Abstract
Herpes zoster has a well-established increased incidence in older adults, but the relationship between age and acute pain severity remains less clear. This retrospective study aimed to explore the association between age and pain intensity in Herpes zoster patients. A total of 613 patients treated at the Second Affiliated Hospital of Guangxi Medical University were included. Pain intensity was measured using the Numerical Rating Scale-11, and statistical models were applied to evaluate age-related pain differences while controlling for confounders. While older age was associated with higher pain scores (β = 0.02, p < 0.001), the effect size was small. Other factors, such as pain duration and inflammatory markers (e.g., CRP levels), showed stronger associations with pain severity. These findings suggest that age may not be the dominant factor in Herpes zoster pain severity, and a more comprehensive approach is required for risk assessment and pain management in clinical practice.
Similar content being viewed by others
Introduction
Herpes zoster (HZ), also known as shingles, results from reactivation of the varicella-zoster virus (VZV) and is characterized by a painful vesicular rash in a dermatomal distribution1. It is a common condition, with an estimated lifetime risk of 30% and incidence that increases markedly with age2,3. The acute pain associated with HZ is often severe and can significantly impact quality of life4,5.
While the increased incidence of HZ in older individuals is well-recognized6,7, the relationship between age and acute pain severity is less clear. Studies have shown that older age is a risk factor for postherpetic neuralgia (PHN), the most common complication of HZ, which causes persistent pain lasting months to years7,8. However, data on age-related differences in acute HZ pain severity are limited and often influenced by comorbidities and other factors8.
Acute pain control is a crucial aspect of HZ management, not only to alleviate suffering but also to potentially reduce the risk of PHN9. The UK National Institute for Health and Care Excellence (NICE) recommends considering patient age when making decisions about HZ treatment10. However, more robust evidence is needed to guide a comprehensive, multifactorial approach to acute pain management. Additionally, there is growing evidence of increasing HZ incidence among younger adults, challenging the traditional age-centric view of HZ risk11.
In this retrospective study, we aimed to evaluate the association between age and acute pain severity, as measured by Numerical Rating Scale-11 (NRS-11) scores, in a cohort of Chinese HZ patients. We hypothesized that older age would be independently associated with higher pain intensity, even after adjusting for potential confounders. Additionally, we explored associated laboratory abnormalities to shed light on potential biochemical correlates of age-related pain vulnerability in this population.
Results
Baseline characteristics of the study population
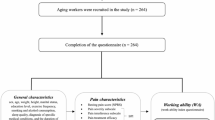
The baseline and pain characteristics of the study population, stratified by age, are presented in Table 1. The study included a total of 613 patients with HZ, with 167 (27.2%) aged 60 years or younger and 446 (72.8%) older than 60 years. The mean NRS-11 pain score was significantly higher in the older age group compared to the younger group (4.9 ± 1.3 vs. 4.6 ± 1.4, p = 0.008). No significant differences were observed between the age groups in terms of pain type, allodynia, gender, marital status, BMI, smoking, alcohol use, affected side, or pain location. However, the older age group had significantly lower levels of albumin, hemoglobin, and red blood cell count, and higher levels of CRP, cystatin C, and white blood cell count compared to the younger group (all p < 0.05).
Unadjusted association between age and NRS-11 score
The unadjusted associations between various patient characteristics and NRS-11 pain scores are shown in Table 2. Persistent pain duration (β = 0.73, 95% CI: 0.48, 0.97, p < 0.001), older age (β = 0.02 per year, 95% CI: 0.01, 0.03, p < 0.001), lower albumin levels (β = -0.05 per unit, 95% CI: -0.08, -0.02, p < 0.001), higher CRP levels (β = 0.01 per unit, 95% CI: 0.00, 0.01, p < 0.001), higher cystatin C levels (β = 0.28 per unit, 95% CI: 0.05, 0.51, p = 0.016), and higher white blood cell count (β = 0.06 per unit, 95% CI: 0.02, 0.10, p = 0.005) were significantly associated with higher NRS-11 pain scores in the univariate analysis. Female gender (β = -0.24, 95% CI: -0.46, -0.03, p = 0.028) and higher BMI (β = -0.03 per unit, 95% CI: -0.07, 0.00, p = 0.041) were associated with lower NRS-11 scores.
