Abstract
Disaster-related deaths can be classified as direct and indirect disaster-related deaths that are becoming more predominant in Japan. To reduce indirect disaster-related deaths, accurate statistics based on medical documentation are essential. However, the definition and reporting of such deaths in Japan present systemic challenges. These deaths are certified and recorded by municipalities at the request of bereaved families seeking condolence grants. This cross-sectional study assessed 755 certified indirect disaster-related deaths after the 2011 Great East Japan Earthquake in the Miyagi Prefecture, Japan, to determine whether medical documents mentioned disaster relevance. Of the 755 cases, 74 (9.8%) death certificates and 145 (19.2%) medical documents described the relevance of disasters. Relevance mentioned only in the self-reported documentation from bereaved families was 536 (71.0%). The median [interquartile range] time from the disaster onset to disaster-related deaths was 21 [7–52] days. The mean age was 79.7-years-old, and 346 (46.7%) of the victims were female. The predominant etiologies of these deaths included circulatory (32.7%) and respiratory (27.7%) diseases. The time periods of the deaths varied among the municipalities, suggesting a lack of consensus among the review committees. Establishing a medical and social consensus for indirect disaster-related deaths and recording them on death certificates is crucial for accurate disaster death data and social resilience.
Similar content being viewed by others
Introduction
To reduce disaster-related deaths, identifying the medically accurate etiology of the death through diagnosis and documentation is imperative1,2. Disaster-related deaths can be broadly classified as direct or indire1 Direct disaster-related deaths are caused by the direct physical impact of hazards, including deaths resulting from crush injuries during earthquakes3, drownings during tsunamis4, and viral pneumonia during pandemics, such as coronavirus disease 2019 (COVID-19)5. Direct deaths, which are the direct consequence of the hazard, can be reduced by disaster risk reduction (DRR), such as early warning systems and seismic-proof buildings if the hazard is an earthquake. By contrast, indirect disaster-related deaths are caused by secondary health effects, including emergency evacuations, relocations, evacuation environments, delays in accessing healthcare, and psychosocial effects5,6,7,8,9. Indirect disaster-related deaths occurring days, weeks, months, and years later due to the health impact of the disaster are becoming more predominant in Japan, where DRR has been implemented. Regardless of the hazard types, there are common health impacts and the potential to prevent indirect disaster-related deaths, making efforts to mitigate them essential6. Tsuboi et al. reported similarities in indirect disaster-related deaths between the 2011 Fukushima Daiichi Nuclear Power Plant (FDNPP) accident in the Great East Japan Earthquake (GEJE) and the 2019 COVID-19 pandemic10. Furthermore, Woolf et al. reported that the increase in the number deaths in the United States (US) during the COVID-19 pandemic was primarily driven by disruptions to healthcare services and widespread societal impacts11.
Japanese Cabinet Office officially defines indirect disaster-related deaths as “deaths because of aggravation of injuries caused by the disaster or illnesses caused by physical burden, such as that of living in evacuation shelters, which are recognized as being caused by the disaster based on the Act on Provision of Disaster Condolence Grant (1973 Law No. 82)"12. Historically, the 1967 Uetsu torrential rain disaster resulted in the creation of a Disaster Condolence Grant System to provide relief to the bereaved families of disaster victims due to direct deaths13. After the 1995 Great Hanshin-Awaji Earthquake (GHAE) the concept of indirect disaster-related deaths became eligible for condolence grants1.
Since then, indirect disaster-related deaths have become a significant social issue, including those after the 2011 GEJE. As of March 31, 2022 (ten years after the onset), 3789 people were officially certified as indirect disaster-related deaths among the 22,214 fatalities (Table 1)14,15. After GEJE, 2372 individuals died within 6 months of the disaster, representing 62.6% of the total number. In contrast, 1417 individuals died after 6 months, accounting for 37.4% of the cases. Respiratory and cardiovascular diseases together were the primary direct causes of nearly half of the indirect disaster-related deaths16. The FDNPP accident further led to chaotic evacuations and healthcare system disruptions, significantly increasing morbidity and mortality17. According to the Reconstruction Agency, factors contributing to indirect disaster-related deaths in Fukushima Prefecture included physical and mental fatigue from living in evacuation shelters (30%), physical and mental fatigue during evacuation to shelters (30%), and delays in initial treatment caused by the dysfunction of hospital facilities (20%)18.
