Abstract
This exploratory study aimed to identify barriers and facilitators of a nurse-led satellite pilot clinic to improve sexually transmitted infection (STI) testing, treatment, and prevention in an Australian male correctional center. A descriptive qualitative research design was utilized to inform program evaluation. Qualitative data were collected from nurses via semi-structured interviews, and from incarcerated participants who attended the satellite clinic through open-ended satisfaction survey responses. Data were analyzed using deductive thematic analysis guided by the consolidated framework for implementation research (CFIR). Six major themes, aligned with the five CFIR domains were developed: (1) Meeting the needs of incarcerated people (outer setting domain); (2) Adaption based on needs; (implementation process domain); (3) Nursing staff motivation (individuals domain); (4) Incarcerated population’s desire to be healthy (individuals domain); (5) Shared vision (inner setting domain); and (6) Efficacy of clinics due to the satellite method (innovation domain). Barriers and facilitators raised by the two participant groups in this study identified a range of key recommendations: (1) Additional sexual health education; (2) Hiring appropriately skilled clinical nurses; (3) Collaborating with policy makers; (4) Continuing intra-organizational cooperation and adaptability; and (5) Additional days, advertising and modes of delivery. These recommendations highlight the requirement for these clinics to meet the needs of the incarcerated population.
Similar content being viewed by others
Introduction
Sexually transmitted infections (STIs; such as gonorrhea, syphilis and chlamydia) continue to be a major global issue with over one million STIs diagnosed daily1. Incarcerated people are at a higher risk of acquiring communicable diseases such as STIs compared to people living in the general community2. It is well-established that sexual risk behaviors such as unprotected sex in carceral settings, increases the risk of STI acquisition, including blood borne viruses such as hepatitis and HIV3,4. Similarly, there are multiple barriers impacting the likelihood of incarcerated populations engaging with health services, including low levels of health literacy, limited facility infrastructure5 and hinderances associated with carceral environments such as lockdowns limiting an individual’s ability to seeking medical services6. Thus, people residing in carceral settings may experience limited access to sexual healthcare7. In addition to enhancing access to a population who is often underserved regarding holistic and essential healthcare, a nurse-led sexual health clinics can improve STI testing, treatment, and prevention. Critically, it has the potential to help mitigate the risk and transmission of STIs within correctional settings8.
Background
STIs are viral, bacterial and parasitic infections that are spread through sexual contact, bodily fluids and skin-to-skin contact9. Some STIs are also transmitted through childbirth10. The World Health Organization (WHO) highlights that incarcerated people are a vulnerable population and at a higher risk of acquiring STIs than the general population7. Consequently WHO has provided recommendations to improve sexual healthcare provision for incarcerated populations inclusive of health interventions focused on the prevention of HIV, viral hepatitis, and STIs7. In Australia, it is well-established that incarcerated people are a vulnerable group and at particular risk of STI acquisition, yet they lack access to education and risk mitigation strategies within the custodial setting11,12.
Parallel to this, nurses have a unique opportunity to contribute to improved health outcomes through sexual healthcare provision13. Research suggest nurses have an important role in delivering patient-centered holistic healthcare and are well-positioned to reduce STI prevalence within the general population14. Horwood et al. conducted a nurse-led telephone-based service to manage chlamydia and gonorrhea infections diagnosed in the general community15. The study utilized ‘specialist’ nurses to run the nurse-led intervention, and was considered as acceptable and feasible by both healthcare providers and patients15. Within the general community, nurse-led clinics have been reported to improve access and uptake of sexual health services16. With STIs placing a significant financial burden on healthcare globally17, nurse-led clinics have also shown to be an affordable means of delivering quality healthcare with a particular impact on vulnerable and high-risk populations18. Similarly, nurse-led STI prevention programs have been successful in improving sexual health outcomes for vulnerable and at risk populations, such as incarcerated people8,19,20.
Taking the aforementioned factors into consideration, a nurse-led satellite clinic initiative for regular STI testing (hereon satellite STI clinic) was conducted in a male correctional center in Queensland, Australia. Drawing on two distinct cohorts, this descriptive qualitative study was conducted to identify the barriers and facilitators of the satellite STI clinic, and to inform clinic evaluation for scalability for: (1) incarcerated people attending the clinic; and (2) nursing staff involved in the implementation of the clinic.
The study
Aims and objectives
The aim of this exploratory research was to investigate the barriers and facilitators of implementing a nurse-led satellite STI clinic to improve STI testing, treatment, and prevention among a population of incarcerated people in a male correctional center in Queensland, Australia to inform clinic evaluation and potential scalability.
Methods
Study design
A descriptive qualitative research design was used to undertake this study. Drawing on the perspectives of incarcerated people attending and clinic nurses delivering the satellite STI clinic respectively, a deductive thematic analysis was used guided by the Consolidated Framework for Implementation Research (CFIR) to explore the barriers and facilitators to implementing the satellite STI clinic in the corrections environment.
The satellite STI testing clinic
Prior to implementing the satellite STI clinic, incarcerated people were required to complete a request form to access health services, including sexual health services. Once assessed and triaged by a healthcare professional, the individual was placed on a waitlist to receive an appointment with relevant healthcare personnel. The time period between a health service request and an appointment varied, and could be delayed due to lockdowns, and triage level (acute–non-acute). Post appointment, delays in care could be attributed to off-site pathology and courier requirements. The implemented satellite STI clinic sought to overcome these issues by providing a total of 26 satellite clinic days (one per week) for a 6-month period. A single clinic nurse travelled to a secure location managed by the carceral facility to provide the satellite STI clinics, and maintained patient nurse confidentiality. Clinics provided STI testing for common STIs including chlamydia, gonorrhoea, trichomoniasis, and syphilis, as well as for BBVs that can be sexually transmitted including HIV, hepatitis C, and hepatitis B through pahtology testing. Screening, prevelance, and treatment rates pertaining to the satellite STI clinic are reported elsewhere (currently under review) and participant numbers are reported below.
Participants attending the clinic were given one-on-one sexual health education based on responses provided in the sexual health history, and individual needs. In the event of a positive STI result, treatment and follow up testing were undertaken, and contact tracing if required.