Adjusted association between age and NRS-11 score
The adjusted associations between age and NRS-11 pain scores are presented in Table 3. In the unadjusted model (Model 1), older age was significantly associated with higher NRS-11 scores (β = 0.02 per year, 95% CI: 0.01, 0.03, p < 0.001). Model 2 included covariates that were selected because they altered the effect estimate by more than 10%. After adjusting for albumin and CRP levels in Model 2, the association between age and NRS-11 scores remained significant (β = 0.02 per year, 95% CI: 0.01, 0.03, p < 0.001). Model 3 extended Model 2 by incorporating additional variables that had shown a significant association (P < 0.05) with NRS-11 scores in the univariate analysis. After further adjusting for gender, BMI, pain duration characteristics, cystatin C, and white blood cell count in Model 3, the association between age and NRS-11 scores persisted (β = 0.02 per year, 95% CI: 0.01, 0.03, p < 0.001).
Subgroup analysis to address age group distribution
The adjusted associations between age and NRS-11 pain scores in different age groups are presented in Table 4. In the subgroup analysis, we stratified patients into two groups: age ≤ 60 years and age > 60 years. In the younger subgroup (age ≤ 60 years), the adjusted coefficient for age was 0.03 per year (95% CI: 0.00, 0.06, P = 0.043). In the older subgroup (age > 60 years), the adjusted coefficient for age was 0.04 per year (95% CI: 0.02, 0.06, P < 0.001). The interaction P-value (P = 0.712) indicated no significant heterogeneity in the association between age and NRS-11 scores across the two subgroups. These findings confirm that the relationship between age and NRS-11 pain scores remains consistent across age strata.
Sensitivity analysis
The adjusted associations between age and NRS-11 pain scores, after applying different approaches to handle missing data, are presented in Tables 5 and 6. Following the exclusion of cases with missing values, 543 cases with complete data were retained for analysis, the adjusted coefficient for age was 0.02 per year (95% CI: 0.01, 0.03, P < 0.001), which is consistent with the primary analysis. After performing multiple imputation using a chained equation approach with 5 replications to account for missing data (n = 613), the adjusted coefficient for age remained at 0.02 per year (95% CI: 0.01, 0.03, P < 0.001).
Non-linear relationship between age and NRS-11 score
Figure 1 depicts the non-linear relationship between age and NRS-11 pain score, as assessed by a generalized additive model (GAM) with adjustments for potential confounders. The P-value for non-linearity was 0.631, indicating a linear relationship between age and NRS-11 score. The fitted smoothing curve (solid red line) and its 95% confidence interval (red shaded area) show a consistent increase in NRS-11 scores with advancing age.
Non-linear relationship between age and NRS-11 pain score, assessed by a generalized additive model (GAM). The solid red line represents the fitted smoothing curve, and the red shaded area indicates the 95% confidence interval. The analysis was performed using a generalized additive model (GAM) to capture the non-linear relationship between age and NRS-11 pain score. Adjustments were made for potential confounders, including albumin, CRP, gender, BMI, pain duration characteristics, cystatin C, and white blood cell count. The P-value for non-linearity was 0.631, indicating a linear relationship between age and NRS-11 score.
Discussion
Previous studies reporting increased HZ incidence and complications in older adults6,7,12,13. Our large retrospective study found a statistically significant but clinically modest association between age and acute HZ pain intensity (β = 0.02, 95% CI: 0.01, 0.03, p < 0.001). The β value of 0.02 indicates that a 10-year age difference corresponds to a 0.2-point increase on the NRS-11 scale, which, while statistically significant, appears modest and may have limited clinical implications in isolation14.
