Abstract
This study aimed to investigate the risk factors for low postoperative blood pressure and construct a machine learning (ML) model based on these features for real-time prediction in patients with oral cancer following reconstruction surgery. The retrospective cohort analysis included adults who had undergone oral cancer resection and free flap reconstruction surgery between December 2022 and December 2023. Patient clinical characteristics were obtained from the electronic medical records. Seven ML techniques were attempted with postoperative hypotension (POH) (mean arterial pressure ˂ 55 mmHg) as the primary outcome. The best-performing ML model was tuned, and the final performance was evaluated using split-set validation, followed by risk factor identification and model interpretability. Of the 727 patients, 412 were finally included, with 66 (16.2%) experiencing POH, resulting in higher inpatient costs and prolonged hospitalization. With an area under the receiver operating characteristic curve of 0.805 (95% confidence interval [CI]: 0.674–0.935), the random forest model demonstrated excellent performance. Shapley additive explanation and feature importance analysis revealed that systolic pressure, heart rate, tumor size, lactic acid level, diastolic pressure, surgical time, total liquid infusion volume, and body mass index were significant risk factors for POH, indicating the robustness of the random forest model.
Similar content being viewed by others
Introduction
Surgical resection has been the mainstay treatment for oral cancers1. However, surgery can result in significant cosmetic deformities and impair oral functions, such as mastication, deglutition, and speech2. The development of a wide range of reconstructive options to improve the quality of life and functionality after ablative surgery is a major advancement in the surgical treatment of oral cancer3. Because of the excellent vascularity and increased rate of partial necrosis of the flap skin island in a pedicled flap, free flap reconstruction is currently the preferred reconstructive process for oral cancer surgery4. However, adverse postoperative outcomes such as flap necrosis and organ dysfunction considerably affect the prognosis and quality of life even after successful surgery4,5.
Hypotension is an independent risk factor for adverse perioperative outcomes6,7. Despite the sophisticated care offered by medical professionals during the postoperative period, which is important for patient recovery, hypotension is frequently an unintended effect. Furthermore, despite its association with substantial patient harm and financial implications8, no studies have investigated the risk factors for postoperative hypotension (POH) across a representative free flap reconstruction surgical population to provide therapeutic relevance to the findings. Therefore, understanding the impact and early recognition of POH on adverse clinical outcomes among postsurgical patients can provide better help formulate strategies for early intervention in oral cancer resection and free flap reconstruction surgery.
Machine learning (ML) is the scientific study of algorithms and statistical models used by computers to complete a certain task without explicit instructions9. In the self-discipline of anesthesiology, multiple machine-learning models have been established to predict clinical outcomes after surgery, with performance comparable to or better than classical modeling10. However, research into the application of these models in the POH is limited.
In this study, we performed a retrospective cohort study on a generalizable cohort of adult patients at a public tertiary hospital to investigate the risk variables for POH after oral cancer resection and free flap reconstruction surgery. We anticipated that, with a comprehensive evaluation of all available perioperative parameters, multiple important variables would be independently associated with POH. Additionally, we hypothesized that critical clinical characteristics can be used to evaluate and build the best-performing prediction ML model, which would vary depending on perioperative risk. These findings may guide the design of future prospective interventional trials aimed at preventing POH.
Methods
Study design
This retrospective observational study was approved by the Research Ethics Committee of Second Xiangya Hospital, Central South University (LYF 20240022, Changsha, China). Research participants were performed in accordance with the Declaration of Helsinki, and each patient provided written informed consent.
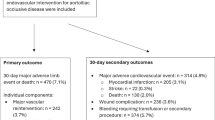
The study design is illustrated in Fig. 1. No intervention measures were involved, and all protected health information except the date of surgery and extremes of age (˃ 80 years) were removed before analysis. The study outcomes, data collection, and statistical methods were established a priori.
Study population
This study included patients who had undergone oral cancer resection and free flap reconstruction surgical procedures at a public tertiary hospital between December 1, 2022, and December 31, 2023. The written informed consent was obtained from all patients before surgery. And the participants were selected based on the availability of the complete data relevant to this study. Adult patients (aged ≥ 18 years) without serious complications such as stage V chronic kidney disease were included. Patients without a history of chemotherapy and/or radiation and those with the availability of complete data were included. In addition, patients who had undergone oral cancer reconstruction surgery were typically admitted to the anesthesia intensive care unit (AICU) for recovery. The final analysis included 412 patients.
