Abstract
To explore the risk factors related to perioperative neurocognitive disorders (PND) in elderly patients with hip fractures, with perioperative acute pain management as the core. This study used a retrospective case-control study method. 90 elderly patients who underwent artificial femoral head replacement or total hip replacement surgery in our hospital from 2022 to 2023 were collected, and divided into PND group and non-PND group based on the occurrence of PND. Collected data on 17 factors and conducted univariate and multivariate regression analysis to analyze the risk factors and contribution value of PND in elderly patients with hip fractures. Univariate analysis showed that compared with the non-PND group, patients in the PND group showed a significant increase in age, higher ASA class, longer surgical time, increased number of nerve block cases, increased postoperative 12 h visual analogue scale (VAS) scores, increased postoperative 24 h VAS scores, and increased levels of CRP, PCT, and BL-6 (P < 0.05). Multivariate regression analysis found that the risk factors for PND were postoperative 12 h VAS scores, postoperative 24 h VAS scores, CRP, PCT, and BL-6. The protective factors were ASA class III and ASA class II. The risk factors for PND in elderly patients undergoing hip fracture surgery included postoperative 12 h VAS scores (OR = 3.356), postoperative 24 h VAS scores (OR = 2.311), CRP (OR = 1.058), PCT (OR = 18.661), and BL-6 (OR = 1.061). The protective factors were ASA class III (OR = 0.039) and ASA class II (OR = 0.016).
Similar content being viewed by others
Introduction
The inexorable march of demographic aging is a reality. With the ongoing aging of a nation’s populace, there is a corresponding rise in the need for surgical interventions. More than one-third of elective surgeries are performed on elderly people, and this proportion will increase with the aging population1,2. As elderly people increasingly rely on surgical treatment, preventing PND, including postoperative delirium, delayed neurocognitive recovery, and postoperative neurocognitive disorders, has become a hot topic in perioperative research3,4. Fractures frequently occur in geriatric patients, with hip fractures being colloquially known as the final fracture one experiences in their lifetime. Perioperative management, especially pain management, is of great significance in elderly fracture surgery. The relationship between pain and PND, as well as the changes in this relationship through pain treatment, are very complex. Inflammation and pain are closely related in biochemistry5,6,7. The clinical evidence related to pain and PND mainly involves acute postoperative pain8,9,10. Adequate diagnosis and management of pain is a core intervention measure during the perioperative period, and is recommended in the consensus guidelines of multiple interdisciplinary working groups to reduce postoperative delirium. Therefore, this study intends to adopt a case-control study, with perioperative acute pain management as the core, to explore the risk factors related to PND in elderly patients with hip fractures.
Materials and methods
Research object
This study adopted a retrospective case-control study method. The study followed the guidelines outlined in the Declaration of Helsinki and passed the Medical Ethics Committee of Provincial People’s Hospital review standard (No.2021035), and informed consent was obtained from the study participants. The study collected 90 elderly patients who underwent artificial femoral head replacement or total hip replacement surgery in our hospital from 2022 to 2023, including 33 patients with PND and 57 patients without PND. Preop cognitive function assessment was 1 day before surgery and the postop 48 h after surgery. According to the presence or absence of PND, they were divided into PND group (n = 33) and non-PND group (n = 57).
Diagnosis, inclusion, exclusion, and removal criteria
Diagnostic criteria for PND: defined as a decrease of ≥ 2 points in postoperative mini mental state examination (MMSE) scores compared to preoperative11.
Inclusion criteria: (1) Elderly patients underwent artificial femoral head replacement or artificial total hip replacement surgery; (2) The clinical data was complete. Exclusion criteria: patients with preoperative delirium or severe neurocognitive disorder, inability to cooperate with neuropsychological and scoring tests for any reason (severe visual, auditory, or language communication disorders), concomitant central nervous system or psychiatric disorders, severe liver and kidney dysfunction or other systemic lesions, long-term alcoholism, or a history of dependence on psychotropic drugs. Removal criteria: If there was a large amount of bleeding exceeding 800 ml during the surgery, blood transfusion was required, or the surgery time exceeded 2 h, serious drug allergy events and other unexpected serious adverse events occurred.
ASA class
Class I: Physically healthy, well developed and nourished, with normal organ functions; Class II: Except for surgical diseases, there were mild comorbidities and functional compensation wass sound; Class III: Severe coexisting condition, limited physical activity, but still able to cope with daily activities; Class IV: Severe comorbidities, loss of daily activity ability, and frequent life-threatening situations; Class V: Near death patients whose life was difficult to maintain for 24 h, regardless of surgery or not; Class VI: Confirmed as brain death, with organs intended for organ transplantation surgery.
