Abstract
Rapid assessment of severity is crucial for timely intervention and improved patient outcomes in heatstroke (HS). However, existing biomarkers are limited in their accuracy and accessibility in ER settings. A prospective pilot study was conducted to assess urinary liver fatty acid-binding protein (L-FABP) levels using a point-of-care testing (POCT) upon HS. Severity was estimated using initial Sequential Organ Failure Assessment (SOFA) scores, and outcomes were measured using modified Rankin Scale (mRS) scores. In 78 severe HS patients, semi-quantitative L-FABP measurements were performed in ER and patients were divided as P-group (positive group, L-FABP ≧ 12.5 ng/mL on POCT) and N-group (negative group: L-FABP < 12.5ng/mL, on POCT). urinary L-FABP concentrations were also measured on admission, with a median concentration of 48.3 ng/mL. The positive correlation was observed between urinary L-FABP concentration and pulse rate (r = 0.300, P < 0.01) and lactate (r = 0.259, P < 0.01). The POCT of L-FABP showed promise in predicting severity, as indicated by higher concentrations in patients with higher initial SOFA scores. Furthermore, the comparison between semi-quantitative POCT measurements and urine concentrations of L-FABP measured by enzyme-linked immunosorbent assay (ELISA) revealed significant differences among three POCT groups (POC Range < 12.5 ng/ml, 12.6–100 ng/ml, and 55 > 100 ng/ml, P = 0.001). Additionally, patients in the POCT positive group had significantly worse outcomes at discharge compared to the negative group, although this difference diminished over time. The study demonstrates the feasibility and potential utility of POCT for initial L-FABP in estimating severity in HS patients. This rapid and accessible testing method may aid in early field triage and intervention, ultimately improving patient outcomes in the management of HS.
Similar content being viewed by others
Background
Global warming is one of the critical problems affecting health, society, and the economy1,2,3. High temperatures are linked to an increase in heat-related illnesses and heatstroke (HS), which have significantly impacted the public health system1,2,3. Clinical laboratory data should be monitored to avoid missing severe heatstroke4, however, the accessibility of these laboratory blood examinations are limited in the prehospital settings, like as in the nursing home, sport field, or outside working place5. Even in the settings of emergency room, blood examinations also take a longer time for confirming results. Therefore, further research has focused on finding point-of-care testing (POCT) biomarkers with better accessibility for diagnosing the severity of HS6. Urinary liver fatty acid-binding protein (L-FABP) has been considered a promising biomarker that could predict dehydration, thus reflecting renal ischemic dysfunction2,7. However, more evidence is necessary before it can be applied to evaluate the severity of severe HS and predict the outcome. Also, there is still less information that compare the POCT and ELISA based L-FABP measurement especially for the severe HS2. This prospective, multicenter cohort pilot study aimed to (1) evaluate the performance of POCT for L-FABP compared to the conventional ELISA-based method, and (2) to assess the utility of POCT-based L-FABP as a biomarker for disease severity and outcome in severe heat stroke patients.
Results
Patient characteristics
Seventy-eight patients were enrolled in this study (Table 1). Their median age was 76.0 years. The median initial core body temperature (rectal, esophageal, or bladder temperature) was 39.6 °C. The median initial Sequential Organ Failure Assessment (SOFA) score was 5.0 (interquartile range (IQR), 3.0–9.0). The median initial Acute Physiology and Chronic Health Evaluation (APACHE) II score was 20.0 (15.0–26.0). All patients were categorized as Japanese Association of Acute Medicine (JAAM) grade III (severest category). The main cause of HS was non-exertional (73 cases; 93.6%), and most cases occurred indoors (49 cases; 62.8%).
Treatment in the emergency room
As the initial treatment in the ER, ice-cold crystalloid infusion (mean, 1500 mL) was performed for 74 (84.1%) patients, while gastric lavage with ice-cold water (4 °C; mean, 1000 mL) was performed for 5 (5.7%) patients. Intravascular temperature management (mean target temperature, 36.0 °C) was performed for 26 (29.5%) patients. The median time to reach a target temperature of the active cooling (38.0 °C) was 61.0 min (IQR, 36.0–111.8 min).
