Abstract
Schistosomiasis, a disease caused by parasitic worms, imposes a significant global health burden, affecting over 240 million people, particularly in low-income regions. To meet the Sustainable Development Goals (SDG), the World Health Organization (WHO) emphasize the need for novel antischistosomal agents. In previous work we identified that cinnarizine, a first-generation antihistamine, has promising antischistosomal activity. This study investigates the therapeutic potential of clocinizine, a chlorinated analogue of cinnarizine, against Schistosoma mansoni. Both in vitro and in vivo studies were conducted to assess its efficacy and compare it to the standard-of-care drug, praziquantel. Clocinizine exhibited potent in vitro antiparasitic activity, with an EC50 of 4.6 µM against adult worms. In a murine model of schistosomiasis, a single oral dose of 400 mg/kg clocinizine salt significantly reduced both worm burden and egg production by 86% and 89%, respectively. These results were comparable to the efficacy of praziquantel at 400 mg/kg, which achieved a 90% reduction in worm burden and an 84% reduction in egg counts. These findings underscore the potential of clocinizine as a promising antischistosomal agent and offer valuable insights for the development of novel cinnarizine-derived compounds with improved selectivity and efficacy.
Similar content being viewed by others
Introduction
Schistosomiasis, caused by parasitic worms of the genus Schistosoma, remains a significant global health challenge, particularly affecting impoverished communities in Africa, the Middle East, South America, and the Caribbean1. Over 240 million individuals worldwide are infected, leading to substantial morbidity and mortality. The disease’s debilitating effects, including tissue fibrosis, organ damage, and cognitive impairment, especially in children, impose a heavy socioeconomic burden on affected regions2.
As part of Sustainable Development Goal (SDG) target 3, the elimination of neglected tropical diseases (NTDs) like schistosomiasis has been prioritized. To achieve this, the World Health Organization (WHO) has set an ambitious roadmap to eliminate schistosomiasis as a public health problem by 2030 3. Among the strategies to meet this target, the development of novel antischistosomal agents is a critical need. Currently, praziquantel is the only drug widely used for schistosomiasis treatment in mass drug administration (MDA) programs4. However, concerns regarding its efficacy, and the potential emergence of drug resistance necessitate the identification of alternative therapeutic options5.
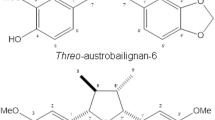
In recent years, antihistamines have emerged as promising candidates for the treatment of schistosomiasis6,7 and other helminth infections8. Our previous research demonstrated that cinnarizine (Fig. 1), a first-generation antihistamine, exhibited potent antischistosomal activity in both in vitro and in vivo assays7. However, the exact mechanism involved in this action is unknown, motivating us to investigate the antischistosomal potential of modified analogues.
Clocinizine (Fig. 1) is a chlorinated analogue of cinnarizine, commercially available for the treatment of hay fever and seasonal allergic rhinitis due to its enhanced efficacy as an antihistaminic agent9. Building upon our previous findings and considering the altered pharmacological profile of clocinizine, the present study aimed to investigate its antischistosomal potential both in vitro and in a murine model of schistosomiasis. Additionally, structural modifications were performed to evaluate molecular features contributing to its efficacy. The results presented here provide valuable insights for designing novel compounds with improved activity and optimized pharmacological profiles.
Results
In vitro antischistosomal activity of clocinizine and its analogues
To evaluate the in vitro antischistosomal activity of clocinizine and its analogues 1 and 2, adult Schistosoma mansoni worm pairs were initially exposed to a 50 µM concentration of the test compounds. If anthelmintic activity was observed, a serial dilution (1:2) was performed to determine the EC50 and EC90 values. Praziquantel was used as a positive control, while 0.5% DMSO served as the negative control.
As summarized in Table 1, clocinizine demonstrated potent antischistosomal activity against both male and female parasites, with EC50 and EC90 values of 4.6 µM and 5.9 µM, respectively. In comparison, praziquantel exhibited EC50 and EC90 values of approximately 1 µM for both male and females schistosomes. Neither compound 1 nor compound 2 showed any activity at 50 µM.
To further investigate the kinetics of clocinizine-induced worm mortality, time-kill assays were conducted. Clocinizine demonstrated a clear time- and concentration-dependent effect on both male and female worms (Fig. 2). At a concentration of 12.5 µM, clocinizine resulted in > 99% mortality for both sexes within 48 h. At a lower concentration of 6.25 µM, complete mortality of all adult worm pairs was observed within 72 h.