To further evaluate the potential impact of the uneven distribution between age groups (167 vs. 446) on our findings, we performed a subgroup analysis stratified by age (age ≤ 60 years and age > 60 years). The association between age and NRS-11 pain scores remained statistically significant in both subgroups, with adjusted coefficients of 0.03 (95% CI: 0, 0.06; P = 0.043) in the younger group and 0.04 (95% CI: 0.02, 0.06; P < 0.001) in the older group. Importantly, the P-value for interaction (P = 0.712) suggests no significant difference in the relationship between age and pain intensity across age strata. Similar to the overall analysis, the association within subgroups, while statistically significant, remained clinically modest and unlikely to influence clinical practice, suggesting that other factors may play a more critical role in pain management.
This small effect size highlights the multifactorial nature of acute HZ pain, where other factors such as pain duration (particularly persistent pain: β = 0.73, 95% CI: 0.48, 0.97, p < 0.001) and inflammatory markers may play more significant roles. Elevated inflammatory markers like CRP have been linked to greater acute HZ pain and PHN risk in previous studies15,16. Elevated CRP levels may reflect a more robust inflammatory response, which could contribute to increased nociceptive signaling and pain intensity17. Lower albumin levels might indicate poor nutritional status or immune function18. Further investigation into additional biological mechanisms is warranted.
These observations have important clinical implications. First, they underscore the need for vigilance and prompt treatment across all age groups, not just older adults. Combined with rising HZ incidence in younger adults11,19, young HZ patients may experience pain as severe as their older counterparts, possibly due to factors such as stress, sleep disturbances, or altered immune function20. This calls for a reexamination of HZ prevention strategies, which is consistent with recent guidelines that emphasize the importance of prompt antiviral therapy in the management of HZ21.
Current HZ vaccine recommendations primarily target older adults, with Shingrix approved for individuals 50 years and older22. Current age-based vaccination policies may not adequately capture high-risk individuals across all age spectra. A risk-factor based approach to vaccination could potentially identify younger individuals who might benefit from early vaccination. Future studies should evaluate the cost-effectiveness of such targeted vaccination strategies, considering both direct medical costs and the broader impact on quality of life2.
While our study provides valuable insights, several methodological considerations warrant discussion. The use of NRS-11 as the sole measure of pain intensity, while widely accepted, may not fully capture the multidimensional nature of pain23.The retrospective design of our study may introduce recall bias, as pain experiences are subjective and influenced by contextual factors. Although NRS-11 scores were recorded during initial consultations to minimize this risk, prospective studies with real-time pain assessments or electronic pain diaries are warranted to further enhance data accuracy. Such studies should also incorporate patient-reported outcomes beyond pain intensity, including measures of functional impairment and quality of life, to better reflect the patient experience24.
The retrospective, single-center design of our study may limit its generalizability. Patients were recruited from a tertiary hospital pain clinic, which may overrepresent individuals with moderate-to-severe pain, potentially limiting applicability to patients managed in primary care settings. Prospective, multicenter studies, including primary care and community-based cohorts, with long-term follow-up are needed to validate our findings and explore the temporal dynamics of age-pain relationships in HZ.
Additionally, the study period spanned five years (2019–2024), during which temporal factors, such as changes in antiviral treatment guidelines, vaccination coverage, or healthcare-seeking behaviors, may have influenced the results. Furthermore, the COVID-19 pandemic likely impacted healthcare access, diagnostic practices, and treatment timelines during specific phases of this period. These potential disruptions cannot be entirely excluded and warrant consideration when interpreting our findings. Future studies should incorporate sensitivity analyses to evaluate temporal variations in clinical outcomes.
Moreover, certain medications may have influenced laboratory parameters measured in our study. For example, anti-inflammatory drugs or corticosteroids could potentially alter CRP levels, while nephrotoxic medications might impact cystatin C levels. Although we did not collect detailed medication histories in this retrospective analysis, this remains a potential source of confounding. Future studies with comprehensive medication data are warranted to assess and adjust for these effects, ensuring a more precise evaluation of the relationship between laboratory parameters and pain intensity.
