Abstract
To evaluate the clinical efficacy and safety of transvaginal natural orifice transluminal endoscopic surgery (vNOTES) for treating benign ovarian tumors in obese patients. A retrospective analysis was conducted on the clinical data of 35 obese patients who underwent vNOTES for benign ovarian tumor resection and 41 obese patients who underwent multi-port laparoscopic surgery (MPLS) during the same period from January 2021 to June 2024 at Qinghai Red Cross Hospital. Key parameters such as operative time, intraoperative blood loss, intraoperative and postoperative complications, hospitalization duration, postoperative anal exhaust time, postoperative visual analog scale (VAS) score, and SF-36 score were analyzed. No statistical differences were observed between the two groups regarding baseline characteristics such as age, body mass index (BMI), tumor diameter, parity, and history of pelvic surgery. The vNOTES group exhibited shorter operative times compared to the MPLS group, with no significant differences in tumor pathology, intraoperative blood loss, or tumor rupture rates. Postoperatively, the vNOTES group had shorter hospital stays, fewer postoperative complications, lower 24-hour postoperative VAS scores, and higher three-month postoperative SF-36 scores compared to the MPLS group. No differences were found between the groups concerning anal exhaust time, sexual satisfaction rate, or 24-hour postoperative VAS scores. vNOTES is a safe and feasible surgical method for treating benign ovarian tumors in obese patients, offering advantages such as no abdominal incisions and quicker postoperative recovery.
Similar content being viewed by others
Introduction
With the rapid development of minimally invasive surgery in recent years, the postoperative quality of life and rapid recovery of patients have become significant concerns for surgeons, besides ensuring surgical success1. In gynecology, vNOTES combines laparoscopy with traditional vaginal surgery, offering advantages such as accelerated postoperative recovery and the absence of abdominal incisions for improved aesthetic outcomes2. In developed countries, over 20% of adult women suffer from obesity3,4,5. When these patients require surgical intervention for gynecological conditions, the increased thickness of the abdominal wall in obese individuals can complicate traditional open or laparoscopic surgeries, raising the risk of surgical difficulties and complications. Therefore, vNOTES may offer advantages for obese patients. The clinical efficacy and safety of vNOTES for treating benign ovarian tumors in obese patients remain unclear. This study aims to evaluate the feasibility and safety of vNOTES by comparing it with MPLS in the treatment of benign ovarian tumors in obese patients, assessing preoperative, intraoperative, and postoperative outcomes to provide guidance for choosing surgical approaches for this patient population.
Materials and methods
General data
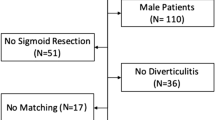
A retrospective analysis was conducted on 35 obese patients who underwent vNOTES for benign ovarian tumor resection at Qinghai Red Cross Hospital from January 2021 to June 2024, and 41 obese patients who received multi-port laparoscopic ovarian tumor resection during the same period. Clinical data were collected and compared to assess the outcomes of both surgical techniques. This retrospective study was conducted at Qinghai Red Cross Hospital and it adhered to the principles outlined in the Declaration of Helsinki. The study was approved by the ethics committee of Qinghai Red Cross Hospital (LW-2024-136). Individual consent was obtained from all patients in this retrospective analysis.
The inclusion criteria were: (1)BMI ≥ 30 kg/m2. (2)Being between 18 and 50 years old. (3)Having a preoperative risk of malignancy index (RMI) indicating a high likelihood of a benign condition. (4)Having regular postoperative follow-up. (5)Providing informed consent by agreeing to participate in the study and signing a consent form. The exclusion criteria were: (1)Patients identifying as asexual. (2)Patients with vaginal stenosis. (3)Patients with vaginal infections. (4)Patients with a history of pelvic surgery. (5)Patients with ovarian cysts larger than 10 cm. (6)Suspected cases of pelvic adhesion. (7)Suspected cases of malignancy. (8)Pregnant Patients.
Surgical techniques
All patients underwent rapid pathologic diagnosis during surgery and all pathological diagnoses were benign. whether or not to place a drain postoperatively was based on selective intraoperative placement, such as the need to place a drain for large surgical wounds and heavy bleeding. In addition, all patients followed the discharge criteria: resumption of a semi-liquid diet; cessation of intravenous rehydration; good pain relief with oral analgesic medication; good wound healing with no signs of infection; and good organ functional status on review and free movement.
