Abstract
Urinary tract infections (UTIs) are prevalent; however, comprehensive and current epidemiological data remain scarce. This study examined the global, national, and regional burden of UTIs by sex, age, and socio-demographic index (SDI) from 1990 to 2021. The 2021 Global Burden of Disease study included age-standardised incidence rate (ASIR), age-standardised prevalence rate (ASPR), age-standardised death rate (ASDR), and age-standardised disability-adjusted life years rate (ASDAR). The estimated annual percentage change was used to depict temporal trends, whereas Pearson correlation analysis explore its correlation with the human development index (HDI), the SDI, and age-standardised rates (ASRs). An autoregressive integrated moving average model forecasted the UTI burden trends. From 1990 to 2021, the number of UTI cases increased by 66.45%, reaching 4.49 billion cases, with an ASIR of 5,531.88 per 100,000 population. The greatest incidence of UTIs was seen in women and older adult men. Tropical Latin America and low–middle SDI regions exhibited the highest ASIR, ASPR, ASDR, and ASDAR, while East Asia showed the lowest. ASDR and ASDAR decreased with higher SDI levels. ASR and HDI were weakly positively correlated with ASDR and ASDAR. ASIR, ASPR, and ASDAR are projected to increase until 2050. The global burden of UTIs is rising and is influenced by geographical location, age, sex, and economic development, crucial for guiding medical practices and forming relevant policies.
Similar content being viewed by others
Introduction
Urinary tract infections (UTIs) are highly prevalent in both community and healthcare-associated infections, with approximately 3 million individuals visiting health services for UTIs each year1. Severe UTIs can lead to renal failure and sepsis2,3. Although antibiotics remain the primary treatment for UTIs, they do not completely prevent recurrence and carry the risk of multidrug resistance4. Globally, it is estimated that there were 0.26 million deaths (95% uncertainty interval [UI]: 0.18–0.36) associated with bacterial antimicrobial resistance (AMR) in UTIs in 20195, imposing approximately $3.5 billion in annual societal costs6. UTIs lead to a significant economic burden and inconvenience in daily life, and increase psychological stress. Over 50% of patients with UTIs experience psychological issues such as anxiety and depression7,8. Therefore, UTIs pose an increasingly serious threat to public health.
Thus far, detailed information regarding the global burden of UTIs remains limited. A systematic review and meta-analysis9, encompassing 38 studies and 981,221 individuals worldwide, found that the incidence of UTIs varied from 1.1 to 3.7% across different regions. However, these studies primarily focused on developing countries, and differences in study design and sample size may have led to biased estimates of incidence rates, limiting their generalisability. Globally, owing to ageing populations and increasingly severe AMR, the total number of UTI cases increased to 404.6 million in 201910. To date, there is a lack of analyses of the epidemiological characteristics from the latest Global Burden of Disease (GBD) 2021 database. Furthermore, UTI incidence rates are closely related to the level of economic development; however, there is a lack of research examining the epidemiological changes of UTIs from this perspective. Such an analysis is crucial for formulating effective public health policies and evaluating their impact on regions and countries with different levels of economic development.
To the best of our knowledge, this study is the first to explore the correlation between economic development and UTIs, identify factors influencing the estimated annual percentage change (EAPC), and predict disease burden trends up to 2050 utilising data from the GBD 2021. The data are comprehensively analysed by sex, age, and socio-demographic index (SDI) regions to identify the main affected populations, which provides valuable insights into the prevention and treatment of UTIs and offers crucial guidance for global public health efforts.
Methods
Data source and study design
The present study leverages data from the Global Burden of Diseases, Injuries, and Risk Factors (GBD) 2021 study, which utilized the most recent epidemiological data and standardized methodologies to comprehensively assess health loss associated with 88 diseases, injuries, and conditions, along with 204 risk factors across 371 countries and regions11. Data for this analysis were sourced from the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool)11. The GBD study utilized a wide range of data sources, including population-based surveys, vital registration systems, and hospital discharge records12.
Study population and case definition
Specifically, urinary tract infections are defined as kidney infections capable of causing systemic symptoms, such as fever and weakness, potentially leading to discomfort and difficulty with daily activities. In addition, UTIs encompass pyelonephritis, cystitis, and urethritis11. The International Classification of Diseases, Tenth Revision (ICD-10) codes for UTIs are accessible via the following URL (http://ghdx.healthdata.org/record/ihme-data/gbd-2021-cause-icd-code-mappings). This study adhered to the Guidelines for Accurate and Transparent Health Estimates Reporting13. Ethical approval was not required for this research, as it utilized publicly available data from the GBD 2021 study.
Data collection and measurements
This study obtained relevant indicators for UTIs from the GBD 2021 database. The indicators included incidence, prevalence, deaths, and disability-adjusted life-years (DALYs).