Comorbidities
Sixty-six (84.6%) patients had at least one comorbidity, with the total percentages of all patients being: diabetes mellitus, 24.4%; hypertension, 28.2%; and psychological disorders (including schizophrenia, depression, dementia, and alcoholic addiction), 29.5%. None of the patients had chronic renal failure requiring hemodialysis.
Outcome measures
The median modified Rankin Scale (mRS) scores were 3.0 (IQR, 1.0–4.0) at discharge, 2.0 (IQR, 0.0–4.0) at 1 month after onset, and 1.0 (IQR, 0.0-3.3) at 3 months after onset. Forty-seven (60.3%) patients had favorable outcomes at 3 months after onset. Four (5.1%) patients died (mRS score, 6) within 3 months after onset. Thirty-six (46.2%) patients experienced worsening of the ability to perform daily activities from the time before HS onset to 3 months after onset (increased mRS scores). The median L-FABP concentrations of all patients were 48.3 ng/mL (IQR, 15.3-219.7 ng/mL) on the initial measurement.
Comparison of point-of-care testing and patient features
Semi-quantitative L-FABP measurements were performed in ER and patients were divided as P-group (positive group, L-FABP ≧ 12.5 ng/mL on POCT) and N-group (negative group: L-FABP < 12.5ng/mL, on POCT). The background characteristics between the P-group and N-group were compared in Table 2. Serum L-FABP concentration was significantly higher in the P-group compared to the N-group (P vs. N, 170.1 vs. 10.1 ng/mL, p < 0.001). Additionally, the initial SOFA score and APACHE II score were higher in the P-group compared to the N-group (Median initial SOFA: 6.0 vs. 4.0, p = 0.013; Median initial APACHE II: 21.0 vs. 16.0, p = 0.022).
We also compared the initial and discharge SOFA scores using the Wilcoxon signed-rank test in both the L-FABP Positive (L-FABP ≥ 12.5 ng/ml) and Negative (L-FABP < 12.5 ng/ml) groups. In both groups, there was a significant decrease in the SOFA score (P = 0.021 for the Positive group and P = 0.014 for the Negative group).
Correlation between urinary L-FABP and pathophysiological parameters
The concentration of urinary L-FABP exhibited a trend of weak positive correlation with pulse rate (r = 0.300, P < 0.01) and lactate (r = 0.259, P < 0.01).
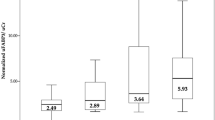
Correlation of POCT L-FABP and the concentrations of L-FABP with ELISA
The L-FABP POC Kit (RENISCHEM®; CMIC, Tokyo, Japan) was designed to distinguish the L-FABP concentrations as high (> 100 ng/ml), medium (12.6–100 ng/ml), or negative (< 12.5 ng/ml) compared to the reference range. The POCT kit distinguished significant differences in the urinary L-FABP concentrations in HS patients (Furthermore, the comparison between semi-quantitative POCT measurements and urine concentrations of L-FABP measured by enzyme-linked immunosorbent assay (ELISA) revealed significant differences among three POCT groups (POC < 12.5 ng/ml: Median 10.1 ng/ml, IQR: 5.6–15.8 ng/ml, POC ≥ 12.5 ng/ml: Median 36.2 ng/ml, IQR: 24.6–58.5 ng/ml and POC > 100 ng/ml: Median 347.9 ng/ml, IQR: 173.1 -857.8 ng/ml, P = 0.001 with ANOVA, supplementary Fig. 1).
The relationship between initial POCT of L-FABP and patients’ outcome
In the N-group, patients demonstrated significantly better functional outcomes at discharge compared to the POCT positive group (mRS 0–2; N-group 62.1% vs. P-group 38.8%, p = 0.046, Fig. 1). However, this disparity diminished by 3 months after the onset of HS, as patients in both groups showed improvement in their recovery (mRS 0–2; N-group 69.0% vs. P-group 55.1%, p = 0.227, Fig. 1).