In conclusion, while age was statistically associated with higher HZ pain scores (β = 0.02), its clinical relevance is limited. Persistent pain duration and inflammatory markers (e.g., CRP) emerged as stronger predictors of pain severity. These findings highlight the need for a multifactorial approach to risk assessment and pain management. Future research should focus on validating these findings in broader populations and exploring targeted vaccination strategies to reduce the disease burden.
Methods
Study design
This retrospective study was conducted at the Second Affiliated Hospital of Guangxi Medical University in China. Ethical approval was obtained from the Ethics Committee of The Second Affiliated Hospital of Guangxi Medical University (approval number: 2024-KY(0509)). Due to the retrospective nature of the study, the Ethics Committee of The Second Affiliated Hospital of Guangxi Medical University waived the need for obtaining informed consent. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines25. This study was conducted in accordance with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations.
Study setting and participants
The study population included patients treated for HZ at the Department of Pain Medicine, Second Affiliated Hospital of Guangxi Medical University, from January 2019 to February 2024. Inclusion criteria were: (1) age ≥ 18 years; (2) International Classification of Diseases (ICD)-10 diagnosis codes for HZ, verified by clinical chart review; (3) Completion of standardized pain assessments prior to treatment initiation. Exclusion criteria were: (1) repeat visits for the same HZ episode; (2) missing baseline pain evaluations; (3) cognitive or communication impairments precluding reliable pain assessment; (4) conditions associated with altered pain perception (e.g., Parkinson’s disease)26.
Data sources, definitions and usage statement
To minimize information bias, we used standardized pain questionnaires and trained personnel for data collection. Data were retrieved from the pain virtual ward system, electronic medical record system, hospital information system, and laboratory information system of the Second Affiliated Hospital of Guangxi Medical University, with approval from the Ethics Committee and the Information Department.The the department of Pain Medicine and the Information Department collaboratively manage the pain virtual ward to ensure data integrity and traceability. These data will be used for further analyses, including identifying additional risk factors, developing pain prediction models, and analyzing pain trajectories. To ensure academic integrity and data transparency, we declare that subsequent studies may continue to use the same or updated datasets to facilitate comparison and comprehensive analysis of different research outcomes.
Patient and public involvement in research
As this was a retrospective observational study using pre-existing data from medical records, patients or the public were not directly involved in the conceptualization, design, or conduct of the research, or in the dissemination of the findings. The study relied on data routinely collected during past clinical care, without additional patient input.
Collected variables
Patient Demographics: Included age, gender, body mass index (BMI), marital status, smoking history, and alcohol use.
Pain-Related Information:
-
(1)
Pain intensity: Assessed using the NRS-11, where patients rated their pain on a scale from 0 (no pain) to 10 (worst possible pain)27. NRS-11 is one of the most widely used and validated tools for assessing pain intensity in clinical and research settings27,28. It has been shown to have high reliability, validity, and responsiveness, comparable to the Visual Analogue Scale (VAS), but with better ease of use and comprehension for patients29. Compared to the VRS and Faces Pain Scale-Revised (FPS-R), the NRS-11 is less influenced by non-pain factors and demonstrates superior sensitivity and test-retest stability28,30.
For HZ patients specifically, the NRS-11 has been widely applied in both acute and chronic pain assessments because of its ability to detect clinically relevant changes in pain intensity and its ease of administration in busy clinical settings31,32,33,34. Given the severe and episodic nature of HZ pain, patients are typically able to accurately quantify their pain on a numerical scale. To minimize potential recall bias, NRS-11 scores were recorded during patients’ initial consultations, when pain intensity was typically at its peak. This approach enhances the reliability of the pain scores collected in this study.
-
(2)
Pain Location: Documented areas of HZ pain.