Estimation methods
Multiple statistical models were employed to estimate the burden of UTIs using the GBD 2021 database. The Disease Modelling Bayesian Meta-Regression (DisMod-MR 2.1) tool was utilized to calculate incidence and prevalence rates11. Moreover, the Cause of Death Ensemble model was applied to estimate mortality rates with precision12. Disability-adjusted life-years (DALYs) were computed by combining years lived with disability and years of life lost, providing a comprehensive measure of disease burden14. Before analysis, the data underwent rigorous quality control and adjustment procedures to ensure accuracy and reliability15.
The GBD framework involves a systematic and comprehensive approach to disease burden estimation, incorporating diverse data sources, standardized methodologies, and advanced statistical modelling techniques to produce robust, comparable estimates of health loss across population and over time16,17.
Socio-demographic index
The SDI measures regional or national development levels, composed of three factors: per capita income, average level of education for individuals aged 15 years and above, and fertility rate of women aged under 25 years. The SDI value ranges from 0 to 1, with a higher value indicating a higher level of economic development. Based on their SDI values, all countries or regions were categorised into five SDI groups18.
Human development index
The human development index (HDI) is a composite index assessing a country’s overall strength, and can be obtained from the website of the World Bank (http://hdr.undp.org/en/content/human-development-index-hdi/). It is derived from three basic variables: gross national income per capita, education level, and life expectancy. The HDI score ranges from 0 to 1, with higher scores indicating higher levels of development19.
Statistics
The age-standardised rates (ASRs) of UTI incidence, prevalence, mortality, and DALYs were obtained from the GBD 2021, and were stratified by country, sex, age, and year. ASRs were calculated using the following formula:
,
where αi represents the age-specific rate in the ith age group, ωi represents the population size (or weight) in the corresponding ith age subgroup in the selected reference standard population, and (A) is the number of age groups20. Each step in the calculation process involved 1,000 iterations to generate 1,000 mean estimates, which were used to compute the final estimates. The 95% UIs were derived from the 25th and 975th values of these 1,000 estimates15. Regression models were used to calculate the EAPC21, and the calculation of the EAPC has been detailed in a previous study15. The EAPCs and their 95% confidence intervals (CI) were used to describe trends in standardised rates. If both the EAPC and the lower limit of the 95% CI were positive, the ASR indicated an upward trend. Conversely, if both the EAPC and the upper limit of the 95% CI were negative, the ASR indicated a downward trend; else, the ASR was considered stable. Hierarchical cluster analysis was performed to classify countries into clusters based on the EAPC of the ASRs, to identify similarities and differences in UTI burden trends among different countries22. Pearson correlation analysis was used to evaluate influencing factors of the EAPC, including the HDI, age-standardised incidence rate (ASIR), age-standardised prevalence rate (ASPR), age-standardised death rate (ASDR), and age-standardised DALYs rate (ASDAR)22. A p-value < 0.05 was considered significant. An autoregressive integrated moving average model was established to forecast the burden of UTIs from 2022 to 205023,24. The database construction, collation, analysis, and mapping were performed by using R (version 3.5.3) software (https://www.r-project.org/).
Results
Global burden
From 1990 to 2019, the global incidence of UTIs rose significantly, from 2,698,152,261 (95% UI: 241,706,586–299,288,509) to 4,491,022,288 (95% UI: 400,893,641–499,843,232) cases, marking a total growth of 1,792,870,027 (66.45%) cases. The ASIR for UTIs rose from 5,294.5 per 100,000 population (95% UI: 4,784.14–5,869.53) in 1990 to 5,531.88 per 100,000 population (95% UI: 4,965.44–6,161.01) in 2021, with an EAPC of 0.15 (95% CI 0.1–0.2) (Table 1, Supplementary Table S1, Additional File 1). In 2021, the prevalence of UTIs reached 8,560,676 cases (95% UI: 7,673,979–9,496,902), with an ASPR of 105.35 per 100,000 population (95% UI: 94.44–116.98). The EAPC for the ASPR was 0.15 (95% CI 0.1–0.19) (Table 1). The global number of deaths due to UTIs was 300,112 (95% UI: 267,926–324,216), representing a 190% increase from 1990. The ASDR was 3.71 per 100,000 population (95% UI: 3.31–4.01), with an EAPC of 1.02 (95% CI 0.95–1.1) (Table 1). The number of DALY cases and the ASDAR in 2021 were 6,848,127 (95% UI: 6,174,870–7,369,068) and 83.74 per 100,000 population (95% UI: 75.54–900.22), respectively, with an EAPC of 0.42 (95% CI 0.35–0.49) (Table 1). These indicate that the global burden of UTIs remained substantial in 2021.