In Japan, bereaved families must apply for condolence grants in their respective municipalities, and the review committee, consisting of municipal officers, medical doctors, and lawyers, certifies these deaths as indirect disaster-related deaths. The cumulative data had served as the sole source of indirect disaster-related death statistics in Japan. On the other hand, the Centers for Disease Control and Prevention (CDC) in the US emphasizes recording the relevance of disasters on death certificates including the disaster types8. The CDC defines indirect disaster-related deaths as those caused by the unsafe or unhealthy disruption of usual services, personal losses, and disruptions of individuals’ lifestyles2,7,8. The condolence grant can be issued based on these death certificates. In this context, no prior studies have quantitatively examined how certification documents, the basis of Japan’s indirect disaster-related death data, reflect medical opinions.
This study aimed to explore the extent to which death certificates and medical documents describe the relevance of a disaster after the GEJE in Miyagi Prefecture, Japan, because no such study has been conducted. Additionally, this study sought to promote social consensus on the definition and reporting of indirect disaster-related deaths for accurate statistics and reduce its occurrence after future disasters.
Methods
Ethical considerations
This study was approved by the Ethics Committee of the Tohoku University Graduate School of Medicine (approval no: 2023-1-489). The committee waived the requirement for obtaining informed consent from the victims or their families, as the administrative documentation used had been anonymized prior to disclosure. This study was conducted in accordance with the principles outlined in the Declaration of Helsinki.
Study design and settings
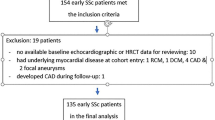
This retrospective, cross-sectional study was conducted using anonymized documentation regarding indirect disaster-related deaths from the Miyagi Prefecture following the 2011 GEJE. The study adhered to the official definition of indirect disaster-related deaths officially outlined by Japan. The study areas are presented in Fig. 1. Cases from Sendai, Ishinomaki, Tagajo, Kesennuma, Natori, Iwanuma, and Watari were reviewed by individual municipal committees, while cases from Minamisanriku, Matsushima, Shichigahama, Misato, Tome, Kurihara, Tomiya, Osaki, and Rifu were evaluated by the Prefectural Joint Review Committee.
Locations of the surveyed municipalities in the Miyagi Prefecture are presented. Sendai, Ishinomaki, Tagajo, Kesennuma, Natori, Iwanuma, and Watari, where cases have been examined by individual municipalities, are shown in light green. Minamisanriku, Matsushima, Shichigahama, Misato, Tome, Kurihara, Tomiya, Osaki, and Rifu, where the cases have been examined by the Prefectural Joint Review Committee, are in dark green. The maps have been created using Adobe Illustrator 2020 (Adobe Inc., Version 24.0, https://www.adobe.com/products/illustrator.html) and Microsoft PowerPoint (Microsoft, Version 16.0, https://www.microsoft.com/powerpoint) during this study and have not been taken/modified from any copyrighted sources.
The municipalities and prefectural governments provided the following anonymized documents: application forms, death certificates, medical reports, and self-reports from bereaved families. The author (MT) requested these administrative documents from the municipalities where individual committees examined the cases. Additionally, the International Research Institute of Disaster Science (IRIDeS) requested documents from the Miyagi Prefectural government, which managed cases reviewed by the Joint Committee as of July 29, 2023.
In this study, death certificates, official medical documents such as insurance applications other than daily medical records, and self-reports by bereaved families were systematically screened to determine whether they contained any description of relevance to the disaster or post-disaster change of life. The types of documents used to certify indirect disaster-related deaths were categorized into three groups: Group A in which the death certificates mentioned disaster relevance; Group B where official medical documentation other than death certificates mentioned disaster relevance; and Group C with non-medical self-reports from bereaved families claiming disaster relevance. Non-certified deaths and cases with insufficient evidence due to document redactions were excluded from the analysis.