Viability of adult S. mansoni worms during exposure to clocinizine. Adult worm pairs were obtained from animals by perfusion 42 days post-infection. Each concentration of clocinizine was tested in triplicate, with the highest concentration of DMSO serving as the control and praziquantel (PZQ) at 2 µM used as the reference drug. Male and female schistosomes were monitored for up to 72 h. Results are expressed as percent mortality, represented by Kaplan-Meier survival curves. Data are presented as the mean ± SD from three independent experiments.
Cytotoxicity profile of clocinizine
To assess the potential cytotoxicity of clocinizine, Vero cells were treated with various concentrations of the drug. Clocinizine demonstrated negligible cytotoxicity up to a concentration of 200 µM, resulting in a selectivity index (SI) of > 40 (Table 1). In contrast, the positive control, doxorubicin, exhibited a CC50 of approximately 10 µM.
In vivo efficacy of clocinizine in an animal model infected with S. mansoni
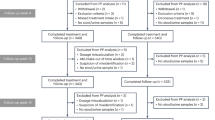
Following the promising in vitro results, the in vivo efficacy of clocinizine was evaluated in a murine model of schistosomiasis. Mice infected with S. mansoni were treated with a single oral dose of 400 mg/kg clocinizine di(hydrogen)maleate or praziquantel. Both drugs were well-tolerated, and all mice survived until the end of the study.
Clocinizine significantly reduced the total worm burden by 86.4% (P < 0.001). Similarly, praziquantel reduced the worm burden by approximately 90% (P < 0.001). Clocinizine also significantly reduced fecal egg counts by ~ 90% (P < 0.001) and immature egg counts in the intestine by approximately 70%. Praziquantel exhibited similar efficacy, reducing fecal egg counts by 88.2% and immature intestinal eggs by 83.8% (Fig. 3).
Therapeutic efficacy of clocinizine in Schistosoma mansoni infection. S. mansoni-infected mice were orally administered a single dose of 400 mg/kg clocinizine or praziquantel 42 days post-infection. Vehicle (water) was administered to the control group. All mice were euthanized on day 56 post-infection. Parasite burdens, as well as intestinal and fecal egg counts, were quantified. Data are presented as the mean ± SD (n = 5). ***P < 0.0001 compared to the infected untreated control.
Discussion
This study highlights the promising antischistosomal activity of clocinizine, a chlorinated analog of cinnarizine, in both in vitro and in vivo models of schistosomiasis. Clocinizine demonstrated efficacy comparable to praziquantel, the current gold-standard treatment, while exhibiting significant improvements over cinnarizine, underscoring its potential as a promising drug candidate for schistosomiasis.
In vitro, clocinizine showed potent schistosomicidal activity, with EC50 values comparable to praziquantel and superior to those of cinnarizine, which had an EC50 of 7.1 µM7. Compared to other drugs, clocinizine’s EC50 value of 4.6 µM places it among the most effective compounds against adult schistosomes, outperforming widely studied drugs such as tamoxifen10, spironolactone11, amiodarone12, and several antihistamines such as promethazine, cinnarizine, desloratadine, and rupatadine7.
Clocinizine’s pharmacokinetic profile supports its potential as an orally active antischistosomal agent. Similar to several other antihistamines, oral administration of clocinizine produces high bioavailability, with a maximum plasma concentration (Cmax) achieved within 1 to 3 h after administration13. Antihistamines typically exhibit a plasma half-life ranging from 4 to 60 h13,14, providing an adequate duration of action that may contribute to sustained efficacy against schistosomes. These characteristics are advantageous for therapeutic use, potentially reducing the need for frequent dosing and enhancing patient compliance.
In vivo, clocinizine demonstrated significant efficacy in a murine model of schistosomiasis. A single oral dose of 400 mg/kg, administered according to the protocol for experimental schistosomiasis in rodents15, achieved a worm burden reduction exceeding 85% and a substantial decrease in egg production. These results closely mirrored those of praziquantel and were markedly superior to cinnarizine, which achieved only a 55.6% reduction in worm burden and had no significant effect on egg production7. However, the use of a 400 mg/kg dose raises important considerations regarding clocinizine’s potential as a drug candidate. While effective against S. mansoni infection, this dose exceeds the desirable range for antihistamines, highlighting potential limitations in the current formulation’s bioavailability. Addressing these limitations through advanced formulation strategies, such as lipid-based carriers or the use of absorption enhancers, could enhance systemic absorption and reduce the required dose16,17. These approaches warrant further investigation in future studies.