Theoretical framework
The CFIR framework is a determinants framework used to consider barriers and facilitators informing an implementation approach21,22. For this study, we selected the updated CFIR framework, as it is the most up-to-date version of a commonly used determinants framework utilized in health service evaluations22. We modified Lam et al.’s CFIR semi-structured interview guide to suit the research environment with the inclusion of the satellite STI testing clinic (a pivotal component regarding the structure and design of this study)23. Table 1 provides an overview of the adaptation to Lam et al.’s CFIR guided semi-structured interview guide23. The CFIR framework was also selected for its ability to facilitate the translation of research into practice by considering: (1) what interventions have worked; (2) where they worked; and (3) why they worked, to collectively assess if and how the intervention was effective, sustainable, and to aid in dissemination21. The CFIR framework considers the constructs for effective implementation based on user feedback through five domains: (1) outer setting; (2) implementation process; (3) individuals; (4) inner setting; and (5) innovation. Within these five domains, there are underlying constructs and sub-constructs; each used to consider what has worked, where, and why22 (see Fig. 1).
Damschroder et al.’s22, updated CFIR framework as it applies to coding.
Study setting and recruitment
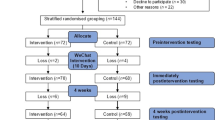
This single-site study was undertaken in a closed high security correctional center in Queensland, Australia. The correctional center had a maximum capacity of 1550 people, including men and a few transgender women, all aged 18 years and over. There was a total of five satellite clinic nurses who were identified for recruitment. A recruitment email was distributed by the Deputy Director of Research for the hospital and health service to create a degree of separation between the researchers and the potential participants. The email contained information about the research along with contact details for a member of the research team to discuss any questions and/or to organize participant information sheets and consent forms prior to taking part in the project.
Incarcerated people residing in the correctional center were eligible to voluntarily participate in the satellite STI testing clinics held between December 2022 and June 2023. Prior to the commencement of the clinics, a verbal presentation was provided by the clinic nurse in each of the prison’s accommodation areas. This presentation provided a comprehensive explanation of the clinic’s program and overall aim. The presentations also advised when the program would commence, how long the clinics and the program would run, what the clinic consultation would entail, the procedure to be taken if a patient received a positive diagnosis, where and when the clinics would be held, and how to participate in the satellite STI clinic program (self-nomination were offered).
Data collection
Clinical nursing staff
Qualitative data were collected and analyzed from satellite STI clinic nurses via semi-structured interviews, lasting up to 30 min in duration. These Interviews were conducted in March and April 2024. Participant information sheets and consent forms were provided to potential satellite STI clinic nursing participants to read, ask questions and sign prior to the interviews. One member of the research team (A.M.), who had no previous contact with the satellite STI clinic nurse participants, carried out data collection via one-on-one semi-structured interviews. These interviews were audio recorded with automatic transcription and then deidentified prior to the lead researcher engaging in data synthesis. Due to participants potentially being known to two of the researchers (A.B. and A.Br.), potential participants were requested not to discuss their recruitment and/or participation in the study with the other parties. Four out of the five clinic nurses participated in the study—this represented 80% of this cohort, and was deemed satisfactory by the author team. This sentiment also aligns with Saunders et al. suggesting a study sample is large enough to reach theoretical saturation when it satisfies the study’s research question, theoretical lens, and analytical framework24.
Incarcerated people
Qualitative data were collected and analyzed from incarcerated people who participated in the satellite STI testing clinic (collected from week five onwards) and provided satisfaction survey responses to the two open-ended questions (2 min in duration). Qualitative responses were provided in 191 clinic sessions. Out of these sessions, 181 incarcerated people participated in the satisfaction survey with nine participants attending the clinics twice, and one participant providing no response. A.B. and A.Br. conducted a medical chart audit to extract these responses which occurred between October 2023 and March 2024, and ensured all data were de-identified and anonymized, to maintain participant confidentiality.
As this is exploratory research, two open-ended questions were asked: ‘What did you find good about the clinic?’ and ‘What could we do to improve?’ These questions were adapted from an inpatient survey conducted by the National Health Service (NHS) Care Quality Commission where the qualitative survey questions were used to consider inpatient experiences in an NHS hospital25. The responses to the question ‘What could we do to improve?’ were used to identify barriers to the implementation of the satellite STI testing clinic, and the responses to ‘What did you find good about the clinic?’ were used to consider facilitators. Due to limitations relating to literacy, and multilingual diversity, the clinic nurse administered the satisfaction survey verbally, documenting responses verbatim.
Data analysis
Qualitative data from the semi-structured interviews and the open-ended satisfaction survey questions were analyzed as separate data sets. One researcher with in-depth understanding of the research environment (A.B) completed the coding to ensure all implied and inferred meanings were captured. The authors then utilized the five CFIR domains, constructs and sub-constructs as codes which were then used to consider the responses to both data sets (see Table 1). Member checking was also completed with the satellite STI clinic nurses with no changes being required to the interview transcripts. All coding was completed using NVIVO software where ‘parent’ and ‘child’ codes were assigned. Confirmability of data analysis and synthesis were completed through multiple group discussions amongst all co-authors with perspectives and experiences of researchers from different disciplinary backgrounds including differing intersecting identities concerning gender, sexuality, and cultural and linguistic backgrounds.
Ethical considerations
The study, with its two data collection methods, was approved by the Townsville Institute of Health Research and Innovation (TIHRI) HREC/2023/QTHS/97545, and the University of Southern Queensland Human Research Ethics Committee ETH2024-0346.
Informed consent was gained from all clinic nurses participating in the study. Due to the incarcerated population being transient in nature, open-ended satisfaction survey questions (part of the archival medical charts) became the method to collect the voice of the incarcerated population. As these open-ended satisfaction survey questions were documented in patient charts, approval to waiver informed consent was gained from the Public Health Act (PHA; PHA 97545) allowing access to medical charts to retrieve the satisfaction responses from incarcerated individuals. This was also in line with the Australian National Statement on Ethical Conduct in Human Research (2007)—updated 2018, and in line with the 1964 Declaration of Helsinki and its later amendments. All methods were carried out in alignment with these ethical standards, guidelines and regulations, including de-identification and anonymization of all data from both cohorts.
