Abstract
This study aimed to examine the associations between substituting sedentary time (ST) with physical activity and sleep with obesity parameters in adults from eight Latin American countries. The sample consisted of 2173 adults aged 18–65 years. Physical activity, ST and sleep were objectively measured using accelerometers. The parameters of obesity were defined using body mass index (BMI) and waist circumference (WC). Regression analyses were conducted for isotemporal analysis of the association between substituting 30 min/day of ST with light physical activity (LPA), moderate to vigorous physical activity (MVPA) and sleep in relation to BMI and WC. Substituting light physical activity with higher intensity was also analyzed. Substituting 30 min/day of ST with MVPA was significantly associated with lower odds of a higher BMI (OR: 0.993, 95%CI 0.990–0.998) and WC (OR: 0.998, 95%CI 0.998–0.999). Conversely, substituting ST with LPA did not show a significant impact on obesity parameters. However, the substitution of 30 min/day of LPA with MVPA was also associated with lower odds of a higher BMI (OR: 0.993, 95%CI 0.989–0.997). The results highlight the importance of replacing ST and increasing the intensity of physical activity as an effective strategy for preventing and managing obesity in Latin America.
Similar content being viewed by others
Introduction
Obesity is a chronic and complex medical condition characterized by the excessive accumulation of body fat, which can lead to various health impairments, including an increased risk of cardiovascular diseases, type 2 diabetes, certain types of cancer, and other chronic conditions1. It is a major public health concern worldwide, especially in Latin America, where its prevalence has been rising faster than in other regions2. Estimates suggest that by 2030, the prevalence of overweight or obesity in Latin American could reach 81.9%3. Several methods are used to diagnose obesity, with body mass index (BMI) and waist circumference (WC) being the most commonly used due to their simple and low-cost methods. BMI stands out for its wide applicability in obesity research, while WC ensures better sensitivity to assess central obesity4.
One effective strategy for preventing obesity is physical activity. Current global physical activity guidelines recommend 150 min of moderate to vigorous physical activity (MVPA) per week. Accumulating light physical activity (LPA) can also be valuable in preventing obesity5,6. Even those who do not meet the recommended levels of physical activity can benefit from practicing some amount6,7. Conversely, sedentary time (ST) constitutes a significant portion of our day, and high levels of ST can increase the risk of obesity6. It´s important to note that ST is considered an independent behavior from physical activity, and studies have suggested specific amounts of physical activity that can mitigate the health risks associated with ST6,8,9,10.
Therefore, it is evident that physical activity and ST are independently associated with the risk of obesity. However, previous studies have highlighted the need to consider the interdependence of these behaviors when assessing their impact on health parameters6,10,11,12,13. There has been growing interest in research analyzing the theoretical effects of substituting ST with different intensities of physical activity on obesity risk10,13,14,15. To understand the impacts of replacing one behavior with another, the concept of isotemporal substitution has emerged15. This paradigm reveals that the benefits associated with different activities are not only determined by the specific activity itself but also by the activity being replaced10,15.
A day is defined by a 24-hour period that includes sleep, LPA, MVPA and ST. Thus, engaging in one behavior (e.g., walking) requires reducing time spent on another behavior (e.g., watching television)10,14,15. Research has shown that substituting ST with equivalent amounts of LPA or MVPA can reduce the risk of non-communicable chronic diseases10,14.
Despite the need for more evidence on isotemporal substitution of different intensities of physical activity and ST in relation to obesity parameters among adults, the literature on this topic is scarce in Latin America16,17. Most studies utilizing this type of analysis have been conducted with samples from Europe and the United States, which do not reflect the socioeconomic and cultural conditions of Latin American countries10,12,14,16. Given the need for studies that consider the interdependence of physical activity levels, ST and sleep time in relation to obesity, and the scarcity of such analyses in Latin America, the aim of the present study was to examine the associations between substituting ST with physical activity of different intensities and sleep with, and obesity parameters in adults from eight Latin American countries. Our hypothesis is that substituting ST with LPA will be negatively associated with obesity parameters, and that higher intensities of physical activity will likely have an even greater effect on obesity parameters.
Methods
Study design and sample
The Latin American Nutrition and Health Study (Estudio Latinoamericano de Nutrición y Salud, ELANS) is a multicentric, cross-sectional study of nutrition and health surveillance, featuring a nationally representative sample of urban populations from eight Latin American countries in 2014–2015: Argentina, Brazil, Chile, Colombia, Costa Rica, Ecuador, Peru, and Venezuela18.
