Abstract
Total knee arthroplasty (TKA) is an effective treatment for end stage osteoarthritis. However, biopsychosocial features are not routinely considered in TKA clinical decision-making, despite increasing evidence to support their role in patient recovery. We have developed a more holistic model of patient care by using machine learning and Bayesian inference methods to build patient-centred predictive models, enhanced by a comprehensive battery of biopsychosocial features. Data from 863 patients with TKA (mean age 68 years (SD 8), 50% women), identified between 2019 and 2022 from four hospitals in NSW, Australia, was included in model development. Predictive models for improvement in patient quality-of-life and knee symptomology at three months post-TKA were developed, as measured by a change in the Short Form-12 Physical Composite Score (PCS) or Western Ontario and McMasters Universities Osteoarthritis Index (WOMAC), respectively. Retained predictive variables in the quality-of-life model included pre-surgery PCS, knee symptomology, nutrition, alcohol consumption, employment, committed action, pain improvement expectation, pain in other places, and hand grip strength. Retained variables for the knee symptomology model were comparable, but also included pre-surgery WOMAC, pain catastrophizing, and exhaustion. Bayesian machine learning methods generated predictive distributions, enabling outcomes and uncertainty to be determined on an individual basis to further inform decision-making.
Similar content being viewed by others
Introduction
Total knee arthroplasty (TKA) is the standard treatment for end-stage osteoarthritis, improving joint function and attenuating local pain, with low rates of mortality1,2. The cumulative revision rate of TKA has been reported at 8%, over the last 20 years in Australian patients2. TKA is commonly undertaken in people aged over 50, with annual rates of over 60,000 in Australia2 and approximately one million in the USA3. With an ageing population driving an escalation in osteoarthritis cases4, it is anticipated that TKA procedures will rise dramatically over the coming decade5, increasing the burden on healthcare services globally.
Despite perceived high success rates, between 10 and 20% of TKA patients continue to report dissatisfaction with surgery outcomes, reflected by enduring pain, limited function, and diminished quality-of-life7,7. These rates persist, even following recent improvements in surgical procedures such as robotic-guided surgery8 and kinematic prosthetic alignment9.
With current dissatisfaction rates, it is informative to consider standard TKA rehabilitation activities. Although no ‘one’ approach exists, current standards strongly emphasize physical aspects of recovery, with many programs focused on improving knee function and enhancing pain relief10. This strong emphasis is surprising given the increasing evidence that pain and dissatisfaction are not solely due to medical and physical variables11. Indeed, it has been suggested that pre-surgical pain catastrophizing and mental health status are associated with post-TKA pain12.
Driven by the escalating burden and cost to healthcare services, there has been a shift in rehabilitation location and types of care teams, resulting in reductions in hospital-based programs and increases in home and community-based services13. To date, this approach has focused on joint mobility and pain management14, with limited stratification of rehabilitation location based on a patient’s individual social needs or psychological features.
A novel approach is to adopt a biopsychosocial model of health which systematically considers biological, psychological, and socio-environmental factors and their complex interactions in understanding illness, health, and healthcare delivery. Indeed, several psychological factors have been associated with, or have the potential to impact, recovery trajectories following TKA15,16,17,18 as summarised by Ditton et al. 202011. Pre-surgical features such as depression, anxiety, and pain catastrophizing have been correlated with pain levels prior to and following surgery12,19,20, and with the need for surgical revision21. In contrast, other “protective” features, such as resilience and committed action, have been linked to post-surgery recovery rates and quality-of-life22,23. Although the importance of adopting a biopsychosocial approach in musculoskeletal disease models of care is increasingly acknowledged, these factors are not routinely reviewed prior to surgery and remain overlooked in rehabilitation and clinical decision-making24.
There have been relatively few studies that consider the ability of biopsychosocial factors to predict patient outcomes post-TKA. Clinical support tools assessing the impact of a broad range of biopsychosocial parameters on recovery outcomes could enable the clinical validity of a more multifaceted and holistic approach to rehabilitative programs. Furthermore, such tools could identify “at risk” patients based on pre-surgical factors, which may more precisely guide the implementation of pre-surgical interventions and rehabilitation strategies.
The increasing availability of clinical data has resulted in a greater use of artificial intelligence (AI)-based predictive modelling in orthopaedic settings25,26. Predictive modelling has the potential to create clinical decision tools that can address several aspects of TKA patient care and management27. Machine learning (ML), which sits under the umbrella of AI, encompasses multivariate approaches, such as traditional regression techniques. What is beneficial with the additional AI/ML approach considered here is that it allows nonlinear relationships between patient inputs and outcomes. However, the clinical utility of these decision tools for TKA remains limited due to a lack of external validation, such that the widespread clinical utility of the model in a larger population has not yet been determined. Possible issues include dataset limitations such as missing patient measures that were found predictive in other studies, the use of existing datasets, low patient numbers, demographic homogeneity, limited data of variables of interest or incomplete datasets. These issues can hinder exploration of the predictive capacity of the clinical variables of interest27,28.
Further, no attempt has been made to quantify the uncertainty of predicted outcomes, which often provides important information for decision-making, without which assurance may be ascribed to a predicted outcome with false confidence. Quantifying prediction uncertainty can be addressed in a mathematically coherent way by using Bayesian inference,29 which provides a means for describing prediction uncertainty based on the model uncertainty and the available data, which will have direct impact on the clinical utility of the models developed. An additional benefit of using Bayesian machine learning (also under the AI umbrella) is that the generated outcome is a predictive distribution, as opposed to a point estimate as provided by traditional approaches. These techniques provide flexibility and additional information that should be considered in decision-making.