Nerve block methods
Iliac fascia block was performed by placing the patient in a flat supine position. After disinfecting and spreading the tissue at the puncture site, an improved iliac fascia gap puncture method was used. The high-frequency ultrasound probe was placed parallel to the inguinal ligament to identify important anatomical landmarks such as the femoral artery, femoral nerve, fascia lata, iliac fascia, and iliopsoas muscle. The probe was rotated and placed 1/3 of the line between the pubic tubercle and the anterior superior iliac spine to search for the “hourglass sign”. The iliopsoas muscle can be identified as located below the sartorius and internal oblique muscles, with the iliac fascia covering above the iliopsoas muscle. Firstly, 2 ml of 2% lidocaine was used for local infiltration anesthesia at the insertion point. Then, the puncture needle was inserted using an in plane technique from the tail end to the head end, passing through the iliac fascia. After no abnormalities were found in the syringe’s suction, 1-2 ml of physiological saline was injected to confirm that the puncture needle tip was located between the iliac fascia and the iliopsoas muscle. Then, 0 33% ropivacaine 30 ml was injected, it can be seen that the iliac fascia and iliopsoas muscle are separated by local anesthesia.
VAS scoring criteria
The basic method was to use a vernier ruler about 10 cm in length, with 10 scales on one side, and two ends marked with “0” and “10” respectively. A score of 0 represented painlessness, and a score of 10 represented the most severe pain that was unbearable.
Outcome measures
Gender, age, ASA class, surgical type, surgical duration, anesthesia method, presence or absence of nerve block, time to ground, length of hospitalization, postoperative 6 h VAS scores, postoperative 12 h VAS scores, postoperative 24 h VAS scores, postoperative 48 h VAS scores, presence or absence of lower limb thrombosis, CRP, PCT, and BL-6.
Statistics
SPSS 23.0 statistical software was used for analysis. Measurements were expressed as mean ± standard deviation (\(\:\stackrel{-}{X}\)±S), and univariate analysis used either an independent sample t-test or a rank test. Count data were expressed as percentages (n%), and the univariate analysis used χ2test. The multivariate analysis used the logisic regression model. A level of P < 0.05 was considered as significant.
Results
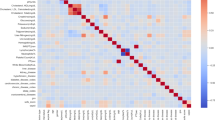
Assignment of PND related risk factors
In order to explore the risk factors related to PND, this study collected 90 elderly patients who underwent artificial femoral head replacement or artificial total hip replacement surgery in our hospital from 2022 to 2023 for a case-control study. Among them, 33 patients had PND and 57 patients did not. We collected data on 17 factors, including gender, age, ASA class, surgical type, surgical duration, anesthesia methods, presence or absence of nerve block, time to ground, length of hospitalization, postoperative 6 h VAS scores, postoperative 12 h VAS scores, postoperative 24 h VAS scores, postoperative 48 h VAS scores, presence or absence of lower limb thrombosis, CRP, PCT, and BL-6. The assigned values of each factor were shown in Table 1.
Single factor analysis of exposure factors related to PND
The univariate analysis of exposure factors for patients in the PND and non-PND groups was shown in Table 2. Among the 17 related factors, there were no statistically significant difference between the two groups in gender, surgical type, anesthesia method, time to ground, length of hospitalization, postoperative 6 h VAS scores, postoperative 48 h VAS scores, and presence or absence of lower limb thrombosis. Compared with the non-PND group, patients in the PND group showed a significant increase in age, higher ASA class, longer surgical duration, decreased number of nerve block cases, increased postoperative VAS scores at 12 h and 24 h, and increased levels of CRP, PLA, and BL-6 (P < 0.05).
Regression analysis of PND related factors
As shown in Table 2, the factors that showed differences between the two groups included age, ASA grading, surgical duration, presence or absence of nerve block, postoperative 12 h VAS scores, postoperative 24 h VAS scores, CRP, PLA, and BL-6. The above factors were included in the regression analysis. As shown in Table 3, according to the test criterion of α = 0.05, among the statistically significant factors, the risk factors were postoperative 12 h VAS scores, postoperative 24 h VAS scores, CRP, PLA, and BL-6, while the protective factors were ASA class III and ASA class II. Patients with a high postoperative 12 h VAS scores had a more than 3-fold increase in odds ratio (OR), with a high postoperative 24 h VAS scores had a more than 2-fold increase in OR, with high postoperative CRP had a more than 1-fold increase in OR, with high postoperative PCT had a more than 18-fold increase in OR, and with high postoperative BL-6 had a more than 1-fold increase in OR. The OR of patients with ASA class III and ASA class II was less than 1, which was a protective factor.