Additionally, determining the lethal dose (LD50) of clocinizine and conducting detailed pharmacokinetic studies are critical next steps to elucidate its safety margins and dose-response relationship. Preliminary data and existing literature suggest that clocinizine exhibits a favorable safety profile, even at high doses, further supporting its potential for therapeutic use13. Future efforts should prioritize optimizing the formulation and identifying the minimum effective dose to advance clocinizine as a practical and scalable treatment option for schistosomiasis.
The superior efficacy of clocinizine in relation to cinnarizine may be attributed to its structural modification regarding the introduction of a chlorine atom. Structure activity relationship (SAR) for antihistamines suggests that presence of chlorine enhances antihistamine selectivity thus reducing the anticholinergic effects. For instance, chlorine insertion in diphenhydramine generated carbinoxamine, which has higher selectivity towards H1 receptor over muscarinic receptors18. Cinnarizine has important affinity to dopamine D2 receptor and calcium channels beyond histamine H1 receptor19, but literature data for clocinizine is scarce. Nonetheless, this structural modification improved clocinizine’s interaction with putative parasite-specific targets or the pharmacokinetics on both parasite and host, thereby enhancing its antiparasitic effects.
In general, invertebrate animals do not express metabotropic (i.e. GPCR) histamine receptors, but they may express a histamine-activated ionotropic receptor (HisCl) that leads to enhanced chloride ion permeation20. Some studies described the expression of two S. mansoni specific metabotropic histamine receptors namely SmGPR-1 and SmGPR-2, expressed in the body wall muscles and subtegumental nerve plexus, respectively21,22. However, there is no information whether cinnarizine or clocinizine may block or have affinity to these receptors. Future studies are essential to elucidate the precise mechanisms of action for both compounds, including their potential interactions with aminergic receptors, calcium channels, or other parasite-specific targets. The significant improvement in antiparasitic activity observed with clocinizine suggests that the addition of a chlorine atom played a crucial role, potentially enhancing binding affinity to its pharmacological target.
Analyzed using the ADMETlab 3.0 platform (available at admetlab3.scbdd.com), clocinizine exhibited higher lipophilicity (logP and logD7.4) and reduced solubility (logS) compared to cinnarizine. These physicochemical differences are likely to influence pharmacokinetic properties. Increased lipophilicity may enhance distribution through biological tissues, including the parasite’s environment, thereby impacting pharmacological activity and potency.
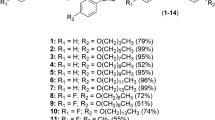
To explore the structural features influencing clocinizine’s efficacy, two additional analogues (1 and 2) were synthesized and tested in vitro against S. mansoni. Compound 1 lacks the 4-chlorophenyl group from clocinizine, while compound 2 is a methoxy-substituted analogue in the region of the cinnamyl moiety. Neither compound displayed significant anthelmintic activity (EC50 > 50 µM). These findings indicate that the presence of the second phenyl group is critical for maintaining activity, and the addition of a 4-chloro substituent further enhances the anthelmintic potency. Conversely, modification in the cinnamyl moiety, as exemplified by compound 2, proved detrimental to activity.
While this study provides compelling evidence for clocinizine’s antischistosomal activity, it is important to address several limitations. Further research is needed to evaluate its pharmacokinetics and pharmacodynamics properties. Additionally, exploring synergistic combinations with existing antischistosomal agents may enhance therapeutic outcomes and mitigate the risk of resistance development.
In conclusion, clocinizine emerges as a promising and safe prototype for developing new treatments for schistosomiasis, demonstrating greater in vivo efficacy than cinnarizine and comparable efficacy to praziquantel. These findings support further preclinical studies to validate clocinizine’s therapeutic potential and advance the search for novel treatment options to schistosomiasis. Moreover, future investigations into its mechanisms of action may provide valuable insights for designing novel cinnarizine-derived compounds with enhanced selectivity and efficacy. Such modifications could enhance clocinizine’s interaction with parasite-specific targets, improve its bioavailability, or both, thereby offering a promising avenue for drug discovery against helminthic infections. These efforts align with the SDGs and the global objective of eliminating these diseases as public health problems.
