Abstract
Kidney cancer, a prevalent malignant tumor in the urinary system, poses a significant disease burden and remains a crucial public health concern. Utilizing GBD(Global Burden of Disease)2021 data, our study examined the standardized incidence, mortality, prevalence, and DALYs(Disability Adjusted Life Years) rate of renal cancer. We calculated the [1-MIR(Mortality to Incidence Ratio)] value to assess treatment outcomes and survival rates, employed a joinpoint regression model to determine the AAPC(Average Annual Percentage Change), and conducted comparative and longitudinal analyses between China and global trends. The SII(Slope Index of Inequality) and the CI(Concentration Index) were used to assess the DALYs inequality caused by kidney cancer, and the SDI(Socio-demographic Index) was used as the basis for the ranking. Through the joinpoint regression model, we calculated the AAPC and conducted a comprehensive analysis of the disease burden of kidney cancer, evaluating its current status and changing trends. From 1990 to 2021, the age-standardized incidence rate, age-standardized mortality rate, age-standardized prevalence rate, and age-standardized DALYs rate of kidney cancer in China were lower than those the global average. However, the growth rate in China was significantly faster than the global average. The age-standardized incidence rate and prevalence rate of kidney cancer in males showed a greater increase compared to females, both in China and globally. Additionally, the age-standardized rate of kidney cancer in males was notably higher than in females, particularly among middle-aged males. The (1-MIR) of renal cancer increased from 0.36 to 0.62 in China and from 0.49 to 0.58 globally. Overall, the treatment effect of renal cancer has shown some successful outcomes. The SII decreased from 53.47 to 50.19, and the CI decreased from 0.342 to 0.289. The health inequality level of kidney cancer was significant but alleviated. From 1990 to 2021, there was a noticeable increase in the global incidence of kidney cancer. Specifically, the standardized incidence and prevalence of kidney cancer in the Chinese population saw a more rapid rise compared to the global average. Additionally, the disease burden of kidney cancer remained significantly higher in males than in females.
Similar content being viewed by others
Introduction
Kidney cancer, a prevalent malignancy of the urinary system, poses a significant global health burden. In 2020, there were approximately 431,000 new cases reported worldwide, as per the latest data from the International Agency for Research on Cancer (IARC) of the World Health Organization (WHO). The incidence and mortality rates of kidney cancer exhibit variations across regions, age groups, and genders. While developed countries currently report the highest rates, trends suggest a potential decline in the future. For instance, some Western European nations have witnessed a decrease in kidney cancer mortality over recent decades1. In the United States, the age-adjusted mortality rate (ASMR) for kidney cancer varies significantly based on sex, race, and age2. However, projections indicate a continued rise in both incidence and mortality globally, including in developing and less developed countries. Notably, kidney cancer ranks as the second most common genitourinary cancer in China, comprising 2–3% of adult cancers and 20% of pediatric cases. Therefore, a comprehensive understanding of the disease burden and epidemiological characteristics of kidney cancer is crucial for the development of effective prevention and intervention strategies.
Previous studies have explored the impact of socioeconomic status on the changing burden of kidney cancer3,4,5. Recent research has shown that exposure to various risk factors has played a role in influencing the prevalence of kidney cancer6. A significant portion of global cancer-related deaths are preventable, with smoking, alcohol consumption, and high BMI being key factors contributing to both cancer deaths and DALYs7. Smoking has been identified as a known risk factor for kidney cancer8,9, with heavy smokers in the Japanese population having a higher risk of renal cell carcinoma, similar to findings in Western countries10. Moreover, smoking has been linked to prognosis in renal cell carcinoma survival across different populations11. Additionally, high BMI, hypertension, and diabetes mellitus have also been recognized as risk factors for kidney cancer12. The association between alcohol consumption and kidney cancer risk remains controversial. Epidemiological trends of kidney cancer vary geographically, and the impact of these risk factors on different genders and age groups is not fully understood. Current research primarily focuses on clinical and treatment aspects of kidney cancer, with limited attention to disease burden. There is a gap in comparative analysis between China and the global landscape, as well as a lack of longitudinal analysis of kidney cancer burden. Therefore, continuous monitoring and analysis of kidney cancer burden, prevention, and control efforts are necessary to comprehensively understand epidemiological characteristics and risk factors across different countries and regions, facilitating more precise prevention and control strategies for kidney cancer.