Findings and discussion
Table 2 presents the six major themes that were developed from the data which are represented in each of the five CFIR domains including: (1) Meeting the needs of incarcerated people (outer setting domain); (2) Adaption based on needs; (implementation process domain); (3) Nursing staff motivation (individuals domain); (4) Incarcerated population’s desire to be healthy (individuals domain); (5) Shared vision (inner setting domain); and (6) Efficacy of clinics due to the satellite method (innovation domain). The barriers and facilitators for each cohort group are presented too.
In four of the five CFIR domains, the incarcerated population and the satellite STI clinic nurses’ responses aligned to develop one single theme within the domain. However, this was not the case with the ‘Individuals domain’, where two separate themes were developed for each cohort with ‘Nursing staff motivation’ as the theme for satellite STI clinic nurses, and ‘The incarcerated population’s desire to be healthy’ as the theme for incarcerated people.
Outer setting domain
Meeting the needs of incarcerated people
The overarching theme developed in the outer setting domain was ‘Meeting the needs of incarcerated people’. The corresponding construct for the nurses was associated with ‘Local conditions’, and for the incarcerated population the construct was associated with ‘Financing’.
Construct: local conditions
This construct related to environmental conditions that affected the implementation of the satellite STI clinics22 and was shown in the barriers identified by the satellite clinic nurses (see Table 2). Previous research has identified that environmental conditions play a significant role in the implementation of interventions in healthcare settings26,27. Within this construct, facilitators for satellite STI clinic nurses included ‘Responding to what incarcerated people want and need’ which was evidenced through the multiple accounts of how the clinics were meeting the needs of the facility’s incarcerated people (see Table 2). Barriers for satellite STI clinic nurses within the environment included factors that reduced the level of sexual health for incarcerated people due to limited access to sexual health services. Also, a low level of literacy and health knowledge within the environment, and the significant impact syphilis had within the State of Queensland, and within corrections were further barriers within this construct (see Table 2). This in turn affected the incarcerated people’s ability to maintain an adequate level of sexual health and wellbeing.
Construct: financing
The funding provided to pilot the satellite STI testing clinic included sexual health education, and has had a positive uptake. Similarly, participants in this study expressed satisfaction with the sexual health education provided which is in alignment with WHO recommendations suggesting that sexual health education is needed among vulnerable and at risk key populations, such as incarcerated populations28 (see Table 2). Insufficient funding was identified as an influential barrier to innovation within the nursing field29. Facilitators for incarcerated people included ‘Positive uptake and satisfaction with the sexual health education provided in the clinics’. The satisfaction survey responses stressed that the sexual health education that was provided was not only positively received but was also meeting the health needs of the incarcerated participants (see Table 2). This facilitator, under the financing construct was also seen as a barrier for incarcerated people which included ‘education funding,’ where incarcerated people wanted more sexual health education than the currently provided funding scheme provided (see Table 2). This indicates that incarcerated people are aware of their lack of sexual health literacy, and they want and need more sexual health education to improve their overall health while serving their time.
Implementation process domain
Adaption based on needs
As explored below, the overarching theme identified in the implementation process domain was ‘Adaption based on need’ and the construct was associated with ‘Adapting’ for satellite STI clinic nurses, while the construct was associated with ‘Reflecting and evaluating’ for incarcerated people.
Construct: adapting
The construct of adapting involved modifying the intervention to align with the workplace for optimal integration22. This aligns with Wiltsey et al.’s expanded framework for reporting adaption and modification to evidence-based interventions (FRAME) which is used to characterize modifications to new evidence based practice (EBP) implementation in healthcare30. Wiltsey et al. highlight that adaptions made to a new implementation in healthcare should be context-specific, and meet the needs of the target population to ensure optimal engagement, acceptance, and health outcomes30. The satellite STI clinic program’s adaptability was identified as both a barrier and a facilitator for the satellite STI clinic nurses to meet the needs of the incarcerated people. This was evident in both the design of this program (satellite methods to overcome inadequate space and to increase healthcare access to a priority healthcare need), and with the adaptions made to the sexual health education, catering specifically for incarcerated people (sexual health education based on current risk activities in the prison) (see Table 2). The satellite STI clinic nurses’ recollections suggested that the sexual health education provided to incarcerated people was quite distinct from the sexual health education provided in the general community (see Table 2). Thus, adaptions taking into account the needs of this vulnerable and at risk cohort are imperative, due to incarcerated populations’ disproportionately higher rates contracting STIs than the non-incarcerated population7. Similarly, the comments made by the satellite STI clinic nurses concerning inadequate space to conduct clinics, suggests that health service expansion is achievable by delivering the clinics through the satellite method (see Table 2).
Construct: reflecting and evaluating
The ‘Reflecting and evaluating’ construct was used to reflect on the success of the implementation of the satellite STI clinic drawing on two sets of qualitative data22. Based on responses to the open-ended satisfaction survey question, the ‘Reflecting and evaluating’ construct was a facilitator for incarcerated people. Here, incarcerated people expressed a high level of satisfaction with the nursing staff who delivered the clinics, including, to a large degree, responding ‘nothing’ or ‘nil’ to the satisfaction survey question ‘What could we do to improve?’ (see Table 2). This satisfaction survey question was designed to identify the barriers of incarcerated people however, the adaptions made to the satellite clinics had an overwhelming positive response.
Individuals domain
Incarcerated population’s desire to be healthy
Two overarching themes developed in the individuals domain were ‘Incarcerated population’s desire to be healthy’, and ‘Nursing staff motivation’.
The theme ‘Incarcerated population’s desire to be healthy’ and the sub-domain construct was associated with the ‘Need’ for incarcerated people. The theme identified in the individuals domain for satellite STI clinics nurses was ‘Nursing staff motivation’ and the constructs and sub-constructs were associated with ‘Mid-level leaders’ construct, and the ‘Innovation recipients’ construct, with a sub-construct of ‘Motivation’ for satellite STI clinic nurses.