-
(3)
Pain type: Pain types were classified using the DN4(Douleur Neuropathique 4) questionnaire and the validated Chinese version of the Neuropathic Pain Diagnostic and Treatment Assessment Scale35,36. The DN4 questionnaire is a widely used tool designed specifically to identify neuropathic pain components, which are highly relevant in HZ due to nerve inflammation and damage. The Chinese version ensures accurate classification of pain types in the Chinese-speaking population, addressing linguistic and cultural differences in pain perception. The selected pain types—burning, pins and needles, electric shock, tingling, itching, and others ( tearing pain, throbbing pain, pulling pain, twitching pain, and aching pain). Classifying these specific subtypes is essential for identifying sensory abnormalities associated with HZ neuropathy and facilitating targeted strategies for the management of neuropathic pain37.
-
(4)
Pain duration characteristics: Classified as intermittent or continuous pain. Different diseases and pain management strategies require different definitions of pain duration38,39,40,41.Considering the generally short disease course of most HZ patients, with some seeking treatment on the first day of pain, continuous pain was defined as pain persisting throughout the day regardless of intensity; intermittent pain was defined as pain with significant relief periods within a day.
-
(5)
Allodynia: Pain due to a stimulus that does not usually provoke pain42.
Laboratory data
Fasting peripheral venous blood samples were collected within 24 h of the initial clinical consultation to ensure consistency with the NRS-11 pain assessment. The laboratory parameters measured included globulin, albumin, hemoglobin, C-reactive protein (CRP), cystatin C, platelet count, red blood cell count, urea, and white blood cell count .All laboratory parameters were analyzed as continuous variables, and no cut-off points were applied.
Charlson Comorbidity Index (CCI)
CCI was used to assess comorbidities, including myocardial infarction, congestive heart failure, cerebrovascular disease, diabetes, moderate/severe renal disease, tumor, leukemia, lymphoma, moderate/severe liver disease, metastatic tumor, and acquired immunodeficiency syndrome (AIDS). Previous studies have shown that CCI may help identify high-risk HZ patients43,44.
Statistical analysis
All analyses were conducted using R Statistical Software (Version 4.2.2, http://www.R-project.org, The R Foundation) and Free Statistics analysis platform (Version 1.9, Beijing, China). Continuous variables were expressed as mean ± standard deviation (SD) or median and interquartile range (IQR), while categorical data were presented as numbers and percentages. Missing values were noted for several variables, with the majority being below 5%. Given the low proportion of missing data and its occurrence primarily in covariates, no special handling was performed for missing values in the primary analysis45. To ensure the robustness of our conclusions, we conducted sensitivity analyses, including (1) multiple imputation using a chained equation approach with 5 replications in the R mice package and (2) a complete case analysis that excluded observations with missing values.
For continuous data with normal distribution, independent samples t-tests were used for comparisons between two groups; for non-normally distributed continuous data, Mann-Whitney U tests were used. Categorical variables were compared using Pearson chi-square tests or Fisher’s exact tests. A P-value of < 0.05 was considered statistically significant.
Univariate linear regression models were initially used to explore the relationship between baseline variables and NRS-11 scores.Variables with P < 0.05 in the univariate analysis were considered for inclusion in the multivariate models. In the subsequent multivariate analysis, Model 1 assessed the association between age and NRS-11 scores without adjusting for any covariates. Model 2 included covariates that were selected because they altered the effect estimate by more than 10%46. Finally, Model 3 extended Model 2 by incorporating additional variables that had shown a significant association (P < 0.05) with NRS-11 scores in the univariate analysis. Additionally, a generalized additive model (GAM) with a natural spline (4 knots) was employed to fit smoothing curves, allowing for a more nuanced understanding of the relationship between age and NRS-11 scores.
Data availability
The datasets are available from the corresponding author on reasonable request.
References
Le, P. & Rothberg, M. Herpes zoster infection. BMJ (Clin. Res. ed.). 364, k5095. https://doi.org/10.1136/bmj.k5095 (2019).