The aim of the current study was to predict improvement and associated prediction certainty in TKA patient outcomes using a comprehensive battery of biopsychosocial features which were selected following an extensive review of the literature11. The impact of pre-surgical features was assessed at three months post-TKA which, although early on in the recovery journey, is associated with the most dramatic change in post-surgery knee function30. Machine learning models based on pre-surgical biopsychosocial features were developed to predict patient-reported TKA outcomes, focussing on improvements in knee symptomology and quality-of-life. A novel Bayesian inference method31 enabled the certainty around the outcome prediction to be determined, further enhancing the clinical use of the model. This approach has the potential to facilitate the allocation of rehabilitation resources towards a more holistic and prioritised model of recovery and the efficiency of rehabilitation service provision.
Methods
Participants
Patients over the age of 18, requiring unilateral or simultaneous bilateral TKA, were referred for inclusion in the study by 11 orthopaedic specialists, with surgery undertaken at one of four Ramsay Healthcare private hospitals in NSW, Australia including: Lake Macquarie Private Hospital, 187 bed capacity facility located in the metropolitan area of a major regional city; Baringa Hospital, 78 bed capacity facility local in a large rural town; Kareena Hospital, 142 bed facility located in the metropolitan area of a major city; and Wollongong Private Hospital, 171 bed facility located in the metropolitan area of a major regional city. Recruitment took place from November 2019 to June 2022. Patients were excluded if they had knee surgery within the prior 6 months, had knee surgery on their other knee scheduled within the following 12 months, or if surgery was due to trauma. All participants provided informed consent prior to study commencement32.
Participant recruitment took place during the COVID-19 pandemic. During this time TKA surgeries were ceased on two occasions for a total duration of 2 months, due to halting elective surgical procedures as mandated by local government bodies. During our recruitment period, we accessed patient surgical schedules with consent of our collaborating surgeons and were able to post and call patients and provide electronic or postal copies of study information. The study design did not require physical contact with the research team as questionnaires were provided online or as hard copies by post. Physical measures were all conducted via telehealth videocall sessions with patients at home eliminating the need for social contact32. When participants were contacted by phone regarding their potential involvement in the study, they were also asked if they consented to undertake 2 physical tests in their home, taking 15 min, that enabled measurements of their mobility, balance, and strength. Participants were provided with a checklist of the following items they required for the video calls:
-
Sufficient internet access and a mobile phone or tablet device or computer with a movable camera.
-
Someone to be at home with them during the call, to assist with holding the device during the call and be there for safety support if the participant stumbles or falls during the assessments.
-
A dining chair or similar chair with a firm seat and arm rests, to perform assessments.
-
A 4-m length floor space with uniform flooring and no trip hazards to perform assessments.
Prior to undertaking study measurements, participants and their support person took part in a training session with the assessor on how to undertake the videocall assessments. During this session the participants were able to practice using the videocall platform and practice undertaking the assessments. To optimize the accuracy of the measurements to be undertaken the assessor discussed with the participant the appropriate location in their home to run the assessments. Appropriate camera location was determined so that the assessor was able to accurately view the participants body positioning during the testing procedures.
Sample size
For machine learning, the required sample size should ensure at least 10 events for each included predictor parameter33. In the current study, we have a total of 39 input variables or 76, after one-hot-encoding, which is a method which converts a categorial variable into multiple separate binary variables (one for each category) to be used in machine learning methods29. This would require 390 participants for models without one-hot-encoding and 760 participants when including one-hot-encoding. We aimed to recruit 1000 TKA patients to ensure sufficient data for predictive modelling analyses, allowing for 20% missing data.
Institutional review board approval
Research methodology was peer-reviewed and approved by the School of Medicine and Public Health at the University of Newcastle, NSW, Australia, in accordance with the Australian Code for the Responsible Conduct of Research. The study was conducted according to the National Statement on Ethical Conduction in Human Research (2007). Ethics approval was granted by the University of Newcastle Human Research Ethics Committee (approval ID: H-2019–0109) on June 21, 2019. Approval for each study site’s participation was reviewed and approved by the Ramsay Research and Governance Office, NSW, Australia.
Predictors and outcome measures
As outlined in the SuPeR Knee™—Support, Predict, Recover protocol (International Registered Report Identifier (IRRID)DERRI-10.2196/48801)),32we included 39 potential biopsychosocial predictive features, collected within the month prior to TKA. Features that had been associated with patient outcomes following TKA were selected based on extensive review of the literature11. Pre-surgery predictors included; psychological features (depression, anxiety, stress, pain catastrophizing, resilience, committed action), sex, age, employment, education, residence (Modified Monash Model34), lifestyle and anthropometric factors (Body Mass Index (BMI), smoking status, physical activity, sleep quality, nutrition/dietary behaviours, alcohol intake), medical history (concomitant conditions, American Society of Anesthesiologists (ASA) score, self-reported Charlson Comorbidity Index), quality-of-life (Short Form-12 (SF-12), physical (PCS) and mental (MCS) health subdomains), knee symptomology and function (Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain, stiffness, knee function sub-scores and the composite score, which is the summation of the sub-scores), pain in other places, and strength and mobility (timed up-and-go, 30-s sit-to-stand, hand grip strength). Participants also reported expectations regarding TKA outcomes, including knee pain attenuation, and achievement of post-surgery activities. The full description of all assessments undertaken can be found in the protocol paper for this study32. A summary of key parameters assessed is shown below:
Body mass index (BMI)
BMI is a highly recognised methods for assessing body weight in adults which is measured by dividing body weight (in kg) by height (in metres) determined prior to surgery35.