MPLS
Under general anesthesia, we selected puncture points at the umbilical region, McBurney’s point, the reverse McBurney’s point, and the midpoint between the reverse McBurney’s point and the umbilicus. Trocar lapascopy and operative instruments were inserted at these sites. Through careful laparoscopic examination of the pelvic cavity, we identified the affected ovary and observed the cyst’s location, diameter, and mobility. The ovarian cortex of the affected ovary was dissected, and the cyst was separated from the normal ovarian tissue, taking care to avoid cyst rupture. The cyst wall was gradually peeled away and placed in a specimen retrieval bag for extraction. The ovarian incision was sutured with absorbable stitches, followed by rapid pathological examination. The pelvic and abdominal cavities were irrigated with saline, a drainage tube was placed, and the puncture sites were sutured.
vNOTES
The surgery was performed by two experienced obstetricians and gynecologists with specialized training in vNOTES and one assistant surgeon from Qinghai Red Cross Hospital. Under general anesthesia, the cervix and posterior vaginal fornix were exposed, and a vasopressin solution (0.12 U/mL) was injected at the junction of the cervical and posterior vaginal wall mucosa to separate the vaginal rectal space. A 2 cm arcuate incision was made at the top of the posterior fornix, the rectum was bluntly separated, and the peritoneum at the rectouterine pouch was opened to access the pelvic cavity. A port was installed, and pneumo-peritoneum was established with an intraoperative pressure maintained at 8–10 mmHg. The remainder of the procedure followed MPLS protocols. The resected specimen was removed transvaginally, and the peritoneum and vaginal wall were sutured with absorbable stitches. An iodine-soaked gauze was placed inside the vagina and removed after 24 h. (see Fig. 1).
Observation indicators
We compared preoperative general conditions (age, body mass index (BMI), tumor diameter, number of deliveries, history of pelvic surgery) and intraoperative conditions (surgical time, tumor pathology, intraoperative blood loss, number of tumor ruptures) between the two groups. Postoperative conditions such as hospital stay duration, incidence of postoperative complications, VAS score at 24 h post-operation, SF-36 score at 3 months post-operation, first flatus time, and sexual satisfaction rate were also assessed.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics (Version 26.0, URL link: https://www.ibm.com/spss). Continuous variables were tested for normality, expressed as mean ± standard deviation if normally distributed, and compared using the t-test. Categorical variables were expressed as n (%) and compared using the χ2 test. A P-value < 0.05 was considered statistically significant.
Results
Preoperative general indicators comparison
No statistical differences were observed between the vNOTES and MPLS groups in terms of age, BMI, tumor diameter, number of deliveries, or history of pelvic surgery (P > 0.05) (see Table 1).
Intraoperative conditions comparison
All surgeries were successfully completed without injury to adjacent organs and all pathological diagnoses were benign. The vNOTES group had significantly shorter operative times compared to the MPLS group (P < 0.05). No significant differences were observed in tumor pathology, intraoperative blood loss, or number of tumor ruptures between the two groups (P > 0.05) (see Table 2).
Postoperative conditions comparison
The vNOTES group experienced shorter hospital stays, fewer postoperative complications, lower VAS scores at 48 h post-operation, and higher SF-36 scores at 3 months post-operation compared to the MPLS group (P < 0.05). However, there were no significant differences between the groups in terms of time to first flatus, sexual satisfaction rate, and VAS scores at 24 h post-operation (P > 0.05). Patients in the MPLS group had surgical incision infections on postoperative days 4 and 5, subcutaneous emphysema on postoperative day 1, and lower-extremity venous thrombosis on postoperative day 5, and patients in the vNOTES group had surgical incision infections on postoperative day 4 (see Table 3).
Discussion
With the rapid advancement of gynecological minimally invasive techniques, there is an increasing focus on treatment efficacy, safety, postoperative recovery speed, quality of life, and cosmetic outcomes6,7. The unique natural cavity of the vagina has facilitated the rapid development of vNOTES in gynecologic surgery8. vNOTES combines the strengths of single-port laparoscopy and traditional vaginal surgery, offering superior clinical outcomes. Therefore, it is especially important to train a gynecologist with vNOTES. Results of a study on the learning curve of vNOTES showed that for a team skilled in minimally invasive surgery, 5 cases are required to rich competence and 25 to rich proficiency in vNOTES hysterectomy, confirming that vNOTES hysterectomy is a feasible and reproducible approach for benign indications with a short learning curve and low rate of perioperative complications9.