Kawai, K., Gebremeskel, B. G. & Acosta, C. J. Systematic review of incidence and complications of herpes zoster: Towards a global perspective. BMJ Open. 4, e004833. https://doi.org/10.1136/bmjopen-2014-004833 (2014).
Yawn, B. P. & Gilden, D. The global epidemiology of herpes zoster. Neurology 81, 928–930. https://doi.org/10.1212/WNL.0b013e3182a3516e (2013).
Mbinta, J. F., Nguyen, B. P., Awuni, P. M. A., Paynter, J. & Simpson, C. R. Post-licensure zoster vaccine effectiveness against herpes zoster and postherpetic neuralgia in older adults: A systematic review and meta-analysis. Lancet Healthy Longev. 3, e263–e275. https://doi.org/10.1016/s2666-7568(22)00039-3 (2022).
Yin, D. et al. A systematic literature review to assess the burden of herpes zoster disease in China. Expert Rev. Anti-infect. Therapy. 19, 165–179. https://doi.org/10.1080/14787210.2020.1792290 (2021).
van Oorschot, D. et al. A systematic literature review of herpes zoster incidence worldwide. Hum. Vaccines Immunotherap. 17, 1714–1732. https://doi.org/10.1080/21645515.2020.1847582 (2021).
Zhang, Z. et al. The incidence of herpes zoster in China: A meta-analysis and evidence quality assessment. Hum. Vaccines Immunother. 19, 2228169. https://doi.org/10.1080/21645515.2023.2228169 (2023).
Joesoef, R. M., Harpaz, R., Leung, J. & Bialek, S. R. Chronic medical conditions as risk factors for herpes zoster. Mayo Clin. Proc. 87, 961–967. https://doi.org/10.1016/j.mayocp.2012.05.021 (2012).
Mallick-Searle, T., Snodgrass, B. & Brant, J. M. Postherpetic neuralgia: Epidemiology, pathophysiology, and pain management pharmacology. J. Multidiscip. Healthc. 9, 447–454. https://doi.org/10.2147/jmdh.S106340 (2016).
Excellence N. I. f. H. a. C. Shingles < (2024). https://cks.nice.org.uk/topics/shingles/
Kawai, K., Yawn, B. P., Wollan, P. & Harpaz, R. Increasing incidence of herpes Zoster over a 60-year period from a Population-based study. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 63, 221–226. https://doi.org/10.1093/cid/ciw296 (2016).
Patil, A., Goldust, M. & Wollina, U. Herpes zoster: A review of clinical manifestations and management. Viruses 14 https://doi.org/10.3390/v14020192 (2022).
Rosamilia, L. L. Herpes zoster presentation, management, and prevention: A modern case-based review. Am. J. Clin. Dermatol. 21, 97–107. https://doi.org/10.1007/s40257-019-00483-1 (2020).
Farrar, J. T., Young, J. P. Jr., LaMoreaux, L., Werth, J. L. & Poole, M. R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 94, 149–158. https://doi.org/10.1016/s0304-3959(01)00349-9 (2001).
Oskay, T., Keskin, C. & Özen, M. Antioxidant and inflammatory biomarkers in herpes zoster. J. Med. Virol. 94, 3924–3929. https://doi.org/10.1002/jmv.27781 (2022).
Yue, J. & Yao, M. Humoral cytokine levels in patients with herpes zoster: A Meta-analysis. J. Pain Res. 17, 887–902. https://doi.org/10.2147/jpr.S449211 (2024).
Parkitny, L. et al. Inflammation in complex regional pain syndrome: A systematic review and meta-analysis. Neurology 80, 106–117. https://doi.org/10.1212/WNL.0b013e31827b1aa1 (2013).
Eckart, A. et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: A prospective study. Am. J. Med. 133, 713–722e717. https://doi.org/10.1016/j.amjmed.2019.10.031 (2020).