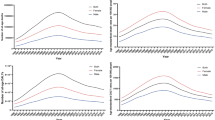
Burden of age and sex
From 1990 to 2021, the ASIR of UTIs increased in both men and women, with the ASIR in women being four times greater than that in men. However, the increase in men (EAPC: 0.32, 95% CI 0.24–0.41) was larger than that in women (EAPC: 0.1, 95% CI 0.06–0.15) (Table 1). In 2021, both the incident cases and ASIR were higher in women across different age groups, although peak ages varied between the sexes. For women, concentrated incidence rates were observed in the 30–34, 35–39, 40–44, and 45–49 age groups, while ≥ 80 years in men (Fig. 1A). Moreover, except for the < 5-year and 5–9-year age groups, the ASIR showed an upward trend across all other age groups, with the largest increase in those aged 90–94-year age group (Supplementary Table S2, Additional File 1). The trends in ASPR and the most affected age groups were consistent with those of the ASIR (Fig. 1B). Compared to 1990, the global number of deaths and the ASDR due to UTIs increased among both men and women in 2021. The number of female deaths surpassed that of male deaths, however, the ASDR was higher in men (3.93, 95% UI: 3.49–4.27) than in women (3.58, 95% UI: 3.11–3.95) (Table 1). Additionally, the ASDR increased with age, and it was significantly higher in older individuals (aged 80 years and above) than in the other age groups (Fig. 1C). In recent years, there has been little difference in the ASDAR between men and women, with women (85.17 per 100,000 in 2021) having a slightly higher rate than did men (83.29 per 100,000 in 2021) (Table 1). However, in the older population, the ASDAR in men was higher than that in women (Fig. 1D).
Burden of bacterial antimicrobial resistance
In 2021, we estimated that 287,200 deaths (95% UI: 253,980 − 320,471) were associated with bacterial AMR, including 67,467 deaths (95% UI: 57,720 − 77,214) directly attributable to bacterial AMR. Escherichia coli is the pathogen with the highest AMR-related mortality rate. Accounting for 125,492 (95% UI: 112,493 − 138,327) related deaths and 27,549.42 (95% UI: 32,347.97-31,750.86) attributable deaths. Klebsiella pneumoniae followed closely, with 40,494.56 (95% UI: 35,438.35-45,550.78) related deaths and 11,400.79 (95% UI: 9,685.02-13,116.56) attributable deaths (Supplementary Tables S3, Additional File 1). These two pathogens accounted for approximately 58% of all related deaths and 50% of all attributable deaths. Among the 21 GBD regions, tropical Latin America had the highest mortality rate, with 9.25 deaths per 100,000 people (95% UI: 7.96–10.53) associated with resistance and 2.04 deaths per 100,000 people (95% UI: 1.72–2.36) directly attributed to resistance. Southern Latin America followed with 7.34 deaths per 100,000 people (95% UI: 7.34–9.27) associated with resistance and 2.04 deaths per 100,000 people (95% UI: 1.59–2.09) directly attributed to resistance. Additionally, Eastern Europe, Central Latin America, and Western Europe also reported high mortality rates associated with AMR (Supplementary Tables S3, Additional File 1).
Regional and national level
SDI region level
The burden of UTIs worldwide is closely related to the SDI level. In 2021. The middle–low SDI region exhibited the highest ASIR, ASPR, ASDR, ASDAR, while the middle–high SDI region showed the lowest ASIR, ASPR and ASDR, and high SDI region had the lowest ASDAR (Table 1). Regarding the trend over three decades, the middle SDI, middle–low SDI and low SDI regions had a rising ASIR and ASPR, while other regions showed a decreasing trend (Fig. 2A,B). Among them, the most pronounced increase was observed in the middle-low SDI region, with an EAPC of 0.22 (95% CI 0.19–0.24), while the middle–high SDI region had the largest decrease, with an EAPC of −0.29 (95% CI −0.37 to 0.21) (Table 1). Regarding ASDR and ASDAR, all SDI regions except the low SDI region showed an upward trend, with the middle SDI region showing the most significant increase (Fig. 2C,D), with an EAPC of 1.6 (95% CI 1.49–1.72). The EAPC for ASDAR in the middle-high SDI region was the highest, at 0.86 (95% CI 0.74–0.98) (Table 1). It is worth noting that although the ASDAR in regions with low SDI has declined, it remains the second highest. Furthermore, by analysing the correlation between the estimated UTI burden and SDI levels in 204 geographical regions from 1990 to 2021, our study found that the ASDR and ASDAR of UTIs decreased overall with higher SDI levels; nevertheless, some fluctuations were observed (Supplementary Fig. S1, Additional File 2).