Correlation between the time of the death and type of documentation
A Steel–Dwass multiple comparison test was conducted for each group to investigate the correlation between the time from the disaster onset to the death; in addition to the type of medical documentation used for certification of indirect disaster-related deaths. The periods of deaths were divided into three subgroups: short-term (30 days after the earthquake), medium-term (31–180 days after the earthquake), and long-term (≥ 181 days after the earthquake). The correlation between the time period of death and type of evidence of medical documentation was analyzed using descriptive statistics.
Statistical analyses
Regarding the victims’ baseline characteristics, categorical data were expressed as n (%); and continuous data were expressed as means and standard deviations (SDs), when normally distributed. When the data did not follow a normal distribution, continuous data were expressed as medians [IQRs]. The etiologies of the deaths were classified according to the International Classification of Diseases, 10th Revision (ICD-10) codes26.
The differences in the time from the disasters to deaths among the municipalities have been presented as scatter plots. When a normal distribution could not be assumed, statistical significance testing was conducted by log-transforming the outcomes and performing a one-way analysis of variance (ANOVA). A sample size calculation was not performed, because all available data were utilized in this study. Data were analyzed using JMP 16 software (SAS Institute Inc., Cary, North Carolina, USA). Statistical significance was set at P < 0.05. All tests were two-sided.
Results
Baseline characteristics of the victims
The anonymized disaster-related deaths database in the Miyagi Prefecture included 755 victims who met the inclusion criteria. Table 2 presents the baseline characteristics of the victims. The mean age of this study population was 79.7 years, and 346 of the victims were female (46.7%). The municipalities in which disaster-related death certification review committees were convened are listed in Table 2. In particular, Sendai (35.1%) and Ishinomaki (34.8%) accounted for most of the cases of indirect disaster-related deaths. The Miyagi Joint Review Committee accounted for 4.9% of all cases of indirect disaster-related deaths. The median time from disaster onset to death was 21 [7–52] days. Regarding the type of documentation, relevance was mentioned in death certificates of 74 (9.8%) victims (Group A) and in the other official medical documentation of 145 (19.2%) victims (Group B). Regarding the remaining 536 victims, relevance was mentioned only in the self-report documentation of bereaved families (Group C). Analysis of the etiologies of the deaths revealed that the most frequent etiology of the deaths included circulatory diseases (I00–I99) in 247 (32.7%) victims. Following this was respiratory diseases (J00–J99); symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99); and neoplasms (C00–D48) in 209 (27.7%), 71 (9.4%), and 66 (8.7%) of the victims, respectively.
As presented in Fig. 2, the median times [IQR] to deaths were 12 [3–30] 31 [10–80], 21 [8–50] days for Groups A, B, and C, respectively. A statistically significant difference was present among all groups regarding the time from the disaster onset to the death.
Figure 3 presents the proportions of documentation types according to the period of indirect disaster-related deaths. Death certificates indicating relevance by a medical doctor for Group A were available in 12.4% of cases for the short-term period. The proportion of death certificates for Group A decreased further during the medium-to-long term period. While the absolute numbers of evidence indicating the relevance by medical documentation for Group B decreased in the medium-to-long term, their proportions increased at 15.0%, 21.9%, and 52.9% in the short -, medium -, and long-term periods, respectively.
Figure 4 reveals that the time from disaster onset to death varied significantly among municipalities where review committees were held (P = 0.046). The mean time from the disaster onset to the death was the longest in Natori at 108.3 days. By contrast, the mean time from the disaster onset to the death was shortest at 28.3 days for Watari. In several municipalities, victims were certified as disaster-related deaths more than 6 months after the disaster onset. The maximum certification periods also varied across municipalities and committees: 680 days in Natori, 201 days in Iwanuma, 1207 days in Tagajo, 1225 days in Ishinomaki, 893 days in Kesennuma, 433 days in Sendai, and 601 days for the Miyagi Joint Review Committee.
Differences in the time periods from the disaster onset to the deaths among the municipalities are shown. The figure reveals both the arithmetic mean (standard deviation [SD]) and geometric mean (SD). The blue horizontal line represents the mean values. The light blue shading indicates a 95% confidence interval. *P-values have been calculated using the analysis of variance for log-transformed outcomes.