Method
Data sources
This study was based on data from the Global Burden of Disease (GBD) 2021 database, which assesses the burden of disease of 459 diseases and injuries and risk factors in 204 countries and territories. Detailed data were downloaded from the Global Health Data Exchange (GHDx) database. Incidence, mortality, prevalence, disability-adjusted life years ratio (DALYs), and [1-MIR (Mortality to Incidence Ratio)] were used to estimate the disease burden of kidney cancer. (1-MIR) can be calculated by the formula 1-mortality/incidence, which is widely used as a surrogate indicator for the 5-year relative survival rate of cancer and an indicator for evaluating the effectiveness of cancer prevention and control13,14. The SII and the CI were used to assess the health inequality caused by kidney cancer in 204 countries and territories, and the SDI was used as the basis for the ranking.
Statistical analysis
Based on comprehensive observation of the data of kidney cancer patients, the disease burden of kidney cancer in China and the world in 1990 and 2021 was compared by gender group. The line chart was used to show the changing trend of the standardized incidence, mortality, prevalence, and DALYs rate of kidney cancer in China and around the world from 1990 to 2021. Bar charts were used to describe the proportion of standardized incidence and mortality of kidney cancer in different age groups of men and women in China and the world in 1990 and 2021. According to the global age-standardized population weight15, the direct standardization method was used to calculate the corresponding standardized rate of some age groups. The formula was as follows: the standardized rate of an index in a certain age group = ∑ the population of the standard age group in the same age group (1 group every 5 years) × the crude rate of the index in the age group/the total standard population. Regression curves and concentration curves were used to describe the health inequalities of kidney cancer in 204 countries and territories. Using the Joinpoint Regression Program 5.1.0 software developed by the American Cancer Institute, a log-linear regression model was used to calculate the average annual percent change (AAPC) of age-standardized incidence, age-standardized mortality, age-standardized prevalence, and DALYs age-standardized rate of kidney disease in China and the world from 1990 to 2021.
Results
Baseline
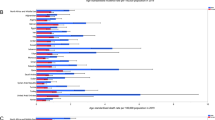
Age-standardized incidence and mortality rates for kidney cancer in 2021 varied widely across the 21 GBD regions. Southern Latin America had the highest age-standardized incidence rate (0.24/105), followed by High-income North America (0.24/105) and Western Europe (9.74/105). On the other hand, Oceania (0.64/105), Central Sub-Saharan Africa (0.95/105), and Western Sub-Saharan Africa (0.98/105) had the lowest age-standardized prevalence rates. In terms of mortality rates, Southern Latin America (4.55/105), Central Europe (4.22/105), and Eastern Europe (3.97/105) were the regions with the highest age-standardized rates, while Oceania (0.41/105), South Asia (0.71/105), and Western Sub-Saharan Africa (0.72/105) had the lowest rates. Among the 204 countries and territories, there was significant variation in age-standardized incidence rates of kidney cancer. The three countries with the highest rates were Argentina (15.60/105), Czechia (14.69/105), and Latvia (14.23/105). In contrast, Micronesia (Federated States of) (0.96/105), Uzbekistan (2.39/105), and Thailand (3.06/105) had the lowest rates. Uruguay (6.47/105), Czechia (5.95/105), and Lithuania (2.25/105) showed the highest age-standardized mortality rates, while Cook Islands (0.24/105), Morocco (0.27/105), and Palau (0.30/105) had the lowest rates. Figures 1 and 2 illustrate the national and district-level age-standardized incidence and mortality rates for all GBD regions in 2021.