21 regions level
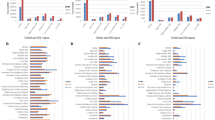
In 2021, Asia had the highest number of reported cases for incidence, prevalence, deaths, and DALYs (Supplementary Fig. S2B, Additional File 2). at 242,068,563 (95% UI: 213,881,727–270,940,840), 4,610,643 (95% UI: 4,094,504–5,153,965), 137,056 (95% UI: 117,692–150,885), and 3,616,403 (95% UI: 3,080,145–3,984,179), respectively (Supplementary Tables S4–S7, Additional File 1). However, tropical Latin America had the highest ASIR, ASPR, ASDR, and ASDAR (Supplementary Fig. S2A, Additional File 2), with rates of 13,021.38 (95% UI: 11,715.27–14,448.99), 248.35 (95% UI: 223.35–276.03), 11.74 (95% UI: 10.16–12.66), and 217.07 (95% UI: 198.1–229.94), respectively. In contrast, East Asia had the lowest ASRs, at 1,188.92 (95% UI: 1,062.4–1,335.12) for the ASIR, 22.61 (95% UI: 20.16–25.51) for the ASPR, 0.7 (95% UI: 0.57–0.94) for the ASDR, and 14.7 (95% UI: 11.52–18.71) for the ASDAR (Supplementary Tables S4–S7, Additional File 1). Regarding the ASIR and ASPR, Andean Latin America ranked second, with 12,329.29 cases per 100,000 population (95% UI: 10,545.34–13,972.53) and 234.98 cases per 100,000 population (95% UI: 201.52–263.81), respectively. The fastest growth was observed in Central Latin America, with an EAPC of 0.63 (95% CI 0.45–0.82) and 0.64 (95% CI 0.45–0.83) (Supplementary Tables S4 and S5, Additional File 1). Regions with high ASDRs included Southern Latin America, Latin America and Caribbean-WB, Eastern Sub-Saharan Africa, and Eastern Africa (Supplementary Table S6, Additional File 1). Regions with high ASDARs included Eastern Sub-Saharan Africa, Eastern Africa, Latin America and Caribbean-WB, and South Asia (Supplementary Table S7, Additional File 1). Southern Latin America experienced the fastest increases in both ASDR and ASDAR, with EAPCs of 5.37 (95% CI 4.71–6.04) and 6.69 (95% CI 5.82–7.58), respectively. Hierarchical cluster analysis of the EAPC for the ASRs revealed significant differences in disease burden trends across regions (Fig. 3): 20 regions showed significant decreases, 32 exhibited an increasing trend, with 21 experiencing minor increases and 11 significant increases, and only Tropical Latin America and Southern Latin America remained stable.
National trends
In 2021, Ecuador reported the highest ASIR (Fig. 4A) and ASPR (Fig. 4B) values, with an ASIR of 15136.7 per 100,000 population (95% UI: 12070.72-18311.87) and an ASPR of 239.28 per 100,000 population (95% UI: 225.21-291.69), respectively. In contrast, China had the lowest rates, with an ASIR of 1,184.13 (95% UI: 1,057.88–1,329.84) and an ASPR of 22.52 (95% UI: 20.1–25.41). Additionally, the most pronounced increase in the ASIR of UTIs was observed in Mexico (EAPC: 1.16, 95% CI 0.79–1.52), while Italy experienced the most significant decrease (EAPC: −2.36, 95% CI −2.91–1.81) (Supplementary Tables S8 and S9, Additional File 1). The rankings in terms of ASDR (Fig. 4C) and ASDAR (Fig. 4D) varied. The countries with the highest ASDR were Barbados (12.96 per 100,000 in 2021), Brazil (11.96 per 100,000 in 2021), and Uruguay (10.75 per 100,000 in 2021). The lowest ASDR was in Montenegro, at 0.16 cases per 100,000 population (95% UI: 0.12–0.2) (Supplementary Table S10, Additional File 1). Turkmenistan had the highest ASDAR, at 298.01 cases per 100,000 population (95% UI: 232.49–380.02), followed by Barbados and Ethiopia, while the Cook Islands had the lowest ASDAR, at 4.83 per 100,000 population (95% UI: 3.76–5.87) (Supplementary Table S11, Additional File 1). Over the past 30 years, the most notable increase in ASDR and ASDAR was observed in Argentina, while the most significant decrease was seen in Qatar (Supplementary Tables S10 and S11, Additional File 1).
Predictions of disease burden of UTI from 2022 to 2050
Based on the GBD 2021 study, the future global disease burden of UTIs from 2022 to 2050 was predicted. Compared to 2022, the global incidence rate, prevalence, and DALY rate of UTIs in 2050 were projected to show an upward trend (Fig. 5), reaching 6,486.39 per 100,000 population, 127.54 per 100,000 population, and 93.37 per 100,000 population, respectively. Similarly, we predicted a significant increase in the number of incident, prevalent, and DALY cases. By 2050, it is anticipated that there will be 652,793,817.2 incident cases, 12,463,119.89 prevalent cases, and 10,160,844.2 DALYs, representing an increase of 43.50%, 43.7%, and 44.92%, respectively. Notably, the mortality risk of patients with UTI is expected to remain relatively stable over the next 30 years. The number of deaths and the ASDR by 2050 were predicted at 297,057.391 and 3.76 cases per 100,000 population, respectively (Supplementary Table S12, Additional File 1).