Data source
A limited dataset of electronic medical records from inpatient settings was extracted as applicable to this study. To ensure data accuracy, a clinician manually audits random subsets of cases to examine and verify the correctness of the data extraction and its source. Our primary outcome and study endpoint was POH, defined as a mean arterial pressure (MAP) ˂ 55 mmHg in the AICU after oral cancer resection and free flap reconstruction11. MAP values were measured using a blood pressure monitor and computed using the formula [(2 × diastolic blood pressure) + systolic blood pressure]/3, as previously described12.
Patient characteristics
The selected study variables included: (1) preoperative parameters, such as age, sex, height, weight, body mass index (BMI), body surface area (BSA), systolic/diastolic pressure, smoking history, alcohol consumption, Charlson comorbidity index (CCI), reoperation, biochemical data (such as leukocyte count, neutrophil ratio, platelet count, hemoglobin, etc.), hospitalization costs, and length of stay and so on; (2) Anesthetic-surgical factors included the American Society of Anesthesiologists (ASA) grade, emergency status, awake tracheal intubation, surgery time, bleeding, blood transfusion, total liquid intake, use of tracheostomy, and dosage of sufentanil, remifentanil, and midazolam. (3) Postoperative variables, including Pathology related data (tumor size, T classification, lymph node metastasis, and tumor stage), brain natriuretic peptide, lactic acid level, oxygenation index, procalcitonin, and erythrocyte sedimentation rate.
Boruta feature selection
The Boruta method is a feature-selection algorithm based on a random forest (RF) classifier. The purpose of the Boruta model is to select the set of features that are most important to the dependent variable13.
ML models
Because not all ML algorithms provided sufficient internal validation, the data were randomly partitioned into 70/30 training and test sets. Specifically, 70% of the data were used to train the ML models, and 30% were used as the test set14. The ML algorithms were trained on the training set in any order, and ten-fold cross-validation was repeated three times to reduce initial overfitting. Owing to concerns regarding how different ML models handle class imbalances, the area under the receiver operating characteristic curve was selected as the major performance parameter. Furthermore, threshold-dependent estimates of sensitivity and specificity at the “best” thresholds were calculated for each model. Bootstrap was calculated with 1000 stratified bootstrap repeats using the “pROC” program. The following ML algorithms were trained: logistic regression (LR), support vector machine (SVM), decision tree (DT), RF, extreme gradient boosting (XGBoost), K-nearest neighbor (KNN), and light gradient boosting machine (LightGBM).
Statistical analyses
Continuous data with a normal distribution are presented as means and standard deviations, and non-normally distributed variables are presented as medians and interquartile ranges. Categorical data are presented as numbers and frequencies (%). Categorical variables were compared using the χ2 or Fisher exact test with Yates adjustments. Student’s t-tests were used to compare continuous variables. The association between POH thresholds and outcomes was assessed using two-tailed hypothesis testing. Patients who met the selection criteria were randomly divided into two cohorts: derivation and validation. Adjusted odds ratios and 95% confidence intervals (CIs) were used to measure the effect size. All statistical analyses, ML model creation and image production were performed using SPSS 24.0 (IBM Corp., Armonk, NY, USA), and GraphPad Prism 8.0 (La Jolla, CA, USA) and R version 4.3.3 (version 4.2.1, R Core Team, Vienna, Austria). Statistical significance was defined as p < 0.05.
Results
Study cohort and patient characteristics
Of the 727 patients who had undergone surgical intervention, free flap reconstruction surgery was not performed in 156, and continuous arterial blood pressure was not monitored and recorded in 47 patients. In total, 412 individuals (average age of 54.2 ± 11.0 years) who met the study requirements were included in the final analysis (Fig. 1). Among them, POH was reported in 66 (16.2%) patients. Baseline and demographic characteristics based on the POH events are summarized in Supplementary Table 1.
Association between POH and healthcare expenditure
The effect of POH on hospitalization costs and postoperative duration of stay was analyzed. Hospitalization costs (99406.2 vs. 91856.4; P < 0.01) and duration of stay (10.7 vs. 9.3; P < 0.001) were higher among patients with POH than in those without POH (Fig. 2A and B).