Comprehensive testing of the logistic regression model was conducted by using Omnibus Tests of Model Coefficients. In this study, P < 0.001 indicated that in the fitted model, at least one of the included variables had a statistically significant OR value, indicating that the model had overall significance. Used the Hosmer and Lemeshow Test to test the goodness of fit of the logistic regression model. In this study, P = 0.268 (i.e. P > 0.05), with a P-value not less than the test level, indicating that the information in the current data had been fully extracted and the model had a high goodness of fit. The prediction accuracy of the logistic regression model: The percentage of accurate observations after reclassification with a cutoff value of 0.500, calculated as the overall prediction accuracy was 87.6%.
Discussion
PND includes postoperative delirium, delayed neurocognitive recovery, and postoperative neurocognitive impairment3,4. Postoperative delirium is defined as an acute fluctuation disorder of attention and consciousness, with an incidence rate of up to 50% in elderly patients and is associated with additional hospitalization costs, higher risk of long-term cognitive impairment, and adverse functional outcomes12,13. Delayed neurocognitive recovery (diagnosed within 30 days after surgery) and postoperative neurocognitive impairment (diagnosed within 3–12 months) are characterized by cognitive deficits in memory and executive function, and are considered key obstacle factors affecting optimal postoperative functional recovery14,15. The relationship between pain and PND, as well as the changes made to this relationship through pain treatment, is very complex. This study adopted a case-control study, with perioperative acute pain management as the core, to explore the risk factors related to PND in elderly patients with hip fractures. A total of 17 factors were included, and factors with statistical differences in univariate analysis were included in logistic regression analysis to explore the contribution of relevant risk factors to PND.
The clinical evidence related to pain and PND mainly involves acute postoperative pain. In a cohort study of 541 elderly patients with hip fractures, it was found that patients with complete cognitive function who experienced any severe postoperative pain at rest on the third day after surgery had a 9-fold increased risk of subsequent delirium8. In a study involving 361 patients with an average age of 66 years who underwent large-scale non cardiac hand surgery, it was found that postoperative resting pain was significantly associated with subsequent postoperative delirium9. In a similar population, patients with higher postoperative pain levels had a significantly higher incidence of postoperative delirium compared to patients with lower pain levels, and patients receiving high-dose opioid drugs had a significantly higher incidence of delirium10. On the contrary, in 89 elderly patients who underwent abdominal surgery, no significant correlation was found between uncontrolled pain and delirium16. This study found that there was no statistically significant difference in VAS scores between the two groups at 6 h and 48 h after surgery. However, an increase in VAS scores at 12 h and 24 h after surgery was a risk factor for PND. 0–3 means mild pain, 4–6 moderate pain, ≧7 severe pain in the VAS scores. Postoperative 12 h VAS scores, PND group (4.36 ± 1.22) vs. non-PND group (3.61 ± 0.98) P = 0.002; Postoperative 24 h VAS scores, PND group (3.97 ± 1.26) vs. non-PND group (3.28 ± 1.32) P = 0.017. There were statistically significant differences between the two groups. And from the mean analysis, although the difference of less than 1 point, the two groups differed from moderate pain. We believe that, there was relevant difference in clinical practice. Patients with high VAS scores at 12 h after surgery had a more than 3-fold increase in OR, while patients with high VAS scores at 24 h after surgery had a more than 2-fold increase in OR. It is speculated that early postoperative acute pain may be a risk factor for PND, and the body may release various inflammatory mediators during pain to participate in the occurrence and development of PND.