The study design was meticulously crafted, following a complex, multi-stage sampling model. Each participating country was stratified by clusters to ensure representativeness across all regions. Major urban areas were randomly selected using the probability proportional to size method. The sample size was calculated with a 95% confidence level and a maximum error of 3.49%. More methodological details have been published previously18.
A total of 10,134 individuals (aged 15–65 years) were invited to participate in the study, and 9218 (47.8% men) agreed to participate. Due to logistical and financial constraints, it was not possible to assess physical activity using accelerometers for all participants. Consequently, a subsample of 2737 participants (29.6%) from the ELANS population was selected18,19. To focus solely on the adult population, individuals under 18 years (adolescents) were excluded. Participants with incomplete data were also excluded from the analyses. Thus, 2173 participants were considered for the analyses (Fig. 1).
Ethics approval and consent to participate
The protocol was approved by the Western Institutional Review Board (#20140605) and registered at Clinical Trials (#NCT02226627). All aspects of the study complied with the Declaration of Helsinki. The ethical review boards also approved each site’s specific protocol from the participating institutions, and informed consent/assent from participants was obtained18.
Physical activity, sedentary time and sleep
Data on the amount and intensity of physical activity and ST were obtained using GT3X + Actigraph accelerometers (Fort Walton Beach, FL, USA). This device model has demonstrated acceptable technical reliability for measuring physical activity and ST20.
Participants were provided with an instruction sheet detailing the use of the accelerometer, its position on the body, and contact information for assistance if needed. They were instructed to wear the device attached to an elastic belt at hip level on the right side of the mid-axillary line for seven consecutive days. They were advised to wear the accelerometer while awake, removing it only during sleep, bathing, or swimming. To ensure consistent data, they were encouraged to wear the device for at least 12 h daily during this period. Data collected for at least five days, including at least one weekend day, with a minimum of ten hours of daily wear time (excluding sleep time), were considered acceptable for analysis19.
Records were obtained at a rate of 30 Hz and subsequently transferred using the ActiLife program (V6.0; ActiGraph, Pensacola, FL) in 60-second intervals. Activity counts were classified as follows: 101–1951 counts/min as LPA and > 1952 counts/min as MVPA. ST was classified as any activity below 100 counts/min21,22. All behaviors were converted to min/day for analysis. Participants were instructed to record the times they put on and removed the accelerometer daily. Sleep duration was calculated by identifying periods of inactivity on the accelerometer during valid days, corresponding to the interval between going to bed (removing the device) and waking up (wearing the device again)23. Total sleep duration was expressed in hours per night for evaluation. More information on accelerometer data can be found in a previous publication19.
Obesity parameters
Data on weight and height were obtained while participants wore light clothing and were barefoot, following standardized protocols and using standardized equipment24. Height was measured to an accuracy of 0.5 cm, with the participant’s head positioned in the Frankfurt Plane. Weight was recorded to an accuracy of 0.1 kg after removing all outer garments, heavy items in pockets, shoes, and socks, using a calibrated electronic scale (Seca 213®, Seca Corporation, Hamburg, Germany), following standard procedures24. BMI was subsequently calculated as body weight in kilograms divided by height in meters squared (kg/m2) and categorized as underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obesity (≥ 30.0 kg/m2)25. Adults with a BMI < 25.0 were classified as having a lower BMI, while those with a BMI of ≥ 25.0 were classified as a higher BMI26.
A non-elastic measuring tape with an accuracy of 0.1 cm was used to measure WC following the guidelines of the World Health Organization27. Participants stood upright, and the measurement was taken after a normal expiration at the midpoint between the lower rib and the iliac crest in the horizontal plane, with the reading taken to the nearest centimeter. For defining “higher WC”, we followed the World Health Organization’s cut-off points: >102 cm for men and > 88 cm for women27.
Covariates
A questionnaire was used to collect demographic data, including age (continuous), sex, country (Argentina, Brazil, Chile, Colombia, Costa Rica, Ecuador, Peru and Venezuela) marital status (single, married/cohabiting, widowed, divorced/separated) socioeconomic status (low, medium and high), education level (none/basic, some/completed higher and university graduate), race/ethnicity (mestizo, white, black and other).