Discussion
This study is the first in Japan to explore the extent to which official death certificates detailing the relevance to a disaster within the certification documents for indirect disaster-related deaths. Our study revealed three substantial findings.
First, many officially recognized indirect disaster-related deaths lacked sufficient documentation of disaster-relatedness in death certificates or other official medical documents. This suggests that the reporting system for indirect disaster-related deaths in Japan may be insufficient from a medical perspective based on death certificates. Similarly, underreporting of indirect disaster-related deaths has also been identified in the US, particularly in relation to Hurricane Katrina27. To address this issue, the American National Association of Medical Examiners recommends the documentation of disaster-relatedness in death certificates and emphasizes the importance of training medical professionals2. Furthermore, the CDC highlights the critical role of death certificates in disasters, not only to provide accurate data for disaster management but also to support the resilience of affected families. Accurate documentation allows families to apply for disaster relief funds from FEMA8. In Japan, however, despite the essential role of death certificates in mortality statistics, systematic documentation of disaster-relevance is lacking1,28. This gap reflects structural problems in Japan’s disaster mortality statistics, indicating that the lack of accurate medical data on indirect disaster-related deaths poses a significant challenge for improving disaster response measures1,7. Thus, it is imperative to establish a medical definition and a reporting system for indirect disaster-related deaths. This new system should complement the existing administrative definition and be built on data collected from official medical records. Failure to incorporate medical perspectives into the recognition process for indirect disaster-related deaths may result in significant discrepancies in the reported figures. The current reporting system relies on the condolence grant program and does not necessarily align with medical definitions1,29. While the condolence grant program is a legally established and vital system for bereaved families, insufficient documentation of medical disaster-relatedness raises societal concerns about families potentially losing access to these grants. Therefore, revisions to the system must involve the formation of social consensus and ensure the rights of bereaved families1,16,29.
Second, this study focused on the complex relationship between the timing of death after a disaster and the type of medical documentation. As shown in Figs. 2 and 3, the frequency of documenting disaster-relevance in death certificates decreased over time. However, indirect disaster-related deaths can occur long after the disaster onset2,8. Physicians signing death certificates must always consider the impact of disaster-related experiences on the causes of death and document this when necessary. Historical precedents include the Nagaoka criteria established after the 2004 Niigata Chuetsu Earthquake, which classified 52 out of 64 deaths as indirect disaster-related deaths based on specific timelines as follows:
-
(1)
Deaths within 1 week of the disaster were considered indirect disaster-related deaths.
-
(2)
Deaths within 1 month were highly likely to be indirect disaster-related deaths.
-
(3)
Deaths exceeding 1 month had a lower likelihood of being disaster-related.
-
(4)
Deaths after 6 months were not considered disaster-related.
However, these criteria did not meet the expectations of bereaved families after the GEJE, as most disaster-related deaths following the FDNPP accident occurred more than 6 months post-disaster1,14,30,31. Furthermore, the CDC has emphasized that the diagnosis of indirect disaster-related deaths should not be limited by the time elapsed since the disaster8. These findings suggest the need for flexible criteria that consider individual circumstances and the specific characteristics of disasters.
Third, this study revealed significant differences in the recognition periods for indirect disaster-related deaths among municipalities. These differences may result from variations in geographic and social factors1. Other challenges include differences in disaster circumstances, application processes, information accessibility, and petition formats across municipalities, which may influence recognition outcomes32,33. The lack of standardized recognition methods and variations in medical documentation further complicate the process. Addressing these issues requires the establishment of objective and equitable diagnostic criteria and reporting systems to obtain accurate statistics on indirect disaster-related deaths. Such a system would enhance the understanding of disaster impacts and facilitate the development of effective disaster response strategies.