Future forecasts of global burden of urinary tract infections. (A) Age-standardised prevalence rates; (B) Age-standardised incidence rates; (C) Age-standardised deaths rates; (D) Age-standardised DALYs rates; (E) Number of incidence cases; (F) Number of prevalence cases; (G) Number of deaths cases; (H) Number of DALYs cases.
Correlation of EAPC with ASR and HDI
We analysed the relationship between EAPC, ASR, and HDI across 204 countries and regions in 2021. Our findings revealed that in 2021, ASR was positively correlated with the EAPCs in ASDR (p < 0·01, P = 0·32) and ASDAR (p < 0·01, P = 0·24). However, no significant correlation was observed between the ASR and the EAPC in ASIR (p = 0·04, p = 0·14) and ASDR (p = 0·06, p = 0·13) (Fig. 6A). Similarly, HDI showed a weak positive correlation with the EAPC in ASDR (p < 0·01, p = 0·32) and ASDAR (p < 0·01, p = 0·24), but no significant correlation was identified with the EAPC in ASIR (p = 0·10, p = − 0·13) and ASPR (p = 0·09, p = − 0·13) (Fig. 6B).
Discussion
Based on the 2021 GBD data, this study comprehensively analysed the epidemiological characteristics and trends of UTIs across different regions. Globally, the ASIR, ASPR, ASDR, and ASDAR of UTIs have all increased, with women and older men being particularly vulnerable populations. Significant variations in disease burden trends exist among countries and regions, likely owing to differences in social development, economic levels, and environmental factors. Notably, regions with a medium–low SDI bear the heaviest disease burden, while medium–high SDI regions bear the lightest. Furthermore, both the ASDR and ASDAR decrease as the SDI level increases. The global incidence rate is projected to continue increasing until 2050, with an expected growth rate of 17.04%. These findings provide valuable information and data for addressing the global health challenges posed by UTIs.
The diagnosis of UTIs is typically based on clinical symptoms and laboratory test results. However, factors such as the difficulty in accurately expressing symptoms in children, the subtlety of symptoms in older adults, and patients’ self-medication without seeking medical attention can contribute to missed diagnoses. Additionally, imperfect monitoring systems in developing countries make it challenging to estimate the incidence of UTIs accurately25. According to a statistical report by Mengistu et al.9, the overall pooled incidence rate of UTIs was 1.6%, showing a decreasing trend over time, contrasting with the incidence rate and trend reported in a GBD study. This discrepancy may arise from the study’s limited scope, which included only 38 studies across 26 countries, leading to regional limitations and variations in the study population and period. Furthermore, the study by Mengistu et al. did not use the more accurate ASRs, affecting the precise estimation of the global disease burden. Additionally, UTI pathogens have shown a significant increase in antibiotic resistance, with highly diverse and strong resistance types26,27 contributing to the rising disease burden of UTIs. Previous research has shown that the ASIR and ASDAR of UTIs rank second and third28, respectively, among healthcare-associated infections, and fourth in deaths caused by bacterial AMR29. Epidemiological data are crucial for prevention, treatment, disease management, and the formulation of relevant health policies for patient care.
Owing to the unique physiological structure of women, UTIs are more common, particularly during menstruation, pregnancy, and menopause. According to the 2019 GBD data18, the highest incidence of UTIs was observed in women aged 25–35 years, a group more susceptible to factors such as sexual activity, lifestyle habits, and pregnancy. However, to some extent, UTIs can be prevented by changing certain behaviours. The latest 2021 GBD data revealed a shift in the high-incidence age group for women in the 40–49-year age group. This shift may be related to decreased oestrogen levels around menopause, thinning of the urethral mucosa, reduced keratinocyte numbers, and diminished self-cleaning ability of the vagina and urethra, all of which facilitate bacterial growth30.
From 1990 to 2021, the ASIR and ASPR of UTIs in women were consistently and significantly higher than those in men. Conversely, the ASDR in men exceeded that in women. Regarding ASDAR, men had higher rates than women did before 2012, although the rates have become comparable between the sexes since then. These findings suggest that the prognosis of men with UTIs may be worse than that of women. Studies31 indicate that men with UTIs often have histories of smoking, alcohol consumption, and being overweight, with the most common comorbidities being respiratory diseases, followed by dyslipidaemia and diabetes. Additionally, older adults’ lower tolerance to severe infections and propensity for multiple complications are high-risk factors for mortality. Furthermore, the burden of UTI in men increases with age, particularly in older men. Previous research32 has also noted that the incidence rate of UTIs in older men is similar to that in women, and is closely related to common comorbid prostate diseases, indwelling catheters, and prolonged hospital stays. However, in both men and women, it has been demonstrated that the older population remains a concern in terms of UTIs32. Previous studies have also shown that the increase in hospital admissions and the economic burden due to UTIs is mainly attributable to individuals over the age of 65 years33. This is related to multiple factors, such as ageing, chronic diseases, polypharmacy, and lifestyle habits.