Data collection on socioeconomic status was conducted using a questionnaire tailored to the specific characteristics of each country, considering legislative requirements and established local standards. Socioeconomic status was stratified into three categories (high, medium, and low) based on the national indices utilized in each country18.
Statistical analysis
Descriptive statistics for continuous variables were summarized as mean and standard deviation, while categorical variables were presented as frequencies and percentages.
To investigate the association between ST, physical activity (LPA and MVPA) and obesity parameters (i.e., BMI and WC), we employed a generalized additive model with a logistic link (GAM LOGIT). This model was selected for its flexibility in modeling non-linear relationships between variables using smooth splines, offering more accurate results compared to traditional linear models. Since our outcome variables (obesity parameters) are categorical with two levels, we used a binomial distribution with a logit link, which is suitable for modeling the probabilities of these events.
During the model selection process, we started with basic linear and generalized linear models (GLM), testing different distributions and links. We then fitted GAM models using splines and compared them based on goodness-of-fit criteria, such as Akaike Information Criterion and Bayesian Information Criterion, as well as cross-validation tests. The final GAM LOGIT model was more effective in capturing the data’s variability and was used for isotemporal substitution analysis, elucidating the impact of replacing ST with different intensity of physical activity on obesity parameters. Cross-validation tests and confusion matrix analysis were performed, and model assumptions (normality of residuals, homoscedasticity, multicollinearity, and autocorrelation) were evaluated. The results were presented as odds ratio (OR) with 95% confidence interval (95%CI). All analyzes were adjusted for country, age, sex, marital status, socioeconomic status, education level, race/ethnicity, and country. A p-value ≤ 0.05 considered statistically significant. The analyses were conducted using R-v4.4.0 software (R Studio).
Results
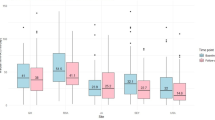
Table 1 provides a profile of study sample. The sample comprised 2173 participants, with 53.2% women, and an average age of 37.9 (SD: 13.0) years. As this study encompasses eight Latin American countries, the majority of participants were from Brazil (19.6%) while the smallest proportion was from Chile (8.4%). Sociodemographic characteristics revealed that 51.9% was married/cohabiting, 51.0% had a high socioeconomic status, 56.9% had only none/basic education level and 52.0% was mestizo. On average, participants spent over 9 h ST, more than 5 h in LPA, less than 1 h in MVPA per day and 10 h sleep. According to BMI, 62.4% were overweight/obese, while 67.5% had abdominal obesity based on WC.
Replacing 30 min/day of ST with MVPA was associated with a 0.7% lower chance of having a higher BMI (OR: 0.993, 95%CI 0.990–0.998). Similarly, substituting 30 min/day of LPA with MVPA resulted in a 0.7% lower chance of having a higher BMI (OR: 0.993, 95%CI 0.989–0.997) (Table 2).
Table 3 shows that isotemporally replacing 30 min/day of ST with MVPA was associated with a 0.2% lower chance of having a higher WC (OR: 0.998, 95%CI 0.998–0.999).
Discussion
The present study aimed to examine the associations between substituting ST with different intensities of physical activity and sleep on obesity parameters, specifically BMI and WC. The results demonstrated that replacing 30 min/day of ST with MVPA was associated with lower odds of having a higher BMI and WC. Additionally, substituting 30 min/day of LPA with MVPA also was associated with lower odds of having a higher BMI.
These findings align with the existing literature, which highlights the potential benefits of replacing ST with MVPA in reducing the odds of obesity, as measured by both BMI and WC. A study conducted in Spain, with subjects aged 55–75 years and BMI between 27 and 40 kg/m2, found that reallocating 30 min/day of ST to MVPA led to significant reductions in both BMI and WC28. Similarly, research in Canada with adults aged 18–79 years observed that substituting ST, LPA or sleep with MVPA was associated with lower BMI and WC, emphasizing the role of MVPA in obesity reduction, particularly among older and overweight/obese individuals29. Furthermore, a study in Japan with adults aged 30–59 years reported decreased body fat mass when replacing 30 min/day of ST or LPA with MVPA, thus supporting the effectiveness of MVPA in managing obesity30.
In the present study, although substituting ST with MVPA yielded favorable results, similar benefits were not observed with LPA. A study involving North American adults found a reduction in WC when substituting sleep, ST or LPA with MVPA, whereas substituting sleep or ST with LPA did not yield significant results31. These findings are consistent with research conducted in Brazil, which showed significant improvements in obesity parameters with ST substitution by MVPA, while substitution by LPA had less consistent effects32.