Inflammation and pain are closely related in biochemistry, with many mediators involved in the damage and inflammatory response of the human peripheral and central nervous systems, and elevated in pain conditions, such as prostaglandins, bradykinin, interleukin, and tumor necrosis factor-α5. This study found that there were differences in inflammatory factors such as PCT, CRP, and BL-6 between patients with and without PND. Compared with the PND group, patients in the non-PND group showed significant increases in CRP, PCT, and BL-6. Subsequent multivariate regression analysis found that patients with high postoperative CRP had an advantage ratio of more than double, patients with high postoperative PCT had an advantage ratio of more than 18 times, and patients with high postoperative BL-6 had an advantage ratio of more than double. In current clinical practice, PCT, CRP, and BL-6 are mainly used for early detection of systemic bacterial infections. Effective diagnosis of bacterial infections enables clinical doctors to initiate antibiotic treatment in a timely manner to prevent abuse and overuse of antibiotics17. In addition, the severity of the disease is positively correlated with elevated serum levels of PCT, especially in sepsis patients, and therefore has prognostic value18. Inflammatory markers refer to proteins whose content suddenly increases in the body when the body is subjected to inflammatory stimuli such as microbial invasion or tissue damage. They play an important role in monitoring the activity and severity of inflammatory diseases, observing treatment effects, and so on. Inflammatory markers are closely related to pain assessment and pain treatment. Inflammatory mediators can stimulate nerve endings, leading to feelings of pain. An animal experimental study pointed out that once inflammatory cytokines, caused by postoperative acute pain, entered the central nervous system, they activated microglia, which further released various pro-inflammatory cytokines, forming a positive feedback amplification mechanism that exacerbated neuronal damage and led to PND19.A narrative review key findings highlighted neuroinflammation, oxidative stress, mitochondrial dysfunction, neurotransmitter imbalances, microvascular changes, and white matter lesions as central to PND pathophysiology, with particular parallels to encephalocele- and sepsis-associated cognitive impairments20. Among these, neuroinflammation, emerged as a pivotal driver, triggering cascades that exacerbate neuronal injury. Oxidative stress and mitochondrial dysfunction synergistically amplify these effects, while neurotransmitter imbalances and microvascular alterations, including white matter lesions, contribute to synaptic dysfunction and cognitive decline20.The patients included in this study did not experience systemic bacterial infections. Considering that the increase in inflammatory mediators mentioned above may be related to fractures and surgical trauma, Yang et al.21 found that the expression of PCT, CRP, and IL-6 in the serum of patients with traumatic shock increased, and the higher the expression level, the worse the prognosis. Therefore, effective perioperative pain management may suppress the inflammatory response caused by diseases and surgical trauma, which is of great significance for preventing PND. Overall, the notion that poorly controlled acute postop pain is an independent risk factor of cognitive dysfunction and many other conditions, especially in elderly, is already known. The idea of effectively managing pain in the preoperative setting is very important, as mentioned. Elevated inflammatory markers are likely not just a result of pain, but in effect, people might experience more or less pain as a result of different (increased) levels of inflammatory response and markers that are present before and after surgery/trauma and that may predispose them to have worse pain.
Appropriate nerve block techniques are very effective for postoperative pain control. A study randomly divided 207 patients at moderate or high risk of delirium who underwent hip fracture surgery into an iliac fascia block group and a sham block group. Upon admission, iliac fascia block or sham block was administered, repeated every 24 h until delirium occurred or discharged. It was found that the use of iliac fascia block significantly reduced the incidence of delirium; In addition, patients receiving iliac fascia block had lower severity of delirium and shorter duration of delirium22. A cohort study of 85 patients undergoing total knee arthroplasty showed that compared to patient controlled analgesia (PCA) alone, the use of femoral nerve analgesia on the basis of PCA was associated with a lower incidence of postoperative delirium; After controlling preoperative cognitive function, the probability of postoperative delirium in the PCA group was significantly higher than that in the group except for the PCA femoral nerve block23. This study found that compared with the PND group, the non-PND group had a significantly higher rate of nerve block, with a significant decrease in VAS at 12 and 24 h after surgery. However, multivariate regression analysis found that although the increase in VAS scores at 12 and 24 h after surgery was a risk factor for PND, there was no statistical significance in the impact of nerve block acceptance on PND. It is speculated that the sample size may be small, and further exploration can be conducted by increasing the sample size in the future.
In addition, univariate analysis found that the ASA grading of patients in the PND group was significantly higher. Multivariate regression analysis found that the OR of patients with ASA grading III and ASA grading II was less than 1. As a protective factor, ASA class is the overall evaluation of preoperative status of patients. Triggered from the perspective of inflammation and stress status, patients with high ASA class had relatively higher levels of inflammatory response, further supplementation indicating that controlling inflammation levels is of great significance for preventing PND. Besides, in this study, univariate analysis found that compared with the non-PND group, patients in the PND group had a significant increase in age and surgery duration. However, in multivariate regression analysis, the impact of the two on PND was not statistically significant. It is speculated that the sample size may be small, and further exploration can be conducted by increasing the sample size in the future. The detection of the model in this study found that the model is generally meaningful, with high goodness of fit, and an overall prediction accuracy of 87.6%.