Nutrition status
Dietary habits of participants prior to the TKA were assessed using the Starting the Conversion Score (STC)36. The STC is a validated 8-point screening tool used to evaluate dietary habits. Participants rate the frequency of ingesting a range of 8 different food types over the past few months. The total scale ranges from 0 to 16, with higher scores associated with worse dietary habits.
Alcohol consumption
Alcohol consumption prior to TKA was evaluated using a modified version of the Alcohol Use Disorders Identification Test (AUDIT) relating to alcohol consumption only (AUDIT-C)37. Participants were asked 3 questions relating to their average alcohol consumption over the last 12 months, with a maximum total scale score of 12. Total scores < 5 indicated low risk consumption, scores ≥ 5 indicated hazardous or harmful consumption.
Social support
The level of social support participants felt they had available to them prior to their TKA was assessed using the Medical Outcomes Study 6 item Social Support Survey (MOS-SSS-6)38. The survey captures information relating to perceived psychological and material support derived from interpersonal relationships. Scores ranged from 6 to 30, with higher scores indicative of higher levels of perceived support.
Committed action
Committed action is a component of ‘psychological flexibility’ and is defined as a person’s capacity to flexibly engage in effective and adaptive behaviours, guided by personally held values, even in the presence of challenges and discomfort39. We used a shortened form of the Committed Action Questionnaire (CAQ-8), which is comprised of 8 statements. Respondents rate the extent to which each item applies to them ranging from 0 (“never true”) to 6 (“always true”). Total scores are calculated by summing the item scores, with a maximum score of 48. Higher scores denote greater committed action.
Pain catastrophizing
We used the Pain Catastrophizing Scale (PCS)40 to measure the level of catastrophic thinking relating to pain prior to TKA. The self-report form consists of 13 items describing thoughts and feelings patients may experience when they are in pain. Respondents provided ratings for each item on a 5-point Likert scale ranging from, 0 (“not at all”), to 4 (“all the time”). Higher scores are associated with higher amounts of pain catastrophizing, with scores higher than 30 associated with high risk of chronic pain.
Pre-surgery hand grip strength assessment
Hand grip strength measures the maximum amount of static force that a person can apply by their hand whilst gripping a handheld dynamometer. It is a reliable proxy for overall strength, and is related to risk of frailty, falls, functional capacity, morbidity, and mortality41. Hand grip strength was assessed prior to surgery. As this assessment requires the use of a calibrated dynamometer (Jamar Diagnostics, Jamar Plus + Hand Dynamometer); a device was provided to each study site. Hospital site staff were trained to undertake these assessments by a member of the research team prior to study commencement.
Data collection
The secure electronic platform Vision Tree Optimal Care™, developed by VisionTree Software, Inc, San Diego, CA, USA, enabled direct entry of data by participants and served as a centralised data repository. An e-consent form was the first item viewed and completed by participants when accessing the platform, with a hard copy included in any posted questionnaires. Participants were asked to sign the consent form prior to commencing the questionnaires. Any hard copies were posted back to the research team and data was entered to the centralised data repository.
All questionnaires were provided to participants with instructions preceding each form on how to enter their responses. Study staff could be contacted if participants required clarification regarding the questions and answers required, however, all questionnaires were based on participants entering their responses directly themselves on to the data forms. Participants at all study sites were disseminated study questionnaires in the same manner. All participants were instructed to complete questionnaires provided at each assessment time within a 48-h window from commencement, providing those who experienced fatigue additional time to complete their responses. For participants completing online questionnaires, reminder emails were sent to encourage questionnaire completion in a timely manner. If incomplete hard copy questionnaires were received, participants were contacted by phone and missing data was collected verbally32.
Data processing
Data were randomly allocated to either training (used to determine the best model) or test (used to assess model performance) datasets using an 80:20 split, the standard ratio used in the machine learning literature29.
Patients had to complete at least one pre-TKA and post-TKA questionnaire to be included. Two datasets were created based on each outcome, where any patient missing the outcome (either SF-12 PCS or WOMAC composite score) was removed to create the corresponding dataset. Remaining missing input data were imputed by either the population mean for numerical inputs or the population mode for categorical measures.
Input predictors
One-hot-encoding29 was applied to each input variable. The optimal set of input predictors was determined via an improved derivative of the ‘forward selection process’ (see the Supplementary Materials Fig. S1 for more information about this process). The predictive ability of each combination of inputs was determined using a linear regression model, using the fivefold cross-validation root mean square error (RMSE) performance metric (further details provided in Supplementary Materials, Fig. S1).
Output prediction modelling
Machine learning-based predictive modelling was undertaken to evaluate the predictive capacity of pre-surgical features on outcomes three months post-TKA. The primary outcome measure was improvement in quality-of-life (SF-12 PCS) with improvement in knee symptomology and function (WOMAC composite score) the secondary outcome measure. The composite WOMAC score is a global score combining the three sub-scores derived by this tool including assessments of self-reported pain, stiffness and functional impairment experienced by the respondent. We acknowledge that the stiffness score is a minor contributor to the composite score due to limited responses relating to this concept. The global/composite score has been shown to have convergent construct validity with a number of knee physical measures, including range of motion as well as several clinical parameters42. In addition, the composite/global WOMAC score has been used in predictive modelling of patient outcomes following total joint replacement by others43,44 with the score was used as an outcome variable to evaluate surgical outcomes in patients with TKA.
