Blomberg, J., Lagergren, P., Martin, L., Mattsson, F. & Lagergren, J. Albumin and C-reactive protein levels predict short-term mortality after percutaneous endoscopic gastrostomy in a prospective cohort study. Gastrointest. Endosc. 73, 29–36 (2011).
Patel, D. A. et al. Economic and survival burden of dysphagia among inpatients in the United States. Dis. Esophagus. 31, 1–7 (2018).
Onder, A. et al. Percutaneous endoscopic gastrostomy: Mortality and risk factors for survival. Gastroenterol. Res. 5, 21–27 (2012).
Tominaga, N. et al. Low serum albumin level is risk factor for patients with percutaneous endoscopic gastrostomy. Intern. Med. 49, 2283–2288 (2010).
Nair, S., Hertan, H. & Pitchumoni, C. S. Hypoalbuminemia is a poor predictor of survival after percutaneous endoscopic gastrostomy in elderly patients with dementia. Am. J. Gastroenterol. 95, 133–136 (2000).
MacLeod, C. S., McKay, R., Barber, D., McKinlay, A. W. & Leeds, J. S. Predicting 30-day mortality following PEG insertion: External validation of the Sheffield Gastrostomy Score and analysis for additional predictors. Clin. Nutr. ESPEN. 42, 227–232 (2021).
Song, Q., Chen, E., Huang, D. & Lv, G. Association of lymphocytes with the duration of survival in artificially fed patients with dysphagia: A retrospective cohort study. World J. Surg. Surg. Res. 5, 1–8 (2022).
Nunes, G., Santos, C. A., Santos, C. & Fonseca, J. Percutaneous endoscopic gastrostomy for nutritional support in dementia patients. Aging Clin. Exp. Res. 28, 983–989 (2016).
Kondwani, J. B. et al. Prevalence of dysphagia and risk of pneumonia and mortality in acute stroke patients: a meta-analysis. BMC Geriatr. 22, 1–10 (2022).
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
K. Shimamoto designed the study, its main conceptual ideas, and the proof outline. R. Matsui significantly contributed to data analysis and interpretation. K.Shimamoto and R. Matsui contributed to the final version of the manuscript. K. Shimamoto and Y.Nishiyama collected the data. K. Nishino and H. Ban contributed to data analysis. All authors critically revised the manuscript, commented on drafts of the manuscript, and approved the final report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shimamoto, K., Matsui, R., Nishiyama, Y. et al. Impact of severe dysphagia on overall survival after percutaneous endoscopic gastrostomy. Sci Rep 15, 3617 (2025). https://doi.org/10.1038/s41598-025-88097-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88097-y