Abstract
To compare the long-term outcomes of monovision surgery using implantable collamer lens (ICL) V4c and femtosecond laser-assisted in situ keratomileusis (FS-LASIK) in myopic patients with early presbyopia. This case series study included 48 eyes of 24 patients (male/female: 10/14, mean age 45.50 ± 3.82 years) and followed-up for 4.5 years (54.00 ± 9.77 months). Patients were examined for spherical equivalent, uncorrected distance visual acuity, corrected distance visual acuity, intraocular pressure, presbyopic add power, visual acuity (VA) (logMAR) of dominant eyes (D-eye), non-dominant eyes (nD-eye), and both eyes (Bi) at 0.4 m, 0.8 m, and 5 m, corneal wavefront aberration, and contrast sensitivity (CS). All surgeries were uneventful. The safety indices of ICL V4c group and FS-LASIK group were 1.17 ± 0.30 and 0.98 ± 0.20 (p < 0.05), and the efficacy indices were 0.79 ± 0.07 and 0.52 ± 0.07 (p < 0.05) respectively. The binocular VA (logMAR) of ICL V4c group and FS-LASIK group at 5.0 m were: 0.02 ± 0.11, 0.18 ± 0.30; 0.8 m: 0.09 ± 0.12, − 0.01 ± 0.11; 0.4 m: − 0.02 ± 0.06, − 0.03 ± 0.08, (p > 0.05 at three distances). Compared with ICL V4c group, lower CS was observed at 1.0 cpd in the FS-LASIK group (1.07 ± 0.31 vs. 0.80 ± 0.51, p = 0.043). Monovision surgery using ICL V4c and FS-LASIK provides good binocular visual acuity at near-to-far distances in myopia patients in the presbyopia age group.
Similar content being viewed by others
Introduction
In 2015, the global prevalence of presbyopia was estimated at 1.8 billion individuals, which increased to 2.1 billion by 20201,2,3. By the year 2050, it is projected that the population with myopia will reach a staggering number of 4.758 billion people, out of which approximately 938 million are expected to have high myopia4. With the aging population, there will be a significant rise in the number of individuals over the age of 40 affected by both myopia and presbyopia. Monovision has emerged as a widely utilized clinical approach for managing myopia in patients with presbyopia5,6,7, involving correction of distant vision in the dominant eye (D-eye) and near vision in the non-dominant eye (nD-eye). Various methods can be employed for monovision treatment including frame spectacles, contact lenses, corneal inlays, Implantable Collamer Lens (ICL) implantation, and lens replacement procedures2,3.
Currently, mainstream refractive surgery like corneal refractive surgery and ICL implantation has great potential for the correction of myopia in the presbyopia age patients8,9,10. The safety and efficacy indices were significantly lower in patients > 40 years old 6 months after femtosecond laser small incision lenticule extraction, with astigmatism residue and a tendency of undercorrection9. Femtosecond laser fabrication of corneal flaps helps to improve the predictability, accuracy, and stability, and makes laser-assisted in situ keratomileusis (LASIK) surgery safer and more accurate. Femtosecond laser-assisted in situ keratomileusis (FS-LAISK) is potentially used to correct high myopia in the presbyopia age patients11,12. With the development and clinical application of ICL V4c, the misgivings regarding ICL implantation-related acceleration of cataract formation have been further reduced or even eliminated13. A previous study showed that it is safe and effective to correct ametropia in myopic patients aged 40 and above10.
However, the long-term comparison between ICL V4c and FS-LASIK were frequently neglected in the presbyopia age patients. Therefore, this study aimed to compare the long-term characteristics of visual quality and contrast sensitivity in these patients, thus providing the basis for their clinical application for myopia correction in the presbyopia age patients.
