Abstract
The sampling of S100B protein has been proposed as a screening tool to identify patients with a low risk of post-traumatic intracranial hemorrhage. Its performance for patients on antiplatelet agents or anticoagulants is still debatable. This exploratory study evaluates the diagnostic accuracy of S100B concentrations, measured within 3 h of head trauma, to rule out intracranial hemorrhage in adults on antiplatelet or anticoagulant therapy. This prospective study enrolled adult patients presenting for head trauma within the last 3 h and under antiplatelets or anticoagulants. We hypothesized that a S100B concentration under 0,100 µg.L-1 rule out intracranial hemorrhage with a negative predictive value over 0,99. Sensitivity, specificity, positive predictive value and negative predictive value were analyzed. From June 2020 to January 2023, 155 patients were included. 119 patients had a S100B level at 0,100 µg.L-1 or over. 8 had an intracranial hemorrhage. The sensitivity of S100B was 1 (95%CI 0,68–1), specificity was 0,25 (95%CI 0,18 − 0,32), positive predictive value was 0,07 (95%CI 0.03–0.13), negative predictive value was 1 (95%CI 0,90 − 1). This study suggests that when performed in a 3-hour period after mild head trauma, S100B measurement is an accurate screening tool to rule out intracranial hemorrhage in patients treated with antiplatelet agents or anticoagulants.
Similar content being viewed by others
Introduction
Traumatic Brain Injury (TBI) is the leading cause of mortality among young adults. Motor vehicle crashes are the leading cause of TBI in young adults, and falls are a leading TBI cause in children and adults over 45 years old1,2. TBI is a major cause of long-term disability, making it a critical public health concern and a socio-economic burden for modern health systems worldwide3. Intracranial hemorrhage represents one of the most serious complications arising from mild head trauma. Bleeding due to subdural hematoma, extradural hematoma or intraparenchymal hemorrhage results in high morbidity, high mortality and long-term disability4,5. The rate of post-traumatic intracranial hemorrhage following mild head trauma varies depending on patient symptoms and medical history. From 0,31% of patients without any medical history up to 6% of patients on antiplatelet agents and 7% in patients under anticoagulants6,7,8. For patients under aspirin alone, the relative risk of significant intracranial hemorrhage appears to depend on age8,9. At the same time, the proportion of patients receiving antiplatelet agents or anticoagulant medications is rising10,11. For those patients, the standard of care predominantly involves a head computed tomography (CT) scan. Until 2022, French guidelines recommended performing a cerebral CT scan for a patient with one of the following: a focal neurological deficit, retrograde amnesia of more than 30 min after trauma, Glasgow coma score less than 15 at 2 h post-trauma, loss of consciousness or amnesia of events associated with one of the following traumatic mechanisms: pedestrian knocked down by a motor vehicle, patient ejected from a vehicle, fall from a height of more than one meter, age over 65 years old, suspicion of skull fracture, any sign of skull base fracture, more than one episode of vomiting in adults, post-traumatic convulsion, a constitutional or iatrogenic bleeding disorders12. In 2022, an update of those guidelines regarding mild head trauma modified the assessment of bleeding risk related to antiplatelet agents. In patients under 65, using a single antiplatelet agent was no longer considered a risk factor13.
The decision to perform a CT scan is primarily based on risk assessment; however, this evaluation can be challenging. After a mild head trauma, many patients with intracranial hemorrhage present only nonspecific symptoms, such as vomiting or amnesia before impact. Most patients do not exhibit an abnormal Glasgow Coma Scale score after two hours, abnormal pupil size or reaction, or lateralizing motor weakness. Clinical decision rules, such as the Canadian CT Head Rule14) or the New Orleans Criteria15 have high sensitivity but lack specificity and some have not been validated for patients receiving antiplatelet or anticoagulant therapy. The consequences are higher healthcare costs, increased irradiation of patients, and reduced CT scan availability in the context of increasing imaging demands. As a result, the length of stay in the emergency department is increasing, overloading the staff and leading to overcrowding, which is linked to increased mortality16. To address this challenge, the assay of the S100B protein has been proposed as a screening tool to identify a low risk of post-traumatic intracranial hemorrhage. S100B levels range from 0.02 µg.L-1 to 0.150 µg.L-1 in healthy adult with variations depending on race17.