Comparison of Patient Outcomes between Positive and Negative Point-of-Care Diagnosis Groups. In the negative point-of-care tested group (L-FABP < 12.5 ng/ml), the percentage of favorable outcomes (mRS 0–2) was higher at discharge, 1 month after onset, and 3 months after onset. The percentage of favorable outcomes was significantly higher, especially at discharge. Abbreviations: mRS, modified Rankin Scale.
Initial physiological and pathological biomarkers for predicting long-term outcomes
To evaluate the prognostic potential of long-term (3-month) favorable outcomes, receiver-operating characteristic (ROC) curve analysis was conducted, and the area under the curves (AUCs) were compared for vital signs and urinary L-FABP concentrations (Fig. 2; Table 3). Given the limited scope of clinical examinations in initial emergency room (ER) care for HS patients, we prioritized vital signs and L-FABP due to their higher accessibility and rapid assessment. Among all initial vital signs and accessible biomarkers, the AUC of L-FABP was the largest (AUC = 0.732) in the ROC analysis. This analysis facilitated the determination of the L-FABP cut-off threshold as 28.6 ng/mL (Table 3). For this cut-off threshold, the sensitivity and specificity were 0.659 and 0.600, respectively.
Initial Physiological and Pathological Biomarkers for Predicting Long-term Outcomes. Given the limited scope of clinical examinations in prehospital settings or initial ER care for HS patients, we prioritized vital signs and L-FABP due to their higher accessibility and rapid assessment. Among all initial vital signs and accessible biomarkers, the AUC of L-FABP was the largest (AUC = 0.732) in the ROC analysis. This analysis facilitated the determination of the L-FABP cut-off threshold as 28.6 ng/mL (Table 3).
Discussion
This study elucidates the feasibility of using semiquantitative POCT to measure L-FABP in patients with HS. The measurement of urinary semiquantitative L-FABP shows promise as a tool for predicting the severity of HS and reflecting patient outcomes. The population testing positive for semiquantitative L-FABP (≥ 12.5 ng/mL) demonstrated worse outcomes at discharge. Among the initial physiological and pathological biomarkers assessed in our study, urine quantitative L-FABP measured by ELISA emerged as the most reliable predictor of a favorable outcome at 3 months post-onset.
The need for biomarkers in heatstroke
Global warming is one of the critical problems affecting health, society, and the economy. HS has emerged as a significant health concern worldwide8. Timely assessment of severity, rapid evacuation from hot and humid environments to suitable medical facilities, and prompt initiation of cooling therapy with intensive care are paramount for patients experiencing severe HS6. Thus, early and accurate diagnosis of severe HS is imperative.
Traditionally, the estimation of HS severity has heavily relied on subjective symptoms reported by patients. For instance, Bouchama defined HS based on criteria such as a core body temperature exceeding 40 °C, hot dry skin, and central nervous system abnormalities like delirium, convulsions, or coma9. Moreover, the classification of heat-related illnesses, including heat cramps, heat exhaustion, and HS, predominantly hinges on patient-reported symptoms. Hence, there’s a pressing need for innovation in quantitatively assessing HS severity.
While clinical and laboratory measurements reflecting organ function are routinely monitored, experimental evidence suggests that these measurements often fall short in accurately reflecting illness severity or long-term prognosis5. Several novel biomarkers, such as high-mobility group box protein-1 (HMGB-1)10, neutrophil gelatinase-associated lipocalin11, and urinary heat shock protein 7212,13, are currently under investigation through animal and preclinical studies. However, these experimental biomarkers typically entail longer assessment times compared to conventional clinical laboratory values and are less accessible and feasible in daily clinical practice.
In recent years, L-FABP has emerged as a novel biomarker in Japan. L-FABP, a 14-kDa fatty acid-binding protein found in the cytoplasm of human renal proximal tubular cells, has shown promise as an effective biomarker for detecting progressive end-stage renal failure and ischemic damage resulting from dehydration in clinical critical care settings7,14,15,16. Given that severe HS primarily involves ischemia due to diminished visceral blood flow, our research team focused on L-FABP as a potential prognostic biomarker for dehydration in HS.