Patients and methods
Subjects
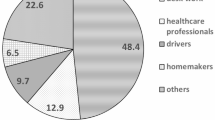
This observational consecutive case series study was conducted at the Eye and Ear, Nose, Throat Hospital of Fudan University, Shanghai, China, between June 2015 and December 2021. 48 eyes of 24 patients with early presbyopia (male/female: 10/14, average age: 45.50 ± 3.82 years, Table 1) were enrolled and recieved binocular FS-LASIK (24 eyes of 12 patients) or ICL V4c implantation (24 eyes of 12 patients) for myopia correction. This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Eye and ENT Hospital of Fudan University (approval number: 2013015). Written informed consent was obtained from all patients before performing all procedures.
The inclusion criteria were as follows: (1) participants aged over 40 years with transparent lenses; (2) a myopia progression rate of less than 0.5D per year within a two-year period; (3) no use of soft contact lenses for more than two weeks, or rigid gas permeable contact lenses for more than three months; and (4) presbyopic add power greater than + 0.50 D and corrected visual acuity not lower than 20/20 at intermediate and near distances, respectively. The exclusion criteria were: (1) diagnosis or suspicion of keratoconus; (2) history of active eye disease or systemic diseases; and (3) corneal endothelial cell density (ECD) below 2000 cells/mm2 or anterior chamber depth (ACD) below 2.8 mm in the ICL V4c group.
Slit lamp examination and fundus examination were completed after pupillary dilation to check the lens transparency and exclude fundus lesions.
Equipment and measured parameters were: (1) Phoropter (RT-5100, Nidek Technologies, Japan): Spherical equivalent (SE), and corrected-distance VA (CDVA). Card-hole method was used to determine the D-eyes and nD-eyes and Fusion Cross-Cylinder method was used to measure prebyopic add power (ADD) at a 33 cm distance with optimal distance visual acuity correction. (2) Canon Full Auto Tonometer TX-F (Canon, Inc., Tokyo, Japan): Intraocular pressure. (3) Pentacam HR (Oculus Optikgerate Wetzlar, Wetzlar, Germany): Corneal thickness, anterior chamber volume, ACD, anterior chamber angle, and white-to-white. (4) SP-2000P (Topcon Corporation, Kyoto, Japan): ECD. (5) IOL Master 700 (Carl Zeiss AG, Germany): white-to-white. (6) IOL Master 500 (Carl Zeiss AG, Germany): axial length. (7) I.Profiler (Zeiss AG, Germany): corneal aberrations within the 5.00 mm radius of the pupil centre. (8) Adaptive Sensory Technology (AST, American): Area Under Line of Contrast Sensitivity Function (AULCSF), CSF Acuity, and contrast sensitivity (CS) under 1.0, 1.5, 3.0, 6.0, 12.0 and 18.0 cpd. The detailed principle and method have been reported previously.14,15.
Monovision
The ICL size was determined using the online calculation software provided by STAAR Surgical (http://en.informer.com/icl-power-calculation-software/, Version 3.0). Subsequently, adjustments were made based on the anterior chamber depth (ACD), angle to angle distances, and white-to-white (WTW) measurements obtained from Pentacam and IOL master devices. The targeted spherical equivalent (SE) ranged from − 0.50 to 0.25 D for patients with D-eyes in both the ICL V4c and FS-LASIK groups, while for patients with nD-eyes, it ranged from − 1.75 to − 0.50 D and − 2.25 to − 0.50 D in the two respective groups accordingly. These target values were personally determined according to their preoperative ADD.
We select a presbypic add of 0.50D as a cut off value to test and ask the patient whether to choose the monovision design in the refraction surgery for myopia correction. When the residual myopic diopters on trial was subjectively accepted by patients and it showed superiority in binocular near-to-far distances, the monovision design was selected.Excessive addition for the nD-eyes was not planned in this study because high monovision-induced anisometropia might be correlated with clinical feature like binocular imbalance. 16.