The prediction models considered were standard linear regression and Bayesian DCC-Tree31. The Bayesian DCC-Tree model can be considered a combination of linear regression and decision trees, moving the model definition closer to that of a neural network, giving more flexibility but with added complexity. Details regarding the application of the DCC-Tree method are provided in Supplementary Materials (Supplementary Materials Table 1). The final model chosen for each output was that with the lowest prediction error (RMSE).
Role of the funding source
The funders of this study had no role in the study design, data collection, data analysis, or results interpretation and did not contribute to the writing of this manuscript.
Results
Cohort demographic and clinical characteristics
A total of 1050 TKA patients across the four sites were enrolled to the study. Data was randomly split, resulting in 840 and 210 patient observations in the training and testing sets respectively. Although all patients consented to participate, a small proportion did not complete all pre-TKA or post-TKA questionnaires (n = 40 (4%)). Pre-TKA data was not successfully collected in a small proportion of participants (n = 31 (3%)) and a sub-group of enrolled participants did not complete three-month post-TKA assessments (n = 116 (11%)).
The entire dataset was used to analyse cohort characteristics after removing any patient who did not complete at least one pre-TKA and post-TKA questionnaire. This resulted in 863 patient observations (694 training/169 testing). To understand lost-to-follow-up, we compared pre-surgery age, WOMAC, and SF-12 sub-scores between groups (lost-to-follow-up: n = 116, included: n = 863). The median age of both groups was comparable. However, participants lost-to-follow-up displayed worse knee symptomology (median WOMAC composite: 53 (10–89) versus 45 (0–96), knee pain: 11 (1–20) versus 9 (0–20), function: 36 (8–62) versus 32 (0–68), P ≤ 0.01) and lower quality-of-life (SF-12 MCS: 48.7 (14.9–68.4) versus 54.9 (14.9–73.2), P < 0.001).
Demographic and clinical characteristics of the study cohort are summarised in Table S2 (Supplementary Materials). The participant group was predominantly 60–80 years (79%), with equal sex representation. Most were retired, but 29% reported being employed, of which equal proportions engaged in manual and non-manual activities. Nearly half had attained a high school education, with 49% undertaking tertiary-level education. Most participants identified as Australian (90%) and resided in metropolitan areas within New South Wales, Australia (75%). Unilateral TKA patients (87%) were most associated with an osteoarthritis diagnosis (99%).
Most participants reported one or two co-morbidities, with ASA scores reported at level 1 or 2. The most common concomitant conditions included cardiovascular disease, respiratory conditions, and diabetes. The common classes of concomitant medications included cardiovascular agents/anti-hypertensives, gastrointestinal agents, blood glucose regulators, and respiratory tract agents, with 43% of participants reported taking five or more medications pre-surgery.
The average BMI was within obese class I, with 50% having a BMI in the ‘above normal’ range35. Reported dietary habits were ‘healthy’ (mean nutrition score of 5). Alcohol consumption was low risk (average score < 5)37, although 30% of participants had scores of 5 or greater (associated with hazardous or harmful consumption). Most participants were non-smokers (98%). High availability of social support was reported by most participants, however, 19% reported scores indicative of low levels of available support.
Psychological features were not normally distributed and are presented in Table S2 (Supplementary Materials) as the median and range for each group. Resilience was left-skewed (skewness: 0.49, kurtosis: 3.33), with most participants reporting high levels of resilience prior to surgery. The median pre-surgery committed action score (35) was above that indicative of high levels (32), despite the large range (10–48) reported. Pain catastrophizing was right-skewed (skewness: 1.61, kurtosis: 5.53), with most participants (76%) reporting low levels of pain catastrophizing prior to surgery. The median pre-surgery depression, anxiety, and stress scores were within normal clinical ranges (scores of 0–9, 0–7, and 0–14, respectively45) with data skewed to the right (skewness: 2.03, 2.17, 1.41, kurtosis: 5.53, 9.01, 5.24, respectively) and a high proportion having low scores for each mood state pre-TKA, despite the large range of scores observed.
The expectation of knee pain reduction from TKA was very high, with 97% of the cohort expecting knee pain to be either very much or much improved by surgery. When asked, 75% reported experiencing pain in places other than their operated knee. Those who reported pain at three or more sites (18%) were categorised as experiencing ‘significant other pain’.
Changes in quality-of-life and knee symptomology 3 months after TKA
TKA was associated with variable levels of improvement in participants’ quality-of-life and knee symptomology at three months post-surgery. Figure 1 shows the distribution of SF-12 PCS and WOMAC composite scores prior to and following surgery. TKA was associated with a significant 21% increase in median SF-12 PCS scores three months post-surgery (45.11 (17.42–63.67)) compared to pre-TKA (37.2 (17.09–58.6)), (Z = -19.14, P < 0.001) with an average change of 6.73 points. Knee symptomology was also improved by TKA, evidenced by a significant reduction (52%) in median WOMAC composite scores three months post-surgery (21 (0–77)) compared to pre-TKA (44 (0–96)), (Z = 23.24, P < 0.001), with an average change of 21.94 points.
Data processing
The final datasets included 682 training and 169 testing datapoints for the SF-12 PCS improvement outcome and 687 training and 169 testing datapoints for the WOMAC composite score improvement outcome. For SF-12 PCS, 4.5% of input training data values were imputed and 4.8% within the testing dataset. For WOMAC composite, 3.6% of input training data values were imputed and 3.3% within the testing dataset.
Retained predictive variables
Table 1 lists the pre-surgical features retained in the machine learning linear regression models for each outcome. In addition to the pre-TKA value, retained parameters included knee symptomology, pain, lifestyle, psychological, and physical functioning. The number of retained features was selected to ensure both optimal performance and logistical feasibility for collection in a clinical setting.