Disease burden of kidney cancer from 1990 to 2021
From 1990 to 2021, the age-standardized incidence, mortality, prevalence, and DALYs rate of kidney cancer in China were lower than the global level. In 2021, the age-standardized incidence rate, age-standardized mortality rate, age-standardized prevalence rate, and age-standardized DALYs rate of kidney cancer in China were 3.319/105, 1.5246/105, 17.754/105, and 34.176/105, respectively, which were higher than those in the world (4.524/105, 1.912/105, and 22.695/105,) and 47.327/105, respectively. Compared with 1990, the age-standardized incidence (3.319/105, vs. 1.794/105,), age-standardized mortality (1.246/105, vs. 1.140/105,), and age-standardized prevalence (17.754/105, vs. 7.191/105,) of kidney cancer in China increased in 2021. The standardized DALYs rate (34.176/105, vs. 35.838/105,) decreased, as shown in Figs. 1 and 2, and Table 1.
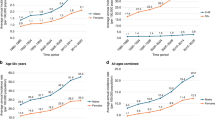
From 1990 to 2021, the age-standardized rate of kidney cancer in males was higher than that in females, both in China and globally. The Chinese standardized incidence and prevalence of kidney cancer growth were significantly higher than the overall global standardized incidence and prevalence of the disease in men than in women, with a significantly higher standardized incidence and prevalence of growth. The age-standardized DALYs rate in Chinese women showed a downward trend, while the age-standardized DALYs rate in Chinese men showed an upward trend. See Fig. 3.
Survival of kidney cancer from 1990 to 2021
There are noticeable variations in Maternal Mortality Ratio (1-MIR) levels across the 204 countries and territories worldwide. As of 2021, Switzerland has the highest (1-MIR) at 0.76, followed by the United States of America at 0.74 and France at 0.74. Conversely, the Central African Republic exhibits the lowest (1-MIR) at 0.14, followed by Somalia at 0.15 and Mozambique at 0.16. Refer to Fig. 4 for visual representation.
From 1990 to 2021, renal cancer (1-MIR) showed an upward trend in both China and the world, and the increase rate of renal cancer (1-MIR) in China was more obvious. The 1-MIR of kidney cancer in China increased from 0.36 to 0.62, and the 1-MIR of kidney cancer globally increased from 0.49 to 0.58. The renal cancer (1-MIR) in China was lower than the global level from 1990 to 2010, but higher than the global level from 2010 to 2021. See Table 2.
Survival analysis of kidney cancer in different age and gender groups from 1990 to 2021
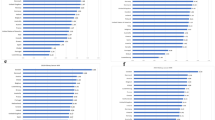
Compared with 1990, the proportion of kidney cancer cases in men in all age groups showed an increasing trend, while the proportion of women in all age groups showed a decreasing trend both in China and globally. In 2021, the proportion of kidney cancer cases in males was much higher than that in females in all age groups under 95 years old in China, especially in the 40–49 year old group. The proportion of kidney cancer cases in males vs. females aged 40–44 years old and 45–49 years old was 79.09% vs. 20.91% and 79.08% vs. 20.92%, respectively. At the same time, the proportion of males in the incidence of kidney cancer in 5–64 years old and > 75 years old and above in China was higher than that of the corresponding global level, especially in the 35–39 age group, which was 77.37% in China and 64.14% in the world, as shown in Fig. 5.
Compared with 1990, in 2021, the proportion of male kidney cancer deaths in all age groups in China and the world showed an increasing trend, especially in people under 5 years old, with an increase of 15.2% and 14.3% in this age group, respectively. In 2021, the proportion of kidney cancer cases in males in all age groups in China was higher than that at the corresponding global level. The proportion of kidney cancer deaths in males was higher than that in females in all age groups in China and the world under 95 years old, especially in the age group 40–54 years old in China. The proportion of male kidney cancer deaths in the 40–44 years old, 45–59 years old, and 50–54 years groups was 82.30%, 83.0%, and 82.37%, respectively, and the corresponding global age level was 73.43%, 75.04%, and 75.56%. See Fig. 6.