Construct: innovation recipients
This construct and its sub-construct of ‘Need’ refer to the participants who were directly affected by the satellite STI clinic, and how the participant’s wellbeing was affected by the clinic’s implementation22. Additionally, satisfaction survey responses from the incarcerated population reflected their ‘desire to be healthy and wanting to get tested’ as a facilitator, including the awareness that testing for STIs is a means to do so (see Table 2). These responses also highlighted the barriers for incarcerated people suggesting the need for additional interventions to support their rights to ‘the enjoyment of the highest attainable standard of physical and mental health’ while serving their sentence, as outlined by International Covenant on Economic, Social and Cultural Rights of which Australia is a signatory31. Multiple studies on STI prevention interventions have been conducted in other jurisdictions in Australia, such as Dolan et al.’s study on a condom distribution program in New South Wales (NSW)32, Scott et al.’s condom distribution program with paired opt-out STI in Victoria (VIC)33, and Yap et al.’s study on dental dam use in NSW34. However, correctional centers in Queensland, Australia have yet to embrace any of these evidence-based primary interventions to protect people from contracting STIs in prison35, including the general population once incarcerated people have served their time.
Nursing staff motivation
Construct: implementation team members
Within this domain, the construct of ‘Implementation team members’ refers to the satellite STI clinic nurses directly involved in implementing the satellite clinic intervention22. A facilitator for satellite clinic nurses included positive outcomes as a result of motivated staff. This facilitator resulted in positive change for the incarcerated population due to nurses passionate about sexual health, driven to invoke change, and had a desire to improve the overall health of incarcerated people (see Table 2).
Construct: mid-level leaders
The ‘Mid-level leaders’ construct refers to those with a medium level of authority within the organization, and their influence on the implementation22 of the satellite STI clinic. The ‘Innovation recipient’ construct with a sub-construct of ‘Motivation’ refers to the people directly involved in the implementation of the satellite clinic, and their motivation to achieve their goal22. The ’Mid-level leaders’ construct was a barrier for satellite clinic nurses as it involved obtaining work unit guideline (WUG) approval for implementing the satellite STI clinic (see Table 2). The required approval, and the bureaucratic nature of healthcare facilities, including wider organizational structures can hinder for interventions to be implemented in a timely manner.
Construct: innovation recipients
Another barrier for satellite STI clinic nurses involved incarcerated people being at risk of impacting the sexual health of the general community. This barrier came under the ‘Innovation recipients’ construct, with a sub-construct of ‘Motivation’ as the satellite STI clinic nurses were motivated by their concern for the health of both incarcerated people and the general community outside the carceral setting (see Table 2). More specifically, as high rates of STIs in carceral settings are transmitted by incarcerated people moving in and out of the custodial setting this is a significant transmission concern affecting the general population36. The ‘Motivation’ sub-construct also applied as a facilitator for satellite STI clinic nurses with multiple accounts from expressing feelings of confidence in applying the WUG, and positive outcomes because of motivated staff (see Table 2).
Inner setting domain
Shared vision
The overarching theme identified in the inner setting domain was ‘Shared vision’ and the construct and sub-constructs were associated with ‘Culture’, ‘Human equality centeredness’, ‘Recipient centeredness’, and ‘Mission alignment’ for satellite STI clinic nurses. The construct for incarcerated participants was ‘Tension for change’.
Construct: mission alignment
The ‘Mission Alignment’ construct refers to the overall commitment of those within the inner setting to achieving the goal of implementing the satellite STI clinic intervention22. This construct applied to the barriers for satellite STI clinic nurses including skepticism, and resistance to change among other health staff within the carceral system and setting (see Table 2). Organizational culture plays a critical role regarding the success of a new implementation26 such as the one explored in this paper.
Construct: tension for change
The ‘Tension for change’ construct relates to the immediate need for change as a result of unacceptable conditions22. Within this construct, barriers for incarcerated people included a lack of advertising, a concern the satellite STI clinic program could discontinue, and the lack of services in other incarcerated settings (see Table 2). This construct also acted as a facilitator for incarcerated people who were very satisfied with how accessible the sexual health services became after the immediate and implemented changes to the STI testing procedure, compared with the previous and time consuming method of accessing the carceral setting’s sexual health services (see Table 2).
Construct: culture
Facilitators for satellite STI clinic nurses included the multilevel interorganizational support, and were identified within the ‘Culture’ construct, which included sub-constructs of ‘Human equality centeredness, and Recipient centeredness’22. These constructs and sub-constructs apply to the common ideals, values, and beliefs shared by all stakeholders involved in implementing the satellite STI clinic intervention. The stakeholders had a shared goal to support the incarcerated populations’ welfare rooted in equality and optimal health. Aside from the perceived delays regarding the satellite STI clinic implementation approval process, the satellite clinic nurses’ expressed an overwhelming support from diverse stakeholders, including health services, and Queensland Corrective Services (QCS) (see Table 2). Previous research on the implementation of EBP found that nurse managers played a significant role in the successful adoption of an EBP intervention37. Similarly, a study by Urquhart et al.38 reported that buy-in and support from program leaders at multiple levels within a clinical department, played a significant role in the successful implementation of the intervention.
Innovation domain
Efficacy of clinics due to satellite method
The overarching theme identified in the innovation domain was ‘Efficacy of clinics due to the satellite method’ and the construct and sub-constructs were associated with ‘Adaptability’ and ‘Relative advantage’ for satellite STI clinic nurses. The constructs and sub-constructs for incarcerated participants were associated with ‘Adaptability’.
Construct: adaptability
The ‘Adaptability’ construct was applied to the barriers identified by both the satellite STI clinic nurses and the incarcerated people. Barriers for the incarcerated people were connected to ‘Not enough days a week’ for STI testing, while the barriers for the satellite clinic nurses, related to possible stigma associated with STI testing within the corrections environment negatively affecting incarcerated people. The ‘Adaptability’ construct relates to the ability of an innovation to be modified and changed within the environment to meet the needs of the recipients22. This construct was applied to these barriers to make recommendations. Facilitators for incarcerated people also came under the ‘Adaptability’ construct which highlighted how the adaptions made to the clinics through the satellite method had a positive outcome. This included the adaptions made to fit the clinic within the carceral environment and meeting the incarcerated people in their accommodations, as opposed to incarcerated people making STI testing appointments and possibly waiting for months before accessing a medical consultation (see Table 2). Here, the incarcerated people noted the ‘Convenience that the satellite clinics provided’ as a facilitator. Facilitators identified by the satellite STI clinic nurses included ‘Improved uptake and improved health outcomes’ (see Table 2).