Machine learning predictive models
Table 2 shows the lowest test RMSE for the quality-of-life outcome was achieved by the machine learning-AI Bayesian DCC-Tree model (RMSE 8.01) and linear regression model for knee symptomology (RMSE 13.34). Reported R2 ranged from 0.24 (quality-of-life) to 0.45 (knee symptomology). Additional performance metrics are provided in Table S3 (Supplementary Materials).
Bayesian Modelling
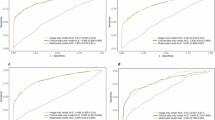
Figure 2 highlights the importance of using Bayesian methods to provide estimates of the range of predictive certainty. Figures 2a,c show example Bayesian predictive distribution for the SF-12 PCS and WOMAC outcome measures respectively. In both cases, the distribution indicates good confidence in the prediction, with the range of high probability density function (PDF) values corresponding to the true patient outcome (purple line), which is also close to that predicted by the standard linear regression model (green line).
However, Fig. 2b,d show examples where the distribution indicates less certainty about the prediction. In Fig. 2b, the true patient outcome is sufficiently different from that predicted by the standard linear regression model, but importantly, is still captured within the range of the distribution. In Fig. 2d, the range of highest PDF values include the true patient outcome, although the other regions are still relatively high, including that which corresponds to the linear regression model. In both cases, the standard linear regression prediction would not accurately reflect the patient’s true trajectory, and moreover incorrectly predicts a positive change, which would negatively affect subsequent decision-making.
Discussion
This study aimed to develop biopsychosocial-based, machine learning models to predict changes in quality-of-life and knee symptomology for individuals following TKA. These models could be used in the development of clinical decision support tools to: improve post-TKA patient outcomes; evolve the type and setting of rehabilitation or pre-habilitation; or help develop the biopsychosocial model of care. To our knowledge, we have considered the most comprehensive battery of pre-surgical biopsychosocial features in TKA predictive models to date.
Our goal was to develop models with optimal performance, a realistic number of inputs, and good clinical validity. The input selection process resulted in the retention of 18 predictors, 13 for each outcome (8 common), from a possible 76 features. The predictive models accounted for up to 24% of the variance in improvement in quality-of-life and 40% for knee symptomology at three months post-TKA. We acknowledge that inclusion of other clinical and surgical variables may lead to improved model performance by accounting for the remaining outcome variance. Indeed, it would be of interest to explore the impact of biopsychosocial features combined with additional surgical and clinical features. This may strengthen the clinical utility of predictive models to inform pre-habilitation and rehabilitation approaches. Our findings reaffirm the importance of biopsychosocial features in patient recovery post-TKA, challenging the prevalent notion that recovery outcomes are primarily determined by joint features and surgical procedures. The predictive models have the potential to complement existing clinical examination and patient engagement by objectively forecasting health outcomes, or by stratification of patients, such that those at risk can be identified and potential patient-tailored therapeutic strategies implemented.
Our protocol enabled the effective prospective collection of patient data to be directly entered into a digital repository. This approach was readily accepted and adhered to by our cohort, with only 11% lost-to-follow-up. Our findings support potential implementation within the clinical setting, enhancing data acquisition for clinical decision-making. Clinical decision tools derived from this data could provide specialists with an evidence-based approach to inform rehabilitation and care in the most efficient and potentially cost-effective manner.
For both outcomes, we observed the pre-surgical value was predictive of the magnitude of change of that variable at three months post-surgery. Those with a higher (better) pre-surgery SF-12 PCS had a lower change post-TKA, with higher changes for those reporting lower pre-surgery values. Similarly, a higher (worse) pre-surgery WOMAC composite score was predictive of a greater change post-TKA, with lower pre-surgery scores resulting in less change. Similar findings have been reported by others, where although TKA patients with higher pre-surgery quality-of-life reported higher post-TKA quality-of-life, the magnitude of change was greater for those with lower pre-TKA quality-of-life46,47,48. As such, pre-surgical features can enable informed patient decision-making regarding TKA, which in turn may influence post-surgical satisfaction.
Other retained variables include modifiable psychological and lifestyle features such as committed action, pain catastrophizing, nutrition status, and alcohol intake, all of which can potentially inform pre-habilitation and rehabilitation strategies to improve patient outcomes. Possible interventions have been reported: committed action can be enhanced by Acceptance and Commitment Therapy49,50, while pain catastrophizing can be attenuated by cognitive behavioural therapy, although research of the impact on post-TKA pain and function has been limited to date51.
It is difficult to directly compare our model performance to those in the literature due to a lack of studies considering the same outcome measures. However, one study52 reported RMSE and R2 for a linear model to predict changes in Oxford Knee Score function (RMSE = 14.33, R2 = 0.39) and pain (RMSE = 18.93, R2 = 0.19) 12 months post-TKA, which was comparable to our reported performance for the three-month post-TKA WOMAC composite model.
One of the benefits of using a probabilistic machine learning modelling approach is the generated predictive uncertainty estimates. Our results showed the ability to perform inference and quantify the prediction uncertainty for clinical outcomes. The novel Bayesian DCC-Tree method showed good predictive performance when applied to the TKA dataset and performed similarly to the linear regression model. Predictive distributions showed that the true outcome was often supported, even when far from the linear regression prediction. Our findings provide interesting insight into the improvements machine learning and Bayesian methods can provide to existing clinical prediction models for TKA.