POH risk model derivation and validation using RF algorithm
Parameters influencing POH occurrence were determined using the Boruta technique, which identified the following 10 risk factors: sodium, surgical time, partial pressure of CO2, heart rate, weight, diastolic pressure, BSA, liquid consumption, tumor size, and systolic pressure (Fig. 3A and B).
Variable shrinkage and selection using the Boruta algorithm. (A), Boruta feature selection model identified 10 of the 50 variables that demonstrated a strong association with POH. The horizontal axis displays the number of variables, while the vertical axis shows the root mean square error value of each variable. (B), Classifier run of Boruta analysis. Every curve represents the Z-value of each variable in the model calculation.
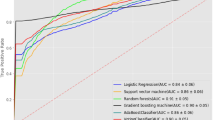
Using the selected variables, seven ML models were developed. After training, the model run on the test set had an area under the receiver operating characteristic curve of 0.726 (95% CI, 0.596–0.847), 0.805 (95% CI, 0.674–0.935), 0.635 (95% CI, 0.506–0.764), 0.716 (95% CI, 0.588–0.844), 0.744 (95% CI, 0.667–0.820), 0.612 (95% CI, 0.468–0.755), and 0.691 (95% CI, 0.563–0.819) for DT, RF, LightGBM, SVM, LR, SVM, and XGboost, respectively. Receiver operating characteristic curves and confusion matrix at “best” thresholds for RF method are illustrated in Fig. 4A and B and Supplementary Fig. 1.
Performance of ML models. (A), ROC curves of the seven ML models, the random forest (RF) outperformed all the six other ML models. (B), Confusion matrix of RF. ML, machine learning; ROC: Receiver operating characteristic; KNN: K-nearest neighbours; RF: Random forest; DT: Decision Trees; LR: Logistic regression; SVM: Support vector machine; XGBoost: Extreme gradient boosting; LightGBM: Light Gradient Boosting Machine.
Feature importance evaluation and model interpretability
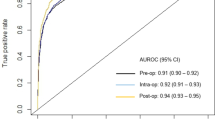
Accepting a prediction model that is not directly explainable and interpretable may not be feasible for the clinicians; therefore, variable importance and Shapley additive explanation (SHAP) analyses were used to identify key risk factors for POH and interpret the final model output by calculating each variable’s contribution to the prediction. The feature importance plot revealed that systolic pressure, heart rate, tumor size, lactic acid, diastolic pressure, surgical time, liquid intake, and BMI were independent predictors of POH in oral cancer resection and free flap reconstructive surgery, which can facilitate the understanding of how a single feature affects the output of the prediction model (Fig. 5A and B). Furthermore, the SHAP explanation analyzes how a particular prediction is created for a specific individual using individualized input data. Figure 6A and B showed specific cases of high- and low-risk POH in oral cancer resection and free flap reconstruction surgery based on different features, respectively.
Feature importance evaluation based on the RF. (A) Summary plots of SHAP values based on the RF. The size of the dots shows the magnitude of the feature’s impact, with larger dots denoting a stronger impact. (B) Feature importance plot based on the RF in terms of accuracy and Gini analysis. A higher value on the X-axis indicates greater importance of the feature in the corresponding model. SHAP: Shapley additive explanation; RF: Random forest.
Constructed SHAP analysis based on the RF for specific individual. (A, B) High-risk (A) and low-risk examples (B) of postoperative low blood pressure in oral cancer resection and free flap reconstruction surgical patients, respectively. The value of f(x) represents the predicted risk of POH for a given sample.
Discussion
In our study, 50 perioperative clinical parameters and seven ML models were investigated and assessed for POH prediction analyses in oral cancer patients undergoing free flap reconstruction surgery. Predictive risk factors were identified, and a prediction model was constructed for patients who required reconstructive surgery using RF models, which outperformed other algorithms, along with clinical and laboratory data easily extracted from the electronic medical record system.
The postoperative period is crucial, and POH in particular has been associated with serious complications15. Khanna et al. reported that increasing levels of hypotension, which were previously considered normal, may predispose to cardiac injury, death, and renal injury in surgical ICU patients16. Tetsuya et al. found that a 5-mm Hg decrease in the lowest MAP was associated with a 28% increase in the risk of acute renal injury following non-cardiac surgery for the lowest MAP < 80 mmHg17. Moreover, a significantly higher rate of postoperative symptomatic hypotension was observed in the abdominal free flap breast reconstruction18. However, to date, no study has analyzed this association in patients undergoing surgeries for oral cancer resection and flap repair. This retrospective study focused on the causes of POH in patients admitted to the AICU undergoing oral cancer reconstructive surgery to facilitate early management. Consistent with previous studies, POH was defined as an MAP less than 55 mmHg.