Conversely, other studies have shown significant benefits of LPA on obesity28,33,34,35. For instance, Galmes-Panades et al. observed reductions in BMI and WC with the reallocation of 30 min/day of ST to LPA28. A study in Greenland indicated that substituting 1 h/day of ST with LPA was associated with lower WC, and replacing with more intense activities resulted in even lower WC. This suggest a negative linear association between total energy expenditure from physical activity and WC and BMI33. Additionally, a Swedish study found that substituting just 10 min/day of ST with LPA was sufficient to reduce WC, with higher intensities leading to even lower WC34. Forthermore, a study in the Netherlands demonstrated that substituting 30 min/day of ST with steps was associated with more favorable WC and lower BMI35.
It is worth noting that studies demonstrating positive effects of substituting ST with LPA on obesity generally involved older participants compared to the present study28,33,34,35. For instance, the study in Spain included a sample with an average age over 55 years28. The Greenland study while having an average age of 43.9 years, included participants aged 18 to 84 years33. Similarly, the study in Sweden focused on older adults aged 50 to 64 years, and the study in the Netherlands had an average age of 60 years34,35. These findings suggest that LPA may have more favorable outcomes for obesity in studies involving older adults, as demonstrated in European and Caribbean studies36,37.
The present study also found no significant results when substituting ST with sleep time. We believe that the potential effects of sleep on obesity prevention could be more pronounced if analyses considered both adherence to sleep duration recommendations and sleep quality38. In studies using isotemporal analyses, the substitution of ST with sleep time and its effects on obesity remain inconclusive and show inconsistent results31,39,40. This inconsistency may be attributed to the set time for isotemporal substitution of behaviors and the similarity in energy expenditure between ST and sleep, as these studies typically focus only on sleep duration without considering adherence to recommended sleep quality and quantity.
The present study provides data from a representative sample across 8 Latin American countries, addressing a significant gap in research on isotemporal substitution of ST with physical activity and its impact on adiposity in adults. Most studies on this topic and population have been published using data from the United States and Europe. Among the few studies in the Latin American region, the study by Gonze et al.32, with data from a specific city in Brazil and through cross-sectional and longitudinal analyses, showed that replacing just 10 min/day of ST with MVPA was the enough to improve obesity rates seen by body mass, BMI and body fat mass32. Our study adds findings on this substitution’s impact on another critical obesity parameters, namely WC. While rare in Latin America, other studies examining isotemporal substitution in obesity have been published, although they involve different age groups compared to ours41,42,43. Other outcomes such as mortality, mental health, biomarkers, and physical fitness were not part of the present study and are also scarce in Latin America and should be considered for future studies16.
The beneficial effects of substituting ST with MVPA on obesity can be explained by various mechanisms. Firstly, this substitution increases total daily energy expenditure, contributing to a caloric deficit and resulting in weight loss44. There is also a potential increase in basal metabolic rate induced by physical activity, which further enhances energy expenditure at rest45. This adaptation may be attributed to the maintenance or increase in lean mass typically associated with higher intensity physical activities, such as strength training, which incurs greater energy expenditure compared to fat mass45,46,47. Physical activity also promotes lipolysis, enhancing fat utilization during exercise, particularly in abdominal region47,48. Hormonal effects from physical activity, such as improved insulin sensitivity and reduced cortisol levels, may contribute to reduced overall and abdominal fat distribution47,49,50. Other related mechanisms could be behavioral, involving lifestyle improvements like better sleep quality and dietary habits, which impact obesity risk50,51,52. All these mechanisms contribute to reducing obesity, and even small substitutions of ST (e.g., 30 min) with MVPA can yield significant health benefits. Furthermore, replacing lower intensity activities with higher intensity ones, such as substituting LPA with MVPA, may be an even more effective strategy in obesity prevention33,34,48. In this regard, even substituting sedentary lying time with sedentary standing time may have beneficial effects53.
Given the increasingly high levels of ST worldwide and declining physical activity rates54,55, especially in Latin America56, this study underscores the importance of reducing ST and replacing it with physical activity. While no significant results were found for LPA, the authors of this study emphasize the health benefits of increasing physical activity of any intensity. Specifically concerning obesity, it is noteworthy that MVPA can offer superior benefits for adults16. Public policies should raise awareness among the population that even small substitutions of ST with physical activity can lead to reduced obesity. Strategies should be developed to promote increased intensity of physical activity among those engaging in LPA, such as replacing slow walking with brisk walking or light jogging.