This assay has been validated in ruling out patients with significant intracranial hemorrhage in both adults and pediatric populations with a conventional threshold of 0,100 µg.L-118,19,20,21. S100B concentration has also been implemented in some European country guidelines13,22. It has great sensitivity reported to be near 100% but poor specificity. The optimal time frame for measuring the S100B level post-trauma is still debated. The 6-hour cut-off has been studied with good sensitivity. But some patients still fall under the 0,100 µg.L-1 threshold23,24. Due to the small half-life of the S100B, the 3-hour cut-off seems to have a better sensitivity25. Its use in patients presenting with traumatic brain injury and treated by antiplatelet agents or anticoagulants is still in debate.
This study aimed to investigate the diagnostic accuracy (sensitivity, specificity positive predictive value (PPV) and negative predictive value (NPV)) of S100B concentrations measured within 3 h of a mild head trauma in patients under antiplatelet agents or anticoagulants and suspected of having a intracranial. We hypothesized that S100B concentration < 0,100 µG.L-1 in blood samples from adult patients with mild TBI rule out traumatic intracranial hemorrhage with a negative predictive value over 0,99. CT-scan was used as the gold standard.
Methods
Ethics of approval statement
This study was conducted in accordance with the principles of the Declaration of Helsinki. The local ethics committee approved the study (GNEDS; Groupe Nantais d’Éthique dans le Domaine de la Santé). Since the analysis was performed on an already taken blood sample used for other purposes, the need for written consent was waived according to local laws. Non-opposition informed consent was obtained from all subjects and recorded in the medical file. The study’s sponsor is the Clinical Research and Innovation Department of Nantes University Hospital (Centre Hospitalier Universitaire de Nantes).
Study design and patients
This was a prospective single-centric exploratory study set in the emergency department of a French level 1 Trauma center. In his emergency department, every patient with a head trauma routinely has a blood sample taken for potential further analysis. All patients aged 18 years or older who had experienced mild head trauma within the past 3 h, were undergoing treatment that could impair hemostasis, such as antiplatelet agents or anticoagulant medications, and could undergo a blood sample within 3 h following the head trauma, were enrolled. Following 2022 guidelines, patients were stratified into three groups: low, intermediate, and high risk of traumatic brain injury. High risk was defined by one of the following risk factors: Hemostasis disorders (anticoagulants, dual antiplatelet therapy, or congenital bleeding disorders), Clinical signs suggestive of a cranial vault or cranial base fracture, Glasgow Coma Scale score less than 15 within 2 h of the trauma without intoxication, more than one episode of vomiting, post-traumatic seizures, focal neurological deficit. Intermediate risk was defined as follows: Age ≥ 65 years with single antiplatelet therapy, Glasgow Coma Scale score less than 15 within 2 h of the trauma with intoxication, trauma with high kinetic energy, amnesia for events occurring more than 30 min before the trauma. Low-risk patients had none of the above risk factors. For high-risk patients, a computerized tomography scan (CT scan) was mandated as soon as possible, with up to an 8-hour delay for intermediate-risk patients and no CT scan needed for low-risk patients.
Exclusion criteria were: inability to consent, need for immediate resuscitation, penetrating trauma, pregnancy, exhibiting neurological deficit signs, intoxication by any substance altering neurological capacities or having a known ongoing cerebral lesion, patients who withdrew consent, were unable to have an S100B blood sample within three hours following head trauma, did not undergo a CT scan during their emergency department stay, or had an antiplatelet or anticoagulant prescription but were not actually taking the medication were excluded from the statistical analysis. Patients meeting any of the specified exclusion criteria were removed from the analysis, including those with incomplete datasets.
CT scan was performed as soon as possible for high-risk patients and at least 6 h after the head trauma for intermediate and low-risk patients. Patients and physicians attending the patient were blinded to the S100B results.
Every data was collected in an electronic case report form. Patients were identified using an anonymous number. The following data were collected: age, gender, head trauma mechanism, vomiting, initial loss of consciousness, initial altered mental status, stigma of head trauma (skin lesions or skin penetration without penetrating skull injury), time between head trauma and S100B and CT scan results, need for surgery and hospital discharge for patient who did not need treatment or follow-up.
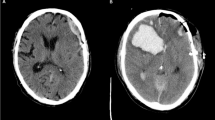
CT scan results were categorized as follows: extradural hematoma, subdural hematoma, parenchymal petechiae, subarachnoid hemorrhage, skull fracture, cranial vault, facial fracture, cervical fracture, cervical strain, pneumocephalus, extracranial hematoma, others. CT scan was classified as positive if at least one of those lesions was found: extradural hematoma, subdural hematoma, parenchymal petechiae or subarachnoid hemorrhage. Other lesions such as skull fracture, pneumocephalus, facial fracture, cervical fracture, cervical strain, and extracranial hematoma were treated accordingly.