The data presented establish the intuitive concept that the risk of POH varies according to the underlying patient and procedural parameters. Systolic pressure, heart rate, tumor size, lactic acid level, diastolic pressure, surgical time, total liquid infusion volume, and BMI were predictive variables for POH in oral cancer resection and free flap reconstructive surgery. Alessandro et al. demonstrated that patients with a low preoperative MAP were at an increased risk of POH, which could be attributed to the decreased capacity19. The hormonal activity in the body, liquid capacity, drug use, and a patient’s preoperative MAP are all obviously interrelated, and postoperative recovery takes time. As a result, it is understandable that preoperative MAP has been noticed to be a significant predictor of POH following tumor removal. Furthermore, individuals undergoing free flap reconstruction surgery are more likely to have large tumors that require longer surgical process, which may result in greater fluid and/or blood loss. Another study proposed preoperative heart rate variability as a predictor of perioperative outcomes because it can provide information on preexisting comorbidities and physiological status as well as dynamic observation of physiological interactions with perioperative events20. Moreover, the increase in arterial lactate in hemodynamically unstable individuals is related to shock and was a predictor of prolonged hospitalization, and lower BMI was an independent predictor of the occurrence of hypotension21. Interestingly, the patient’s total liquid infusion volume was independently correlated with POH. One possible reason for these findings is that preoperative variables such as surgical time and BMI, associated with the total liquid infusion volume, demonstrated stronger independent correlations with POH. Additionally, studies have suggested that the POH may be influenced by the surgeon’s experience or expertise. However, as surgical proficiency improves and plateaus, the rate of reoperations due to flap necrosis in our facility remains quite low22.
Our findings highlighted the reliability and interpretability of the RF algorithm in predicting the POH risk. Certain ML algorithms have been applied in perioperative treatment, such as predicting sepsis, acute renal injury following cardiac surgery, and postoperative adverse events23,24. Given their superior performance in ensemble learning, RF algorithms outperform other models in predicting mortality among patients with myocardial infarction undergoing cardiac surgery25,26. To date, only one study has demonstrated that RF model exhibits the best predictive performance, with an accuracy of 90% in preventing intraoperative hypotension during cesarean section surgery27. However, to our knowledge, no studies have analyzed the application of RF algorithms to predict POH in surgical operations, especially in patients with oral cancer who underwent free flap reconstruction surgery. In this study, with an area under the receiver operating characteristic curve of 0.805 (95% CI: 0.674–0.935), the RF model outperformed the other six ML models. Furthermore, the SHAP explanation was analyzed based on the RF analysis to determine high- and low-risk POH predictions for individual patients. Overall, our data suggest the potential for aggressive real-time monitoring or to trigger an alert to notify clinicians of early intervention in oral cancer resection and free flap reconstruction surgery.
This study had certain limitations. First, this single-center study used a dataset extracted over a one-year period. Utilizing a larger dataset with a longer timeframe could have yielded slightly different results, as clinical practice may have evolved over the duration of the study. Second, because this was a retrospective study, several features closely associated with POH were not easily available as discrete values in the electronic health records for incorporation into the model. For example, the postoperative wound drainage volume, free flap necrosis, details of airway management, and preoperative laboratory values may have improved the discrimination and clinical value of the model. Finally, considering the intermittent recording of MAP, there was the potential for unstable MAP readings and potentially missing instances of POH, especially during the night shifts with relatively fewer staff. Further prospective studies with larger sample sizes are warranted.
Conclusion
The incidence of POH in patients undergoing inpatient oral cancer resection and free flap reconstruction surgical procedures is 16.2%. An explainable RF model was successfully developed to predict POH based on clinical data that were easily extracted from electronic health systems. Notably, the SHAP explanation based on RF analyzes how specific predictions were made for individual patients by integrating personalized input data. Our findings will enable the triggering of an alert to notify clinicians for early intervention and could help guide the design of future prospective interventional trials aimed at preventing POH.
Data availability
The data used to support the findings of this study are included within the article.
