Abstract
Background: Death in dyslipidemia is a significant health problem, dietary intervention plays an important role in this context. Objective: Our study investigated the association between dietary patterns and all-cause mortality in individuals with dyslipidemia. This will lay a foundation for the relevant departments to develop more precise and targeted dietary strategies and help high-risk people with early prevention by adjusting their dietary patterns, which may reduce their mortality and reduce the medical burden. Methods: This study included 5369 participants. Factor analysis identified distinct dietary patterns, each categorized into tertiles based on factor scores: low, medium, and high. Cox proportional hazards regression models were estimated the hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the association between dietary patterns and all-cause mortality in individuals with dyslipidemia. Results: Over a median follow-up of 12.61 years, 365 deaths occurred among the 5369 participants. Four primary dietary patterns were identified. We found that compared to the lowest tertile, the highest tertile of the equilibrium pattern (HR=0.740, 95%CI: 0.565~0.969) and the aquatic products and poultry high loadings pattern (HR=0.757, 95%CI: 0.575~0.997) were negatively correlated with all-cause mortality. Conversely, the grain-tuber and vegetables high loadings pattern (HR=1.338, 95%CI: 1.031~1.737) was positively correlated with all-cause mortality. The oil and salt high loadings pattern (HR=0.973, 95%CI: 0.747~1.268) was not statistically significant. Conclusions: The equilibrium pattern and the aquatic products and poultry high loadings pattern were linked to a lower risk of all-cause mortality among individuals with dyslipidemia, whereas the grain-tuber and vegetables high loadings pattern was linked to a higher risk. The results implying that adopting appropriate dietary pattern could provide survival benefit for individuals with dyslipidemia. However, this study has only considered dietary intake at baseline, and future research should consider the dynamic changes in dietary habits over time.
Similar content being viewed by others
Introduction
Dyslipidemia is characterized by elevated levels of triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), or decreased levels of high-density lipoprotein cholesterol (HDL-C)1,2. It is a multifactorial disease commonly caused by age, genetics, physical activity, current smoking, alcohol consumption and diet3,4. In 2019, a global survey revealed that dyslipidemia caused approximately 98.62 million disabilities and 4.4 million deaths which imposed a vast medical burden2. A study demonstrated that a 10% decrease in all-cause mortality was associated with a 1 mmo1/L drop in LDL-C following statin therapy in a population with varying risk stratification for atherosclerotic cardiovascular disease (ASCVD)5. A meta-analysis of the association between HDL-C and all-cause mortality showed that both higher and lower HDL-C levels could significantly increase the risk of all-cause mortality, demonstrating a J-shaped association6. Abnormal cholesterol levels may increase the risk of both cause-specific and all-cause mortality according to these researches.
In Western countries, the main types of dyslipidemia are high TC and high LDL-C, and the main types of dyslipidemia in Chinese adults are low HDL-C and high TG7. This difference may be related to the low dietary fat and cholesterol intake of the Chinese residents. Unreasonable diet is prone to a variety of chronic diseases such as metabolic syndrome, cardiovascular disease, cancer and death8,9. Cumulative evidence indicates that dietary interventions represent one of the most effective strategies to prevent the risk factors of dyslipidemia10, and targeted shifts to healthier diets could prevent a significant proportion of chronic disease deaths11,12. Previous studies often focused on single nutrients or food groups13,14, which may not fully capture the complex interactions in dietary habits. Therefore, analyzing dietary patterns as a whole has become increasingly important in understanding their impact on health outcomes15. Dietary patterns refer to the amount, proportion, type, or blend of various foods, drinks, and nutrients in a diet, as well as the frequency of their consumption16. Evidently, the analysis of dietary patterns provides a more comprehensive understanding of the association between diet and disease than focusing on a single nutrient or food group17. Dietary patterns are various due to different eating habits in different countries. Rice and wheat are the common staples in China. Some people tend to adopt the traditional Chinese dietary patterns when choosing, which focuses on the combination of grains, vegetables, fruits and meat18. With the development of globalization, some western dietary patterns are gradually introduced and accepted, such as high energy, high fat fast food patterns19. Previous studies have found that healthy dietary patterns decrease the risk of all-cause mortality in the older18 and the female20. However, it is worth noting what effects of dietary patterns on all-cause mortality in individuals with dyslipidemia is unclear.