L-FABP has been approved for diagnostic testing of acute kidney injury in Japan17 and can be measured within minutes using either a commercial-based assay kit or a POCT kit, with high accuracy. The POCT L-FABP kit requires only a small urine sample and can be performed outside hospital settings, such as in field triage at athletic events or at home, without the need for blood samples. Due to its high accessibility and feasibility, L-FABP represents a promising biomarker for clinical use in HS.
Urinary L-FABP as a reflection of heatstroke severity
In our study, we found a significant correlation between the initial urinary concentration of L-FABP and the SOFA score on the first day of admission. The pathophysiology of HS is multifaceted, involving interactions among heat cytotoxicity, coagulation, and inflammation, all contributing to systemic injury18. Heat-related injury and severe dehydration instigate an inflammatory response mediated by heat shock proteins, inflammasomes, and various pro-inflammatory and anti-inflammatory cytokines. Additionally, heat injury induces cytotoxic effects via inflammation, leading to non-programmed necrosis and programmed cell death, including apoptosis, necroptosis, and pyroptosis18. These forms of cell death are associated with coagulation and inflammation activation, with damage-associated molecular patterns (DAMPs) such as HMGB-1 leaking from damaged cells18,19.
The SOFA score assesses organ function or failure based on scores for six different systems: respiratory, cardiovascular, hepatic, coagulation, renal, and neurological. The positive correlation between urinary L-FABP concentration and SOFA score can be attributed to both direct and indirect reasons. L-FABP serves as a promising biomarker for predicting dehydration and reflecting renal ischemic dysfunction2,7. Moreover, its localization in the cytoplasm of renal proximal tubular cells suggests its potential to indicate tubular necrosis resulting from dehydration due to HS2,7. The disturbance of microvascular coagulation triggered by serum HMGB-1 also contributes to renal ischemic changes, further linking the increase in urinary L-FABP to the severity of HS pathology characterized by heightened renal ischemia induced by increased coagulation triggered by serum HMGB-118.
Implementation of L-FABP measurements with POCT
The potential of urinary L-FABP in determining the pathology of severe HS is indeed promising, particularly in providing insights into ischemic visceral cell damage. The fact that it serves as a biomarker for acute renal failure and is covered by medical insurance in Japan adds to its significance. The accessibility of POCT kits for L-FABP in Japan further enhances its utility, especially considering its low invasiveness and the elimination of the need for blood samples.
Given that a notable proportion of severe non-exertional HS cases occur among elderly individuals who are often indoors and under the care of home nurses or caregivers, the easy daily measurement of L-FABP using a POCT kit could be transformative. Early detection through such means could potentially lead to a reduction in the number of HS cases, particularly among vulnerable populations.
This research revealing a correlation between urinary L-FABP concentration and patient outcomes is crucial. Establishing a threshold for worse longer outcomes at 28.6 ng/mL provides a tangible marker for prognosis. With the cut-off value for positive appearance in POCT kits set at 12.5 ng/mL, there’s a clear indication for intervention. Identifying positive POCT results in prehospital settings could facilitate timely decisions for patient transfer to tertiary emergency medical centers for high-level intensive care.
Limitations
This pilot study is subject to several limitations. Firstly, our focus was primarily on severe cases of HS. Mild HS diagnosis predominantly relies on subjective symptoms, potentially leading to misclassification and misdiagnosis within this study population. Consequently, the prognostic utility of L-FABP for patients with mild HS remains unexplored.
Secondly, the study involved a relatively small sample size, and some cases were not consistently tracked throughout the entire study period. We did not calculate the sample size due to the limited availability of reference studies on L-FABP measurements in heatstroke patients. This may introduce variability and limit the generalizability of our findings.
Thirdly, the majority of patients included in the study were elderly and experienced non-exertional HS. In Japan, a significant portion of emergent HS cases (60%) occurs in elderly individuals aged over 65 years and indoors, and 93.6% were diagnosed with non-exertional heat stroke, which means the onset time for most cases remains unclear. Consequently, the study population may represent a unique subset compared to populations in other countries, potentially limiting the applicability of our results to younger populations with exertional HS.