Cross-country inequality analysis
The analysis of health inequalities for kidney cancer showed significant differences in the distribution of DALYs related to SDI across 204 countries and territories. These differences decreased over time, indicating an improvement in kidney cancer health inequities globally. The SII in 1990 was 53.47, meaning that countries with the highest SDI had an excess of 53.47 DALYs of kidney cancer per 100,000 population compared to countries with the lowest SDI. By 2021, this gap had narrowed to 50.19, demonstrating a reduction in absolute inequality. Meanwhile, the CI also showed a decline from 0.342 in 1990 to 0.289 in 2021, further confirming the reduction in health inequality. These data reflect the positive impact of global health policies and interventions in reducing health inequalities. However, this inequity persists, and sustained attention and efforts are needed to further reduce global health inequities in kidney cancer. By using DALYs as a measure, we can more accurately assess and compare the burden of health across countries and at different points in time, as well as the extent of health inequalities. See Fig. 7.
Joinpoint regression analysis of the disease burden of kidney cancer from 1990 to 2021
From 1990 to 2021, the standardized incidence and prevalence of kidney cancer in China and worldwide exhibited an increasing trend, while the standardized DALYs rate showed a decreasing trend. Notably, the standardized mortality rate in China increased, contrasting the global decreasing trend. The rise in age-standardized incidence and prevalence rates in China outpaced those observed globally. The AAPC values for age-standardized incidence, mortality, prevalence, and DALYs rate of kidney cancer in China were 1.98%, 0.18%, 2.94%, and − 0.28%, respectively, whereas the global AAPCs were 0.49%, -0.13%, -0.89%, and − 0.37%, respectively. The most significant change was seen in the age-standardized prevalence of kidney cancer. Refer to Table 3 for detailed data.
When analyzing the period from 1990 to 2021, the age-standardized incidence and prevalence rates of kidney cancer displayed an upward trajectory in both men and women in China and globally, with the age-standardized mortality rate decreasing in women but increasing in men. The changes observed in age-standardized rates for men and women in China were more pronounced than those at the global level. Specifically, the age-standardized incidence rates for Chinese males vs. Chinese females and global males vs. global females were 2.33% vs. 1.12% and 0.68% vs. 0.15%, respectively. The age-standardized incidence rates for Chinese men vs. Chinese women and global men vs. global women were 3.58% vs. 1.81% and 1.15% vs. 0.43%, respectively. Refer to Table 3 for prevalence figures.
Discussion
This study analyzed the burden of kidney cancer in China over a 30-year period using the latest GBD2021 cancer statistics. The research compared the incidence, mortality, prevalence, and DALYs rate of kidney cancer in China to global levels from 1990 to 2021. The findings revealed that the age-standardized rates of kidney cancer in China were lower than the global average, but the growth rate of incidence and prevalence in China outpaced the global trends. While the incidence and prevalence rates increased in both China and globally, the age-standardized DALYs rate decreased. At the same time, the SII and CI revealed that the current global absolute and relative health inequity indexes of kidney cancer are still significant, but have decreased in 2021 compared with before, indicating that the level of global health inequity of kidney cancer has been reduced. The study also noted a rising trend in 1-MIR for kidney cancer in both China and worldwide, with a more significant increase observed in China. Notably, since 2010, the 1-MIR of kidney cancer in China has surpassed the global level, suggesting improved survival rates and successful prevention and control efforts.