Several limitations to our study are worth noting. First is possible response bias, considering that our lost-to-follow-up group, albeit 11%, was characterised by worse knee symptomology and quality-of-life. We also observed skewness in pre-surgery psychological features, with a high proportion of the cohort displaying normal mood status, low pain catastrophizing, and high committed action, and as such, the true effects of these predictors may be underestimated. Secondly, recovery outcomes were assessed three months post-TKA. Although possibly considered early in the recovery journey, changes in knee symptomology occur rapidly within the first three months, with subsequent, slower, improvements continuing up to 12 months post-surgery30,53. The impact of psychological factors on patient outcomes may differ at later time points, and as such, analysis from the current study may be limited to early recovery outcomes. While beyond the current scope, investigating the predictive capacity of biopsychosocial features on patient quality-of-life and knee symptomology at later post-surgical timepoints would be of interest. Lastly, we were mindful of reducing surgeon and institutional bias by including patients referred by 11 surgeons across four hospitals. However, all procedures were undertaken in the private healthcare sector. As patients undergoing TKA may differ in the public sector, external validation will be required to assess suitability in a wider clinical setting.
Conclusions
The improvement in patient quality-of-life and knee symptomology three months post-TKA can be predicted based on patients’ pre-surgery biopsychosocial features. This study substantiates the importance of a more comprehensive and holistic therapeutic strategy for TKA and post-operative rehabilitation. Bayesian analysis emphasised the importance of considering the predictive uncertainty, where this information could better inform clinical decision-making. Our predictive models have the potential for stratification according to individual needs, allowing for more targeted service provision, maximizing the impact potential, and supporting appropriate follow-up rehabilitation services by identifying ‘at risk’ individuals early in their recovery journey.
Data availability
Data sharing of the SuPeR Knee data are de-identified participant-level data. Access with be through the Principal Investigator, or named delegate, contacted at karen.ribbons@newcastle.edu.au after approval of a written proposal, with a signed data access agreement after publication of this manuscript. A full data dictionary will be available. The study protocol is available via open access https://www.researchprotocols.org/2023/1/e48801/
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body Mass Index
- DCC:
-
Divide, Conquer, Combine
- PDF:
-
Probability density function
- RMSE:
-
Root Mean Square Error
- SF-12 MCS:
-
Short Form Version 12 Mental Health Composite Score
- SF-12 PCS:
-
Short Form Version 12 Physical Health Composite Score
- TKA:
-
Total knee arthroplasty
- WOMAC:
-
Western Ontario and McMasters Universities Osteoarthritis Index
References
Robertsson, O. et al. Knee arthroplasty in Denmark, Norway, and Sweden. A pilot from the Nordic Arthroplasty Register Association. Acta Orthop. 81(1), 82–89. https://doi.org/10.3109/17453671003685442 (2010).
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee, and Shoulder Arthroplasty: Annual Report 2022. Adelaide, SA: AOA.
Singh, J. A., Yu, S., Chen, L. & Clevland, J. D. Rates of total joint replacement in the United States: Future projections to 2020–2040 using the national inpatient sample. J. Rheumatol. 46(9), 1134–1140. https://doi.org/10.3899/jrheum.170990 (2019).
Chen, X., Tang, H., Lin, J. & Zeng, R. Temporal trends in the disease burden of osteoarthritis from 1990 to 2019, and projections until 2030. Plos One 18(7), e0288561. https://doi.org/10.1371/journal.pone.0288561 (2023).
Shichman, I., Roof, M., Askew, N., Nherera, L., Rozell, J. C., Seyler, T.M., Schwarzkopf R. Projections and epidemiology of primary hip and knee arthroplasty in medicare patients to 2040–2060. JBJS Open Access e22.00112 (2023). https://doi.org/10.2106/JBJS.OA.22.00112
DeFrance, M. J. & Scuderi, G. R. Are 20% of patients actually dissatisfied following total knee arthroplasty? A systematic review of the literature. J. Arthroplasty 38, 594–599. https://doi.org/10.1016/j.arth.2022.10.011 (2023).
Kahlenberg, C. A. et al. Patient satisfaction after total knee replacement: A systematic review. HSS J. 14, 192–201. https://doi.org/10.1007/s11420-018-9614-8 (2018).
Saber, A. Y., Marappa-Ganeshan, R., Mabrouk, A. Robotic-Assisted Total Knee Arthroplasty. [Updated 2023 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564396/
Gao, Z.-X. et al. Comparison of kinematic alignment and mechanical alignment in total knee arthroplasty: A meta-analysis of randomized controlled clinical trials. Orthop. Surg. 12, 1567–1578. https://doi.org/10.1111/os.12826 (2020).
Sattler, L., Hing, W. & Vertullo, C. Changes to rehabilitation after total knee replacement. Austr. J. Gen. Pract. 49(9), 587–591. https://doi.org/10.31128/AJGP-03-20-5297 (2020).
Ditton, E. et al. Improving patient outcomes following total knee arthroplasty: Identifying rehabilitation pathways based on modifiable psychological risk and resillience factors. Front. Psychol. 11, 1–15 (2020).
Olsen Lindberg, M. F. et al. Factors correlated with pain after total knee arthroplasty: A systematic review and meta-analysis. Plos One 18(3), e0283446 (2023).
Naylor, J. M., Hart, A., Mittal, R., Harris, I. & Xuan, W. The value of inpatient rehabilitation after uncomplicated knee arthroplasty: A propensity score analysis. Med. J. Australia 207(6), 250–255. https://doi.org/10.5694/mja16.01362 (2017).