Surgeries
One experienced surgeon (XZ) performed all surgeries. In FS-LASIK surgery, flap was created in 7.5 mm diameter and 100 µm thickness with standard 90° hinges and 90° side cut angles using a 500 kHz VisuMax femtosecond laser system with a pulse energy of 130 nJ (Carl Zeiss Meditec, Jena, Germany), and stroma was ablated using a MEL 90 excimer laser with a pulse energy of 185 nJ (Carl Zeiss Meditec). The planned optic zone of 6.35 ± 0.25 mm (range 6.10–6.70). After FS-LASIK, a soft contact lens was worn and removed at 1 day postoperatively. The detailed steps are described in a previous study17. In ICL V4c implantation surgeries, after topical anaesthesia, a viscoelastic agent was injected in the anterior chamber followed with implantation of ICL V4c through the lateral corneal incision. Thereafter, the manipulator was used for ICL adjustment, and a balanced salt solution was used to replace the viscoelastic agent. Postoperatively, antibiotic and steroid eye drops were administered. The detailed steps are described in a previous study18.
Follow-up
We conducted a 4.5-year follow-up with the period ranging from 45 to 75 months and an average of 54.00 ± 6.77 months. The relevant parameters were assessed at 1 month postoperatively (ECD at 3 months postoperatively) and the final follow-up visit. Subjective satisfaction regarding visual acuity at near and far distances was recorded before surgery, 3-month after surgery, and at the last follow-up visit using a scoring system ranging from 1 to 5: (1) very dissatisfied; (2) dissatisfied; (3) satisfactory; (4) highly satisfactory; and (5) excellent.
Statistical analysis
The results are expressed as mean ± standard deviation. All statistical analyses were performed using the Statistical Package for the Social Sciences software version 25.0. (SPSS, Inc., Chicago, IL, USA). Definitions: safety index (SI) = postoperative CDVA/preoperative CDVA, efficacy index (EI) = the postoperative UDVA/preoperative CDVA. Kolmogorov–Smirnov test was used for Normality check. We used repeated-ANOVA (Analysis of Variance) to compare the pre- and post-treatment normally distributed data between D- and nD-eyes. One-way ANOVA was used to compare normally distributed data measured only at the last follow-up between the D- and nD-eyes, such as aberration and qCSF test results. Wilcoxon signed-rank test was used for non-normally distributed data. Statistical significance was set at p < 0.05.
Results
Safety
All surgeries were uneventful, and no cataract or retinal detachment was observed in the follow-up. The safety indices of the ICL V4c group at 1 month and 54 months postoperatively were 1.27 ± 0.22 and 1.17 ± 0.30 (p > 0.05), respectively. The corresponding values of the FS-LASIK group were 1.01 ± 0.07 and 0.98 ± 0.20 (p > 0.05), respectively. (p < 0.001 between groups at all time points) Tables 2 and 3 provide the visual and biometric parameters of the D-eyes or nD-eyes between two groups, respectively. Figures 1 and 2 show the CDVA and UDVA (Figs. 1A–C, 2A–C) outcomes of the two groups respectively.
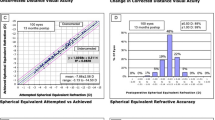
Clinical outcomes of 24 eyes (12 dominant eyes and 12 nondominant eyes) with myopia at the last follow-up after implantable collamer lens (ICL V4c) implantation. (A) Postoperative uncorrected distance visual acuity (UDVA) vs. preoperative corrected distance visual acuity (CDVA); (B) Difference between postoperative UDVA and preoperative CDVA; (C) Change in CDVA; (D) Attempted spherical equivalent refraction change versus the achieved spherical equivalent refraction change; (E) Distribution of postoperative spherical equivalent refraction accuracy; (F) Stability of spherical equivalent refraction up to 54 months. D, diopters; Postop, postoperative; Preop, preoperative; mon, month(s).
Clinical outcomes of 24 eyes (12 dominant eyes and 12 nondominant eyes) with myopia at the last follow-up after femtosecond laser-assisted in situ keratomileusis (FS-LASIK). (A) Postoperative uncorrected distance visual acuity (UDVA) versus preoperative corrected distance visual acuity (CDVA); (B) Difference between postoperative UDVA and preoperative CDVA; (C) Change in CDVA; (D) Attempted spherical equivalent refraction change versus the achieved spherical equivalent refraction change; (E) Distribution of postoperative spherical equivalent refraction accuracy; (F) Stability of spherical equivalent refraction up to 54 months. D, diopters; Postop, postoperative; Preop, preoperative; mon, month(s).