References
Ranganath, K., Jalisi, S. M., Naples, J. G. & Gomez, E. D. Comparing outcomes of radial forearm free flaps and anterolateral thigh free flaps in oral cavity reconstruction: a systematic review and meta-analysis. Oral Oncol. 135, 106214. https://doi.org/10.1016/j.oraloncology.2022.106214 (2022).
Quadri, P. & McMullen, C. Oral Cavity Reconstruction. Otolaryngol. Clin. North. Am. 56, 671–686. https://doi.org/10.1016/j.otc.2023.04.002 (2023).
Gilbert, R. W. Reconstruction of the oral cavity; past, present and future. Oral Oncol. 108, 104683. https://doi.org/10.1016/j.oraloncology.2020.104683 (2020).
Wang, S., Yin, S., Zhang, Z. L., Su, X. & Xu, Z. F. Quality of life after oral Cancer Resection and Free Flap Reconstruction. J. Oral Maxillofac. Surg. 77, 1724–1732. https://doi.org/10.1016/j.joms.2019.02.029 (2019).
Choi, N., Park, S. I., Kim, H., Sohn, I. & Jeong, H. S. The impact of unplanned reoperations in head and neck cancer surgery on survival. Oral Oncol. 83, 38–45. https://doi.org/10.1016/j.oraloncology.2018.06.004 (2018).
McEvoy, M. D. et al. Perioperative Quality Initiative consensus statement on postoperative blood pressure, risk and outcomes for elective surgery. Br. J. Anaesth. 122, 575–586. https://doi.org/10.1016/j.bja.2019.01.019 (2019).
Mezue, K., Goyal, A., Pressman, G. S., Horrow, J. C. & Rangaswami, J. Blood pressure variability predicts adverse events and Cardiovascular outcomes in chronic kidney disease: a post-hoc analysis of the SPRINT Trial. Am. J. Hypertens. 31, 48–52. https://doi.org/10.1093/ajh/hpx128 (2017).
Maheshwari, K. et al. Association between Perioperative Hypotension and Delirium in Postoperative critically ill patients: a retrospective cohort analysis. Anesth. Analg. 130, 636–643. https://doi.org/10.1213/ane.0000000000004517 (2020).
Kaneko, H. et al. Machine learning-based models for predicting clinical outcomes after surgery in unilateral primary aldosteronism. Sci. Rep. 12, 5781. https://doi.org/10.1038/s41598-022-09706-8 (2022).
Rellum, S. R. et al. Effect of the machine learning-derived Hypotension Prediction Index (HPI) combined with diagnostic guidance versus standard care on depth and duration of intraoperative and postoperative hypotension in elective cardiac surgery patients: HYPE-2 - study protocol of a randomised clinical trial. BMJ open. 13, e061832. https://doi.org/10.1136/bmjopen-2022-061832 (2023).
Salmasi, V. et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or Absolute Thresholds, and Acute kidney and myocardial Injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology 126, 47–65. https://doi.org/10.1097/aln.0000000000001432 (2017).
Kendale, S., Kulkarni, P., Rosenberg, A. D. & Wang, J. Supervised machine-learning Predictive Analytics for Prediction of Postinduction Hypotension. Anesthesiology 129, 675–688. https://doi.org/10.1097/aln.0000000000002374 (2018).
Zhou, H., Xin, Y. & Li, S. A diabetes prediction model based on Boruta feature selection and ensemble learning. BMC Bioinform. 24, 224. https://doi.org/10.1186/s12859-023-05300-5 (2023).
Muñoz, A. J. et al. Development of a predictive model of venous thromboembolism recurrence in anticoagulated cancer patients using machine learning. Thromb. Res. 228, 181–188. https://doi.org/10.1016/j.thromres.2023.06.015 (2023).
Sessler, D. I. et al. Period-dependent associations between Hypotension during and for four days after noncardiac surgery and a composite of myocardial infarction and death: a Substudy of the POISE-2 trial. Anesthesiology 128, 317–327. https://doi.org/10.1097/aln.0000000000001985 (2018).
Khanna, A. K. et al. Association between Mean arterial pressure and acute kidney Injury and a Composite of Myocardial Injury and Mortality in Postoperative critically ill patients: a retrospective cohort analysis. Crit. Care Med. 47, 910–917. https://doi.org/10.1097/ccm.0000000000003763 (2019).