In 2021, Tropical Latin America had the highest global ASRs of incidence, prevalence, and mortality for UTIs, and the disease burden in this region has not shown significant changes from 1990 to 2021. Ecuador had the highest ASIR globally, whereas Brazil ranked second in terms of ASIR, ASDR, incidence, and deaths. Despite its large population, China ranked fourth in the number of UTI cases but had the lowest incidence rate globally. This indicates that Latin America, represented by Brazil, has a relatively high disease burden. This may be attributable to the tropical climate of the region, which is hot and conducive to sweating. If hydration is not adequately maintained, urine tends to concentrate, creating a favourable environment for bacterial growth. Additionally, an increase in multidrug resistance significantly contributes to a higher disease burden. Among these 21 regions, Tropical Latin America ranked second in deaths related to UTIs and pyelonephritis associated with bacterial antibiotic resistance5. A study34 conducted in Brazil also highlighted that Proteus mirabilis isolated from patients with community-acquired UTI possesses multiple virulence factors and exhibits strong biofilm-forming abilities, correlating with antibiotic resistance.
The burden of UTIs varies across regions and countries with different SDI levels. Regions with low–medium SDI levels exhibit the highest incidence and prevalence rates. Over the past three decades, the incidence rate in these low–medium SDI regions has increased, while that in the high-SDI regions has declined. Economic development is closely linked to sanitary conditions and behavioural habits35,36, which are significant factors for UTIs. In Bangladesh37, being one of the lower–middle SDI countries, it has been reported that 80% of private tap water sources and most pond waters are contaminated with Escherichia coli, leading to a high UTI prevalence rate of 35.54%. In addition to having lower incidence rates, regions with medium–high SDI levels also show a lower ASDR and ASDAR attributable to UTIs. As socioeconomic levels improve, the reduction in UTI-related ASDR and ASDAR becomes more pronounced. Economic development often brings about improvements in sanitary conditions and advancements in medical technology, enabling timely, effective, and standardised treatments that reduce complications and adverse outcomes. Furthermore, it can enhance health education efforts to promote the adoption of healthy habits, thereby reducing the recurrence of UTIs.
This study had certain limitations. First, the data sources and quality of the GBD contained discrepancies in data collection, differences in diagnostic criteria, and variations in testing methods, all of which may affect the accurate assessment of disease burden. Second, countries with less-developed economies often have underdeveloped health regulatory systems and lack high-quality epidemiological studies, potentially leading to an underestimation of the actual disease burden. Finally, owing to the limitations of the GBD database, we could not explore the correlation between risk factors and UTIs or the epidemiological differences among various types of UTIs. These constraints suggest that the study results should be interpreted with caution, and that more precise data and analytical methods should be sought in future research.
Conclusions
This study revealed that from 1990 to 2021, the global burden of UTIs showed an overall upward trend, with a particularly pronounced disease burden among women, older men, and low–middle SDI regions. However, significant differences were observed across sexes, age groups, countries, regions, and SDI areas, indicating the need for targeted prevention and treatment strategies in specific populations and regions.
Data availability
The datasets supporting the conclusions of this article are available from the Global Health Data Exchange (GHDx) query tool, http://ghdx.healthdata.org/gbd-results-tool.
Abbreviations
- AMR:
-
Antimicrobial resistance
- ASIR:
-
Age-standardised incidence rate
- ASDAR:
-
Age-standardised disability-adjusted life years rate
- ASDR:
-
Age-standardised death rate
- ASPR:
-
Age-standardised prevalence rate
- ASR:
-
Age-standardised rate
- CI:
-
Confidence interval
- DALYs:
-
Disability-adjusted life-years
- EAPC:
-
Estimated annual percentage change
- GBD:
-
Global burden of disease
- HDI:
-
Human development index
- SDI:
-
Socio-demographic index
- UI:
-
Uncertainty interval
- UTI:
-
Urinary tract infection
References
Takhar, S. S. & Moran, G. J. Diagnosis and management of urinary tract infection in the emergency department and outpatient settings. Infect. Dis. Clin. North. Am. 28 (1), 33–48. https://doi.org/10.1016/j.idc.2013.10.003 (2014).
Bendall, M. J. A review of urinary tract infection in the elderly. J. Antimicrob. Chemother. 13 (Suppl B), 69–78. https://doi.org/10.1093/jac/13.suppl_b.69 (1984).
Shaifali, I., Gupta, U., Mahmood, S. E. & Ahmed, J. Antibiotic susceptibility patterns of urinary pathogens in female outpatients. N Am. J. Med. Sci. 4 (4), 163–169. https://doi.org/10.4103/1947-2714.9494 (2012).