In the ICL V4c group, the preoperative, 3-months, and 54-months postoperative ECD were 3109.41 ± 126.92 cell/mm2, 2767.77 ± 61.1 cell/mm2 (vs. preoperative, p = 0.067), and 2571.36 ± 62.02 cell/mm2 (vs. preoperative, p = 0.016 and vs. 3-mon postoperative, p = 0.026), respectively.
Efficacy
The efficacy indices of the ICL V4c group and FS-LASIK group were not significant between 1 and 54 months postoperatively (1.12 ± 0.25 and 0.79 ± 0. 07 for ICL V4c group, and 0.79 ± 0.06 and 0.52 ± 0.07 for FS-LASIK group, respectively). The efficacy indices in the ICL V4c group were significantly higher than that of the FS-LASIK group at all time points with all p < 0.01.
Predictability
There was a significant linear correlation in the two groups between the achieved SE and the attempted value (p < 0.001). (Figs. 1D, 2D) At the last follow-up, the SE in 66.67% and 58.33% of the eyes was within ± 0.50 D of the target value and that in 95.83% and 83.33% of the eyes was within ± 1.00 D of the target value in ICL V4c group (Fig. 1E) and FS-LASIK group (Fig. 2E), respectively.
Stability
Spherical equivalent in the ICL V4c group were − 11.80 ± 3.36 D, − 0.28 ± 0.69 D, and − 0.80 ± 0.59 D preoperatively, 1 month, and 54 months postoperatively, respectively. (Fig. 1F) The corresponding figures for the FS-LASIK group were − 8.13 ± 3.78 D, − 0.84 ± 1.05 D, and − 1.43 ± 1.14 D, respectively. (Fig. 2F) The change of SE in two groups were not significantly different between two follow-up time points (− 0.52 ± 0.18 D vs. − 0.59 ± 0.18 D, p = 0.76).
Monovision
The preoperative and 54 months postoperative ADD values of the two groups are shown in Table 2. The progression of presbyopia in ADD was significant in the ICL V4c and FS-LASIK groups (0.69 ± 0.60 D vs. 0.48 ± 0.41 D), and the values were equivalent to 0.14 ± 0.13 D per year and 0.10 ± 0.09 D per year (p = 0.248), respectively. Figures 3A and 4A present the uncorrected visual acuity at near to far distances of two groups at 54 months after ICL V4c implantation, respectively. D-eyes shower advantage in VA at 5.0 m distance (75.00% and 75.00% eyes with 20/32 or better in Snellen lines in two groups, respectively). (Figs. 3B, 4B) nD-eyes shower advantage in VA at 0.4 m distance (100% and 91.67% eyes with 20/32 or better in Snellen lines in two groups, respectively). (Figs. 3C, 4C) Binocular visual acuity in 100%, 91.67%, and 75.00% eyes of ICL V4c group was 20/25 or better in Snellen lines, the corresponding eyes in FS-LASIK group was 83.33%, 83.33%, and 66.67%. (Figs. 3D, 4D).
Uncorrected Visual Acuity at near to far distances at 54 months after implantable collamer lens (ICL V4c) implantation. (A) Last follow-up UDVA (logMAR) of Dominant eyes, nonDominant eyes and Binocular. (B) Last follow-up UDVA (Snellen) of the Dominant eyes. (C) Last follow-up UDVA (Snellen) of the Nondominant eyes. (D) Last follow-up Binocular UDVA (Snellen).
Uncorrected Visual Acuity at near to far distances at 54 months after femtosecond laser-assisted in situ keratomileusis (FS-LASIK). (A) Last follow-up UDVA (logMAR) of Dominant eyes, nonDominant eyes and Binocular. (B) Last follow-up UDVA (Snellen) of the Dominant eyes. (C) Last follow-up UDVA (Snellen) of the Nondominant eyes. (D) Last follow-up Binocular UDVA (Snellen).