Therefore, we hypothesize that there might be a specific association between different dietary patterns and all-cause mortality in individuals with dyslipidemia. Our study explored the specific association by obtaining participants’ death information through about 13 years of follow-up. Our ultimate goal is to identify low-risk dietary patterns for dyslipidemia so as to reduce the possibility of death and improve overall survival benefit.
Methods
Study design and participants
This study utilized data from the Guizhou Population Health Cohort Study (GPHCS) which was established in 2010. A total of 9280 permanent residents aged ≥ 18 years were selected from 12 districts (counties) using multi-stage random cluster sampling for baseline investigation. All participants were followed up twice, in 2016–2020 and 2023, with the outcome of this study derived from the second follow-up. Dyslipidemia was defined as a self-reported diagnosis by a doctor or the use of lipid-lowering medications. According to the Chinese Adult Dyslipidemia Prevention and Treatment Guidelines (Revised Edition 2016), the criteria for dyslipidemia are TC ≥ 6.2 mmol/L, TG ≥ 2.3 mmol/L, LDL-C ≥ 4.1 mmol/L, or HDL-C < 1.0 mmol/L21. We excluded participants who were lost to follow-up or lacked clear outcome information that had a total of 5369 participants were included in the final analysis (Fig. 1). This study was approved by the Ethics Committee of the Guizhou Center for Disease Control and Prevention (No. : S2017-02), and all participants provided informed consent.
Data collection
Participant information was collected using the Chinese Chronic Disease Surveillance (2010) personal questionnaire designed by the Chinese Center for Disease Control and Prevention, including general sociodemographic characteristics (gender, age, marital status, educational levels, etc.), lifestyle factors (current smoking, harmful drinking, total activity, etc.), health status (history of hypertension, chronic obstructive pulmonary disease, etc.), and dietary information. Physical examinations included height, weight, blood pressure, and other parameters of all participants, and the blood biochemical indexes included TC, TG, LDL-C, HDL-C. All the medical staff involved in the survey in this study were uniformly trained and passed the assessment.
Assessment of dietary patterns
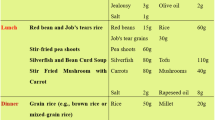
The dietary survey employed a semi-quantitative food frequency questionnaire (FFQ) from the Chinese Chronic Disease Surveillance (2010) individual questionnaire. At baseline, our study assessed the frequency (never, daily, weekly, monthly and annual) and average amount per consumption (in “liang” or “cups (250 ml)”) of 11 types of food items, including grain-tuber products (rice, wheat, potatoes, sweet potatoes, etc.), pork, poultry meats (chicken, duck, geese, etc.), aquatic products (fish, shrimp, etc.), fresh vegetables, fresh fruits, eggs, bean products, dairy products, pastries, and fried foods over the past 12 months. We also assessed the consumption of cooking oil and salt in the past 30 days using the household questionnaire of Chronic Disease and Nutrition Monitoring in Guizhou Province, and then converted these into the daily intake of cooking oil or salt per person according to the number of family dinners. A total of 13 food groups were included. To obtain the dietary patterns of the participants, we used factor analysis to reduce the dimensionality of food; the Kaiser-Meyer-Olkin test (KMO > 0.50) and Bartlett’s test of sphericity (P < 0.05) indicated that the factor analysis was suitable22. We extracted the number of factors based on eigenvalues > 1.0 and the scree plot, if the absolute rotated factor loading ≥ 0.40, it is the characteristic food in this pattern, and the pattern is named according to these foods18. Each pattern was divided into three groups by tertiles of factor scores: low, medium, and high, with higher factor scores indicating greater adherence to that pattern.
Outcomes
The primary outcome was all-cause mortality. Death information of the participants was obtained by contacting the family members of deceased. In other hand, the cause and time of death were traced through the death registration information system of Guizhou Province and the essential public health service system if the family members could not be contacted18. The follow-up data of participants was censored at the time of death, loss to follow-up, or at the end of the follow-up period. Survival time was defined as the period from the date of the baseline survey to the date of death from any cause or the end of follow-up23. Follow-up data of this study were available until August 2023, with a maximum duration of approximately 13 years.