Harpaz, R. & Leung, J. W. The epidemiology of Herpes Zoster in the United States during the era of varicella and herpes zoster vaccines: Changing patterns among older adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 69, 341–344. https://doi.org/10.1093/cid/ciy953 (2019).
Hadley, G. R. et al. Post-herpetic neuralgia: A review. Curr. Pain Headache Rep. 20 https://doi.org/10.1007/s11916-016-0548-x (2016).
Werner, R. N. et al. European consensus-based (S2k) Guideline on the management of herpes zoster - guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV), part 1: Diagnosis. J. Eur. Acad. Dermatol. Venereol. JEADV. 31, 9–19. https://doi.org/10.1111/jdv.13995 (2017).
Dooling, K. L. et al. Recommendations of the advisory committee on immunization practices for Use of herpes zoster vaccines. MMWR Morb. Mortal. Wkly Rep. 67, 103–108. https://doi.org/10.15585/mmwr.mm6703a5 (2018).
Wood, B. M., Nicholas, M. K., Blyth, F., Asghari, A. & Gibson, S. Assessing pain in older people with persistent pain: The NRS is valid but only provides part of the picture. J. Pain. 11, 1259–1266. https://doi.org/10.1016/j.jpain.2010.02.025 (2010).
Coplan, P. M. et al. Development of a measure of the burden of pain due to herpes zoster and postherpetic neuralgia for prevention trials: Adaptation of the brief pain inventory. J. Pain. 5, 344–356. https://doi.org/10.1016/j.jpain.2004.06.001 (2004).
Vandenbroucke, J. P. et al. Strengthening the reporting of Observational studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 4, e297. https://doi.org/10.1371/journal.pmed.0040297 (2007).
Breivik, H. et al. Assessment of pain. Br. J. Anaesth. 101, 17–24. https://doi.org/10.1093/bja/aen103 (2008).
Ferreira-Valente, M. A., Pais-Ribeiro, J. L. & Jensen, M. P. Validity of four pain intensity rating scales. Pain 152, 2399–2404. https://doi.org/10.1016/j.pain.2011.07.005 (2011).
Euasobhon, P. et al. Reliability and responsivity of pain intensity scales in individuals with chronic pain. Pain 163, e1184–e1191. https://doi.org/10.1097/j.pain.0000000000002692 (2022).
Breivik, H. Patients’ subjective acute pain rating scales (VAS, NRS) are fine; More elaborate evaluations needed for chronic pain, especially in the elderly and demented patients. Scandinavian J. Pain. 15, 73–74. https://doi.org/10.1016/j.sjpain.2017.01.001 (2017).
Thong, I. S. K., Jensen, M. P., Miró, J. & Tan, G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R measure? Scandinavian J. Pain. 18, 99–107. https://doi.org/10.1515/sjpain-2018-0012 (2018).
Imafuku, S. et al. One-year follow-up of zoster-associated pain in 764 immunocompetent patients with acute herpes zoster treated with famciclovir (FAMILIAR study). J. Eur. Acad. Dermatol. Venereol. JEADV. 28, 1716–1722. https://doi.org/10.1111/jdv.12379 (2014).
Wang, X. X., Zhang, Y. & Fan, B. F. Predicting postherpetic neuralgia in patients with herpes zoster by machine learning: A retrospective study. Pain Therapy. 9, 627–635. https://doi.org/10.1007/s40122-020-00196-y (2020).
Wang, L., Lei, X., Lan, Z., He, R. & Jiang, Z. Ultrasound-guided thoracic paravertebral injection of platelet-rich plasma for the treatment of thoracic herpes zoster-related Pain: A study protocol. Pain Therapy. https://doi.org/10.1007/s40122-024-00691-6 (2024).
Peng, Z. et al. Development of a model for predicting the effectiveness of pulsed radiofrequency on zoster-associated pain. Pain Therapy. 11, 253–267. https://doi.org/10.1007/s40122-022-00355-3 (2022).