The potential underlying mechanisms of postoperative neurocognitive disorders (PND) are complex and multifaceted. Surgery and anesthesia can trigger neuroinflammation, which is characterized by the release of pro-inflammatory cytokines and the activation of microglia and astrocytes. This inflammation can disrupt neuronal function and contribute to cognitive decline24. The generation of reactive oxygen species (ROS) during surgery and anesthesia can lead to oxidative stress, causing mitochondrial damage and further exacerbating neuroinflammation25. Mitochondria play a crucial role in neuronal function due to their involvement in energy metabolism. Surgery and anesthesia can induce mitochondrial dysfunction, affecting ATP production, mitochondrial membrane potential, and calcium buffering, which can lead to impaired neuronal function and cognitive decline25. Changes in synaptic plasticity and neurotransmitter imbalances can occur following surgery, affecting memory and cognitive abilities25. Autophagy is essential for maintaining cellular health by clearing damaged components. Disruptions in autophagy can contribute to the accumulation of damaged proteins and organelles, potentially leading to cognitive impairment26. The blood-brain barrier (BBB) is crucial for maintaining the brain’s microenvironment. Surgery and anesthesia can affect the integrity of the BBB, allowing peripheral immune cells and molecules to access the CNS and contribute to neuroinflammation27. Emerging evidence suggests that the gut microbiota can influence brain function and behavior, and changes in this axis following surgery may contribute to cognitive decline26. Neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), are essential for neuronal survival and function. Reduced levels of these factors following surgery may contribute to cognitive impairment26. These mechanisms highlight the complexity of PND and suggest that a combination of factors, including surgical trauma, anesthesia, and individual patient characteristics, contribute to the development of postoperative cognitive dysfunction. Understanding these mechanisms is crucial for developing effective prevention and treatment strategies for PND.
Due to the limitations of experimental conditions and time in this study, there are still some shortcomings in the experimental design. The sample size of the experiment is not large enough. The molecular mechanisms underlying the changes in patient pain levels, inflammatory factors, and their relationship with PND are still unclear. Therefore, it is necessary to construct animal models for further exploration.
Moreover, decreased MMSE scores can be attributed to various factors, including preoperative conditions and postoperative complications. preoperative delirium, delirium, physical abnormalities (dementia, prior stroke, or transient ischemic attacks), alcohol abuse, frailty. malnutrition, and vitamin d deficiency can also affect a patient’s cognitive function and lead to lower MMSE scores. These factors highlight the multifaceted nature of cognitive function and the importance of considering a wide range of preoperative and postoperative variables when interpreting MMSE scores.
In summary, the risk factors for PND in elderly patients undergoing hip fracture surgery included postoperative 12 h VAS score (OR = 3.356), postoperative 24 h VAS score (OR = 2.311), CRP (OR = 1.058), PCT (OR = 18.661), and BL-6 (OR = 1.061). The protective factors were ASA class III (OR = 0.039) and ASA class II (OR = 0.016).
Data availability
Data is provided within the related files.
References
Surgery, N. S. A. ; (2010). Available from: https://www.cdc.gov/nchs/nsas/index.htm
Survey, N. H. D. ; (2010). Available from: https://www.cdc.gov/nchs/nhds/index.htm
Evered, L. et al. Recommendations for the Nomenclature of Cognitive Change Associated with Anaesthesia and Surgery-2018[J]. Anesthesiology 129 (5), 872–879 (2018).
Mahanna-Gabrielli, E. et al. State of the clinical science of perioperative brain health: report from the American Society of Anesthesiologists Brain Health Initiative Summit 2018[J]. Br. J. Anaesth. 123 (4), 464–478 (2019).
Naser, P. V., Kuner, R. & Molecular Cellular and Circuit Basis of Cholinergic Modulation of Pain[J]. Neuroscience 387, 135–148 (2018).
Vaurio, L. E. et al. Postoperative delirium: the importance of pain and pain management[J]. Anesth. Analg. 102 (4), 1267–1273 (2006).
Kosar, C. M. et al. Lancet Psychiatry, 1(6): 431–436. (2014).
Morrison, R. S. et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture[J]. J. Gerontol. Biol. Sci. Med. Sci. 58 (1), 76–81 (2003).