Fourthly, we did not measure daily urine volume but assessed serum chemical biomarkers, namely BUN (blood urea nitrogen) and creatinine. This limitation may lead to an underestimation of dehydration. These limitations underscore the need for further research with larger and more diverse study populations to validate the findings and expand our understanding of the utility of L-FABP as a prognostic biomarker for HS across different severity levels and demographic groups.
Conclusion
In conclusion, the POCT of L-FABP emerges as a valuable tool for predicting the pathophysiological severity of HS while also reflecting patient outcomes. This POCT holds promise for feasibility in field or prehospital settings, facilitating timely triage of HS patients to identify severe cases effectively. The correlation observed between urinary L-FABP concentration and HS pathology, as indicated by the SOFA score, underscores its potential as a promising prognostic biomarker for severe HS. These findings highlight the potential of urinary L-FABP as a valuable clinical tool for assessing and managing HS patients, particularly in emergency and critical care settings.
Methods
Patient population
This prospective, multicenter cohort study encompassed 10 tertiary emergency medical centers across Japan, including Nippon Medical School Hospital, Osaka University Hospital, Tokyo Metropolitan Tama Medical Center, Nara Medical University Hospital, Teikyo University Hospital, Asahikawa Medical University Hospital, Shinmatsudo Central General Hospital, Omori Hospital Toho University Medical Center, Yamaguchi University Hospital, and Aizu Chuo Hospital. The study included individuals aged 18 years and older, with severe HS, and with a measurable core body temperature (rectal, bladder, or esophageal temperature). Patients meeting the criteria for severe HS were enrolled over three consecutive summer seasons (2019–2021) in Japan, diagnosed according to the Japanese Association of Acute Medicine criteria for HS20,21. The exclusion criteria comprised patients strongly suspected of sepsis or infectious disease.
Treatment and patient management
Emergency room (ER) treatment adhered generally to the Japanese HS consensus22 and guidelines23, including rapid evacuation from hot and humid conditions, external cooling via cooling blankets and/or ice packs, ice-cold crystalloid rapid infusion, and/or gastric lavage with ice-cold water. Additionally, computer-controlled active cooling devices (such as intravascular temperature management devices1 and gel-pad cooling devices) were employed. General resuscitation, including secured airway management, artificial ventilation, and vasopressor use, was administered based on individual physician discretion.
Blood and urine samples and biomarker measurements
Blood and urine samples were collected immediately after admission and before resuscitation. Clinical laboratory data (i.e., hepatic enzymes, blood urea nitrogen, creatinine, blood count, coagulative parameters) were measured using the serum samples.
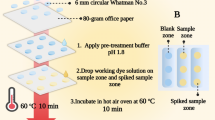
Urine samples were collected using a urinary catheter and L-FABP was measured semi- qualitative L-FABP with POCT (RENISCHEM® L-FABP POC Kit; CMIC Holdings Co., Ltd., Tokyo, Japan), we kept the rest of urine as the frozen sample for batch quantitative analysis. The rest of the urine samples were stored in a plastic tube, and stored at -80 °C in a deep freezer, for the subsequent batch analyses. The POCT kit was designed to determine whether the L-FABP level was high (≥ 100 ng/mL), medium (between ≥ 12.5 ng/mL and < 100 ng/mL), or low (< 12.5 ng/mL) compared to the reference range. We defined negative group (N-group: L-FABP < 12.5ng/mL) and positive group (P-group, L-FABP ≧ 12.5 ng/mL) for the clear judgment (i.e. all-or-none appearance of the test strip).
To confirm the agreement analysis for checking the feasibility of POCT in HS population, L-FABP levels in the urine samples were also measured using an enzyme-linked immunosorbent assay (ELISA) kit (L-FABP; CMIC Holdings Co., Ltd., Tokyo, Japan)by subsequent batch analyses.
The SOFA score24 and APACHE II score25 of each patient were also calculated.