This study provides a comprehensive overview of indirect disaster-related deaths of a wide area of municipalities affected by the GEJE, including multiple regions in Miyagi Prefecture. Indirect disaster-related deaths predominantly occurred among older adults, with approximately half of them attributed to cardiovascular and respiratory diseases, aligning with findings from other regions affected by the GEJE16,33,34,35,36. Previous research on the relationship between indirect disaster-related deaths and long-term care certification found that individuals with long-term care certification were more likely to die from cardiovascular or respiratory diseases during the acute phase of a disaster, while those without certification were more likely to die from malignant diseases during the later phase26. Additionally, analyses of mortality typologies revealed that individuals who were at home at the time of the earthquake exhibited higher mortality rates from cardiovascular diseases and malignancies, accounting for approximately half of all deaths. Conversely, those in hospitals or facilities at the time of the earthquake showed higher mortality rates from respiratory diseases and senility, comprising one-third of all deaths26. Furthermore, specific vulnerable groups, including individuals with disabilities, those requiring long-term care, and individuals with depression, exhibited unique characteristics. These findings emphasize the need for tailored post-disaster support that addresses the specific needs of each group rather than adopting uniform support measures26. From a disaster preparedness perspective, evacuation planning and support strategies must be strengthened, particularly for vulnerable populations such as older adults and individuals with disabilities26,37,38. Improving evacuation shelter environments remains a critical priority to address leading causes of death, such as cardiovascular and respiratory diseases5,39. Notably, approximately half of all indirect disaster-related deaths occurred at home40. This finding highlights delays in medical support for home evacuees, who are less likely to receive adequate assistance compared to those in evacuation shelters. To reduce indirect disaster-related deaths, proactive outreach efforts and primary care interventions are essential for home evacuees40. Indirect disaster-related deaths due to malignant tumors have been noted, suggesting delays in cancer screening and interruptions in treatment following earthquakes35,36,41. While most deaths occurred within 1 month of the disaster, fatalities were observed up to 4 years later. In Fukushima, such deaths continued to be recorded even a decade after the disaster14. Identifying causal links for chronic-phase deaths remains challenging due to factors such as hospital closures and the exacerbation of health conditions caused by environmental changes and stress during evacuation42. These findings underscore the importance of implementing medium- to long-term strategies. Efforts to diagnose and document indirect disaster-related deaths based on medical perspectives and to integrate these findings into emergency medical responses are crucial for reducing disaster-related mortality. Such measures are expected to enhance resilience to future disasters while addressing the unique vulnerabilities of at-risk populations43,44,45.
This study had some limitations. First, it was retrospective in nature. Second, the study relied on death certificates submitted by bereaved families to the local government’s Disaster Condolence Grants Review Committee, introducing a risk of selection bias. This limitation highlights the potential for underestimation of indirect disaster-related deaths, as cases where families did not apply for disaster condolence grants, for any reason, were excluded. Currently, data on indirect disaster-related deaths in Japan rely solely on cases that have received disaster condolence grants, which may not comprehensively reflect the actual number of such deaths. Third, when the time elapsed between the disaster and occurrence of death extends to the medium or long term, repeated environmental changes following the disaster make the establishment of a causal relationship between death and disaster scientifically challenging. Fourth, information bias may have occurred during the certification process, as disaster-relatedness on death certificates was recorded by certifiers. Fifth, while this study attempted to minimize bias by including a diverse range of municipalities within Miyagi Prefecture, its focus on specific regions in Japan may limit external validity. However, it is important to note that only a few countries have institutional frameworks for reporting indirect disaster-related deaths. As aging populations become a global challenge, insights gained from Japan’s experience may serve as valuable guide for other countries likely to face similar issues in the future. Sixth, as a cross-sectional study, it could not rule out reverse causation. Seventh, this study employed univariate analysis, meaning that confounding factors such as socioeconomic status, medical history, and lifestyle may have influenced the results. Eighth, the documents provided by local governments were anonymized for ethical reasons, resulting in partial uncertainty regarding victim information. This missing data may have led to either an overestimation or underestimation of the study results.
Definitively, in this study, we investigated the indirect disaster-related deaths in multiple municipalities across the Miyagi Prefecture after the GEJE. Surveillance of medical diagnostic documentation revealed the minimal recording of disaster relevance on death certificates. Moreover, a lack of consensus existed regarding indirect disaster-related deaths among the different regions. This study emphasized the importance of recording disaster relevance on death certificates. In addition, the requisite to develop a consensus regarding indirect disaster-related deaths in Japan through broad medical and social discussions was highlighted. This approach will enable evidence-based emergency response and social resilience, particularly for vulnerable populations.