Shimada, T. et al. Association between postoperative hypotension and acute kidney injury after noncardiac surgery: a historical cohort analysis. Can. J. Anaesth. 70, 1892–1900. https://doi.org/10.1007/s12630-023-02601-4 (2023).
Anolik, R. A. et al. Occurrence of symptomatic hypotension in patients undergoing breast free flaps: is enhanced recovery after surgery to blame? Plast. Reconstr. Surg. 145, 606–616. https://doi.org/10.1097/prs.0000000000006537 (2020).
Parente, A. et al. Risk factors for postoperative hypotension after adrenalectomy for phaeochromocytoma: derivation of the PACS risk score. Eur. J. Surg. Oncol. 49, 497–504. https://doi.org/10.1016/j.ejso.2022.10.006 (2023).
Frandsen, M. N., Mehlsen, J., Foss, N. B. & Kehlet, H. Preoperative heart rate variability as a predictor of perioperative outcomes: a systematic review without meta-analysis. J. Clin. Monit. Comput. 36, 947–960. https://doi.org/10.1007/s10877-022-00819-z (2022).
Souza, S. P. et al. Arterial lactate as a predictor of postoperative complications in head and neck squamous cell carcinoma. Braz J. Otorhinolaryngol. 88 (Suppl 1), S97–s101. https://doi.org/10.1016/j.bjorl.2021.04.008 (2022).
Gong, Z., Zhang, S., Chen, C., Zhi, Y. & Zi, M. Reconstruction of Complex lateral Skull Base defects after oral Cancer Resection with Individualized Anterolateral Thigh Flap. Front. Oncol. 11, 743370. https://doi.org/10.3389/fonc.2021.743370 (2021).
Tseng, P. Y. et al. Prediction of the development of acute kidney injury following cardiac surgery by machine learning. Crit. Care. 24, 478. https://doi.org/10.1186/s13054-020-03179-9 (2020).
D’Ascenzo, F. et al. Machine learning-based prediction of adverse events following an acute coronary syndrome (PRAISE): a modelling study of pooled datasets. Lancet 397, 199–207. https://doi.org/10.1016/s0140-6736(20)32519-8 (2021).
Zakariazadeh, A. Smart meter data classification using optimized random forest algorithm. ISA Trans. 126, 361–369. https://doi.org/10.1016/j.isatra.2021.07.051 (2022).
Allyn, J. et al. A comparison of a machine learning model with EuroSCORE II in Predicting Mortality after Elective Cardiac surgery: a decision curve analysis. PLoS One. 12, e0169772. https://doi.org/10.1371/journal.pone.0169772 (2017).
Yang, X., Li, Y. M., Wang, Q., Li, R. & Zhang, P. Machine learning model based on RCA-PDCA nursing methods and differentiating factors to predict hypotension during cesarean section surgery. Comput. Biol. Med. 174, 108395. https://doi.org/10.1016/j.compbiomed.2024.108395 (2024).
Acknowledgements
We would like to thank the staff of the department of anesthesiology in Second Xiangya Hospital of Central South University who helped make this study possible.
Funding
This study was supported by the Natural Science Foundation of Hunan Province (2022JJ70061), the Key Fund Project of Hunan Provincial Department of Education (22A0011), the National Natural Science Foundation of China (82103641 and 82071347) and Health Research Project of Hunan Provincial Health Commission (W20243113).
Author information
Authors and Affiliations
Contributions
SZ, YZ and RD contributed to the study design. XO and HL contributed to data collection, manuscript writing, data processing, and figure mapping. YZ, HL and RD contributed to data proofreading. SZ and YZ contributed to formal analysis; and writing-original draft preparation; RD and SZ contributed to review and editing. All authors reviewed the manuscript. All author read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Second Xiangya Hospital, Central South University, Changsha, China (LYF 20240022). All patients participating in this study voluntarily provided informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, S., Zhang, Y., Ouyang, X. et al. Random forest algorithm for predicting postoperative hypotension in oral cancer resection and free flap reconstruction surgery. Sci Rep 15, 5452 (2025). https://doi.org/10.1038/s41598-025-89621-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-89621-w
Keywords
This article is cited by
-
Machine learning to predict the role of CHWs in shifting birth preferences away from homebirth in India
Scientific Reports (2025)