Patient outcomes
Outcomes were evaluated utilizing the mRS26 score at discharge, 1 month post-onset, and 3 months post-onset by physicians blinded to patients’ biomarker status. A favorable outcome was defined as an mRS score between 0 and 227,28.
Statistical analysis
Variables were expressed as median and IQR for continuous non-parametric data and as numbers and percentages for categorical data. Inter-group comparisons for non-parametric data were conducted using the Mann-Whitney U-test. Correlations between non-parametric data sets were assessed via regression analysis. The prognostic potential of L-FABP was evaluated through ROC curve analysis, with the AUCs compared. Statistical analyses were performed using StatFlex software (version 7; Artech, Osaka, Japan), with significance set at P < 0.05.
Ethical considerations
The study protocol received approval from the Institutional Review Board of the Primary Research Center (Nippon Medical School Hospital; number 31-04-1120) and each participating research hospital. Written informed consent was obtained from all patients and patients’ relatives at their respective institutions. All methods were performed in accordance with the relevant guidelines and regulations.
Data availability
The data used to support the findings of this study are included within the article.
References
Yokobori, S. et al. Feasibility and safety of intravascular temperature management for severe heat stroke: a prospective Multicenter Pilot Study. Crit. Care Med. 46 (7), e670–e6. https://doi.org/10.1097/CCM.0000000000003153 (2018).
Sakamoto, T. et al. Wearing a face mask during controlled-intensity exercise is not a risk factor for exertional heatstroke: a pilot study. Acute Med. Surg. 8 (1), e712. https://doi.org/10.1002/ams2.712 (2021).
Obinata, H. et al. Indicators of Acute kidney Injury as biomarkers to Differentiate Heatstroke from Coronavirus Disease 2019: a Retrospective Multicenter Analysis. J. Nippon Med. Sch. 8 (1), 80–86. https://doi.org/10.1272/jnms.JNMS.2021_88-107 (2021).
Shapiro, Y. & Seidman, D. S. Field and clinical observations of exertional heat stroke patients. Med. Sci. Sports Exerc. 22 (1), 6–14 (1990).
Leon, L. R. & Bouchama, A. Heat stroke. Compr Physiol. 5(2): 611 – 47. https://doi.org/10.1002/cphy.c140017 (2015).
Epstein, Y., Yanovich, R. Heatstroke. N. Engl. J. Med. 380(25): 2449–2459. doi: https://doi.org/10.1056/NEJMra1810762 (2019).
Doi, K. et al. Evaluation of new acute kidney injury biomarkers in a mixed intensive care unit. Crit. Care Med. 39 (11), 2464–2469. https://doi.org/10.1097/CCM.0b013e318225761a (2011).
Alsaiqali, M. et al. The effects of heatwaves on Human Morbidity in Primary Care settings: a case-crossover study. Int. J. Environ. Res. Public. Health 19 (2). https://doi.org/10.3390/ijerph19020832 (2022).
Bouchama, A. & Knochel, J. P. Heat stroke. N Engl. J. Med. 346 (25), 1978–1988. https://doi.org/10.1056/NEJMra011089 (2002).
Tong, H. S. et al. Early elevated HMGB1 level predicting the outcome in exertional heatstroke. J Trauma. 71(4): 808 – 14. https://doi.org/10.1097/TA.0b013e318220b957 (2011).
Segev, G. et al. Characterization of kidney damage using several renal biomarkers in dogs with naturally occurring heatstroke. Vet. J. 206 (2), 231–235. https://doi.org/10.1016/j.tvjl.2015.07.004 (2015).
Bruchim, Y. et al. Urinary heat shock protein 72 as a biomarker of acute kidney injury in dogs. Vet. J. 225, 32–34. https://doi.org/10.1016/j.tvjl.2017.04.008 (2017).
Dehbi, M. et al. Hsp-72, a candidate prognostic indicator of heatstroke. Cell. Stress Chaperones 15 (5), 593–603. https://doi.org/10.1007/s12192-010-0172-3 (2010).