Data availability
The administrative documentation is not publicly available due to ethical restrictions. The summarized data for interpretation are available upon reasonable request from corresponding author Motohiro Tsuboi (tsuboi.motohiro.r8@dc.tohoku.ac.jp).
References
Tsuboi, M. et al. Disaster-related deaths after the Fukushima Daiichi nuclear power plant accident: Definition of the term and lessons learned. Environ. Adv. https://doi.org/10.1016/j.envadv.2022.100248 (2022).
Utley, S. et al. National Association of Medical Examiners position paper: Recommendations for the documentation and certification of disaster-related deaths. Am. J. Forensic Med. Pathol. 44, 80–90 (2023).
Buyurgan, Ç. S. et al. Demographic and clinical characteristics of earthquake victims presented to the emergency department with and without crush injury upon the 2023 Kahramanmaras (Turkey) earthquake. Prehosp. Disaster Med. 38, 707–715 (2023).
Zheng, X., Feng, C. & Ishiwatari, M. Examining the indirect death surveillance system of the great East Japan earthquake and tsunami. Int. J. Environ. Res. Public Health 19, 12351 (2022).
Tsuboi, M. et al. Comparison of mortality patterns after the Fukushima Daiichi Nuclear Power Plant radiation disaster and during the COVID-19 pandemic. J. Radiol. Prot. 42, 031502 (2022).
Yamanouchi, S. et al. Survey of preventable disaster deaths at medical institutions in areas affected by the Great East Japan Earthquake: Retrospective survey of medical institutions in Miyagi Prefecture. Prehosp. Disaster Med. 32, 515–522 (2017).
Combs, D. L., Quenemoen, L. E., Parrish, R. G. & Davis, J. H. Assessing disaster-attributed mortality: Development and application of a definition and classification matrix. Int. J. Epidemiol. 28, 1124–1129 (1999).
National Center for Health Statistics. A Reference Guide for Certification of Deaths in the Event of a Natural, Human-Induced, or Chemical/Radiological Disasters. https://stacks.cdc.gov/view/cdc/49294. (2017).
Zhao, T. & Tsubokura, M. Risks associated with evacuation and disaster-related death after a radiation disaster: Summary of research results from Hamadori region, Fukushima. Radiat. Prot. Dosimetry. 200, 1524–1527 (2024).
Tsuboi, M. et al. Indirect disaster-related deaths: A comparison between the Fukushima Daiichi Nuclear Power Plant accident and the COVID-19 pandemic. J. Radiol. Prot. 42, 031502 (2022).
Woolf, S. H., Chapman, D. A. & Lee, J. H. COVID-19 as the leading cause of death in the United States. JAMA. 325, 123–124 (2021).
Cabinet Office of Japan. Disaster-Related Deaths [in Japanese], https://www.bousai.go.jp/taisaku/kyuujo/pdf/r01kaigi/siryo8.pdf. (2022).
Cabinet Office of Japan. Act. on Provision of Disaster Condolence Grant [in Japanese]. https://elaws.e-gov.go.jp/document?lawid=348AC0100000082. (1973).
Cabinet Office of Japan. Number of Earthquake-Related Deaths in the Great East Japan Earthquake [in Japanese]. https://www.reconstruction.go.jp/topics/main-cat2/sub-cat2-6/20220630_kanrenshi.pdf. (2022).
The National Police Agency of Japan. Ten Years Since the Great East Japan Earthquake [in Japanese]. https://www.npa.go.jp/hakusyo/r03/honbun/html/xf111000.html. (2021).
Tsuboi, M. et al. Analysis of disaster-related deaths in the Great East Japan Earthquake: A retrospective observational study using data from Ishinomaki city, Miyagi, Japan. Int. J. Environ. Res. Public Health. 19, 4087 (2022).