Methods
Synthesis of the compounds
All the starting materials and chemicals were purchased from Sigma-Aldrich (St. Louis, MO, USA) and LabSynth (Diadema, SP, Brazil) in adequate purity levels for synthesis.
Clocinizine was prepared as depicted in the scheme 1. Briefly, 1-(4-chlorobenzhydryl)piperazine (0,5 mmol, 0,141 g), cinnamyl chloride (0,55 mmol, 0,095 g) and potassium carbonate (1 mmol, 0,161 g) were added to 15 mL of acetone. The mixture was stirred for 24 h and then the solvent was evaporated. The residue was taken up with 15 mL of dichloromethane (DCM) and washed twice with purified water. The organic layer was dried with anhydrous Na2SO4 and evaporated. The crude material was purified through column chromatography using DCM: MeOH as eluent to yield 0,130 g (65%) of clocinizine1. H NMR (300 MHz, CDCl3) δ 7.43–7.09 (m, 14 H), 6.51 (d, J = 15.9 Hz, 1 H), 6.28 (dt, J = 15.8, 6.1 Hz, 1 H), 4.22 (s, 1 H), 3.19 (d, J = 6.7 Hz, 2 H), 2.56 (sl, 4 H), 2.45 (sl, 4 H). The NMR data is in accordance with literature reports23,24 .
Compound 1-benzyl‐4‐[(2E)‐3‐phenylprop‐2‐en‐1‐yl]piperazine (1) was synthesized by the same synthetic protocol (Scheme 1) but using 0,088 g of 1-benzylpiperazine as starting material, yielding 0,077 g (52%) of the purified product. TLC Rf 0.21 (50:1 DCM: MeOH)1. H NMR (300 MHz, CDCl3) δ 7.41–7.12 (m, 10 H), 6.50 (d, J = 15.9 Hz, 1 H), 6.27 (dt, J = 15.8, 6.7 Hz, 1 H), 3.51 (s, 2 H), 3.15 (d, J = 6.7 Hz, 2 H), 2.51 (sl, 8 H)13. C NMR (75 MHz, CDCl3) δ 138.16, 137.00, 133.04, 129.23, 128.58, 128.23, 127.49, 127.05, 126.68, 126.35, 63.09, 61.09, 53.25, 53.10. The NMR data is in accordance with previous literature report25.
Compound 1-[(4‐chlorophenyl)(phenyl)methyl]‐4‐[(2E)‐3‐(4‐methoxyphenyl)prop‐2‐en‐1‐yl]piperazine (2) was prepared from 1-(4-chlorobenzhydryl)piperazine (0,5 mmol, 0,141 g) by reacting with 4-methoxycinnamaldehyde (1 mmol, 0,167 g) (Scheme 2). The reactants were dissolved in 15 mL of acetonitrile and stirred for 1 h, and thereafter 1,5 mmol (0,094 g) of sodium cyanoborohydride were added and the mixture stirred for 20 h. The solvent was evaporated and the residue was taken up in 15 mL of ethyl acetate, washed twice with 15 mL of 5% aqueous sodium bicarbonate solution and 15 mL of purified water. The organic layer was separated, dried with anhydrous Na2SO4 and evaporated. The crude material was purified through column chromatography using DCM: MeOH as eluent to yield 0,150 g (70%) of 2. TLC Rf 0.1 (70:1 DCM: MeOH)1. H NMR (300 MHz, CDCl3) δ 7.40–7.20 (m, 13 H), 6.83 (d, J = 8.6 Hz, 6 H), 6.44 (d, J = 15.8 Hz, 1 H), 6.20–5.99 (m, 1 H), 4.21 (s, 1 H), 3.78 (s, 3 H), 3.14 (d, J = 6.8 Hz, 2 H), 2.53 (sl, 4 H), 2.43 (sl, 4 H)13. C NMR (75 MHz, CDCl3) δ 159.16, 142.15, 141.36, 132.72, 132.53, 129.73, 129.21, 128.64, 128.58, 127.86, 127.49, 127.15, 123.97, 113.99, 75.40, 61.05, 55.29, 53.32, 51.72.
To improve solubility, the compounds were converted into their respective di-(hydrogen)maleate salts by reacting the free bases with an excess of maleic acid in organic solvent26,27, to produce white solids with high purity (> 95%).