Serum S100B measurement
A measurement of the S100B was then performed on the blood sample that had already been drawn. Serum S100B concentrations were determined by an electrochemiluminescence immunoassay using a Roche Diagnosticts Cobas 8000 e602 or Cobas Pro e801 instrument (Meylan, France) according to the manufacturer’s instructions. Based on other studies in adults, the cutoff was set at 0,100 µg.L–1. Patients exhibiting serum concentrations below this threshold were considered S100B negative, and those above this cutoff were considered S100B positive.
The S100B threshold has been described to vary depending on the age and the origin of the bleeding. Because older patients are more likely to fall and be treated with antiplatelet agents or anticoagulants, they are the most likely to benefit from an S100B sampling. However, in older patients, the rise of the S100B threshold could be due to increased blood-brain barrier permeability, an increase in extracerebral sources of S100B or a decline in S100B clearance26. A study that included patients over 65 years old established that these patients had higher serum S100B values than the overall adult populations, resulting in a low specificity of 19%18. Oris et al. suggested that a 0,150 µg.L-1 threshold was the most efficient in patients over 80 years old27. For patients included in this study and over 80 years old, we separately calculated the effectiveness of the 0,150 µg/L-1 threshold and assessed how these results impact the overall diagnosis performance of the S100B assay.
Sample size estimation
A formal sample size calculation was performed for a potential future trial, guided by parameters derived from previous research and aimed at achieving NPV of 0.99. The calculation assumed a sensitivity of 0.99, a specificity of 0.30, an NPV of 0.95, a PPV of 0.13, a disease prevalence of 10%, a statistical power of 80%, and an alpha risk of 0.05.
Statistical analysis
Parametric data were expressed as mean ± standard deviation. Non-parametric data were expressed as the median with interquartile range. Qualitative data were expressed as a percentage with a 95% confidence interval using the Wilson score. Number of subjects necessary to achieve statistical power was calculated using the method described by Mercaldo et al.28 through the bdpv package v1.3.
The Student’s t-test was used when the data were normally distributed, Mann-Whitney U test was used for non-normally distributed data. Qualitative data were compared using the Chi-squared test. When the Chi-squared was not applicable due to the sample size, the Fisher exact test was used. The statistical analysis was performed using RStudio© 2022.02.3 based on R 4.2.3 for Windows. A p-value under 0.05 was considered statistically significant.
Results
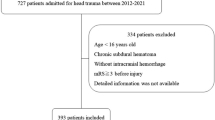
From June 2020 to January 2023, 201 patients were included in the study population. 46 (23%) of them had to be secondarily excluded: 2 withdrew their consent, 5 (2,4%) did not have a CT scan, 7 (3,5%) had no treatment effectively taken, 1 neither had a CT scan nor a treatment effectively taken, 4 patients (1,9%) did not have a S100B results, 27 patients (13%) had a blood sample taken after the 3-hour period.
Overall, 155 patients were included in the analyzed sample. Five patients (3%) were classified as low risk, 87 patients (56%) as intermediate risk, and 63 patients (41%) as high risk. The flow chart is detailed in Fig. 1.
Patients’ ages ranged from 39 to 98 years old. The mean age was 82 IQR [75–87], with 143 (92%) patients being 65 years old and over, and 91 (59%) patients being 80 years old and over. Most patients were male (84 patients, 54%). The cause of trauma was mostly a ground-level fall (127 patients, 82%). Most of them presented with a head trauma stigma (119 patients, 77%). The most used medication was aspirin (81 patients, 52%). Anticoagulants were present in 57 patients (37%). The most used anticoagulant was apixaban (26%). 5 (3%) patients were included with a low risk of traumatic brain injury before the modification of the guidelines. Characteristics of the population are described in Table 1.
A CT scan revealed anomalies in 66 patients (43%). Out of these, 8 patients (5%) had an intracranial hemorrhage, 3 of them had multiple injuries: 1 (0,6%) extradural hemorrhage, 3 (1,9%) subdural hemorrhages, 6 (3,8%) subarachnoid hemorrhages, 2 (1.3%) of which also presented intracerebral petechiae. Characteristics of those patients are presented in Table 2. One patient (0,6%) had a skull fracture without intracranial hemorrhage, 2 patients (1,3%) had a cervical spine fracture, and 2 patients (1,3%) had a facial bone fracture. Numerous patients (53; 34%), exhibited an extracranial hematoma without any additional injury. No case of pneumocephalus was observed among any patients. No patient needed surgical management.