Other covariates
According to the definition by the International Expert Committee, diabetes mellitus was diagnosed as fasting plasma glucose (FPG) ≥ 7.0 mmol/L, 75 g oral glucose tolerance test (OGTT) ≥ 11.1 mmol/L, or being on hypoglycemic therapy24. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg, diastolic blood pressure (DBP) ≥ 90 mmHg, or self-reported use of anti-hypertensive medications25. Cardio-cerebrovascular disease (CVD) was defined as a self-reported diagnosis of CVD by a doctor or the underlying cause of death being myocardial infarction/cerebral haemorrhage/cerebral infarction. Daily smoking was defined as being smoked daily at the time of the survey. Dangerous drinking was defined as an average daily alcohol intake of ≥ 41 g and < 61 g in male drinkers, and ≥ 21 g and < 41 g for female drinkers26. Obesity was defined as a body mass index (BMI) ≥ 28 kg/ m2 27. Marital status was categorized as single, married/cohabiting, divorced/widowed/separated, or others. Educational levels were categorized as junior high school and below, senior high school/technical school, and junior college and above. Habitation was categorized as urban and rural.
Statistical analysis
Data analysis and visualization were conducted using SPSS 26.0 and R 4.3.0. Measurement data not following the normal distribution were expressed as the median (quartile range) and enumeration data were expressed as frequency (constituent ratio). In the General sociodemographic characteristics, comparisons between groups were performed using the Mann-Whitney U test or the chi-square test. In the distribution of baseline characteristics of different dietary patterns, comparisons between groups were performed using the Kruskal-Wallis H test or the chi-square test. We used Schoenfeld residuals to examine the proportional hazards assumption and the main variables’ compliance with the proportional hypothesis (P > 0.05). Multivariate Cox proportional hazards regression models were used to analyze the association between dietary patterns and mortality in individuals with dyslipidemia, with survival time and outcomes (death or survival) as dependent variables and tertiles of factor scores as covariates. Confounders such as gender, age, marital status, daily smoking, dangerous drinking, sleep, hypertension, diabetes, CVD, chronic obstructive pulmonary disease (COPD), asthma, obesity, educational levels, taking lipid-lowering medications, total activity, TC, and LDL-C were adjusted and controlled as covariates. Collinearity between the covariates was weak (VIF < 5, tolerance close to 1). For the key variable of average daily intake of food groups, the missing values were treated by the mean-filling method; other covariates were not processed due to the small number of missing values. The P value of trend tests was calculated by including the median score of each pattern tertile as a continuous variable in the models28. Sensitivity analysis was performed excluding those who were followed up for less than 2 person-years, or were diagnosed with malignant tumors at baseline. All statistical tests were two-sided and P < 0.05 was defined as statistically significant.
Results
General characteristics
Among the 5369 participants, 52.8% were female; 78.7% were married/cohabiting; 69.5% lived in rural areas and 84.7% had an educational level of junior high school or below. There were a total of 365 deaths during the follow-up period. Statistically significant differences were observed between the death group and the survival group in terms of gender, age, marital status, daily smoking, sleep, hypertension, diabetes, CVD, COPD, asthma, educational levels, total activity, TC and LDL-C (P < 0.05), as shown in Table 1.
Classification of dietary patterns
The factor analysis results showed that the KMO test statistic was 0.641(> 0.50) and the P value of the Bartlett test was < 0.001. We extracted four dietary patterns: the equilibrium pattern, which primarily consisted of fresh fruits, eggs, bean products, dairy products and pastries; the oil and salt high loadings pattern, which primarily consisted of cooking oil and salt; the grain-tuber and vegetables high loadings pattern, which primarily consisted of grain-tuber products (rice, wheat, potatoes, sweet potatoes, etc.) and fresh vegetables; and the aquatic products and poultry high loadings pattern, which primarily consisted of poultry meat (chicken, duck, geese, etc.) and aquatic products (fish, shrimp, etc.). The variance contribution rates of the four dietary patterns were 13.20%, 10.45%, 10.41%, and 9.98%; cumulatively, 44.04% of the total variation was explained. The sizes of factor loading for each food group in the four dietary pattern are shown in Fig. 2.