The results indicate that vNOTES significantly reduces operative time in obese patients. Traditional laparoscopic surgery is more challenging in obese patients, particularly during puncture and insufflation10,11. In contrast, vNOTES eliminates the need for abdominal wall incisions, thus simplifying these steps and reducing operative time12. Shorter operative time not only decreases anesthesia duration but may also lower the risk of intraoperative complications13. Obese patients often have additional health issues such as hypertension and diabetes, which increase anesthesia risks14. vNOTES reduces both anesthesia time and medication usage, thereby mitigating anesthesia-related risks15. A randomized controlled trial involving 114 patients showed that the operative time for the vNOTES group (48.33 ± 33.12 min) was significantly shorter compared to the MLPS group (72.23 ± 43.63 min), with fewer intraoperative complications, suggesting that vNOTES is a promising method for ovarian cystectomy16.
The study further found that postoperative complications and hospital stay were significantly lower in the vNOTES group compared to the MLPS group, although intraoperative blood loss did not differ statistically between the two groups. Due to the thicker abdominal wall in obese patients, traditional laparoscopic surgery requires multiple abdominal wall incisions, increasing the risk of postoperative wound infection, hernias, and poor wound healing17,18,19. By accessing the abdominal cavity via the vagina, vNOTES avoids abdominal wall incisions, significantly reducing related complications and accelerating postoperative recovery, which is particularly crucial for obese patients20,21,22. Research has shown that vNOTES leads to a notable reduction in hospital stay and faster postoperative recovery, benefiting both patient rehabilitation and healthcare resource utilization. Additionally, vNOTES has been associated with fewer postoperative wound infections and hernias, providing robust evidence for its safety22. However, it is important to note that while vNOTES demonstrates a lower complication rate in this study, it does not eliminate all risks23. The use of natural orifices for abdominal access may increase the risk of intraoperative infection, particularly if procedures are not performed correctly or preoperative disinfection is inadequate24. Future research should focus on further reducing potential risks associated with vNOTES to ensure its safety in clinical practice.
The study also found that vNOTES resulted in significantly lower VAS scores at 48 h postoperative and higher SF-36 scores at 3 months postoperative. The absence of abdominal wall incisions in vNOTES contributes to significantly reduced postoperative pain25. Obese patients are particularly sensitive to postoperative pain, and effective pain management is crucial for recovery26. Reduced postoperative pain facilitates early mobilization and rapid recovery, allowing patients to return to normal life and social activities sooner, thereby improving postoperative quality of life27. Studies have shown that vNOTES results in significantly lower VAS scores compared to MLPS, indicating that the smaller surgical wounds and faster recovery associated with vNOTES reduce postoperative pain and offer advantages in enhancing long-term quality of life28. Although no significant differences were observed in sexual satisfaction between the two groups, and long-term pregnancy and delivery outcomes were not statistically significant due to the short study duration and small sample size, further extensive clinical research is needed to determine these aspects.
In conclusion, the results of this study suggest that vNOTES offers significant advantages in the treatment of benign ovarian tumors in obese patients, including shorter operative and hospital stay times, fewer postoperative complications and pain, and improved quality of life. vNOTES is a safe and effective surgical approach for treating benign ovarian tumors in obese patients. However, given the complexity of the procedure and potential risks, further large-scale, prospective studies are needed to validate its safety and efficacy in diverse patient populations.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Baekelandt, J. Transvaginal natural orifice transluminal endoscopic surgery: a new approach to ovarian cystectomy. Fertil. Steril. 109 (2), 366. https://doi.org/10.1016/j.fertnstert.2017.10.037 (2018).
Terzi, H., Turkay, U., Uzun, N. D. & Salıcı, M. Hysterectomy and salpingo-oophorectomy by transvaginal natural orifice transluminal endoscopic surgery (V-NOTES) assisted by an umbilical camera: case report and new hybrid technique in gynecology. Int. J. Surg. Case Rep. 51, 349–351. https://doi.org/10.1016/j.ijscr.2018.08.053 (2018).
Li, C. B. & Hua, K. Q. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologic surgeries: a systematic review. Asian J. Surg. 43 (1), 44–51. https://doi.org/10.1016/j.asjsur.2019.07.014 (2020).