In this study, we opted for a 30-minute replacement interval because this duration can yield significant health benefits and aligns with the majority of studies conducting isotemporal replacement analyses16. However, it is important to note that smaller increments, such as 10 min, could also be explored in future research. This approach would enable us to capture more realistic changes, considering the challenges the general population faces in increasing their physical activity levels.
The study presents several limitations, including: (I) Sleep time was determined based on device removal at night, which may lead to potential overestimation of sleep duration as participants could remove the device before actually sleeping and start using it after waking up. However, measures were taken to mitigate this issue, including clear instructions for participants to remove the device only when going to bed and to start using it immediately upon waking up. Additionally, participants recorded these times daily, and these records were reviewed to identify and correct any discrepancies; (II) Total accelerometer wear time also varied among participants, which may have influenced the results. Some individuals reported an average of 23 h, while others reported only the minimum requirement of 10 h. To mitigate this limitation, we performed appropriate statistical analyses and tests, utilizing models that account for this variability and comparing different analytical approaches. These efforts helped reinforce the validity of our findings; (III) Accelerometers have limitations in measuring physical activity for individuals engaged in aquatic activities, martial arts, and cycling; (IV) The cross-sectional analysis does not allow for causal interpretation; (V) Isotemporal substitution studies are theoretical models, and despite adjustment for relevant confounding factors, there remains a possibility of unconsidered factors influencing final results; (VI) Other determinants of obesity, such as caloric and dietary intake, were not considered; (VII) Only urban populations were included in the study; (VIII) Although BMI is a widely used and practical measure of obesity in population studies, its low sensitivity and lack of precision in certain contexts limit its ability to capture all aspects of obesity. To address this limitation, we also considered waist circumference as an alternative measure.
On the other hand, the study also has notable strengths that should be considered. These include a large sample size from eight Latin American countries using a rigorous quality control program to ensure high-quality data across all countries18. Objective measures were employed to assess physical activity and ST, which is uncommon in Latin America57. Isotemporal analyses using accelerometer data allow for more precise interpretations related to physical activity and ST. A systematic review of isotemporal analysis and obesity did not identify any published studies using data from Latin America16. Therefore, this study fills an important gap in the literature with data from this region.
Conclusion
In conclusion, our findings suggest that replacing 30 min/day of ST with higher intensity physical activity is associated with lower odds of obesity parameters among Latin American adults. These results reinforce the importance of reducing ST and increasing the intensity of physical activity as a potentially effective strategy for preventing obesity in Latin America. Future research conducting isotemporal analyses with accelerometer data in Latin America would be highly valuable to confirm or refute the findings of the present study.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due the terms of consent/assent to which the participants agreed but are available from the corresponding author on reasonable request. Please contact the corresponding author to discuss availability of data and materials.
References
Purnell, J. Q. What is obesity? Definition as a disease, with implications for care. Gastroenterol. Clin. North. Am. 52, 261–275. https://doi.org/10.1016/j.gtc.2023.03.001 (2023).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642. https://doi.org/10.1016/s0140-6736(17)32129-3 (2017).
Kelly, T., Yang, W., Chen, C. S., Reynolds, K. & He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 32 https://doi.org/10.1038/ijo.2008.102 (2008).
Liu, X., He, M. & Li, Y. Adult obesity diagnostic tool: A narrative review. Med. (Baltim). 103, e37946. https://doi.org/10.1097/md.0000000000037946 (2024).
Amagasa, S. et al. Is objectively measured light-intensity physical activity associated with health outcomes after adjustment for moderate-to-vigorous physical activity in adults? A systematic review. Int. J. Behav. Nutr. Phys. Act. 15, 65. https://doi.org/10.1186/s12966-018-0695-z (2018).
Bourdier, P., Simon, C., Bessesen, D. H., Blanc, S. & Bergouignan, A. The role of physical activity in the regulation of body weight: The overlooked contribution of light physical activity and sedentary behaviors. Obes. Rev. 24, e13528. https://doi.org/10.1111/obr.13528 (2023).
O’Donovan, G., Lee, I. M., Hamer, M. & Stamatakis, E. Association of Weekend Warrior and other Leisure Time physical activity patterns with risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. JAMA Intern. Med. 177, 335–342. https://doi.org/10.1001/jamainternmed.2016.8014 (2017).