The size of factor loading for each food group in the four dietary pattern. a: Equilibrium pattern; b: Oil and salt high loadings pattern; c: Grain-tuber and vegetables high loadings pattern; d: Aquatic products and poultry high loadings pattern. The values in the radar plot represent the size of the factor payload corresponding to each food group in the four dietary patterns. The factor loading ≥ 0.40 was considered a characteristic food for this dietary pattern.
Distribution of dietary patterns
In the equilibrium pattern, there were differences in gender, marital status, hypertension, etc. In the oil and salt high loadings pattern, there were differences in dangerous drinking, educational levels, etc.; In the grain-tuber and vegetables high loadings pattern, there were differences in gender, daily smoking, etc.; In the aquatic products and poultry high loadings pattern, there were differences in age, sleep, etc. Age, educational levels, TC, and LDL-C showed differences across the four dietary patterns. The details are shown in Table 2.
Longitudinal association of dietary patterns and all-cause mortality
In the fully adjusted model, we found that compared to the lowest tertile, the highest tertile of the equilibrium pattern and the aquatic products and poultry high loadings pattern were associated with a lower risk of all-cause mortality; the grain-tuber and vegetables high loadings pattern was associated with a higher risk of all-cause mortality; the oil and salt high loadings pattern showed no statistical significance either before or after adjustment. And known from the trend test of model 3, those patterns were all statistically significant except the oil and salt high loadings pattern(Table 3). The risk of all-cause mortality in individuals with dyslipidemia also decreased/increased as the factor scores increased(Ptrend <0.05).
Sensitivity analysis
We conducted sensitivity analyses for the model 3 and obtained results similar to the risk analysis above, which were robust and reliable (Fig. 3).
Discussion
This long-term prospective cohort study enhanced the understanding of dietary patterns and all-cause mortality in individuals with dyslipidemia. We found that participants with a higher adherence to the equilibrium pattern and the aquatic products and poultry high loadings pattern had 26.0% and 24.3% lower risks of all-cause mortality, respectively, while the grain-tuber and vegetables high loadings pattern was associated with a 33.8% higher risk of all-cause mortality. In contrast, the oil and salt high loadings pattern was not statistically significant. Therefore, it is important to take action regarding appropriate dietary patterns for individuals with dyslipidemia to diminish mortality risk.
Diet is a direct factor affecting the status of blood lipids29, and it remains relatively stable over a long period30. Adjusting dietary structure is usually the most economical, practical, and acceptable way to reduce the risk of all-cause mortality in individuals with dyslipidemia. The “equilibrium pattern” in our study corresponded to a healthy pattern which included fresh fruits, eggs, soy products, dairy products, and pastries. In the general population, previous studies have found vegetables, fruits, fish, low-fat dairy products, poultry, beans, olive oil, and nuts are common components of a healthy diet, which are negatively correlated with the risk of coronary heart disease, CVD mortality and all-cause mortality31. Probably, vegetables and fruits are rich in dietary fiber, vitamins, polyphenols and other bioactive substances that benefit health. Moreover, dairy products are rich in minerals such as calcium and potassium, and eggs contain unsaturated fatty acids and lecithin, which can effectively reduce TG levels and increase HDL-C levels. Bean products are rich in isoflavones which are involved in the regulation of cholesterol homeostasis32,33 and might change the blood lipid profile of the body, thus reducing the risk of mortality in individuals with dyslipidemia. For the public, dietary patterns that include grains and vegetables are associated with a reduced risk of all-cause mortality16,34. However, the opposite effect was found in our study. The “grain-tuber and vegetables high loadings pattern” was similar to the high carbohydrate pattern because of the high carbohydrate content of cereals and the high starch content of tubers, carbohydrates account for more than 50% of daily energy intake, therefore, the quality and source of these carbohydrates are important because the intake of refined grains is associated with an increased risk of metabolic diseases35, while whole-grain intake is associated with a decreased risk of metabolic disease36. High-carbohydrate diets are common in Asia and countries with poor economic advantages, and tend to contain higher refined carbohydrates such as white rice; these types of diets may reflect poor food quality37 and cause a long-term high-glycemic load, where may lead to negative metabolic consequences38. In China, Guizhou is a province which considers white rice as staple food. The excess will be converted into glucose and stored when carbohydrate intake exceeds the energy consumed by the human body. If the glucose cannot be