119 patients (77%) had a S100B level at 0,100 µg.L-1 or over. 98 patients (63%) could be discharged, and 57 (37%) needed hospitalizations. Of these, 7 patients (4,5%) required hospital admission for monitoring and treatment of the head trauma, with none needing surgery. 50 patients (32%) were hospitalized for a condition unrelated to their head trauma.
Mean S100B level was 0,322 ± 0,390 µg.L-1 with a median of 0,163 [0,1002–0,379]. Mean S100B level of the intracranial hemorrhage group was 0,472 ± 0,265 µg.L-1 vs. 0,314 ± 0,395 µg.L-1 in the no TBI group. Median S100B level of the intracranial hemorrhage group was 0,462 µg.L-1 [0,233–0,699] vs. 0,160 µg.L-1 [0,100–0,357]. This difference was not statistically significant (p-value = 0,14). The results are shown in Fig. 2.
The sensitivity of S100B was 1 (95%CI 0.68–1), the specificity was 0,25 (95%CI 0,18 − 0,32), the positive predictive value was 0,07 (95%CI 0,03 − 0,13), and the negative predictive value was 1 (95%CI 0,90 − 1).
In ROC analysis for prediction for intracranial injury reveal by CT scan, the AUC value was 0.75 (95% CI, 0.59–0.89; p = 0.02) (Fig. 3).
The mean time between head trauma onset to the blood draw was 132 ± 42 min, while the mean time between head trauma onset and CT scan was 383 ± 149 min.
For patients over 80 years old, in our population, the sensitivity of S100B was 1 (95%CI 0,59 − 1), specificity was 0,41 (95%CI 0.31-0,53), NPV was 1 (95%CI 0,9–1), PPV was 0,12 (95%CI 0,10 − 0,14) and the overall results were sensitivity: 1 (95%CI 0,63 − 1), specificity: 0,39 (95%CI 0,31 − 0,47), NPV: 1 (95%CI 0,94 − 1) and PPV: 0,08 (95%CI 0,07 − 0,09).
A sample size calculation, targeting a negative predictive value (NPV) of 0.99 and based on parameters derived from previous studies, estimated that 6 271 participants would be required for a future trial, assuming no secondary exclusions or loss to follow-up.
Discussion
Among our patients receiving various treatments, 5.2% experienced intracranial hemorrhage, a rate lower than that commonly reported in cases of mild head trauma23. This finding may be explained by several factors. Most of the patients were over 80 years old and sustained mild head trauma following ground-level fall. It is possible that variations in patient age and the types of trauma studied in other research account for the differences between our findings and previously reported data. Additionally, the exclusion of patients with alcohol intoxication or substance abuse may have introduced a selection bias, as intoxication is frequently associated with mild head injuries29. Another potential source of bias stems from the organization of prehospital care in France. Patients with suspected life-threatening injuries, including intracranial hemorrhage, are often identified by prehospital teams and transported directly to intensive care units, operating rooms, or CT imaging facilities via mobile intensive care units. This practice could have influenced the composition of our study population and may partially explain the observed discrepancy.
S100B did not perform as well as expected. The specificity was reported to be 0,30 but only reached 0.25 in our specific population. This variation can be attributed to the diversity within our population, including differences in treatment, mechanisms of injury and age. A stratified strategy to implement specific S100 thresholds in each group could improve the sensitivity and specificity of S100B.
In this study, S100B demonstrated strong performance as a rule-out biomarker, achieving a NPV of 1. The 0,150 µg.L-1 threshold for patients over 80 years old could improve its statistical characteristics and avoid more unnecessary CT scans. Presently, using S100B remains constrained by the pretest risk, as it is not recommended for patients exhibiting additional risk factors, such as those receiving anticoagulants or other than aspirin antiplatelet agents. Our results suggest, with limited power, that a wider strategy could be implemented with other risk factors of TBI, potentially enabling the safe discharge of patients with suspected traumatic injury. The poor specificity of this assay still necessitates 70% of unnecessary CT scans, which may limit its applicability in routine clinical practice. A better rule-out strategy is still needed.
Alternative biomarkers are currently being investigated to extend the time between trauma and subsequent blood tests. However, as of the present, the results obtained from these studies have been inconclusive24,25.