Subjective satisfaction
Supplementary Fig. 1 describes the subjective satisfaction with distance and near VA preoperatively, 3 months postoperatively, and at the last follow-up. In the ICL V4c group, the satisfaction rates (scores 4 or 5) of near VA were 33.3%, 91.67%, and 66.67% respectively, and that of distance VA at three follow-up time points were 0%, 83.33%, and 80.00%, respectively. In the FS-LASIK group, the satisfaction rates of near VA were 33.3%, 83.33%, and 66.67% respectively, and that of distance VA at three follow-up time points were 0%, 83.33%, and 50.00%, respectively.
Aberrations
There was no significant difference in wavefront aberrations between the dominant and non-dominant eyes in the two groups at the last follow-up (Supplementary Fig. 2). There was no significant difference between the two groups in HOAs; however, the FS-LASIK group showed significantly higher coma and spherical aberration, and significantly lower trefoil compared with the ICL V4c group.
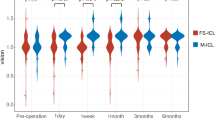
qCSF
Table 4 provides the CS at different spatial frequencies at the last follow-up. There was a significant difference between the dominant and non-dominant eyes in CS at 1.0–3.0 cpd AULCSF and CSF Acuity in the FS-LASIK group. (Fig. 5A,B). There was no significant difference between the dominant and non-dominant eyes in ICL V4c group or binocular comparison of the two groups (Fig. 5C).
Discussion
This study provides further support for 4.5 years long-term safety of ICL V4c implantation and FS-LASIK for myopia correction in the presbyopia age patients. Monovision surgery using ICL V4c or FS-LASIK provides long-term safety and good binocular vision in myopic presbyopes.
Previous studies comparing FS-LASIK and SMILE have provided evidence regarding the safety and efficacy of both procedures in both short-term and long-term follow-up assessments17,19,20,21. The safety index was found to be 1.17 for ICL V4c implantation and 0.98 for FS-LASIK, which is comparable to the safety index of 1.22 observed in a previous study involving patients over 40 years who underwent ICL V4c implantation during a 43-month follow-up period22. In cases where myopia exceeds -11.00D, FS-LASIK demonstrates feasibility as well as comparable safety and efficacy with ICL V4c, while SMILE may have limitations23,24,25. Therefore, this study opted for FS-LASIK instead of SMILE when comparing it with ICL V4c implantation due to the anticipation of including more subjects with high or ultra-high myopia in the ICL V4c groups. In the clinical research center of this study, ICL V4c implantation are more expensive than FS-LASIK, in that case, patients might choose FS-LASIK prior to ICL V4c implantation when they meet the indication of the two procedures. Meanwhile, that was the reason of the inadequate match between two groups, a part of patients who choose ICL V4c implantation were out of the indication of FS-LASIK. The ICL V4c demonstrated a higher SI at the last follow-up, which was consistent with the enhanced object image effect achieved by ICL compared to LASIK26. There was no significant difference in ECD between the preoperative and 3-month postoperative levels, indicating an annual decrease rate of 1.75% in the ICL V4c group. Previous studies have reported a decrease rate of 0.6% per year in healthy adults27 and 0.93–4% per year in long-term follow-up after ICL implantation28,29. The relatively higher ECD decrease rates observed might be associated with older age. At the last follow-up, all subjects had an ECD greater than 2000 cells/mm2, confirming the safety of both ICL V4c implantation and FS-LASIK for myopia correction in this age group.Efficacy indices data are biased due to monovision design in this study, because the intentionally undercorrected non-dominant eyes have lower efficacy indices. Our previous findings suggested that binocular visual acuity at near-to-far distances might be better than simple efficacy indices in the assessment of monovision design.
In predictability, Our results were similar to a previous study with 96.67% of eyes within ± 1.00D of the target value in patients over 40 years old underwent ICL V4c implantation28. Progressed myopia with − 0.52 D and − 0.59 D in two groups was acceptable in 54-months follow-up8,30. Patients were counselled about the possibility of myopia progression especially in patient over − 10.00 D before surgery in this study. The results be a reference to clinical practice and preoperative counsel.