used in time, it will eventually be converted into fat and stored in the body. Dietary patterns with high intakes of rice and vegetables and moderate intakes of animal foods were associated with an increased risk of general and central obesity39, and obesity is a recognized risk factor for dyslipidemia7. Hyperlipidemia may increase the risk of cardiovascular disease and death from various causes in this population. In the study of Seidelmann et al., there was a U-shaped association between carbohydrate intake and all-cause mortality; a high intake of carbohydrate was associated with a significantly increased risk of all-cause mortality40. The “aquatic products and poultry high loadings pattern” was associated with a lower risk of all-cause mortality. An appropriate amount of fish and seafood can provide the body with a large amount of polyunsaturated fatty acids41,42; high unsaturated fat and low saturated fat content have been proven to improve blood lipid levels43. Therefore, the intake of various aquatic products and poultry has a specific protective effect on blood lipids32. Laural et al. showed that dietary patterns including more unsaturated vegetable oils, fish, or poultry in adults were associated with a decreased risk of all-cause mortality34; we obtained a similar result to that of the general population. In daily diets, lower intake of salt is associated with reduced cardiovascular disease and all-cause mortality44; however, we did not find a significant correlation between the “oil and salt high loadings pattern” and all-cause mortality in individuals with dyslipidemia, which should be confirmed by further research. On these grounds, we recommend that the daily diet should emphasize a balanced diet with various collocations. In addition, we also recommend the intake of high quality protein such as lean meat, fish and shrimp, poultry meat, beans, dairy products, etc. It is worth noting that people with dyslipidemia need to reduce the consumption of refined grains, eat more whole grains such as whole wheat bread, brown rice, which is particularly important for reducing the risk of all-cause mortality in individuals with dyslipidemia.
This study has several strengths. We selected individuals with dyslipidemia as participants who could be more targeted in developing nutritional strategies and interventions for this population and thus potentially reducing their risk of death. Secondly, we used dietary patterns to analyze diet conditions and evaluate the long-term cumulative effect of the diet as a whole which could more comprehensively reflect the impact of actual eating behaviors on the death. Additionally, this study adopted a prospective cohort study which could more accurately explore the causal association between dietary patterns and the risk of all-cause mortality by tracking and observing them over a period, having specific exploratory and unique characteristics in this field. However, we also faced some significant limitations that should be noted. Firstly, dietary surveys looked at the food consumption of participants in the past, and this could be subject to recall bias. Moreover, there was no clear line between dietary patterns. Secondly, our study only assessed the participants’ dietary data at baseline and did not conduct repeated dietary assessments during the follow-up which ignores the dynamic characteristics of diet over time and may introduce some measurement errors. Thirdly, potential effects of dietary confounders such as micronutrient intake were not measured. In addition, our research identified some dietary patterns that are beneficial for individuals with dyslipidemia, but further randomized clinical trials are needed to validate our results.
Conclusion
In conclusion, the findings of this study contribute to a deeper understanding of the association between dietary patterns and the risk of all-cause mortality. Adopting an appropriate dietary pattern can reduce the risk of all-cause mortality and provide survival benefits for individuals with dyslipidemia, thereby promoting the development of public health initiatives aimed at prevention. On the other hand, it deserves our attention that consider the utilization of resources for high-risk population strategies may be more consistent with the cost-benefit principle. Therefore, future research should be more dedicated to making specific dietary recommendations for partial individuals at high risk of mortality in the future, not just the general population.
Data availability
Application for data sets generated during and/or analyzed during the current study may be considered by the corresponding author on reasonable request.
References
Anderson, T. J. et al. The new dyslipidemia guidelines: What is the debate? Can. J. Cardiol. 31, 605 (2015).
Pirillo, A., Casula, M., Olmastroni, E., Norata, G. D. & Catapano, A. L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 18, 689 (2021).
Mary, L. & Adams, J. G. D. L. The impact of key modifiable risk factors on leading chronic conditions. Prev. Med. Int. J. Devoted Pract. Theory. 120, 113 (2019).
Oates, G. R. et al. Sociodemographic patterns of chronic disease: How the mid-south region compares to the rest of the country. Am. J. Prev. Med. 52, 31 (2017).