Construct: relative advantage
Facilitators for the satellite STI clinic nurses came under the ‘Relative advantage’ construct referring to an implementation being more beneficial and suitable than the previous method22. In this instance, satellite STI clinic nurses noted an increased uptake of STI testing, and an improved health outcome by treating participants receiving a positive STI diagnosis more efficiently, and through sexual health education.
Recommendations
Outer setting domain
The overarching theme for the outer setting domain related to ‘Meeting the needs of incarcerated people’. The needs identified by both incarcerated people and satellite STI clinic nurses highlighted that incarcerated people both want and need sexual health education. To meet this need and recommendation, additional funding is required by offering further STI testing through the week, coupled with sexual health education, with more staff engaged in the STI testing, treatment and prevention. Limited access to health services both within and outside the carceral setting was a barrier to incarcerated people receiving testing, treatment, and prevention through sexual health education. This issue is compounded with the low level of health literacy among the carceral population, including difficulties understanding health promotion messaging due to poor reading skills (see Table 2). A study by Tenibiaje et al. considered the literacy and health literacy levels among incarcerated adults in Nigerian prisons which were both found to be deficient within this cohort39. This study highlighted the significant impact low levels of literacy have on health literacy which in turn has a deteremental effect on the health and wellbeing of incarcerated populations39.
Satellite STI clinic nurses identified how taking the STI testing, and sexual health education to the incarcerated population in their accommodation setting, resulted in increased number of incarcerated people being tested, treated, and educated (see Table 2). This positive outcome was rooted in improved access. Findings from this study parallels with that of Pimenta et al.’s study focusing on opportunistic testing for chlamydia in both primary and secondary healthcare environments and the positive associations this may have40. Although access to testing was not a factor in Pimenta et al.’s study, testing asymptomatic patients opportunistically no matter their initial reason for attending the healthcare facility, was found to be both acceptable, and a suitable method for upscale40.
Recommendations
The need for additional funding and education related to sexual health for incarcerated people
A key recommendation relates to the continued funding for the satellite STI clinic to maximize continued fruitful uptake, and for the upscale of the satellite STI clinics nation-wide. It is recommended that the additional funding be allocated to the improvement and expansion of the sexual health education component of this satellite STI clinic to better align with WHO’s recommendations to provide comprehensive sexuality education, including STIs and HIV, and adequate health service interventions for vulnerable populations, such as incarcerated people1.
Implementation process domain
The overarching theme for the implementation process domain was ‘Adaption based on need.’ This theme was strongly focused on listening to feedback, responding to the needs of incarcerated people and satellite STI clinical nurses, and adapting the process if required. Whilst one incarcerated participant requested ‘More confidentiality, NO prison Corrections Officer’ (see Table 2) this is an inactionable request as nursing staff are, due to safety precautions, required to be accompanied by prison officers when conducting clinics.
Similarly, to the authors’ knowledge, satellite clinics providing mobile medical care within carceral settings is an under-researched area. However, studies involving mobile STI testing clinics within the community have, similar to the current study, had positive outcomes in relation to improving testing and treatment for the targeted population41. For example, a study by Heese et al. focused on mobile STI testing within the community found that taking STI testing to/near to populations vulnerable to contracting STIs, improved accessibility and uptake41. As such and for future upscale, the authors of this article recommend the STI clinics remain satellite to reduce the burden on medical centers, to improve workflow, and importantly, increase access and uptake to STI testing, treatment and prevention through sexual health education. Parallel to this, both incarcerated people and satellite STI clinic nurses highlighted that high risk STI-inducing behaviors were undertaken in the carceral setting (see Table 2), offering valuable insights into how and why some STIs are spreading in real time. This information would further enhance the sexual health education to be adapted to be further relevant and meet the needs of the incarcerated population.
Recommendations
Having appropriately skilled nursing staff running the clinics
Future staffing considerations should include nurses who are approachable, non-judgmental, knowledgeable, and capable of building therapeutic working relationships with incarcerated people. Whilst the lead author intends to upscale the satellite STI testing program with the sexual health team currently in place, the inclusion of an increased staffing pool to implement the clinic at each center during upscale is imperative for its success. Open-ended satisfaction survey responses need to be monitored to ensure incarcerated people’s high satisfaction with the nurses delivering the satellite STI clinic continues.
Individuals domain
The overarching theme for the Individuals domain was ‘Nursing staff motivation’, and the ‘Incarcerated population’s desire to be healthy.’ One barrier relating to gaining approval for the WUG process, was associated with the extensive time satellite STI clinic nurses were spending applying for and gaining WUG approval (see Table 2). A study by McFadyen and Rankin identified that research involving vulnerable populations, often have gatekeepers outside the ethics approval process who may contribute additional barriers for researchers42. Apa et al.’s study exploring the challenges and strategies to conduct research in prisons had similar findings, highlighting the additional barriers to obtaining appropriate permissions when conducting research with incarcerated people, including the additional time required to review protocols for implementation43. When developing a collaborate research relationship Apa et al., stress how establishing prison contacts, and maintaining rigorous research methods are key to successfully conducting research with incarcerated populations43. In applying this learning, and to overcome the barriers experienced in this study, future practice would benefit from including the development of a statewide carceral implementation toolkit. Once approved, this toolkit could be applied to carceral environments negating the need for multiple applications, expediating the implementation of the satellite STI testing clinic. As reported in research, evidence-informed toolkits are used to facilitate the implementation of evidence-based interventions by providing resources that are adaptable and customizable, in turn accelerating the process of translating research into practice44.
A large cohort of the incarcerated people also requested, through the open-ended survey questions, access to prophylaxis such as condoms (see Table 2). Currently, accessing these items through diverse STI and BBV preventative programs are unavailable to people incarcerated in Queensland35. Yet some programs in correctional centers in other Australian jurisdictions offer access to condoms (and dental dams) through vending machines, such as NSW, VIC, Western Australia, and Tasmania12.