Tanigawa, K., Hosoi, Y., Hirohashi, N., Iwasaki, Y. & Kamiya, K. Loss of life after evacuation: Lessons learned from the Fukushima accident. Lancet. 379, 889–891 (2012).
Japan Reconstruction Agency. Report on Disaster-Related Deaths in the Great East Japan Earthquake [in Japanese]. https://www.reconstruction.go.jp/topics/20120821_shinsaikanrenshihoukoku.pdf. (2012).
Cabinet Office of Japan. Overview of the Great Hanshin-Awaji Earthquake and Damage [in Japanese]. https://www.bousai.go.jp/kyoiku/kyokun/pdf/101.pdf. (2000).
Niigata Prefecture. Record of the Great Niigata Chuetsu Earthquake [in Japanese]. https://www.pref.niigata.lg.jp/sec/dobokukanri/1300136465340.html. (2019).
Kumamoto Prefecture. Damage Situation regarding the Kumamoto Earthquake in 2008 [in Japanese] https://www.pref.kumamoto.jp/uploaded/attachment/209778.pdf. (2023).
Mainichi newspapers. 83 People in Hiroshima, Okayama, Ehime Recognized as "Disaster-Related Deaths" 5 Years after Torrential Rains in Western Japan [in Japanese]. https://mainichi.jp/articles/20230705/k00/00m/040/278000c. (2023).
Cabinet Office of Japan. Damage from the 2008 Hokkaido Bombei East Japan earthquake [in Japanese]. https://www.bousai.go.jp/updates/h30jishin_hokkaido/index.html. (2019).
Cabinet Office of Japan. Damage Typhoon 19 in 2028, etc. [in Japanese]. https://www.bousai.go.jp/updates/r1typhoon19/pdf/r1typhoon19_45.pdf. (2020).
Ishikawa Prefectural Government. Report on Disaster Damage in Ishikawa Prefecture [in Japanese]. https://www.pref.ishikawa.lg.jp/saigai/documents/higaihou_181_1227_1600.pdf. (2023).
Yoshimura, H. et al. Categorization of disaster-related deaths in Minamisoma city after the Fukushima nuclear disaster using clustering analysis. Sci. Rep. 14, 2946 (2024).
Noe, R. Applications: Disaster-Related Mortality Surveillance: Challenges and Considerations for Local and state health departments. https://www.sciencedirect.com/science/article/abs/pii/B9780128093184000071. (2018).
World Health Organization. Medical Certification of Cause of Death: Instructions for Physicians on Use of International Form of Medical Certificate of Cause of Death, 4th ed. https://iris.who.int/handle/10665/40557. (1979).
Tsuboi, M. et al. Symposium on disaster-related deaths after the Fukushima Daiichi Nuclear Power Plant accident. J. Radiol. Prot. 42, 033502 (2022).
Ichiseki, H. Features of disaster-related deaths after the Great East Japan Earthquake. Lancet 381, 204 (2013).
Yamamura, M. et al. Disaster-related deaths: Interpretation as an indicator of the medium-to-long-term impact of disaster and its caveats. J. Glob. Health. 14, 03030 (2024).
Okamoto, T. The Necessity of Providing Reconstruction Information by Professionals Such as Legal Experts [in Japanese]. https://www.f-gakkai.net/wp-content/uploads/2014/10/11-1-2.pdf. (2014).
Uchi, Y. et al. Features of causes of indirect certified disaster-related death in areas affected by the Fukushima Daiichi nuclear power plant accident: An observational study. BMJ Open. 14, e084009 (2024).
Preliminary analysis of certified disaster-related death in the affected area of the Fukushima Daiichi nuclear power plant accident following the Great East Japan Earthquake: An observational study. https://www.icrpdopoii.org/1054320/pyop3947. (2022).
Ozaki, A. et al. Social isolation and cancer management after the 2011 triple disaster in Fukushima, Japan: A case report of breast cancer with patient and provider delay. Medicine. 95, e4027 (2016).
Saito, H. et al. The long term participation trend for the colorectal cancer screening after the 2011 triple disaster in Minamisoma City, Fukushima, Japan. Sci. Rep. 11, 23851 (2021).