The ADD progression rates were similar between ICL V4c group (0.10 D per year), FS-LASIK group (0.14 D per year), and a previous study (0.17 D per year)22. Monovision surgery using ICL V4c or FS-LASIK provides similarly good binocular VA at near-to-far distance. These results and the subjective satisfaction results agree with previous findings (81.25% for near VA and 87.50% for distance VA)22. The decreased satisfaction rate of near VA might be explained with the relatively higher ADD progression in the ICL V4c group (0.69 D vs. 0.48D), while that of distance VA might be correlated to higher preoperative ADD in the FS-LASIK group (1.33 D vs. 0.71 D), as more refraction sphere was reserved in nD-eyes in this group. Besides, the short-term satisfaction included partial psychological factors like immediately improved visual experience, and this part of the subjective satisfaction may decrease in the long-term follow-up.
The trefoil aberration was significant higher in ICL V4c group than FS-LASIK group. There are several possible explanations: firstly, the centre of ICL might deviate from the visual axis31; seconds, higher trefoil aberration might be attributed to the corneal incision31; third, the pupil dilation under scotopic environment in aberration measurement, as the optical zone might be relatively smaller in ICL V4c groups32,33. Meanwhile, FS-LASIK might introduce coma and spherical aberration due to eccentric ablation34.
The novel qCSF test was firstly applied for CSF evaluation between D-eye and nD-eye in monovision surgery utilizing ICL V4c implantation and FS-LASIK. A previous study reported that age instead of refraction error was significant correlated with qCSF readings35,36. Previous study reported similar contrast sensitivity outcomes of the 3 methods—PRK, FS-LASIK, and SMILE—in patients with mild and moderate myopia37. While in the high myopia patients in this study, compared with the FS-LASIK group, the ICL V4c group showed high readings of CS in nD-eyes in low spatial frequency, which might be attributed by the retinal magnification after ICL implantation26.
This study had several limitations: first, it was a single-centre study with relatively small size of participants. Multicentre studies with larger sample size are needed to provide high-quality clinical evidence; second, the study did not include the preoperative results of aberration and qCSF test due to the upgrading of equipment. More reliable measurements are suggested on the long-term follow-up preoperative and postoperative test for aberrations and contrast sensitivity function data; third, inadequate match between the ICL V4c group and the FS-LASIK group, which was limited by the differences of characteristics and indications of the two surgeries. FS-LAISK is potentially used to correct high myopia, though ICL V4c shows better performance in superhigh myopia correction. A better-matched pair study would provide more solid evidence; fourth, there is no clear breakdown of the changes and trends observed at intermediate time points. The enrolled patients got followed-up at different time points, making it difficult to analysis and get a solid conclusion, a more rigorous plan in the follow- up will help in the trends observation.
In conclusion, Monovision surgery using ICL V4c or FS-LASIK are practicable for correction of myopia in patients in the presbyopia age group, with long-term efficacy and good subjective satisfaction at near and far distances.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due funding requirement but are available from the corresponding author on reasonable request.
References
Fricke, T. R. et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia. Ophthalmology 125(10), 1492–1499 (2018).
Lindstrom, R. L. et al. Corneal inlays for presbyopia correction. Curr. Opin. Ophthalmol. 24(4), 281–287 (2013).
Binder, P. S. Intracorneal inlays for the correction of presbyopia. Eye Contact Lens Sci. Clin. Pract. 43(5), 267–275 (2017).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016).
Jain, S., Arora, I. & Azar, D. T. Success of monovision in presbyopes: Review of the literature and potential applications to refractive surgery. Surv. Ophthalmol. 40(6), 491–499 (1996).
Kollbaum, P. S. & Bradley, A. Correction of presbyopia: Old problems with old (and new) solutions. Clin. Exp. Optom. 103(1), 21–30 (2020).