Ekelund, U. et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388, 1302–1310. https://doi.org/10.1016/s0140-6736(16)30370-1 (2016).
Silveira, E. A. et al. Sedentary behavior, physical inactivity, abdominal obesity and obesity in adults and older adults: A systematic review and meta-analysis. Clin. Nutr. ESPEN. 50, 63–73. https://doi.org/10.1016/j.clnesp.2022.06.001 (2022).
Chastin, S. F., Palarea-Albaladejo, J., Dontje, M. L. & Skelton, D. A. Combined effects of Time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: A Novel Compositional Data Analysis Approach. PLoS ONE. 10, e0139984. https://doi.org/10.1371/journal.pone.0139984 (2015).
Nishida, Y. et al. Sedentary time, physical activity, and serum SPARC in a middle-aged population. Eur. J. Sport Sci. 22, 1786–1794. https://doi.org/10.1080/17461391.2021.1974573 (2022).
Larsen, S. C., O’Driscoll, R., Horgan, G., Mikkelsen, M. K. & Specht, I. O. Substituting sedentary time with sleep or physical activity and subsequent weight-loss maintenance. Obes. (Silver Spring). 31, 515–524. https://doi.org/10.1002/oby.23631 (2023).
Yamanaka, E. et al. Effects of substituting sedentary time with physical activity on body mass index in Japanese adults with Down syndrome: A cross-sectional study. Heliyon 10, e29294. https://doi.org/10.1016/j.heliyon.2024.e29294 (2024).
Cao, Z., Xu, C., Zhang, P. & Wang, Y. Associations of sedentary time and physical activity with adverse health conditions: Outcome-wide analyses using isotemporal substitution model. EClinicalMedicine 48, 101424. https://doi.org/10.1016/j.eclinm.2022.101424 (2022).
Mekary, R. A., Willett, W. C., Hu, F. B. & Ding, E. L. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am. J. Epidemiol. 170, 519–527. https://doi.org/10.1093/aje/kwp163 (2009).
Grgic, J. et al. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: A systematic scoping review of isotemporal substitution studies. Int. J. Behav. Nutr. Phys. Act. 15, 69. https://doi.org/10.1186/s12966-018-0691-3 (2018).
Sadarangani, K. P. et al. Exchanging screen for non-screen sitting time or physical activity might attenuate depression and anxiety: A cross-sectional isotemporal analysis during early pandemics in South America. J. Sci. Med. Sport. 26, 309–315. https://doi.org/10.1016/j.jsams.2023.04.007 (2023).
Fisberg, M. et al. Latin American Study of Nutrition and Health (ELANS): Rationale and study design. BMC Public. Health. 16, 93. https://doi.org/10.1186/s12889-016-2765-y (2016).
Ferrari, G. L. M. et al. Methodological design for the assessment of physical activity and sedentary time in eight latin American countries - the ELANS study. MethodsX 7, 100843. https://doi.org/10.1016/j.mex.2020.100843 (2020).
Sasaki, J. E., John, D. & Freedson, P. S. Validation and comparison of ActiGraph activity monitors. J. Sci. Med. Sport. 14, 411–416. https://doi.org/10.1016/j.jsams.2011.04.003 (2011).
Matthews, C. E. et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 167, 875–881. https://doi.org/10.1093/aje/kwm390 (2008).
Freedson, P. S., Melanson, E. & Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 30, 777–781. https://doi.org/10.1097/00005768-199805000-00021 (1998).
Colley, R., Connor Gorber, S. & Tremblay, M. S. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. 21, 63–69 (2010).
Lohman, T. G., Roche, A. F. & Martorell, R. Anthropometric Standardization Reference Manual (Human Kinetics Books, 1988).
Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. vol. 894, pp. 1–253 (World Health Organization technical report series, 2000).
Weir, C. B. & Jan, A. BMI classification percentile and cut off points. (2023).
World Health Organization. Waist circumference and waist-hip ratio. (Report of a WHO expert consultation. Geneva, 2008).
Galmes-Panades, A. M. et al. Isotemporal substitution of inactive time with physical activity and time in bed: Cross-sectional associations with cardiometabolic health in the PREDIMED-Plus study. Int. J. Behav. Nutr. Phys. Act. 16, 137. https://doi.org/10.1186/s12966-019-0892-4 (2019).