From 1990 to 2021, the incidence of kidney cancer in China has been steadily increasing, with the age-standardized incidence rate remaining below the global average. However, the annual increase in the age-standardized incidence rate among the Chinese population has been higher than the global average, with China experiencing a threefold increase compared to the global level. The rise in kidney cancer incidence in China may be attributed to overdiagnosis in recent decades, facilitated by advancements in detection methods that can now identify even small renal masses16,17. Furthermore, both the prevalence and mortality rates of kidney cancer in China have been on the rise, aligning with findings from previous research18. Lifestyle factors such as smoking and alcohol consumption have been identified as potential risk factors for kidney cancer19, with smoking significantly increasing the risk and alcohol consumption also being confirmed as a significant risk factor10. The increasing prevalence of chronic diseases in recent years may also contribute to the rising rates of kidney cancer, with studies showing associations between hypertension, diabetes, chronic kidney disease, and the risk of developing kidney cancer20,21. In addition, the incidence of kidney cancer has increased significantly since 2019, which is probably affected by the COVID-19 epidemic. Patients with COVID-19 not only show lung damage, but also are often accompanied by multiple organ damage such as kidney damage22. The COVID-19 pandemic has led to the delay and interruption of treatment for patients with renal cell carcinoma, affecting the treatment effect and prognosis of patients23. In the meantime, patients with COVID-19 require more hospitalizations than uninfected patients24, but the significant impact on cancer outcomes remains to be demonstrated.
From 1990 to 2021, the age-standardized incidence, mortality, and prevalence of kidney cancer in men in China and globally were consistently higher than those in women. This trend of higher rates in men was also observed in previous studies25,26. Specifically, the standardized mortality rate of kidney cancer in men has increased, indicating a higher risk of death in recent years compared to women27. Previous research has highlighted that men with chronic kidney disease are more likely to be diagnosed with advanced cancer and have a higher mortality rate. Smoking is a known risk factor for kidney cancer incidence and prognosis28. Furthermore, studies suggest that women’s greater emphasis on health checkups may lead to earlier detection and treatment of kidney cancer, resulting in lower mortality rates29. Gender differences in the pathogenesis, clinical manifestations, and imaging findings of renal cell carcinoma may impact diagnosis and treatment strategies30. In terms of age distribution, the proportion of males in all age groups has increased from 1990 to 2021, contrasting with the trend in females. Notably, the high proportion of standardized mortality rate in males is concentrated in the middle-aged group, particularly significant in Chinese males aged 40–54 in 2021, highlighting the severity of kidney cancer in the middle-aged male population.
The prevention of cancer and reduction in associated deaths can largely be achieved through widespread adoption of effective prevention measures. It is crucial to assess the long-term success and efficiency of such prevention programs. The Mortality-to-Incidence Ratio (MIR) is recognized as a straightforward and informative measure to gauge the effectiveness of cancer control programs31. Previous research has demonstrated that (1-MIR) is linked to the success of cancer prevention and control efforts, and has been utilized to explore the correlation between healthcare systems and cancer outcomes on a national32 and global scale33. Previous studies have shown that (1-MIR) is associated with the effectiveness of cancer prevention and control, and this indicator has been used to examine the relationship between the health care system and cancer outcomes in the United States and globally34,35. In this study, (1-MIR) was used to evaluate the survival of kidney cancer and the effectiveness of cancer control in China and globally. This study employed (1-MIR) to assess the survival rates of kidney cancer and the effectiveness of cancer control efforts in China and globally. Between 1990 and 2021, the (1-MIR) for kidney cancer exhibited an upward trajectory in both China and worldwide, with a more pronounced increase observed in China. Throughout this period, the (1-MIR) for kidney cancer in China remained below the global average, but surpassed it after 2010, indicating a significant enhancement in kidney cancer survival rates. This improvement in kidney cancer survival could be attributed to factors such as socio-economic development and advancements in healthcare systems36,37. Furthermore, the continual enhancement of cancer prevention and control systems over the past three decades has played a pivotal role in this progress38.