Wang, Y. F. et al. Development and validation of a Taiwan version of the DN4-T questionnaire. J. Chin. Med. Assoc. JCMA. 82, 623–627. https://doi.org/10.1097/jcma.0000000000000129 (2019).
Zongbin, J. et al. Development and validation of a Chinese scale for diagnosis and efficacy evaluation of Neuropathic Pain. Chin. J. Painol. 18, 466–475. https://doi.org/10.3760/cma.j.cn101658-20220705-00106 (2022).
Truini, A. et al. Joint European Academy of Neurology-European Pain Federation-Neuropathic Pain Special Interest Group of the International Association for the Study of Pain guidelines on neuropathic pain assessment. Eur. J. Neurol. 30, 2177–2196. https://doi.org/10.1111/ene.15831 (2023).
Ritchie, C. S. et al. Impact of persistent pain on function, cognition, and well-being of older adults. J. Am. Geriatr. Soc. 71, 26–35. https://doi.org/10.1111/jgs.18125 (2023).
Rong, W. et al. Persistent moderate to severe pain and long-term cognitive decline. Eur. J. Pain. 25, 2065–2074. https://doi.org/10.1002/ejp.1826 (2021).
Sellevold, V. B. et al. Many patients with persistent Pain 1 Year after TKA Report Improvement by 5 to 7 years: A mixed-methods study. Clin. Orthop. Relat. Res. 480, 2075–2088. https://doi.org/10.1097/corr.0000000000002183 (2022).
Hunnicutt, J. N., Ulbricht, C. M., Tjia, J. & Lapane, K. L. Pain and pharmacologic pain management in long-stay nursing home residents. Pain 158, 1091–1099. https://doi.org/10.1097/j.pain.0000000000000887 (2017).
Jensen, T. S. & Finnerup, N. B. Allodynia and hyperalgesia in neuropathic pain: Clinical manifestations and mechanisms. Lancet Neurol. 13, 924–935. https://doi.org/10.1016/s1474-4422(14)70102-4 (2014).
Cho, S. I., Lee, D. H. & Park, Y. M. Identification of herpes zoster high-risk group using Charlson comorbidity index: A nationwide retrospective cohort study. J. Dermatol. 47, 47–53. https://doi.org/10.1111/1346-8138.15115 (2020).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40, 373–383. https://doi.org/10.1016/0021-9681(87)90171-8 (1987).
Jakobsen, J. C., Gluud, C., Wetterslev, J. & Winkel, P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med. Res. Methodol. 17 https://doi.org/10.1186/s12874-017-0442-1 (2017).
Jaddoe, V. W. et al. First trimester fetal growth restriction and cardiovascular risk factors in school age children: Population based cohort study. BMJ (Clin. Res. Ed.). 348, g14. https://doi.org/10.1136/bmj.g14 (2014).
Acknowledgements
We would like to thank the Department of Pain Medicine and and Information Department at Guangxi Medical University for providing the necessary resources and support for this study. Special thanks to all the patients whose data contributed to this research.
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
L.W. and A.L. contributed equally as co-first authors, while R.H. and Z.J. served as co-corresponding authors. L.W. and A.L. conceptualized, designed the study, and conducted statistical analysis. Z.L. and S.X. managed data collection and prepared study materials, including tables and figures. L.W. and A.L. drafted the main manuscript text. R.H. and Z.J. provided overall guidance and critically revised the manuscript.All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval for this study was granted by the Ethics Committee of The Second Affiliated Hospital of Guangxi Medical University (2024-KY(0509)). Due to the retrospective nature of the study, the Ethics Committee of The Second Affiliated Hospital of Guangxi Medical University waived the need for obtaining informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, L., Li, A., Lan, Z. et al. The association between age and acute pain sensitivity in patients with Herpes Zoster. Sci Rep 15, 5495 (2025). https://doi.org/10.1038/s41598-025-88618-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88618-9