Colley, R. C., Michaud, I. & Garriguet, D. Reallocating time between sleep, sedentary and active behaviours: Associations with obesity and health in Canadian adults. Health Rep. 29, 3–13 (2018).
Ma, J., Ma, D. & Kim, J. Effects of substituting types of physical activity on body Fat Mass and work efficiency among workers. Int. J. Environ. Res. Public. Health. 18 https://doi.org/10.3390/ijerph18105101 (2021).
Buman, M. P. et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: Associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am. J. Epidemiol. 179, 323–334. https://doi.org/10.1093/aje/kwt292 (2014).
Gonze, B. B., Ostolin, P. & Lopes Valentim Di, T. Effects of substituting sedentary behavior with light-intensity or moderate-to-vigorous physical activity on obesity indices in adults: A prospective short-term follow-up study. Int J Environ Res Public Health. 18, (2021). https://doi.org/10.3390/ijerph182413335
Dahl-Petersen, I. K., Brage, S., Bjerregaard, P., Tolstrup, J. S. & Jørgensen, M. E. Physical activity and abdominal Fat distribution in Greenland. Med. Sci. Sports Exerc. 49, 2064–2070. https://doi.org/10.1249/mss.0000000000001337 (2017).
Ekblom-Bak, E., Ekblom, Ö., Bergström, G. & Börjesson, M. Isotemporal substitution of sedentary time by physical activity of different intensities and bout lengths, and its associations with metabolic risk. Eur. J. Prev. Cardiol. 23, 967–974. https://doi.org/10.1177/2047487315619734 (2016).
JD, V. D. B. et al. Replacement effects of Sedentary Time on metabolic outcomes: The Maastricht Study. Med. Sci. Sports Exerc. 49, 1351–1358. https://doi.org/10.1249/mss.0000000000001248 (2017).
Gába, A. et al. Prospective study on sedentary behaviour patterns and changes in body composition parameters in older women: A compositional and isotemporal substitution analysis. Clin. nutr. 40, 2301–2307. https://doi.org/10.1016/j.clnu.2020.10.020 (2021).
Marron, M. M. & Cvejkus, R. K. Replacing sedentary time with light activity was associated with less adiposity across several depots in African ancestry men. Obes. (Silver Spring). 30, 2489–2496. https://doi.org/10.1002/oby.23582 (2022).
Ogilvie, R. P. & Patel, S. R. The epidemiology of sleep and obesity. Sleep. Health. 3, 383–388 (2017).
Rosique-Esteban, N. et al. Leisure-time physical activity, sedentary behaviors, sleep, and cardiometabolic risk factors at baseline in the PREDIMED-PLUS intervention trial: A cross-sectional analysis. PLoS ONE. 12, e0172253. https://doi.org/10.1371/journal.pone.0172253 (2017).
Varela-Mato, V. et al. Cross-sectional surveillance study to phenotype lorry drivers’ sedentary behaviours, physical activity and cardio-metabolic health. BMJ Open. 7, e013162. https://doi.org/10.1136/bmjopen-2016-013162 (2017).
Cabanas-Sánchez, V., De la Cámara, M. A., Sadarangani, K. P., Higueras-Fresnillo, S. & Martinez-Gomez, D. Associations of daily activities measured by a pattern-recognition activity monitor with overall and abdominal obesity in older people: The IMPACT65 + study. Int. J. Obes. 43, 2545–2554. https://doi.org/10.1038/s41366-019-0439-4 (2019).
Domingues, S. F. & da Diniz, C. Sleep, sedentary behavior, and physical activity in Brazilian adolescents: Achievement recommendations and BMI associations through compositional data analysis. PLoS ONE. 17, e0266926. https://doi.org/10.1371/journal.pone.0266926 (2022).
Moura, B. P., Rufino, R. L., Faria, R. C. & Amorim, P. R. S. Effects of isotemporal substitution of sedentary behavior with light-intensity or moderate-to-vigorous physical activity on cardiometabolic markers in male adolescents. PLoS ONE. 14, e0225856. https://doi.org/10.1371/journal.pone.0225856 (2019).
Powers, S. K. & Howley, E. T. Exercise Physiology: Theory and Application to Fitness and Performance (McGraw-Hill Education, 2015).
Pontzer, H. et al. Daily energy expenditure through the human life course. Science 373, 808–812. https://doi.org/10.1126/science.abe5017 (2021).