Drugs and reagents
Roswell Park Memorial Institute (RPMI) 1640 medium, Dulbecco’s Modified Eagle Medium (DMEM), heat-inactivated fetal calf serum, and penicillin-streptomycin solutions (10,000 U/mL penicillin G sodium salt and 10 mg/mL streptomycin sulfate) were procured from Vitrocell (Campinas, SP, Brazil). HEPES buffer, dimethyl sulfoxide (DMSO), and thiazolyl blue tetrazolium bromide (MTT) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Praziquantel was generously supplied by Ecovet Indústria Veterinária Ltda (São Paulo, SP, Brazil). All test compounds were solubilized in DMSO for use in in vitro experiments.
Animals, parasites, and cells
The Schistosoma mansoni life cycle (BH strain) was maintained at Guarulhos University (Guarulhos, SP, Brazil) using Biomphalaria glabrata snails as intermediate hosts and Swiss mice as definitive hosts. Three-week-old female Swiss mice were purchased from Animais de Laboratório Criação e Comércio (São Paulo, Brazil), while snails were obtained from the molluscary of the Research Center on Neglected Diseases at Guarulhos University. Both mollusks and rodents were housed under controlled environmental conditions (25 °C, 50% humidity) with a 12-hour light/dark cycle and ad libitum access to water and food. Four-week-old Swiss mice were subcutaneously infected with S. mansoni cercariae obtained from infected snails.
Vero cells (ATCC CCL-81, monkey kidney epithelial cells) were cultured in DMEM supplemented with 2 mM L-glutamine, 10% heat-inactivated fetal bovine serum, and antibiotics (100 U/mL penicillin, 100 µg/mL streptomycin). The cells were maintained at 37 °C in a 5% CO₂ humidified atmosphere in 25 cm² culture flasks (Corning, Tewksbury, MA, USA) and harvested using 0.25% trypsin-EDTA solution.
In vitro antiparasitic assay
Adult S. mansoni worms were recovered from infected mice via dissection at 49 days post-infection and maintained in RPMI 1640 medium supplemented with 5% fetal calf serum, 100 U/mL penicillin, and 100 µg/mL streptomycin at 37 °C in a 5% CO₂ atmosphere. Clocinizine di-(hydrogen)maleate and its analogues 1 and 2 were prepared at a starting concentration of 50 µM, then serially diluted at a 1:2 ratio in RPMI medium. The solutions were dispensed into 24-well plates (Corning, New York, NY, USA), with one male and one female S. mansoni worm added to each well. DMSO (0.5%) served as the negative control, while serial dilutions of praziquantel (starting at 2 µM) were used as the positive control. Worm viability was assessed at 0, 24, 48, and 72 h using an inverted microscope28. Death was defined as the absence of movement for at least one minute when stimulated with tweezers29. Experiments were performed in triplicate, and results were expressed as the percentage of viable parasites relative to controls6.
In vitro cytotoxicity assay
Cytotoxicity was evaluated using the MTT assay. Vero cells were seeded at 2 × 10³ cells per well in 96-well plates and incubated with serial dilutions of clocinizine di-(hydrogen)maleate (starting at 200 µM) for 72 h at 37 °C in a 5% CO₂ atmosphere. Serial dilutions of doxorubicin (starting at 20 µM) were used as a positive control. Following incubation, MTT solution was added, and plates were incubated for an additional 4 h. Absorbance was measured at 595 nm using an Epoch spectrophotometer (BioTek Instruments, Winooski, VT, USA)30,31. The percentage of viable cells was calculated relative to untreated controls, and selectivity indices (SI) were determined as the ratio of the CC50 in Vero cells to the EC50 for schistosomes. Each experiment was conducted in triplicate31.
In vivo studies in S. mansoni-infected mice
In vivo efficacy was evaluated using a murine model of schistosomiasis. Three-week-old Swiss mice were subcutaneously infected with 80 S. mansoni cercariae each. The animals were divided into three groups (n = 5 per group) and treated on day 42 post-infection with a single oral dose of clocinizine salt, praziquantel (400 mg/kg) or vehicle (water) by oral gavage32,33. On day 56 post-infection, mice were euthanized using CO₂ inhalation, and worms were collected, sexed, and counted to determine worm burden reduction. Egg burden reduction was evaluated by counting immature eggs in the intestine and eggs in the feces34. All experiments were performed by blinded investigators to reduce bias.