Recommendations
Collaboration with policy makers
It is recommended that policy makers work with correctional services to consider the implementation of a condom/dental dam distribution, for incarcerated populations within the next six months to ensure alignment with WHO recommendations7 and incarnated people’s right to ‘the enjoyment of the highest attainable standard of physical and mental health’31. Additionally, these policy makers could work to incorporate this as ‘core business’ within state and national strategies with a large scale evaluation, including health economic evaluation for future research within the same timeframe.
Inner setting domain
The overarching theme within the inner setting domain was ‘Shared vision’ based on the high levels of support of implementing the satellite STI testing clinic evident both from the incarcerated peoples’ open-ended survey responses, and the responses from satellite STI clinic nurses (see Table 2). Scholars have identified that successful integration of EBP require support from both the researchers implementing the intervention, and from diverse stakeholders within the organization/setting38,45. Within this context, the satellite STI clinic nurses identified that the satellite STI testing program received overwhelming support from all levels within Queensland Health, and that of QCS (see Table 2). At each level of the organizations a shared vision was present, in turn playing a contributing factor to the clinic’s success.
Recommendations
Continued intraorganizational cooperation, and the continued adaptability of the program
It is recommended that for upscale of this satellite STI testing program, further communication, co-operation and input from all levels within Queensland Health and QCS be maintained. It is also recommended that the satellite STI clinics continue to be adapted, where and when required, considering stakeholder input at all levels. With continued senior level support, being embedded in policy, and not susceptible to changes to staffing and/or changes to ruling political parties, this program has a greater chance to continue and thrive.
Successful implementation of this recommendation will be evidenced by a continuation of open communication pathways, intraorganizational cooperation, and adaptability of the satellite STI clinic program. It is also recommended that this model, due to its adaptability, be embedded into all quality improvement activities, to enhance EBP within correctional settings, and to enhance clinically relevant research culture. This model can also be adapted to each specific future carceral site to enhance relevance and feasibility.
Innovation domain
The overarching theme for the innovation domain related to the ‘Efficacy of clinics due to the ‘satellite method’. This was strongly supported by the incarcerated participants and the satellite STI clinic nurses, with both expressing the effectiveness of the satellite STI clinic method, and the need for additional days to run the clinics (see Table 2). This need also considered the delays deriving from the pathology section of the carceral setting needing to send the pathology specimen to the local hospital, and the needs of the incarcerated people to have a quick turnaround from testing to treatment, especially if an individual tested positive. Advertising of future satellite STI clinics was also asked for, and a small number of incarcerated people requested that STI testing also be made available in the medical center (see Table 2).
Recommendations
Additional days, advertising, and modes of delivery
It is recommended that for the upscale of this project, satellite STI testing clinics should be delivered and offered additional days per week based on the demand outstripping the current and available financial resources. Similarly, the clinics will need to be announced and advertised in advance to provide adequate awareness that the nurses will be attending, and when. Finally, it is recommended that testing be offered in the medical center as an additional service securing accessibility. These recommendations should be implemented within the study site, and as a core component regarding the upscale of the clinics. To evaluate the success of these recommendations, additional closed and open-ended satisfaction survey questions can be included for the incarcerated population.
Strengths and limitations
This study had multiple strengths, including the innovative nature of the study and the high level of uptake and acceptance, in turn demonstrating the need for clinic upscale. A key strength of the study was the innovative delivery of the satellite method to overcomes barriers that are impeding on incarcerated people from accessing STI testing, treatment and prevention within the carceral environment. This was evidenced by the nursing staff motivation, shared vision, and the incarcerated persons’ desire to be healthy. The clinics were well-received with engagement from multiple stakeholders, including multiple levels within Queensland Health, and QCS. This study has the potential for upscaling and promoting STI testing, treatment and prevention through sexual health education, collectively contributing to EBP and having real-world translational impact. Through EBP, this nurse-led sexual health clinic meets the needs of incarcerated people, by providing access to sexual health services, in an environment, typically known for challenging access these services. As such, this well-utilized and accepted model could be applied to other health care interventions focused on improving access to care for incarcerated people.
There were multiple limitations to this study including significant time delays associated with data collection due to multiple external research approval processes. Another limitation was the brevity of qualitative feedback from both the incarcerated population and from the satellite STI clinic nurses. It is recommended that in-depth interviews are conducted with future participants to gain greater insights regarding barriers/facilitators associated with the satellite STI clinic to inform future quality improvements, and adaptations of the program to meet the needs of incarcerated people.
A further limitation concerned the demands for the clinic outweighing the service delivery where funding allocated to run the clinic provided limited staffing and hours. Additional staffing and availability of hours would provide a better understanding of potential demand/uptake for the satellite STI clinic. However, initial findings are promising and warrant continuation of this service with room for adaption and to be replicated in further correctional settings in Australia, including globally.
As this study was within one correctional site in Queensland, Australia, caution must be used regarding generalizability of findings to other correctional facilities, including those outside of Queensland and Australia. However, the initial findings from this exploratory study provide the potential for further widescale implementation and evaluation.
Similarly, the potential needs of diverse sub-groups within the incarcerated cohort were unknown due the brevity of questions in the satisfaction survey, and those choosing to not engage with the pilot clinic and/or not completing the evaluation component of the satellite STI testing clinic. Likewise, although incarcerated transgender women residing in the facility were invited to utilize the satellite STI testing clinic, data related to the gender of the participants was not collected. As such, no unique data were collected concerning the transgender women who may have engaged in the service. The demographic data collected included sex assigned at birth but neglected to collect data surrounding the gender the participants identified with. Brömdal et al., highlight that transgender women within carceral setting are more susceptible to sexual violence, lack sexual health knowledge, and have reduced access to sexual health services, collectively increasing their vulnerability to contract STIs46. This oversight translated to valuable data from a vulnerable and at-risk sub-group within the carceral setting was not considered.