D’Onofrio, G., Kirschner, J., Prather, H., Goldman, D. & Rozanski, A. Musculoskeletal exercise: Its role in promoting health and longevity. Prog.s Cardiovasc. Dis. 77, 25–36. https://doi.org/10.1016/j.pcad.2023.02.006 (2023).
Laurens, C., de Glisezinski, I., Larrouy, D., Harant, I. & Moro, C. Influence of acute and chronic exercise on abdominal fat lipolysis: An update. Front. Physiol. 11, 575363. https://doi.org/10.3389/fphys.2020.575363 (2020).
Harris, M. B. & Kuo, C. H. Scientific challenges on theory of fat burning by exercise. Front. Physiol. 12, 685166. https://doi.org/10.3389/fphys.2021.685166 (2021).
Athanasiou, N. & Bogdanis, G. C. Endocrine responses of the stress system to different types of exercise. Rev. Endocr. Metab. Disord. 24, 251–266. https://doi.org/10.1007/s11154-022-09758-1 (2023).
Ruegsegger, G. N. & Booth, F. W. Health benefits of Exercise. Cold Spring Harb Perspect. Med. 8 https://doi.org/10.1101/cshperspect.a029694 (2018).
Sejbuk, M. & Mirończuk-Chodakowska, I. Sleep quality a narrative review on nutrition, stimulants, and physical activity as important factors. Nutrients. 14, (2022). https://doi.org/10.3390/nu14091912
Gillman, M. W. et al. Relationships of physical activity with dietary behaviors among adults. Prev. Med. 32, 295–301. https://doi.org/10.1006/pmed.2000.0812 (2001).
Debache, I. & Bergouignan, A. Associations of sensor-derived physical behavior with metabolic health: A compositional analysis in the record multisensor study. Int. J. Environ. Res. Public. Health. 16 https://doi.org/10.3390/ijerph16050741 (2019).
Church, T. S. et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE. 6, e19657. https://doi.org/10.1371/journal.pone.0019657 (2011).
Thorp, A. A., Owen, N., Neuhaus, M. & Dunstan, D. W. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am. J. Prev. Med. 41, 207–215. https://doi.org/10.1016/j.amepre.2011.05.004 (2011).
Guthold, R., Stevens, G. A., Riley, L. M. & Bull, F. C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Global Health. 6, e1077–e1086. https://doi.org/10.1016/s2214-109x(18)30357-7 (2018).
Ferrari, G. et al. Meeting 24-h movement guidelines and markers of adiposity in adults from eight Latin America countries: The ELANS study. Sci. Rep. 12, 11382. https://doi.org/10.1038/s41598-022-15504-z (2022).
Acknowledgements
The authors would like to thank the staff and participants from each of the participating sites who made substantial contributions to ELANS. The following are members of ELANS Study Group: Georgina Gómez, Attilio Rigotti, Lilia Yadira Cortés, Martha Yépez García, María Liria, Marianella Herrera-Cuenca, Viviana Guajardo.
Funding
Fieldwork and data analysis compromised in ELANS protocol was supported by a scientific grant from the Coca Cola Company, and by grant and/ or support from Instituto Pensi/Hospital Infantil Sabara, International Life Science Institute of Argentina, Universidad de Costa Rica, Pontificia Universidad Católica de Chile, Pontificia Universidad Javeriana, Universidad Central de Venezuela (CENDES-UCV)/Fundación Bengoa, Universidad San Francisco de Quito, and Instituto de Investigación Nutricional de Peru. This paper presents independent research. The views expressed in this publication are those of the authors and not necessarily those of the acknowledged institutions. The funding sponsors had no role in study design; the collection, analyses, or interpretation of data; writing of the manuscript; or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
ERdV, DS, and GF, conceived, designed, and helped to write and revise the manuscript; MF, and I.K., were responsible for coordinating the study, contributed to the intellectual content, and revise the manuscript, DGDC, MF, IK, and PdVM, interpreted the data, helped to write and revise the manuscript. All authors contributed to the study design, critically reviewed the manuscript, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
de Victo, E.R., Sales, D., Christofaro, D.G.D. et al. Isotemporal substitution of sedentary time with different physical activity intensities and sleep in obesity parameters across eight latin American countries. Sci Rep 15, 4081 (2025). https://doi.org/10.1038/s41598-025-88230-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88230-x