Bravi, M. et al. upervised versus unsupervised rehabilitation following knee arthroplasty: A systematic review and meta-analysis. The Knee 40, 71–89. https://doi.org/10.1016/j.knee.2022.11.013 (2023).
Shan, Y. et al. Predictors of psychological resilience trajectories in patients with knee arthroplasty: A longitudinal study. J. Adv. Nurs. 16, 1–13. https://doi.org/10.1111/jan.15421 (2022).
Cremeans-Smith, J. K., Greene, K. & Delahanty, D. L. Resilience and recovery from total knee arthroplasty (TKA): A pathway for optimizing patient outcomes. J. Behav. Med. 45(3), 481–489. https://doi.org/10.1007/s10865-022-00287-5 (2022).
Springer, B. D. & Sotile, W. M. The psychology of total joint arthroplasty. J. Arthroplasty 35, S46–S49. https://doi.org/10.1016/j.arth.2020.01.002 (2020).
Kazarian, G. S., Anthony, C. A., Lawrie, C. M. & Barrack, R. L. The impact of psychological factors and their treatment on the results of total knee arthroplasty. J. Bone Joint Surg. Am. 103, 1744–1756. https://doi.org/10.2106/JBJS.20.01479 (2021).
Ashoorion, V. et al. Predictors of persistent post-surgical pain following total knee arthroplasty: A systematic review and meta-analysis of observational studies. Pain Med. 24(4), 369–381 (2023).
Hardy, A. et al. Pain catastrophizing and pre-operative psychological state are predictive of chronic pain after joint arthroplasty of the hip, knee or shoulder: Results of a prospective, comparative study at one year follow up. Int. Orthop. 46, 2461–2469. https://doi.org/10.1007/s00264-022-05542-7 (2022).
Sorel, J. C. et al. Do symptoms of anxiety and/or depression and pain intensity before primary total knee arthroplasty influence reason for revision? Results of an observational study from eh Dutch arthroplasty register in 56,233 patients. General Hosp. Psychiatry 78, 42–49. https://doi.org/10.1016/j.genhosppsych.2022.07.001 (2022).
Nwankwo, V. C. et al. Resilience and pain catastrophizing among patients with total knee arthroplasty: A cohort study to examine psychological constructs as predictors of post-operative outcomes. Health Qual. Life Outcomes 19, 136. https://doi.org/10.1186/s12955-021-01772-2 (2021).
Trinh, J. Q. et al. Resilience and depression influence clinical outcomes following primary total joint arthroplasty. J. Arthroplasty 36, 1520–1526. https://doi.org/10.1016/j.arth.2020.11.032 (2021).
Lin, I. et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: Systematic review. Br. J. Sports Med. 54, 79–86. https://doi.org/10.1136/bjsports-2018-099878 (2020).
Entezari, B. et al. Improving resource utilization for arthroplasty care by leveraging machine learning and optimization: A systematic review. Arthroplasty Today 20, 101116. https://doi.org/10.1016/j.artd.2023.101116 (2023).
Chang, W.-J., Naylor, J., Nararajan, P., Liu, V. & Adie, S. Evaluating methodological quality of prognostic prediction models on patient reported outcome measures after total hip replacement and total knee replacement surgery: A systematic review protocol. Syst. Rev. 11, 165. https://doi.org/10.1186/s13643-022-02039-7 (2022).
Kurmis, A. P. A role for artificial intelligence applications insides and outside of the operating theatre: A review of contemporary use associated with total knee arthroplasty. Arthroplasty 5(1), 40. https://doi.org/10.1186/s42836-023-00189-0 (2023).
Cochrane, J. A. et al. Clinical decision support tools for predicting outcomes in patients undergoing total knee arthroplasty: A systematic review. J. Arthroplasty 36(5), 1832–1845 (2021).
Murphy, K. P. Machine learning: a probabilistic perspective (MIT Press, 2012).
Naal, F. D. et al. Clinical improvement and satisfaction after total joint replacement: A prospective 12-month evaluation on the patients’ perspective. Qual. Life Res. 24, 2917–2925. https://doi.org/10.1007/s11136-015-1042-3 (2015).
Cochrane JA, Wills A, Johnson SJ. Divide, Conquer, Combine Bayesian Decision Tree Sampling. arXiv preprint arXiv:2403.18147. 2024 Mar 26.
Ribbons, K. et al. Using pre-surgical biopsychosocial features to develop an advanced clinical decision-making support tool for predicting recovery trajectories in patients undergoing total knee arthroplasty (SuPeR Knee – Support, Predict, Recover): Protocol for a prospective observational study. JMIR Res. Protocols 12, e48801 (2023).
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R. & Feinstein, A. R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 49(12), 1373–1379. https://doi.org/10.1016/s0895-4356(96)00236-3 (1996).
Australian Government, Department of Health and Aged Care. Modified Monash Model. Canberra, Australia: Australian Government, Department of Health and Aged Care; 2021. https://www.health.gov.au/health-topics/rural-health-workforce/classifications/mmm. Accessed October 2, 2022
Australian Government Department of Health and Aged Care. 29 July 2021. www.https/health.gov.au/topics/overweight-and-obesity/bmi-and-waist
Paxton, A., Strycker, L., Toobert, D., Ammerman, A. & Glasgow, R. Starting the conversation performance of a brief dietary assessment, and intervention tool for health professionals. Am. J. Prev. Med. 40(1), 67–71. https://doi.org/10.1016/j.amepre.2010.10.009 (2011).