In the context of utilizing S100B as a biomarker in TBI, a critical constraint is the necessity of a 3-hour window between the onset of head trauma and blood sample collection. This prerequisite establishes specific restrictions, notably when the trauma occurs at a significant distance from the hospital, when the patient experiences a period of unconsciousness of indeterminate duration following the traumatic event, is unreliable in his recording of the events, or when the patient does not have access to a medical evaluation within this 3-hour time frame.
Intracranial hemorrhage is but one category within the diverse array of traumatic brain injuries. The pathophysiological mechanisms associated with elevated levels of S100B protein are such that its utility as a predictive tool for other forms of injury, such as diffuse axonal injuries, is limited30. Finally, the biomarkers’ quantification, especially in polytrauma, increases the probability of false positive readings due to the presence of S100B in various other tissues31.
Limitations
This study was discontinued early for the following reasons.
First, the reduction of head trauma during the COVID-19 pandemic has reduced our capacities for inclusion32. In November 2022, French guidelines for suspected mild traumatic brain injury were updated13. First, for patients under 65 years old on aspirin but without additional symptoms, a CT scan was no longer recommended. Second, S100B was approved by these guidelines as a rule-out biomarker for intracranial hemorrhage in patients with blunt head trauma who were on aspirin and had an intermediate risk of intracranial hemorrhage. As a result, for these patients, a CT scan was not recommended if their S100B serum level was below 0.100 µg/L. Consequently, they could not be included in our study since no CT scan was performed. These guideline changes drastically reduced our potential for inclusion, as this population represented a significant portion of our original study sample.
Increasing crowding in our emergency department made recruiting patients within the 3-hour timeframe challenging. As a result, the unknown characteristics of those presenting within the 3-hour window but not included could introduce a selection bias.
As well, as a single-center study in a level 1 trauma center, this study could be affected by further selection bias as patients at risk of intracranial hemorrhage were more likely to present to this emergency department.
In this study, we decided not to include patients who experienced blunt head trauma and did not take any hemostasis-impairing drugs, as intracranial hemorrhage is rarer in this population6. Therefore, patients who undergo a CT scan in this group usually have a higher pretest probability of intracranial hemorrhage. Including this population would have introduced a selection bias. Nevertheless, to assess the performance of S100B in this setting and to determine whether S100B levels are linked to the drugs taken, including patients who do not take antiplatelet or anticoagulant drugs would be beneficial.
Fifty patients were hospitalized for a condition unrelated to their head trauma. Various conditions have been linked to elevated S100B levels, including Alzheimer’s disease33, sepsis-associated encephalopathy34, melanoma35, schizophrenia36, stroke37, and extracerebral trauma31. In this study, we did not monitor diagnoses unrelated to head trauma. Therefore, it is possible that some patients had S100B levels affected by these coexisting conditions, which would be more likely among hospitalized patients.
During the study period, standard coagulation tests were not consistently performed for patients not receiving anticoagulant therapy. As a result, we may have overlooked some antiplatelet-treated patients with an unknown hypocoagulable status.
Serum S100B measurements were conducted using two different machines. Although both were calibrated according to the manufacturer’s instructions, variations between the devices could introduce measurement bias.
Finally, the sample size of this study, while informative, is insufficient compared to the large sample size required to achieve statistical significance. As a result, it cannot validate the use of S100B as a rule-out marker for intracranial hemorrhage.
Conclusion
Although limited in power, this study suggests that when S100B sampling is done in a 3-hour period, and the result is under 0,100 µg.L-1 after mild head trauma in patients treated with antiplatelet agents or anticoagulants, we could safely rule out intracranial hemorrhage without CT scan. However, the poor specificity and PPV demonstrate that S100B sampling cannot be relied upon to diagnose intracranial hemorrhage. This underscore the need for improved biological markers or assessment strategies to reduce the number of CT scans performed on patients without intracranial hemorrhage.
Data availability
The datasets used and analyzed during the current study is provided within the supplementary information files.
References
Capizzi, A., Woo, J. & Verduzco-Gutierrez, M. Traumatic Brain Injury: an overview of Epidemiology, Pathophysiology, and Medical Management. Med. Clin. North. Am. 104, 213–238 (2020).
Van den Brand, C. L. et al. Traumatic brain injury in the Netherlands, trends in emergency department visits, hospitalization, and mortality between 1998 and 2012. Eur. J. Emerg. Med. 25, 355–361 (2018).
Nelson, L. D. et al. Functional recovery, symptoms, and Quality of Life 1 to 5 years after traumatic brain Injury. JAMA Netw. Open. 6, e233660. https://doi.org/10.1001/jamanetworkopen.2023.3660 (2023).