Beerepoot, M. A. J. et al. Lactobacilli vs antibiotics to prevent urinary tract infections: a Randomized, Double-blind, Noninferiority Trial in Postmenopausal Women. Arch. Intern. Med. 172 (9), 704–712. https://doi.org/10.1001/archinternmed.2012.777 (2012).
Li, X. et al. Global and Regional Burden of bacterial antimicrobial resistance in urinary tract infections in 2019. J. Clin. Med. 11 (10), 2817. https://doi.org/10.3390/jcm11102817 (2022).
Flores-Mireles, A. L., Walker, J. N., Caparon, M. & Hultgren, S. J. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 13 (5), 269–284. https://doi.org/10.1038/nrmicro3432 (2015).
Coyne, K. S., Wein, A. J. & Tubaro, A. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 103 (Suppl 3), 4–11. https://doi.org/10.1111/j.1464-410X.2009.08371.x (2009).
Wagenlehner, F., Wullt, B., Ballarini, S., Zingg, D. & Naber, K. G. Social and economic burden of recurrent urinary tract infections and quality of life: a patient web-based study (GESPRIT). Expert Rev. Pharmacoeconomics Outcomes Res. 18 (1), 107–117. https://doi.org/10.1080/14737167.2017.1359543 (2018).
Mengistu, D. A. et al. Incidence of urinary tract infection among patients: systematic review and Meta-analysis. Inquiry 60, 469580231168746. https://doi.org/10.1177/00469580231168746 (2023).
Zeng, Z., Zhan, J., Zhang, K., Chen, H. & Cheng, S. Global, regional, and national burden of urinary tract infections from 1990 to 2019: an analysis of the global burden of disease study 2019. World J. Urol. 40 (3), 755–763. https://doi.org/10.1007/s00345-021-03913-0 (2022).
Qin, Y. et al. Global Burden and Trends in Incidence, Mortality, and Disability of Stomach Cancer From 1990 to 2017. Clin Transl Gastroenterol. ;12(10):e00406. Published 2021 Oct 5. (2021). https://doi.org/10.14309/ctg.0000000000000406
Murray, C. J. L. GBD 2021 collaborators. Findings from the global burden of Disease Study 2021. Lancet 403 (10440), 2259–2262. https://doi.org/10.1016/S0140-6736(24)00769-4 (2024).
Stevens, G. A. et al. Guidelines for Accurate and Transparent Health estimates reporting: the GATHER statement. Lancet 388 (10062), e19–e23. https://doi.org/10.1016/S0140-6736(16)30388-9 (2016).
GBD 2021 US Burden of Disease and Forecasting Collaborators. Burden of disease scenarios by state in the USA, 2022-50: a forecasting analysis for the global burden of Disease Study 2021. Lancet (London England). 404 (10469), 2341–2370. https://doi.org/10.1016/S0140-6736(24)02246-3 (2024).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet 396 (10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Chen, S. et al. Dynamic changes and future trend predictions of the global burden of anxiety disorders: analysis of 204 countries and regions from 1990 to 2021 and the impact of the COVID-19 pandemic. EClinicalMedicine 79, 103014. https://doi.org/10.1016/j.eclinm.2024.103014 (2024). Published 2024 Dec 27.
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133–2161. (2024). https://doi.org/10.1016/S0140-6736(24)00757-8
Zhu, C. et al. Epidemiological trends of urinary tract infections, urolithiasis and benign prostatic hyperplasia in 203 countries and territories from 1990 to 2019. Mil Med. Res. 8 (1), 64. https://doi.org/10.1186/s40779-021-00359-8 (2021).
Namayandeh, S. M., Khazaei, Z., Lari Najafi, M., Goodarzi, E. & Moslem, A. GLOBAL leukemia in children 0–14 statistics 2018, incidence and mortality and Human Development Index (HDI): GLOBOCAN sources and methods. Asian Pac. J. Cancer Prev. 21 (5), 1487–1494. https://doi.org/10.31557/APJCP.2020.21.5.1487 (2020).
GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1160–1203. (2020). https://doi.org/10.1016/S0140-6736(20)30977-6
Clegg, L. X., Hankey, B. F., Tiwari, R., Feuer, E. J. & Edwards, B. K. Estimating average annual per cent change in trend analysis. Stat. Med. 28 (29), 3670–3682. https://doi.org/10.1002/sim.3733 (2009).
Xu, Y. et al. Global trends and forecasts of breast cancer incidence and deaths. Sci. Data. 10 (1), 334. https://doi.org/10.1038/s41597-023-02253-5 (2023).
Vollset, S. E. et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the global burden of Disease Study. Lancet 396 (10258), 1285–1306. https://doi.org/10.1016/S0140-6736(20)30677-2 (2020).