Badiglian-Filho, L., Fukazawa, E. M., Faloppa, C. & Baiocchi, G. Ovarian sparing cystectomy for borderline serous tumor through vNOTES (vaginal natural orifices transluminal endoscopic surgery). Int. J. Gynecol. Cancer. 30 (8), 1253–1254. https://doi.org/10.1136/ijgc-2020-001513 (2020).
Kaya, C. et al. Conventional laparoscopy or vaginally assisted natural orifice transluminal endoscopic surgery for adnexal pathologies: a paired sample cross-sectional study. J. Invest. Surg. 34 (11), 1185–1190. https://doi.org/10.1080/08941939.2020.1789246 (2021).
Ozceltik, G., Yeniel, A. O., Atay, A. O. & Itil, I. M. Simplified two-step technique for transvaginal natural orifice transluminal endoscopic surgery. Fertil. Steril. 114 (3), 665–666. https://doi.org/10.1016/j.fertnstert.2020.05.002 (2020).
Goldenberg, M., Burke, Y. Z., Matanes, E. & Lowenstein, L. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) for prophylactic bilateral salpingo-oophorectomy. Surg. Oncol. 35, 79–80. https://doi.org/10.1016/j.suronc.2020.07.006 (2020).
Lowenstein, L. et al. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) for omentectomy - a case series. Surg. Oncol. 34, 186–189. https://doi.org/10.1016/j.suronc.2020.04.018 (2020).
Mereu, L. et al. Cumulative sum analysis of learning curve process for vaginal natural orifice transluminal endoscopic surgery hysterectomy. J. Minim. Invasive Gynecol. 30 (7), 582–586 (2023). Epub 2023 Mar 24. PMID: 36966920.
Jung, Y., Rattanaburi, A., Kim, O., Park, J. H. & Lee, K. H. A simple gasless direct suturing technique to achieve ovarian hemostasis during transvaginal natural orifice transluminal endoscopic surgery ovarian cystectomy. J. Laparoendosc Adv. Surg. Tech. A. 31 (9), 1046–1050. https://doi.org/10.1089/lap.2020.0575 (2021).
Mat, E., Kale, A., Yıldız, G., Başol, G. & Gündogdu, E. C. Alternative method for the diagnosis of acid cases of unknown cause: transvaginal natural orifice transluminal endoscopic surgery. J. Obstet. Gynaecol. Res. 47 (2), 645–652. https://doi.org/10.1111/jog.14575 (2021).
Huang, L., Lin, Y. H., Yang, Y., Gong, Z. L. & He, L. Comparative analysis of vaginal natural orifice transluminal endoscopic surgery versus transumbilical laparoendoscopic single-site surgery in ovarian cystectomy. J. Obstet. Gynaecol. Res. 47 (2), 757–764. https://doi.org/10.1111/jog.14603 (2021).
Kita, M., Sumi, G., Butsuhara, Y., Hisamatsu, Y. & Okada, H. Resection of vaginal recurrence of granulosa cell tumor by pneumovaginal endoscopic surgery. Gynecol. Oncol. Rep. 36, 100743. https://doi.org/10.1016/j.gore.2021.100743 (2021).
Brandão, P., Almeida, A. & Ramôa, P. vNOTES for adnexal procedures. J. Obstet. Gynaecol. 41 (7), 1134–1138. https://doi.org/10.1080/01443615.2020.1841124 (2021).
Yassa, M. et al. The comparison of Transvaginal Natural Orifice Transluminal endoscopic surgery and conventional laparoscopy in opportunistic bilateral salpingectomy for permanent female sterilization. J. Minim. Invasive Gynecol. 29 (2), 257–264e1. https://doi.org/10.1016/j.jmig.2021.08.009 (2022).
Netter, A., Niddam, R., Agostini, A. & Crochet, P. Vaginal NOTES approach for risk-reducing salpingo-oophorectomy in BRCA mutation carriers: a video demonstration. J. Gynecol. Obstet. Hum. Reprod. 50 (10), 102212. https://doi.org/10.1016/j.jogoh.2021.102212 (2021).
Li, P. C., Chen, H. & Ding, D. C. Shoulder pain after natural orifice transluminal endoscopic surgery decreased with abdominal compression and pulmonary recruitment maneuver: a retrospective study. Taiwan. J. Obstet. Gynecol. 60 (5), 878–881. https://doi.org/10.1016/j.tjog.2021.07.017 (2021).