Data analysis
Statistical analyses were performed using GraphPad Prism 8.0 (San Diego, CA, USA). EC50, EC90, and CC50 values were derived from sigmoidal dose-response curves8. The non-parametric Kruskal-Wallis test was applied to compare worm burden and egg counts between control and treatment groups. Statistical significance was defined as P < 0.05.
Data availability
All relevant data for this study are included within the manuscript. The raw data that support the findings of this study are available from the corresponding author upon reasonable request.
References
WHO guideline on control. and elimination of human schistosomiasis. https://www.who.int/publications/i/item/9789240041608
McManus, D. P. et al. Schistosomiasis. Nat. Rev. Dis. Primers. 4, 13 (2018).
World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A road map for Neglected Tropical Diseases 2021–2030 (World Health Organization, 2020). https://www.who.int/publications/i/item/9789240010352
Spangenberg, T. Alternatives to praziquantel for the prevention and control of schistosomiasis. ACS Infect. Dis. 7, 939–942 (2021).
Ferreira, L. L. G., de Moraes, J. & Andricopulo, A. D. Approaches to advance drug discovery for neglected tropical diseases. Drug Discov Today. 27, 2278–2287 (2022).
Roquini, D. B. et al. Promethazine exhibits antiparasitic properties in vitro and reduces worm burden, egg production, hepato-, and splenomegaly in a schistosomiasis animal model. Antimicrob. Agents Chemother. 63 (19), e01208 (2019).
Xavier, R. P. et al. H1-antihistamines as antischistosomal drugs: in vitro and in vivo studies. Parasit. Vectors. 13, 278 (2020).
Roquini, D. B. et al. Antihistamines H1 as potential anthelmintic agents against the zoonotic parasite Angiostrongylus cantonensis. ACS Omega. 9, 31159–31165 (2024).
Criado, P., Criado, R., Maruta, C. & Filho, C. D. Histamine, histamine receptors and antihistamines: New concepts. Bras. Dermatol. 85, 195–210 (2010).
Silva, T. C. et al. New evidence for tamoxifen as an antischistosomal agent: In vitro, in vivo and target fishing studies. Future Med. Chem. 13, 945–957 (2021).
Guerra, R. A. et al. In vitro and in vivo studies of spironolactone as an antischistosomal drug capable of clinical repurposing. Antimicrob. Agents Chemother. 63, e01722–e01718 (2019).
Porto, R. et al. Antiparasitic properties of cardiovascular agents against human intravascular parasite Schistosoma mansoni. Pharmaceuticals (Basel). 14, 686 (2021).
Simons, F. E. H1-receptor antagonists. Comparative tolerability and safety. Drug Saf. 10, 350–380 (1994).
Simons, F. E. & Simons, K. J. Histamine and H1-antihistamines: Celebrating a century of progress. J. Allergy Clin. Immunol. 128, 1139–1150 (2011).
Lago, E. M. et al. Antischistosomal agents: State of art and perspectives. Future Med. Chem. 10, 89–120 (2018).
Mengarda, A. C., Iles, B., Longo, J. P. & de Moraes, J. Recent trends in praziquantel nanoformulations for helminthiasis treatment. Expert Opin. Drug Deliv. 19, 383–393 (2022).
Mengarda, A. C., Iles, B., Longo, J. P. & de Moraes, J. Recent approaches in nanocarrier-based therapies for neglected tropical diseases. Wiley Interdiscip Rev. Nanomed. Nanobiotechnol. 15, e1852 (2023).
Kubo, N., Shirakawa, O., Kuno, T. & Tanaka, C. Antimuscarinic effects of antihistamines: Quantitative evaluation by receptor-binding assay. Jpn J. Pharmacol. 43, 277–282 (1987).
Harding, S. D. et al. The IUPHAR/BPS guide to PHARMACOLOGY in 2024. Nucleic Acids Res. 52, D1438–D1449 (2024).
Jones, A. K. & Sattelle, D. B. The cys-loop ligand-gated ion channel gene superfamily of the nematode, Caenorhabditis elegans. Invert. Neurosci. 8, 41–47 (2008).
Hamdan, F. F. et al. A novel Schistosoma mansoni G protein-coupled receptor is responsive to histamine. Mol. Biochem. Parasitol. 119, 75–86 (2002).
El-Shehabi, F. & Ribeiro, P. Histamine signalling in Schistosoma mansoni: Immunolocalisation and characterisation of a new histamine-responsive receptor (SmGPR-2). Int. J. Parasitol. 40, 1395–1406 (2010).