This study adapted Lam et al.’s CFIR guided semi-structured interview questions, which presented to be a feasible and replicable semi-structured interviewing framework and can be applied to multiple different research environments23. In applying these semi-structured interview questions to this study, we were able to conduct an evaluation of the constructs for the effective implementation of the satellite STI testing clinic based on the nurses’ feedback. However, one limitation in utilizing this framework was the potential for unintentionally excluding themes that did not fit within the CFIR construct. The potential omission of themes was also highlighted within Lam et al.’s evaluation of the farmwork as a potential limitation23. This limitation therefore also applies to our use of deductive analysis where the strict adherence to pre-existing objectives47, such as our research question, and codes applied from the CFIR framework meant that important underlying themes that did not fit within these constructs may have been overlooked.
Implication for policy and practice
To reach more correctional centers and more incarcerated people, the satellite STI clinic initiative is intended to be upscaled. With potential changes to policy, strategy and funding, a national rollout has potential benefits including a larger evaluation, health economic analysis. It also has the potential to be adapted for other specific health conditions and respond to emerging needs. With an evidence-informed implementation toolkit, the aspiration of reaching more correctional centers and providing adequate care to more incarcerated people are in reach with the provision of adequate funding and resources. The findings of this study have the potential to inform sexual health education programs, sexual health education materials, and future policies focused on the improvement of health outcomes for incarcerated people, including other relevant vulnerable, at-risk and priority sub-groups.
Conclusion
Overall, this study considered the barriers and facilitators to implementing a nurse-led satellite STI clinic to improve STI testing, treatment, and prevention in a male correctional center in Queensland, Australia. Results of the qualitative analysis highlight that the clinic was well-received by both incarcerated participants and satellite STI clinic nursing staff, and that education plays a pivotal role in ensuring long-term success and sustainability of such initiatives. Future research may benefit from including adapted versions of the semi-structured interview questions when evaluating new interventions and expanding on the open-ended satisfaction survey questions to be more nuanced in nature exploring the barriers and facilitators of the satellite STI testing clinic more in-depth.
Data availability
The participants of this study did not give written consent for their data to be shared publicly. Similarly, due to the sensitive nature of the research, supporting data are not available.
References
World Health Organization. Sexually Transmitted Infections: Evidence Brief (World Health Organization, 2019).
Australian Institute of Health and Welfare. The Health of People in Australia’s Prisons 2022 (Australian Institute of Health and Welfare Canberra, 2022).
World Health Organization Infectious diseases in prison. In Prisons and Health (eds Enggist, S. et al.) 73 (WHO Regional Office for Europe, 2014).
Moazen, B. et al. Availability, Coverage and Barriers Towards Condom Provision in Prisons: A Review of the Evidence (Institut für Suchtforschung (ISFF), Frankfurt University of Applied Sciences, 2019).
Queensland Government. Reducing Barriers to Health and Wellbeing: The Queensland Prisoner Health and Wellbeing Strategy 2020–2025. https://clinicalexcellence.qld.gov.au/sites/default/files/docs/about-us/what-we-do/office-prisoner-health-and-wellbeing/qld-prison-health-wellbeing-strategy.pdf (2020).
Audit office of New South Wales. Access to Health Services in Custody (Health Justice Management and Administration Service Delivery, 2021).
World Health Organization. Recommended Package of Interventions for HIV, viral Hepatitis and STI Prevention, Diagnosis, Treatment and Care for People in Prisons and Other Closed Settings Policy Brief (World Health Organization, 2023).
Kelly, C., Templeton, M., Allen, K. & Lohan, M. Improving sexual healthcare delivery for men in prison: A nurse-led initiative. J. Clin. Nurs. 29, 2285–2292. https://doi.org/10.1111/jocn.15237 (2020).
BC Centre for Disease Control. Smart Sex Resources-Know Your Chances. https://smartsexresource.com/sexually-transmitted-infections/sti-basics/know-your-chances/ (2024).
Mayo Foundation for Medical Education and Research. Sexually Transmitted Diseases (STDs)-Symptoms and Causes. https://www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/symptoms-causes/syc-20351240 (2023).
Australian Government. (ed Department of Health) (Australian Government, 2018).
Simpson, P. L., Gardoll, B., White, L. & Butler, T. HIV polices in Australian prisons: A structured review assessing compliance with international guidelines. Lancet Reg. Health West. Pac. 41, 100813 (2023).
Bungay, V., Handlovsky, I., Phillips, J. C. & Prescott, C. A scoping review of the literature on nursing practices with persons seeking care for sexually transmitted infections. J. Clin. Nurs. 26, 33–48 (2017).
East, L. & Jackson, D. Vol. 44, 47–49 (Taylor & Francis, 2013).
Horwood, J. et al. Management of chlamydia and gonorrhoea infections diagnosed in primary care using a centralised nurse-led telephone-based service: Mixed methods evaluation. BMC Fam. Pract. 21, 1–10 (2020).
Selfridge, M. et al. Exploring nurse-led HIV pre-exposure prophylaxis in a community health care clinic. Public Health Nurs. 37, 871–879 (2020).
Gottlieb, S. L. et al. Toward global prevention of sexually transmitted infections (STIs): The need for STI vaccines. Vaccine 32, 1527–1535 (2014).
Wagner, L. P. & Zabler, B. Costs saved by visiting a nurse-led primary care facility comparison of primary care models. Policy Polit. Nurs. Pract. https://doi.org/10.1177/15271544241247767 (2024).
Lloyd, A. R. et al. Safety and effectiveness of a nurse-led outreach program for assessment and treatment of chronic hepatitis C in the custodial setting. Clin. Infect. Dis. 56, 1078–1084 (2013).
Winter, R. J. et al. A nurse-led intervention improved blood-borne virus testing and vaccination in Victorian prisons. Aust. N. Z. J. Public Health 40(6), 592–594 (2016).
Damschroder, L. J. et al. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 4, 50. https://doi.org/10.1186/1748-5908-4-50 (2009).
Damschroder, L. J., Reardon, C. M., Widerquist, M. A. O. & Lowery, J. The updated consolidated framework for implementation research based on user feedback. Implement. Sci. 17, 75. https://doi.org/10.1186/s13012-022-01245-0 (2022).
Lam, H. et al. Identifying actionable strategies: Using consolidated framework for implementation research (CFIR)-informed interviews to evaluate the implementation of a multilevel intervention to improve colorectal cancer screening. Implement. Sci. Commun. 2, 57 (2021).