Karakaş, S. et al. Comparison of vNOTES technique with conventional laparoscopy in gynecological emergency cases. Minim. Invasive Ther. Allied Technol. 31 (5), 803–809. https://doi.org/10.1080/13645706.2021.2025111 (2022).
Hurni, Y., Romito, F. & Huber, D. Transvaginal natural orifice transluminal endoscopic surgery for surgical staging of early-stage ovarian cancers: a report of two cases. Front. Surg. 9, 833126. https://doi.org/10.3389/fsurg.2022.833126 (2022).
Badiglian-Filho, L., Baiocchi, G. & Baekelandt, J. 10 steps to approach large ovarian masses through vNOTES. Int. J. Gynecol. Cancer 26, ijgc-2022-003421. https://doi.org/10.1136/ijgc-2022-003421 (2022).
Jegaden, M., Debras, E., Pourcelot, A. G., Capmas, P. & Fernandez, H. vNOTES for ovarian drilling: a new minimal invasive technique. J. Minim. Invasive Gynecol. 29 (8), 932–933. https://doi.org/10.1016/j.jmig.2022.06.007 (2022).
Jegaden, M. et al. Innovations in surgery to perform an ovarian drilling. J. Gynecol. Obstet. Hum. Reprod. 52 (1), 102499. https://doi.org/10.1016/j.jogoh.2022.102499 (2023).
Guan, X., Guan, Z., Sunkara, S. & Thigpen, B. Indocyanine Green-Assisted Retrograde Ureterolysis in Robotic Transvaginal NOTES for the Management of Stage IV Endometriosis with Obliterated Cul-de-sac. J. Minim. Invasive Gynecol. 30 (4), 266–267. https://doi.org/10.1016/j.jmig.2023.02.005 (2023).
Chang, C. H. & Ding, D. C. Comparing outcomes of ovarian cystectomy by vaginal natural orifice transluminal endoscopic surgery versus laparoendoscopic single-site surgery: A retrospective cohort study. J. Chin. Med. Assoc. 86 (7), 682–687. https://doi.org/10.1097/JCMA.0000000000000933 (2023).
Xie, A. et al. Transvaginal natural orifice endoscopic surgery for ovarian cystectomy: a more suitable surgical approach for the day-care procedure. Front. Med. (Lausanne) 10, 1164970. https://doi.org/10.3389/fmed.2023.1164970 (2023).
Chen, L. Y. & Ding, D. C. Vaginal natural orifice transluminal endoscopic surgery in a second-trimester pregnant woman with an ovarian teratoma. Gynecol. Minim. Invasive Ther. 12 (2), 116–119. https://doi.org/10.4103/gmit.gmit_107_22 (2023).
Hurni, Y. & Huber, D. Omentectomy for oncological surgical staging by transvaginal natural orifice transluminal endoscopic surgery (vNOTES): a preliminary study. Front. Surg. 10, 1224770. https://doi.org/10.3389/fsurg.2023.1224770 (2023).
Anderson, D., Garcia, K., Fang, W. & Dueñas-Garcia, O. Feasibility of opportunistic salpingectomy at the time of a vNOTES hysterectomy: A retrospective cohort. Int. J. Gynaecol. Obstet. 163 (3), 1026–1027. https://doi.org/10.1002/ijgo.15085 (2023).
Acknowledgements
Thanks for funding from the Basic Research Program of Qinghai Provincial Science and Technology Department and Qinghai Province obstetrics and gynecology disease clinical medical research center.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Qinghai Province obstetrics and gynecology disease clinical medical research center(2024-SF-L03).
Author information
Authors and Affiliations
Contributions
WF: Writing – Original Draft, Data Management. LYQ: Data Management, Writing - Review and Editing. XY: Data Management, Writing – Review & Edit. WDD: Data Management, Writing – Review & Edit. LLL: Investigating, Writing - Censoring and Editing. SYJ: Formal Analysis, Writing – Review and Editing. BX: Formal Analysis, Writing – Review and Editing. MCH: Investigation, Methodology, Project administration, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. WLH: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. BYF: Conceptualization, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The studies involving humans were approved by Qinghai Red Cross Hospital (KY-2024-89). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, F., Liu, Y., Xing, Y. et al. Clinical efficacy and safety study of vNOTES for benign ovarian tumors in obese patients. Sci Rep 15, 4609 (2025). https://doi.org/10.1038/s41598-025-88599-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88599-9