Knoll, M. et al. An R package for an integrated evaluation of statistical approaches to cancer incidence projection. BMC Med. Res. Methodol. 20 (1), 257. https://doi.org/10.1186/s12874-020-01133-5 (2020).
Allegranzi, B. et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377 (9761), 228–241. https://doi.org/10.1016/S0140-6736(10)61458-4 (2011).
Mellano, E. M. et al. The role of chronic mesh infection in delayed-onset vaginal mesh complications or recurrent urinary tract infections: results from explanted mesh cultures. Female Pelvic Med. Reconstr. Surg. 22 (3), 166–171. https://doi.org/10.1097/SPV.0000000000000246 (2016).
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. (2022). https://doi.org/10.1016/S0140-6736(21)02724-0
Cassini, A. et al. Burden of six Healthcare-Associated infections on European Population Health: estimating incidence-based disability-adjusted life years through a Population prevalence-based Modelling Study. PLoS Med. 13 (10), e1002150. https://doi.org/10.1371/journal.pmed.1002150 (2016).
GBD 2019 Antimicrobial Resistance Collaborators. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022;400(10369):2221–2248. (2022). https://doi.org/10.1016/S0140-6736(22)02185-7
Raz, R. Postmenopausal women with recurrent UTI. Int. J. Antimicrob. Agents. 17 (4), 269–271. https://doi.org/10.1016/s0924-8579(00)00355-1 (2001).
Fernández-García, S. et al. Urinary tract infections in men in primary care in Catalonia, Spain. Antibiot. (Basel). 12 (11), 1611. https://doi.org/10.3390/antibiotics12111611 (2023).
Rowe, T. A. & Juthani-Mehta, M. Diagnosis and management of urinary tract infection in older adults. Infect. Dis. Clin. North. Am. 28 (1), 75–89. https://doi.org/10.1016/j.idc.2013.10.004 (2014).
Bardsley, M., Blunt, I., Davies, S. & Dixon, J. Is secondary preventive care improving? Observational study of 10-year trends in emergency admissions for conditions amenable to ambulatory care. BMJ Open. 3 (1), e002007. https://doi.org/10.1136/bmjopen-2012-002007 (2013).
Danilo de Oliveira, W. et al. Virulence, resistance and clonality of Proteus mirabilis isolated from patients with community-acquired urinary tract infection (CA-UTI) in Brazil. Microb. Pathog. 152, 104642. https://doi.org/10.1016/j.micpath.2020.104642 (2021).
Andersen, L. & Dowdell, E. B. Access to clean water and urinary tract infections in Haitian women. Public. Health Nurs. 36 (6), 800–805. https://doi.org/10.1111/phn.12660 (2019).
Graham, J. P., Amato, H. K., Mendizabal-Cabrera, R., Alvarez, D. & Ramay, B. M. Waterborne urinary tract infections: have we overlooked an important source of exposure? Am. J. Trop. Med. Hyg. 105 (1), 12–17. https://doi.org/10.4269/ajtmh.20-1271 (2021).
Sarkar, P. et al. Self-reported urinary tract infection and bacterial vaginosis symptoms among indigenous adolescents during seasonal periods of water scarcity: a cross‐sectional study in Bandarban Hill District of Bangladesh. Health Sci. Rep. 7 (5), e2107. https://doi.org/10.1002/hsr2.2107 (2024).
Acknowledgements
We extend our gratitude to the contributors of the 2021 Global Burden of Diseases, Injuries, and Risk Factors Study for their invaluable work. We also express our sincere appreciation to the Institute for Health Metrics and Evaluation (IHME) for making the GBD data available for this research.
Funding
This work was sponsored by the Jiangsu Provincial Medical Innovation Center (No. 202215), the Postgraduate Research and Practice Innovation Program of Jiangsu Province (SJCX23_0907, SJCX24_1009), and Research Project of Jiangsu Provincial Maternal and Child Health Care Association (FYX202308).
Author information
Authors and Affiliations
Contributions
Conceptualisation, YH, JZ, XZ, and WH; methodology, YH and JZ; software, LW, RY, and PZ; data curation, YH and CH; formal analysis, YH and JZ; original draft preparation, review, and editing, YH, JZ, XZ, and WH; visualisation, LW, TQ, and SY; funding acquisition, YH, RY, and WH. All the authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study did not require ethical approval or consent as it utilised available data from the GBD 2021 study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, Y., Zhao, J., Wang, L. et al. Epidemiological trends and predictions of urinary tract infections in the global burden of disease study 2021. Sci Rep 15, 4702 (2025). https://doi.org/10.1038/s41598-025-89240-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89240-5
Keywords
This article is cited by
-
Global, regional, and national lifetime probabilities of urinary tract infections and interstitial nephritis from 1990 to 2021
Journal of Health, Population and Nutrition (2025)
-
Gepotidacin: First Approval
Drugs (2025)