This study examined the disease burden trends of kidney cancer from 1990 to 2021, comparing data between China and the global population. Findings indicate that the global disease burden continues to increase, with males experiencing a significantly higher burden than females. The age-standardized incidence and prevalence of kidney cancer in China are rising at a faster rate than the global average. The study underscores the urgent need for increased attention to the serious disease burden of kidney cancer. It also highlights the importance of enhancing research on risk factor exposure and strengthening prevention and control strategies.
Data availability
The data that support the findings of this study are available in GBD2021 at ghdx.healthdata.org.
References
Levi, F., Lucchini, F., Negri, E. & La Vecchia, C. Decreasing mortality from kidney cancer in Europe. Ann. Oncol. 15(7), 1130–1135 (2004).
Abdallah, N. et al. Kidney cancer mortality in the United States between 1999 and 2020: An observational analysis of outcomes by gender, race, and ethnicity. J. Name Unspecified, 4563–4563 (2023).
Kim, L. H. et al. Alcohol consumption and socioeconomic status associated with the risk of kidney cancer in a large Australian cohort study. Ann. Epidemiol. 84, 16–24 (2023).
Mellemgaard, A., Engholm, G., McLaughlin, J. K. & Olsen, J. H. Risk factors for renal cell carcinoma in Denmark. I. Role of socioeconomic status, tobacco use, beverages, and family history. Cancer Causes Control. 5 (2), 105–113 (1994).
Zi, H. et al. Global, regional, and national burden of kidney, bladder, and prostate cancers and their attributable risk factors, 1990–2019. Mil Med. Res. 8(1), 60 (2021).
Tian, Y. Q. et al. Trends and risk factors of global incidence, mortality, and disability of genitourinary cancers from 1990 to 2019: Systematic analysis for the global burden of Disease Study 2019. Front. Public. Health. 11, 1119374 (2023).
Tran, K. B. et al. The global burden of cancer attributable to risk factors, 2010–2019: A systematic analysis for the global burden of Disease Study 2019. Lancet 400(10352), 563–591 (2022).
Washoo, M. et al. Cigarette smoking and other risk factors for kidney cancer death in a Japanese population: Japan Collaborative Cohort Study for evaluation of Cancer Risk (JACC Study). Asian Pac. J. Cancer Prev. 14 (11), 6523–6528 (2013).
Kurasawa, S. et al. Association of kidney function with cancer incidence and its influence on the cancer risk of smoking: The Japan Multi-institutional Collaborative Cohort Study. Int. J. Cancer. 153(4), 732–741 (2023).
Huang, J. et al. A global trend analysis of kidney cancer incidence and mortality and their associations with smoking, alcohol consumption, and metabolic syndrome. Eur. Urol. Focus. 8(1), 200–209 (2022).
Bara, A. et al. The prognostic role of cigarette smoking in kidney cancer survival. Cancer Med. 12(13), 14756–14766 (2023).
Guo, K. et al. Association between chronic kidney disease and cancer, including the mortality of cancer patients: National health and nutrition examination survey 1999–2014. Am. J. Transl Res. 144, 2356–2366 (2022).
Asadzadeh Vostakolaei, F. et al. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur. J. Public. Health. 21(5), 573–577 (2011).
Choi, E. et al. Cancer mortality-to-incidence ratio as an indicator of cancer management outcomes in Organization for Economic Cooperation and Development countries. Epidemiol. Health, 39, (2017).
GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the global burden of Disease Study 2019. Lancet 396 (10258), 1160–1203 (2020).
Sun, M. et al. Age-adjusted incidence, mortality, and survival rates of stage-specific renal cell carcinoma in North America: a trend analysis. Eur. Urol. 59(1), 135–141 (2011).
Laguna, M. P. Re: international variations and trends in renal cell carcinoma incidence and mortality. J. Urol. 194(4), 950–951 (2015).
Wang, Z. et al. Burden of kidney cancer and attributed risk factors in China from 1990 to 2019. Front. Public. Health 10, 1062504 (2022).