Saunders, B. et al. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 52, 1893–1907 (2018).
NHS Care quality commission. Adult Inpatient Survey 2021. https://nhssurveys.org/wp-content/surveys/02-adults-inpatients/04-analysis-reporting/2021/Scored%20questionnaire.pdf (2021).
Li, S.-A., Jeffs, L., Barwick, M. & Stevens, B. Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: A systematic integrative review. Syst. Rev. 7, 1–19 (2018).
McCullough, M. B. et al. The interplay of contextual elements in implementation: An ethnographic case study. BMC Health Serv. Res. 15, 1–12 (2015).
World Health Organization. Consolidated Guidelines on HIV, Viral Hepatitis and STI Prevention, Diagnosis, Treatment and Care for Key Populations. https://iris.who.int/bitstream/handle/10665/360601/9789240052390-eng.pdf?sequence=1 (2022).
O’Hara, S., Ackerman, M. H., Raderstorf, T., Kilbridge, J. F. & Melnyk, B. M. Building and sustaining a culture of innovation in nursing academics, research, policy, and practice: Outcomes of the National Innovation Summit. J. Prof. Nurs. 43, 5–11 (2022).
Wiltsey Stirman, S., Baumann, A. A. & Miller, C. J. The FRAME: An expanded framework for reporting adaptations and modifications to evidence-based interventions. Implement. Sci. 14, 1–10 (2019).
United Nations Human Rights Office of the High Commissioner. International Covenant on Economic, Social and Cultural Rights (United Nations, Treaty Series, 1976).
Dolan, K., Lowe, D. & Shearer, J. Evaluation of the condom distribution program in New South Wales prisons, Australia. J. Law Med. Ethics 32, 124–128 (2004).
Scott, N., McBryde, E., Kirwan, A. & Stoove, M. Modelling the impact of condom distribution on the incidence and prevalence of sexually transmitted infections in an adult male prison system. PLoS ONE 10, e0144869 (2015).
Yap, L. et al. Sexual practices and dental dam use among women prisoners—a mixed methods study. Sex. Health 7, 170–176 (2010).
Butler, T. et al. Sexual Health and Behaviour of Queensland Prisoners (National Drug Research Institute, 2010).
Kinner, S. A. & Young, J. T. Understanding and improving the health of people who experience incarceration: An overview and synthesis. Epidemiol. Rev. 40, 4–11 (2018).
Kueny, A., Shever, L. L., Lehan Mackin, M. & Titler, M. G. Facilitating the implementation of evidence-based practice through contextual support and nursing leadership. J. Healthc. Leadersh. 7, 29–39 (2015).
Urquhart, R., Porter, G. A., Sargeant, J., Jackson, L. & Grunfeld, E. Multi-level factors influence the implementation and use of complex innovations in cancer care: A multiple case study of synoptic reporting. Implement. Sci. 9, 1–16 (2014).
Tenibiaje, D. J. Investigating literacy and health literacy in Nigerian Prisons. Int. J. Humanit. Soc. Sci. Educ. IJHSSE 1, 139–148 (2014).
Pimenta, J. et al. Opportunistic screening for genital chlamydial infection. I: Acceptability of urine testing in primary and secondary healthcare settings. Sex. Transm. Infect. 79, 16–21 (2003).
Hesse, E. A. et al. Feasibility and acceptability of point-of-care testing for sexually transmissible infections among men and women in mobile van settings. Sex. Health 12, 71–73 (2014).
McFadyen, J. & Rankin, J. The role of gatekeepers in research: Learning from reflexivity and reflection. GSTF J. Nurs. Health Care JNHC 4, 82–88 (2016).
Apa, Z. L. et al. Challenges and strategies for research in prisons. Public Health Nurs. 29, 467–472 (2012).
Thoele, K., Ferren, M., Moffat, L., Keen, A. & Newhouse, R. Development and use of a toolkit to facilitate implementation of an evidence-based intervention: A descriptive case study. Implement. Sci. Commun. 1, 1–12 (2020).
Mathieson, A., Grande, G. & Luker, K. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: A systematic mixed-studies review and qualitative synthesis. Prim. Health Care Res. Dev. 20, e6 (2019).
Brömdal, A., Mullens, A. B., Phillips, T. M. & Gow, J. Experiences of transgender prisoners and their knowledge, attitudes, and practices regarding sexual behaviors and HIV/STIs: A systematic review. Int. J. Transgenderism 20, 4–20 (2019).
Gale, N. K., Heath, G., Cameron, E., Rashid, S. & Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 13, 1–8 (2013).
Acknowledgements
We would like to acknowledge the following people for providing unwavering support for this research. Without their commitment to improving the health of the incarcerated population, this research would not have been possible. The QCS managerial team; and from Metro North Hospital and Health Service, the site’s Assistant Nursing Director, site Nurse Practitioner, and site Clinical Nurses.
Funding
Funding for this study was received from the Nursing and Midwifery Fellowship (Round 7) which was used to pay the salaries of the nurses that delivered the clinic.
Author information
Authors and Affiliations
Contributions
A.B. conceptualized this study, wrote the manuscript, and prepared all figures and tables. L.E. oversaw the entire study from conceptualization to final draft. A.M. conducted interviews with clinic nurses. A.B. and A.Br. conducted data collection through medical chart audits. A.B., A.M., A.Br., K.K., S.O., and L.E. all contributed to the design, method selection, development, and revision of this study. All authors have reviewed the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Ms ABs was funded by the University of Southern Queensland Research Training Program Stipend Scholarship to aid in the cost of living whilst undertaking this research. She has also received support from the Qld Health Study and Research Assistance Scheme (SARAS) in the form of time to complete the research. Additionally, AB was employed by Qld Health while engaged in the research project. Professor LE, Associate Professor ABr, Professor AM, Adjunct Associate Professor KK, and Professor SO declare no potential competing interest. The authors declare no non-financial competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Balmer, A., Brömdal, A., Mullens, A.B. et al. A nurse-led satellite clinic initiative for STI testing in an Australian correctional center: a qualitative study. Sci Rep 15, 5321 (2025). https://doi.org/10.1038/s41598-025-89468-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89468-1