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D. & Bradley, K. A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care of Quality Improvement (ACQUIP). Alcohol use disorders identification test. Arch. Intern Med. 158(16), 1789–1795. https://doi.org/10.1001/archinte.158.16.1789 (1998).
Holden, L., Lee, C., Hockey, R., Ware, R. S. & Dobson, A. J. Validation of the MOS Social-Support Survey 6-item (MOS-SSS-6) measure with two large population-based samples of Australian women. Qual. Life Res. 23, 2849–2853. https://doi.org/10.1007/s11136-014-0741-5 (2014).
McCracken, L., Chilcot, J. & Norton, S. Further development in the assessment of psychological flexibility: A shortened Committed Action Questionnaire (CAQ-8). Eur. J. Pain 19, 677–685. https://doi.org/10.1002/ejp.589 (2015).
Sullivan, M. J. L., Bishop, S. R. & Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 7(4), 524–532 (1995).
Roberts, H. C. et al. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 40(4), 423–429. https://doi.org/10.1093/ageing/afr051 (2011).
McConnell, S., Kolopack, P. & Davis, A. M. The Western Onatrio and McMaster Universities Osteoarthritis Index (WOMAC): A review of its utility and measurement properties. Arthritis Rheum. 45(5), 453–461 (2001).
Dowsey, M. M., Spelman, T. & Choong, P. F. Development of a prognostic nomogram for predicting the probability of nonresponse to total knee arthroplasty 1 Year after surgery. J. Arthroplasty 31, 1654e60 (2016).
Garriga, C. et al. Development of a model predicting non-satisfaction 1 year after primary total knee replacement in the UK and transportation to Switzerland. Sci. Rep. 8, 3380 (2018).
Lovibond, P. F. & Lovibond, S. H. The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 33(3), 335–343 (1995).
Zhou, Y., Dowsey, M., Spelman, T., Choong, P. & Schilling, C. SMART choice (knee) tool: A patient-focused predictive model to predict improvement in health-related quality of life after total knee arthroplasty. ANZ J. Surg. 93, 316–327 (2023).
Ohyama, Y., Iwamura, T., Hshino, T. & Miyata, K. Prognostic models of quality of life after total knee replacement: A systematic review. Physiother. Theory Pract. 10, 1–12. https://doi.org/10.1080/09593985.2023.2211716 (2023).
Hofstede, S. N. et al. The influence of preoperative determinants on quality of life, functioning and pain after total knee and hip replacement: A pooled analysis of Dutch cohorts. BMC Musculoskeletal Disord. 19(1), 68. https://doi.org/10.1186/s12891-018-1991-0 (2018).
Lin, J., Klatt, L.-I., McCracken, L. M. & Baumeister, H. Psychological flexibility mediates the effect of an online-based acceptance and commitment therapy for chronic pain: An investigation of change processes. Pain J. Online 159(4), 663–672. https://doi.org/10.1097/j.pain.0000000000001134 (2018).
Roddy, M. K. et al. One-day acceptance and commitment therapy workshop for preventing persistent post-surgical pain and dysfunction in at-risk veterans: A randomized controlled trial protocol. J. Psychom. Res. 138, 110250. https://doi.org/10.1016/j.jpsychores.2020.110250 (2020).
Buvanendran, A. et al. Preoperative cognitive-behavioural therapy for reducing pain catastrophizing and improving pain outcomes after total knee replacement: A randomized clinical trial. Reg. Anesth. Pain Med. 46, 313–321. https://doi.org/10.1136/rapm-2020-102258 (2021).
Buus, A. A. O. et al. Patient -reported outcomes for function and pain in total knee arthroplasty patients. Nurs. Res. Online 71(5), E39–E47. https://doi.org/10.1097/NNR.0000000000000602 (2022).
Kuklinski, D. et al. Thresholds for meaningful improvement in WOMAC scores need to be adjusted to patient characteristics after hip and knee replacement. J. Orthop. 29, 50–59. https://doi.org/10.1016/j.jor.2022.01.002 (2022).
Acknowledgements
We would like to acknowledge the SuPeR Knee research assistants who were involved with data collection for this study. We are thankful to the Centre for Rehab Innovations (CRI) data analysts for their role in data management, processing, and analysis. We also extend our thanks to the CRI team members for their involvement in the study design and administrative support for the project. We would also like to acknowledge the time provided by all study participants, and the collaboration and support from all participating Ramsay Healthcare Orthopaedic surgeons and their administrative teams involved with participant enrolment to the study.
Funding
Funding for this study was provided by the Ramsay Hospital Research Foundation, Sydney, Australia.
Author information
Authors and Affiliations
Contributions
MN, MP, RW, SJ, AW conceptualized the study. MN was instrumental in funding acquisition. KR and JC wrote the original draft with all other co-authors involved in the review and editing process. JC, SJ and KR directly accessed and verified the underlying data reported in this manuscript and undertook the machine learning and statistical analysis. ED provided insights into the data collection tools and clinical validity of the study findings. SJ and AW supervised the data collection and processing aspects of the study. KR managed the project administration and all aspects of the investigation. RW, MP and MN provided guidance with the scope and clinical aspects of the protocol. MN oversaw the project. All authors agreed to the publication of the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethics approval was granted by the University of Newcastle Human Research Ethics Committee (approval ID: H-2019-0109) on June 21, 2019.
Consent to participate
Informed consent was obtained from all participants who took part in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ribbons, K., Cochrane, J., Johnson, S. et al. Biopsychosocial based machine learning models predict patient improvement after total knee arthroplasty. Sci Rep 15, 4926 (2025). https://doi.org/10.1038/s41598-025-88560-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88560-w