Thuijls, G. et al. Early diagnosis of intestinal ischemia using urinary and plasma fatty acid binding proteins. Ann. Surg. 253 (2), 303–308. https://doi.org/10.1097/SLA.0b013e318207a767 (2011).
Yamamoto, T. et al. Renal L-type fatty acid–binding protein in acute ischemic injury. J. Am. Soc. Nephrol. 18 (11), 2894–2902. https://doi.org/10.1681/ASN.2007010097 (2007).
Negishi, K. et al. Monitoring of urinary L-type fatty acid-binding protein predicts histological severity of acute kidney injury. Am. J. Pathol. 174 (4), 1154–1159. https://doi.org/10.2353/ajpath.2009.080644 (2009).
Goto, H. et al. Early biomarkers for kidney injury in heat-related illness patients: a prospective observational study at Japanese self-defense force Fuji Hospital. Nephrol. Dial Transpl. 38 (3), 644–654. https://doi.org/10.1093/ndt/gfac166 (2022).
Iba, T., Connors, J. M., Levi, M. & Levy, J. H. Heatstroke-induced coagulopathy: Biomarkers, mechanistic insights, and patient management. EClinicalMedicine 44: 101276. https://doi.org/10.1016/j.eclinm.2022.101276 (2022).
Hirose, T. et al. Presence of neutrophil extracellular traps and citrullinated histone H3 in the bloodstream of critically ill patients. PLoS One 9 (11), e111755. https://doi.org/10.1371/journal.pone.0111755 (2014).
Kondo, Y. et al. Comparison between the Bouchama and Japanese Association for Acute Medicine Heatstroke Criteria with Regard to the diagnosis and prediction of mortality of Heatstroke patients: a Multicenter Observational Study. Int. J. Environ. Res. Public. Health 16 (18). https://doi.org/10.3390/ijerph16183433 (2019).
Shimazaki, J. et al. Clinical characteristics, prognostic factors, and outcomes of heat-related illness (Heatstroke Study 2017–2018). Acute Med. Surg. 7 (1), e516. https://doi.org/10.1002/ams2.516 (2020).
Hifumi, T., Kondo, Y., Shimizu, K. & Miyake, Y. Heat stroke. J. Intensive Care. 6, 30. https://doi.org/10.1186/s40560-018-0298-4 (2018).
Working group on heatstroke medical care during the C-e. Heatstroke management during the COVID-19 epidemic: recommendations from the experts in Japan. Acute Med. Surg. 7 (1), e560. https://doi.org/10.1002/ams2.560 (2020).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22 (7), 707–710. https://doi.org/10.1007/BF01709751 (1996).
Knaus, W. A., Draper, E. A., Wagner, D. P. & Zimmerman, J. E. APACHE II: a severity of disease classification system. Crit. Care Med. 13 (10), 818–829 (1985).
van Swieten, J. C. et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19 (5), 604–607. https://doi.org/10.1161/01.str.19.5.604 (1988).
Grossestreuer, A. V. et al. Inter-rater reliability of post-arrest cerebral performance category (CPC) scores. Resuscitation 109, 21–24. https://doi.org/10.1016/j.resuscitation.2016.09.006 (2016).
Savio, K. et al. Reliability of the modified Rankin Scale applied by telephone. Neurol. Int. 5 (1), e2. https://doi.org/10.4081/ni.2013.e2 (2013).
Acknowledgements
Technical support and material support were provided by the CMIC Holdings Co., Ltd. and Shino-Test Corporation, Tokyo, Japan.
Author information
Authors and Affiliations
Contributions
SY, and JS contributed to the study design, study execution and manuscript preparation. JS contributed to the analysis of results and assistance with statistical processing. All authors (SY, JS, HK, HA, JK, ST, ES, RI, MF, SS, KS, and HY) have approved the final manuscript and attest to the integrity of the original data and analyses described in the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yokobori, S., Shimazaki, J., Kaneko, H. et al. The feasibility of point-of-care testing for initial urinary liver fatty acid-binding protein to estimate severity in severe heatstroke. Sci Rep 15, 5255 (2025). https://doi.org/10.1038/s41598-025-89767-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89767-7