Leung, J. M. et al. Does preoperative risk for delirium moderate the effects of postoperative pain and opiate use on postoperative delirium?[J]. Am. J. Geriatr. Psychiatry. 21 (10), 946–956 (2013).
Ganai, S. et al. Adverse outcomes of geriatric patients undergoing abdominal surgery who are at high risk for delirium[J]. Arch. Surg. 142 (11), 1072–1078 (2007).
Mu, D. L. et al. Parecoxib supplementation to Morphine Analgesia decreases incidence of Delirium in Elderly patients after hip or knee replacement surgery: a randomized controlled Trial[J]. Anesth. Analg. 124 (6), 1992–2000 (2017).
Marcantonio, E. R. Delirium in hospitalized older Adults[J]. N Engl. J. Med. 377 (15), 1456–1466 (2017).
Sprung, J. et al. Postoperative delirium in elderly patients is associated with subsequent cognitive impairment[J]. Br. J. Anaesth. 119 (2), 316–323 (2017).
Berger, M. et al. Neurocognitive function after cardiac surgery: from phenotypes to Mechanisms[J]. Anesthesiology 129 (4), 829–851 (2018).
Evered, L. A. & Silbert, B. S. Postoperative cognitive dysfunction and noncardiac Surgery[J]. Anesth. Analg. 127 (2), 496–505 (2018).
Schofield, P. The Assessment of Pain in Older people: UK National Guidelines[J]. Age Ageing. 47 (suppl_1), i1–i22 (2018).
Cleland, D. A., Eranki, A. P. & Procalcitonin in StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.: Treasure Island (FL) ineligible companies. Disclosure: Ambika Eranki declares no relevant financial relationships with ineligible companies. (2023).
Christ-Crain, M. & Müller, B. Biomarkers in respiratory tract infections: diagnostic guides to antibiotic prescription, prognostic markers and mediators[J]. Eur. Respir J. 30 (3), 556–573 (2007).
Zhao, Y. F. et al. TNF-α - mediated peripheral and central inflammation are associated with increased incidence of PND in acute postoperative pain[J]. BMC Anesthesiol. 21 (1), 79 (2021).
Wang, T. et al. Recent advances in the mechanisms of postoperative neurocognitive dysfunction: a narrative Review[J]. Biomedicines 13 (1), 115 (2025).
Li, Y. et al. Application value of procalcitonin, C-reactive protein and interleukin-6 in the evaluation of traumatic shock[J]. Exp. Ther. Med. 17 (6), 4586–4592 (2019).
Mouzopoulos, G. et al. Fascia Iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study[J]. J. Orthop. Traumatol. 10 (3), 127–133 (2009).
Kinjo, S. et al. Does using a femoral nerve block for total knee replacement decrease postoperative delirium?[J]. BMC Anesthesiol. 12, 4 (2012).
Skvarc, D. R. et al. Post-operative cognitive dysfunction: an exploration of the inflammatory hypothesis and novel therapies[J]. Neurosci. Biobehav Rev. 84, 116–133 (2018).
Zhang, Z. et al. Unraveling the role and mechanism of mitochondria in postoperative cognitive dysfunction: a narrative review[J]. J. Neuroinflammation. 21 (1), 293 (2024).
Ye, F., Wei, C. & Wu, A. The potential mechanism of mitochondrial homeostasis in postoperative neurocognitive disorders: an in-depth review[J]. Ann. Med. 56 (1), 2411012 (2024).
Li, Z. et al. Neuroinflammation as the underlying mechanism of postoperative cognitive dysfunction and therapeutic Strategies[J]. Front. Cell. Neurosci. 16, 843069 (2022).
Funding
This work was supported by the Natural Science Basic Research Program of Shaanxi Province(2023-JC-QN-0961)and the Science and Technology Development Incubation Fund of Shaanxi Provincial People’s Hospital (2023YJY-46).
Author information
Authors and Affiliations
Contributions
Yan Cheng and Minmin Yi proposed paper ideas, collected data, organized data, and wrote papers; Jianwei Guo developed assessment indicators, overalled control, and reviewed papers. All authors agree to the publication of the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics committee of Shaanxi Provincial People’s Hospital. The authors confirm that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Written inform consent were obtained from the participants at the beginning of survey.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, J., Cheng, Y. & Yi, M. Analysis of risk factors related to perioperative neurocognitive disorders in elderly patients with hip fractures. Sci Rep 15, 4816 (2025). https://doi.org/10.1038/s41598-025-89633-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-89633-6