Baigent, C., Blackwell, L. & Emberson, J. Efficacy and safety of more intense lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomized trials. Lancet 376, 1670 (2010).
Zhong, G. et al. HDL-C is associated with mortality from all causes, cardiovascular disease and cancer in a J-shaped dose-response fashion: A pooled analysis of 37 prospective cohort studies. Eur. J. Prev. Cardiol. 27, 1187 (2020).
Pan, L. et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 248, 2 (2016).
Wang et al. Fruit and vegetable intake and total cause of death and cardiovascular and cerebrovascular death in type 2 diabetes patients. Public. Health China. 39, 1013 (2023). (in Chinese).
Wang, Y. et al. Associations between plant-based dietary patterns and risks of type 2 diabetes, cardiovascular disease, cancer, and mortality - A systematic review and meta-analysis. Nutr. J. 22, 46 (2023).
Neuhouser, M. L. The importance of healthy dietary patterns in chronic disease prevention. Nutr. Res. 70, 3 (2019).
Organization, W. H. Presented at the IChemE (unpublished) (2013).
Joint, W. H. O. F. A. O., Expert Consultation On Diet, N. A. T. P. & Organization, W. H. Diet, nutrition and the prevention of chronic diseases: Report of a Joint WHO/FAO Expert Consultation. Publ. World Health Organ. 916, 1 (2003).
Nguyen, B. et al. Fruit and vegetable consumption and all-cause mortality: Evidence from a large Australian cohort study. Int. J. Behav. Nutr. Phys.. 13, 9 (2016).
Rong, Y. et al. Egg consumption and risk of coronary heart disease and stroke: Dose-response meta-analysis of prospective cohort studies. BMJ-Brit. Med. J. 346, e8539 (2013).
Reedy, J., Subar, A. F., George, S. M. & Krebs-Smith, S. M. Extending methods in dietary patterns research. Nutrients 10 (2018).
Boushey, C. et al. Dietary Patterns and All-Cause Mortality: A Systematic Review (USDA Nutrition Evidence Systematic Review, 2020).
Ocke, M. C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 72, 191 (2013).
Chen, Y. et al. Association between dietary patterns and all-cause mortality in the Chinese old: Analysis of the Chinese Longitudinal Healthy Longevity Survey Cohort. Nutrients 16, 1605 (2024).
Jiang, K. et al. Dietary patterns and obesity in Chinese adults: A systematic review and meta-analysis. Nutrients 14 (2022).
Cai, H. et al. A prospective study of dietary patterns and mortality in Chinese women. Epidemiology 18, 393 (2007).
Chinese Joint Committee for Revised Guidelines for the Prevention. Treatment of dyslipidemia, Chinese guidelines for the prevention and treatment of dyslipidemia in adults (revised 2016). Chin. J. Circ. 31, 937 (2016). (in Chinese).
Luong, R. et al. Empirically derived dietary patterns are associated with major adverse cardiovascular events, all-cause mortality, and congestive cardiac failure in older men: The Concord Health and Ageing in Men Project. J. Nutr. Health Aging. 28, 100020 (2024).
Schober, P. & Vetter, T. R. Survival analysis and interpretation of time-to-event data: The tortoise and the hare. Anesth. Analgesia J. Int. Anesth. Res. Soc. 127, 792 (2018).
Petersmann, A. et al. Definition, classification and diagnosis of diabetes Mellitus. Exp. Clin. Endocr. Diabetes. 126, 406 (2018).
Vischer, A. S. & Burkard, T. Principles of blood pressure measurement - Current techniques, office vs ambulatory blood pressure measurement. Adv. Exp. Med. Biol. 956, 85 (2017).
Mai geng, Z. Data Analysis Manual of Chronic Diseases and risk Factors in China (People’s Health Publishing House, 2022). (in Chinese).
Obesity Group, Endocrinology Branch of Chinese Medical Association. Chinese expert consensus of prevention and treatment of adult obesity. Chin. J. Endocrinol. Metab. 27, 711 (2011). (in Chinese).
Gao, M. et al. Associations between dietary patterns and the incidence of total and fatal cardiovascular disease and all-cause mortality in 116,806 individuals from the UK Biobank: A prospective cohort study. BMC Med. 19, 83 (2021).