Lafosse, E. et al. Presbyopia and the aging eye: Existing refractive approaches and their potential impact on dry eye signs and symptoms. Cont. Lens. Anterior Eye. 43(2), 103–114 (2020).
Luo, W. et al. Four-year visual outcomes and optical quality of SMILE and implantable collamer lens V4c (EVO-ICL) implantation for high myopia: A retrospective study. BMC Ophthalmol. 23(1), 341 (2023).
Primavera, L. et al. Influence of age on small incision lenticule extraction outcomes. Br. J. Ophthalmol. 106, 341–348 (2020).
Tañá-Rivero, P. et al. Posterior-chamber phakic intraocular lens implantation in patients over 40 years of age. J. Ophthalmol. 2020, 7457902 (2020).
Fu, Y. et al. Clinical outcomes after small-incision lenticule extraction versus femtosecond laser-assisted LASIK for high myopia: A meta-analysis. PLoS One 16(2), e0242059 (2021).
Zhao, Y. et al. Comparison of posterior corneal elevation after SMILE and FS-LASIK in correcting myopia over—9.0 diopters. Ann. Transl. Med. 9(5), 373 (2021).
Choi, J. H. et al. Ten-year clinical outcomes after implantation of a posterior chamber phakic intraocular lens for myopia. J. Cataract Refract. Surg. 45(11), 1555–1561 (2019).
Vilaseca, M. et al. Intra- and intersession repeatability of a double-pass instrument. Optom. Vis. Sci. 87(9), 675–681 (2010).
Ieong, A. et al. Quality of life in high myopia before and after implantable collamer lens implantation. Ophthalmology 117(12), 2295–2300 (2010).
Ye, Y. et al. Binocular imbalance in patients after implantable collamer lens V4c implantation or femtosecond laser-assisted in situ keratomileusis for myopia with presbyopia. Front. Neurosci. 17, 1204792 (2023).
Han, T. et al. Three-year outcomes of small incision lenticule extraction (SMILE) and femtosecond laser-assisted laser in situ keratomileusis (FS-LASIK) for myopia and myopic astigmatism. Br. J. Ophthalmol. 103(4), 565–568 (2019).
Chen, X. et al. Comparison of early changes in and factors affecting vault following posterior chamber phakic Implantable Collamer Lens implantation without and with a central hole (ICL V4 and ICL V4c). BMC Ophthalmol. 16(1), 161 (2016).
Liu, T. et al. Visual and optical quality outcomes of SMILE and FS-LASIK for myopia in the very early phase after surgery. BMC Ophthalmol. 19(1), 88 (2019).
Li, M. et al. Five-year results of small incision lenticule extraction (SMILE) and femtosecond laserLASIK (FS-LASIK) for myopia. Acta Ophthalmol. 97(3), e373–e380 (2019).
Zhao, P. et al. Comparison of correcting myopia and astigmatism with SMILE or FS-LASIK and postoperative higher-order aberrations. Int. J. Ophthalmol. 14(4), 523–528 (2021).
Ye, Y. et al. Long-term follow-up for monovision surgery by Implantable Collamer Lens V4c implantation for myopia correction in early presbyopia. Graefes Arch. Clin. Exp. Ophthalmol. 260(8), 2763–2771 (2022).
Zhou, X. et al. Two-year observation of posterior corneal elevations after small incision lenticule extraction (SMILE) for myopia higher than −10 dioptres. Br. J. Ophthalmol. 104(1), 142–148 (2019).
Niu, L. et al. One-year visual outcomes and optical quality of femtosecond laser small incision lenticule extraction and visian implantable collamer lens (ICL V4c) implantation for high myopia. Acta Ophthalmol. 98(6), e662–e667 (2020).
Han, T. et al. Refractive outcomes comparing small-incision lenticule extraction and femtosecond laser–assisted laser in situ keratomileusis for high myopia. J. Cataract Refract. Surg. 46(3), 419–427 (2020).
Kamiya, K. et al. Effects of myopic correction by replacement of spectacles, laser in situ keratomileusis, and phakic intraocular lens implantation on modulation transfer function and retinal magnification. Nippon Ganka Gakkai Zasshi 112, 519–524 (2008).