Narsaiah, A. V. & Narsimha, P. Efficient synthesis of antihistamines clocinizine and chlorcyclizine. Med. Chem. Res. 21, 538–541 (2012).
Yu, T. et al. A novel synthetic approach to diarylmethylpiperazine drugs. Lett. Org. Chem. 15, 485–490 (2018).
Liang, H. et al. Synthesis of cyanamides from cyanogen bromide under mild conditions through N-cyanation of allylic tertiary amines. Synlett 28, 2675–2679 (2017).
Corrêa, M. F. et al. Novel potent (dihydro)benzofuranyl piperazines as human histamine receptor ligands - functional characterization and modeling studies on H3 and H4 receptors. Bioorg. Med. Chem. 30, 115924 (2021).
Varela, M. T., Romanelli, M., Amaral, M., Tempone, A. G. & Fernandes, J. P. Piperazine amides with desirable solubility, physicochemical and drug-like properties: Synthesis and evaluation of the anti-Trypanosoma cruzi activity. Saudi Pharm. J. 31, 1265–1273 (2023).
Mengarda, A. C. et al. Licarin A, a neolignan isolated from Nectandra oppositifolia Nees & Mart. (Lauraceae), exhibited moderate preclinical efficacy against Schistosoma mansoni infection. Phytother. Res. 35, 5154–5162 (2021).
Rocha, V. C. et al. Evaluating the antischistosomal activity of dehydrodieugenol B and its methyl ether isolated from Nectandra leucantha-a preclinical study against Schistosoma mansoni infection. ACS Omega. 8, 40890–40897 (2023).
Amorim, C. R. et al. Schiff bases of 4-phenyl-2-aminothiazoles as hits to new antischistosomals: Synthesis, in vitro, in vivo and in silico studies. Eur. J. Pharm. Sci. 150, 105371 (2020).
Brito, J. R. et al. Neolignans isolated from Saururus cernuus L. (Saururaceae) exhibit efficacy against Schistosoma mansoni. Sci. Rep. 12, 19320 (2022).
Queiroz, L. et al. In vitro and in vivo evaluation of cnicin from blessed thistle (Centaurea benedicta) and its inclusion complexes with cyclodextrins against Schistosoma mansoni. Parasitol. Res. 120, 1321–1333 (2021).
Sessa, D. P. et al. 15β-Senecioyl-oxy-ent-kaur-16-en-19-oic acid, a diterpene isolated from Baccharis Lateralis, as promising oral compound for the treatment of schistosomiasis. J. Nat. Prod. 83, 3744–3750 (2020).
Souza, D. C. S. et al. In vivo antischistosomal efficacy of PorPonderosaderosa γ-lactones. Phytomedicine 135, 156045 (2024).
Acknowledgements
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, Grant 2019/24028-8 and 2023/08418-6). TRT received postgraduate fellowships from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Finance Code 001). MS and FBL are also grateful to FAPESP for the shcolarships (Grants 2023/17755-6 and 2023/03485-7). JPSF and JdM hold Research Productivity Grants from CNPq (grant 307829/2021-9 and 312211/2021-0). The funding agencies had no involvement in the study’s design, data collection, analysis, interpretation, or the preparation of this manuscript. The authors also thank Rayssa A. Cajas for her assistance in in vivo experiments. Special thanks to Mariana (B) Silva for her technical support at the Núcleo de Pesquisa em Doenças Negligenciadas, Guarulhos University, Brazil.
Author information
Authors and Affiliations
Contributions
T.C., J.P.S.F., and J.d.M. contributed to conceptualization; T.C., T.R.T., M.S., F.B.L., and M.C.C.E.S. contributed to experiments and data interpretation; T.C., J.P.S.F. and J.d.M. contributed to writing - original draft and visualization; J.P.S.F. and J.d.M. contributed with resources, writing - review & editing; J.P.S.F. and J.d.M. contributed to project administration and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in accordance with the ARRIVE guidelines and approved by the Committee for the Ethical Use of Animals in Experimentation at Guarulhos University (Guarulhos, SP, Brazil) under protocol number #065/24. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Castro, T., Teixeira, T.R., Siegl, M. et al. Discovery of clocinizine as a potential oral drug against Schistosoma mansoni infection. Sci Rep 15, 30816 (2025). https://doi.org/10.1038/s41598-025-89434-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89434-x