Rizzuto, D. & Fratiglioni, L. Lifestyle factors related to mortality and survival: A mini-review. Gerontology 60(4), 327–335 (2014).
Haggstrom, C. et al. Metabolic factors associated with risk of renal cell carcinoma. PLoS One, 10(2), e0130147 (2015).
Hofmann, J. N. et al. Chronic kidney disease and risk of renal cell carcinoma: Differences by race. Epidemiology 26(1), 59–67 (2015).
Kuusk, T. et al. Impact of the first surge of the COVID-19 pandemic on a tertiary referral centre for kidney cancer. BJU Int. 128(6), 752–758 (2021).
Gross, O. et al. COVID-19-associated nephritis: Early warning for disease severity and complications? Lancet (London England) 395(10236), e87 (2020).
Gold, S. A. & Margulis, V. Uncovering a link between COVID-19 and renal cell carcinoma. Nat. Reviews Urol. 20(6), 330–331 (2023).
Martin, R. F., Robotic & Surgery Surg. Clin. North. Am., 100(2), xiii–xiv (2020).
Liu, J. et al. Identification of liver metastasis-associated genes in human colon carcinoma by mRNA profiling. Chin. J. Cancer Res. 30(6), 633 (2018).
Shemilt, R. et al. #5996 sex differences in the diagnosis of advanced cancer and subsequent outcome in people with CKD. Nephrol. Dial Transpl. 38(Suppl 1), gfad063c5996 (2023).
Mangone, L. et al. Trends in incidence and mortality of kidney cancer in a northern Italian province: An update to 2020. Biology 11(7), 1048 (2022).
Jani, C. et al. Examining trends in kidney cancer mortality by gender and race in the United States: A 20-year analysis. Oncologist 28(Suppl 1), S8–S9 (2023).
Beebe-Dimmer, J. L. et al. Body mass index and renal cell cancer: The influence of race and sex. Epidemiology 23(6), 821–828 (2012).
Asadzadeh Vostakolaei, F. et al. The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur. J. Public. Health. 21, 573–577 (2011).
Sugerman, P. B. & Savage, N. W. Oral cancer in Australia: 1983–1996. Aust Dent. J. 47(1), 45–56 (2002).
Wang, S. C. et al. The gender difference and mortality-to-incidence ratio relate to health care disparities in bladder cancer: National estimates from 33 countries. Sci. Rep. 7(1), 4360 (2017).
Adams, S. A. et al. Decreased cancer mortality-to-incidence ratios with increased accessibility of federally qualified health centers. J. Community Health 40(5), 933–941 (2015).
Sunkara, V. & Hebert, J. R. The colorectal cancer mortality-to-incidence ratio as an indicator of global cancer screening and care. Cancer 121(9), 1563–1569 (2015).
a, X. F. et al. The relationship between urologic cancer outcomes and national Human Development Index: trend in recent years. BMC Urol., 22(2), (2022).
Sung, W. W. et al. Favorable mortality-to-incidence ratios of kidney cancer are associated with advanced health care systems. BMC Cancer 18(1), 1–7 (2018).
Eisinger, F. Knowledge-based cancer control. Curr. Oncol. Rep. 20(Suppl 1), 19 (2018).
Acknowledgements
We express our gratitude for the remarkable contributions made by the Global Burden of diseases, injuries, and risk factors study 2021 team and the JD_GBDR study group.
Author information
Authors and Affiliations
Contributions
All authors wrote the main manuscript text. Jun Xiong is the corresponding author and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Public information were used and analyzed in this study, so no ethical approval was required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qiao, Z., Xiong, J., Zhang, S. et al. A comparative analysis of global and Chinese trends in the burden of kidney cancer from 1990 to 2021. Sci Rep 15, 4558 (2025). https://doi.org/10.1038/s41598-025-88682-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88682-1