Bourne, W., Nelson, L. R. & Hodge, D. O. Central corneal endothelial cell changes over a ten-year period. Invest. Ophthalmol. Vis. Sci. 38, 779–782 (1997).
Ye, Y. et al. Long-term evaluation of anterior lens density after implantable collamer lens V4c implantation in patients with myopia over 40 years old. Br. J. Ophthalmol. 106(11), 1508–1513 (2022).
Yang, W. et al. Changes in anterior lens density after Implantable Collamer Lens V4c implantation: A 4-year prospective observational study. Acta Ophthalmol. 99(3), 326–333 (2021).
Chen, X. et al. Effect of long-term rotation on astigmatism following EVO-toric intraocular collamer lens implantation. Front. Med. (Lausanne). 10, 1194006 (2023).
Wan, T. et al. Comparative study of implantable collamer lens implantation in treating four degrees of myopia: Six-month observation of visual results, higher-order aberrations, and amplitude of accommodation. Curr. Eye Res. 45(7), 839–846 (2020).
Kamiya, K. et al. Visual performance after posterior chamber phakic intraocular lens implantation and wavefront-guided laser in situ keratomileusis for low to moderate myopia. Am. J. Ophthalmol. 153(6), 1178–1186 (2012).
Pérez-Vives, C. et al. Optical quality of hyperopic and myopic phakic intraocular lenses. Indian J Ophthalmol. 62(4), 437–441 (2014).
Miao, H. et al. Visual outcomes and optical quality after femtosecond laser small incision lenticule extraction: An 18-month prospective study. J. Refract,. Surg. 31(11), 726–731 (2015).
Ye, Y. et al. A novel quick contrast sensitivity function test in Chinese adults with myopia and its related parameters. Graefe’s Arch. Clin. Exp. Ophthalmol. 261(7), 2071–2080 (2023).
Li, Z. et al. Effect of age and refractive error on quick contrast sensitivity function in Chinese adults: a pilot study. Eye (Lond). 35(3), 966–972 (2021).
Janiszewska-Bil, D. et al. Comparison of vision correction and corneal thickness at 180-day follow-up after femtosecond laser-assisted in-situ keratomileusis (FS-LASIK), photorefractive keratectomy (PRK), and small incision lenticule extraction (SMILE): A study from a single center in Poland of 120 patients with myopia. Med. Sci. Monit. 16(29), e939099. https://doi.org/10.12659/MSM.939099 (2023).
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
National Key Research and Development Program of China (2024YFC2510805); Key Project of the Regional Innovation and Development Joint Fund of the National Natural Science Foundation of China(U24A20708); Shanghai Engineering Research Center of Laser and Autostereoscopic 3D for Vision Care (20DZ2255000); National Natural Science Foundation of China (Grant No. 82271119, 82471116); Shanghai Rising-Star Program (23QA1401000); Healthy Young Talents Project of Shanghai Municipal Health Commission (2022YQ015); Shanghai Oriental Talents-Technology Platform Program (QNKJ2024055).
Author information
Authors and Affiliations
Contributions
Study concept and design (YY, YX, ZZ, JZ, XZ); data collection (YY, YX, ZZ, FL, LN, WS, XW, JZ); data analysis and interpretation (YY, FL); drafting of the manuscript (YY, FL, JZ, XZ); critical revision of the manuscript (JZ, XZ); supervision (XZ). All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of Ethics
This study followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Eye and ENT Hospital of Fudan University (approval number: 2013015). Informed consent was obtained from all participants.
Consent for publication
Written informed consent was obtained from the patients for the publication of this paper. Patient names and the eyes/facial region of study participants is not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ye, Y., Xian, Y., Liu, F. et al. Comparison of monovision surgery using ICL V4c or femtosecond laser LASIK for myopia correction in the presbyopia age patients. Sci Rep 15, 7629 (2025). https://doi.org/10.1038/s41598-025-88588-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88588-y