Sawano, T. et al. Successful emergency evacuation from a hospital within a 5-km radius of Fukushima Daiichi Nuclear Power Plant: The importance of cooperation with an external body. J. Radiat. Res. 62(Supplement 1), i122–i128 (2021).
Yamamura, M. et al. Case Report: Difficulties faced by a home oxygen therapy patient who died after the Fukushima Daiichi nuclear power plant accident. Front. Public Health. 12, 1394376 (2024).
Onishi, H. et al. Ultrasound cardiography examinations detect victims’ long-term realized and potential consequences after major disasters: A case-control study. Environ. Health Prev. Med. 23, 37 (2018).
Tsuboi, M. et al. Evacuation at home delayed the first medical intervention in Minamisanriku town after the 2011 Great East Japan Earthquake. Prehosp. Disaster Med. 38, 301–310 (2023).
Ozaki, A. et al. Breast cancer provider interval length in Fukushima, Japan, after the 2011 triple disaster: A long-term retrospective study. Clin. Breast Cancer 20, e127–e150 (2020).
Kitazawa, K. et al. Disaster-related deaths with alcohol-related diseases after the Fukushima Daiichi nuclear power plant accident: Case series. Front. Public Health 11, 1292776 (2023).
Hung, K. K. C. et al. Health emergency and disaster risk management workforce development strategies: Delphi consensus study. Prehosp. Disaster Med. 37, 735–748 (2022).
Hung, K. K. C. et al. Health workforce development in health emergency and disaster risk management: The need for evidence-based recommendations. Int. J. Environ. Res. Public Health 18, 3382 (2021).
Mao, X., Fung, O. W., Hu, X. & Loke, A. Y. Characteristics of resilience among disaster rescue workers: A systematic review. Disaster Med. Public Health Prep. 16, 380–389 (2022).
Acknowledgements
The authors express their sincere gratitude to the municipal offices and their staff in Miyagi Prefecture for providing anonymized documentation regarding indirect disaster-related deaths following the 2011 Great East Japan Earthquake. Additionally, the authors would like to thank Editage (https://www.editage.com/) for their assistance with English language editing.
Funding
This study was partially supported by a Project Grant from the Co-Creation Center for Disaster Resilience, IRIDeS, Tohoku University, Japan. In addition, this study was partially supported by the National Research Institute for Earth Science and Disaster Prevention’s “2022 Social Expectations Discovery Study for Improving Disaster Resilience” (to author: Motohiro Tsuboi), JSPS KAKENHI Grant Number 17H00840, 17H06108, 21H05001 (to author: Shinichi Egawa) and the Ministry of Health, Labour and Welfare (MHLW) Health and Labour Sciences Research Grant Number JPMH24LA2001 (to author: Nahoko Harada).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The study was conceptualized by Motohiro Tsuboi, Hiroyuki Sasaki, Hyejeong Park, and Shinichi Egawa. The methodology was devised by Motohiro Tsuboi, Hiroyuki Sasaki, Hyejeong Park, Nahoko Harada, Manabu Hibiya, and Shinichi Egawa. Material preparation was handled by Motohiro Tsuboi, and Shinichi Egawa. The first draft of the manuscript was written by Motohiro Tsuboi, Hiroyuki Sasaki, Hyejeong Park, and Shinichi Egawa, and all authors commented on previous versions of the manuscript. The manuscript was reviewed and edited by Motohiro Tsuboi, Hiroyuki Sasaki, Hyejeong Park, Masaharu Tsubokura, Toyoaki Sawano, Nahoko Harada, Fumiyasu Zaima, Akihiro Uto, Tadashi Okamoto, Toshihiko Watanabe, Manabu Hibiya, Shinsaku Ueda, Noboru Sakamoto, Koichi Yasaka, Shigemasa Taguchi, Kazuya Kiyota, and Shinichi Egawa. The study was supervised by Shinichi Egawa. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tsuboi, M., Sasaki, H., Park, H. et al. Medical perspective on the systemic challenges involving indirect disaster-related deaths in Japan. Sci Rep 15, 5225 (2025). https://doi.org/10.1038/s41598-025-89349-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89349-7