Shridhar, K. et al. Association between empirically derived dietary patterns with blood lipids, fasting blood glucose and blood pressure in adults - The India migration study. Nutr. J. 17, 15 (2018).
Nagel, G., Zoller, D., Ruf, T., Rohrmann, S. & Linseisen, J. Long-term reproducibility of a food-frequency questionnaire and dietary changes in the European prospective investigation into cancer and nutrition (EPIC)-Heidelberg cohort. Br. J. Nutr. 98, 194 (2007).
Jayedi, A., Soltani, S., Abdolshahi, A. & Shab-Bidar, S. Healthy and unhealthy dietary patterns and the risk of chronic disease: An umbrella review of meta-analyses of prospective cohort studies. Br. J. Nutr. 124, 1133 (2020).
Schoeneck, M. & Iggman, D. The effects of foods on LDL cholesterol levels: a systematic review of the accumulated evidence from systematic reviews and meta-analyses of randomized controlled trials. Nutr. Metabolism Cardiovasc. Diseases: NMCD. 31, 1325 (2021).
Zhang, T. & Chi, X. X. The effect of genistein on lipid levels and LDLR, LXRalpha and ABCG1 expression in postmenopausal women with hyperlipidemia. Diabetol. Metab. Syndr. 11, 111 (2019).
English, L. K. et al. Evaluation of dietary patterns and all-cause mortality: A systematic review. JAMA Netw. Open 4, e2122277 (2021).
Sahyoun, N. R., Jacques, P. F., Zhang, X. L., Juan, W. & McKeown, N. M. Whole-grain intake is inversely associated with the metabolic syndrome and mortality in older adults. Am. J. Clin. Nutr. 83, 124 (2006).
Ye, E. Q., Chacko, S. A., Chou, E. L., Kugizaki, M. & Liu, S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J. Nutr. 142, 1304 (2012).
Dehghan, M. et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 390, 2050 (2017).
Augustin, L. et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. 25, 795 (2015).
Medina-Remón, A., Kirwan, R., Lamuela-Raventós, R. M. & Estruch, R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit. Rev. Food Sci. 2, 262 (2017).
Seidelmann, S. B. et al. Dietary carbohydrate intake and mortality: A prospective cohort study and meta-analysis. Lancet Public Health 3, e419 (2018).
Tuttolomondo, A. et al. Metabolic and vascular effect of the Mediterranean diet. Int. J. Mol. Sci. 20, 4716 (2019).
Masana, M. F., Koyanagi, A., Haro, J. M. & Tyrovolas, S. n-3 fatty acids, Mediterranean diet and cognitive function in normal aging: A systematic review. Exp. Gerontol. 91, 39 (2017).
Mensink, R. P., Zock, P. L., Kester, A. D. & Katan, M. B. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: A meta-analysis of 60 controlled trials. Am. J. Clin. Nutr. 77, 1146 (2003).
He, F. J., Tan, M., Ma, Y. & MacGregor, G. A. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 75, 632 (2020).
Acknowledgements
We thank all the participants and the managements of the Guizhou Population Health Cohort Study for their participation and assistance.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Guizhou Province Science and Technology Support Program (Grant number: Qiankehe [2018]2819) and the Provincial Key Construction Discipline Project of the Guizhou Provincial Health Commission.
Author information
Authors and Affiliations
Contributions
Conceptualization, L.Y. and F.Z.; Data curation, Y.W.; Formal analysis, Q.A.; Investigation, L.Y. and Y.W.; Methodology, L.Y., L.Y., X.L. and Z.W.; Project administration, T.L.; Resources, Q.A. and T.L.; Software, X.L.; Supervision, T.L; Validation, Q.Z.; Visualization, L.Y.; Writing – original draft, L.Y. and K.T.; Writing – review & editing, L.Y. and Z.W. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Guizhou Center for Disease Control and Prevention (No. : S2017-02), for studies involving humans.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yin, L., Yu, L., Wang, Y. et al. Dietary patterns and risk of all-cause mortality in individuals with dyslipidemia based on a prospective cohort in Guizhou China. Sci Rep 15, 7395 (2025). https://doi.org/10.1038/s41598-025-88101-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88101-5