Ma, Z. et al. In-hospital mortality and risk factors among elderly patients with traumatic brain injury: protocol for a systematic review and meta-analysis. BMJ Open. 13, e065371. https://doi.org/10.1136/bmjopen-2022-065371 (2023).
van Essen, T. A. et al. Mortality reduction of Acute surgery in traumatic Acute Subdural Hematoma since the 19th century: systematic review and Meta-analysis with dramatic effect: is surgery the obvious parachute? J. Neurotrauma. 40, 22–32 (2023).
Easter, J. S. et al. Will Neuroimaging reveal a severe Intracranial Injury in this adult with minor Head Trauma? The rational clinical examination systematic review. JAMA 314, 2672–2681 (2015).
Alter, S. M. et al. Antiplatelet therapy is associated with a high rate of intracranial hemorrhage in patients with head injuries. Trauma. Surg. Acute Care Open. 5, e000520. https://doi.org/10.1136/tsaco-2020-000520 (2020).
Probst, M. A. et al. Prevalence of Intracranial Injury in adult patients with Blunt Head Trauma with and without anticoagulant or antiplatelet use. Ann. Emerg. Med. 75, 354–364 (2020).
Fiorelli, E. M. et al. Incremental risk of intracranial hemorrhage after mild traumatic brain Injury in patients on Antiplatelet Therapy: systematic review and Meta-analysis. J. Emerg. Med. 59, 843–855 (2020).
Tokioka, F. et al. Frequency and clinical features of radiographic head injury caused by inpatient falls: a single-centre retrospective cohort study. BMJ Open. 13, e066426. https://doi.org/10.1136/bmjopen-2022-066426 (2023).
Laic, R. A. G. Long-term outcomes after traumatic brain injury in elderly patients on antithrombotic therapy. Acta Neurochir. (Wien). 165, 1297–1307 (2023).
Jehlé, E. et al. Traumatisme crânien léger (score de Glasgow De 13 à 15): triage, évaluation, examens complémentaires et prise en charge précoce chez le nouveau-né, L’enfant et l’adulte. Ann. Fr. Med. Urgence. 2, 199–214 (2012).
Gil-Jardiné, C. et al. Management of patients suffering from mild traumatic brain injury 2023. Anaesth. Crit. Care Pain Med. 42, 101260 (2023).
Stiell, I. G. et al. The Canadian CT Head Rule for patients with minor head injury. Lancet 357, 1391–1396 (2001).
Stiell, I. G. et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA 294, 1511–1518 (2005).
Valli, G. et al. In-hospital mortality in the emergency department: clinical and etiological differences between early and late deaths among patients awaiting admission. Clin. Exp. Emerg. Med. 8, 325–332 (2021).
Ben Abdesselam, O., Vally, J., Adem, C., Foglietti, M-J. & Beaudeux, J-L. Reference values for serum S-100B protein depend on the race of individuals. Clin. Chem. 49, 836–837 (2003).
Allouchery, G. et al. Clinical validation of S100B in the management of a mild traumatic brain injury: issues from an interventional cohort of 1449 adult patients. Clin. Chem. Lab. Med. 56, 1897–1904 (2018).
Amoo, M. et al. S100B, GFAP, UCH-L1 and NSE as predictors of abnormalities on CT imaging following mild traumatic brain injury: a systematic review and meta-analysis of diagnostic test accuracy. Neurosurg. Rev. 45, 1171–1193 (2022).
Rogan, A. et al. Can serum biomarkers be used to rule out significant intracranial pathology in emergency department patients with mild traumatic brain injury? A systemic Review & Meta-Analysis. Injury 53, 259–271 (2023).
Oris, C. et al. The Biomarker S100B and mild traumatic brain Injury: a Meta-analysis. Pediatrics 141, e20180037 (2018).
Undén, J. et al. Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults: an evidence and consensus-based update. BMC Med. 11, 50 (2013).
David, A. et al. Evaluation of S100B blood level as a biomarker to avoid computed tomography in patients with mild head trauma under antithrombotic medication. Diagn. Interventional Imaging. 98, 551–556 (2017).
Rogan, A. et al. Diagnostic performance of S100B as a rule-out test for intracranial pathology in head-injured patients presenting to the emergency department who meet NICE Head Injury Guideline criteria for CT-head scan. Emerg. Med. J. 40, 159–166 (2023).
Laribi, S. et al. S100B blood level measurement to exclude cerebral lesions after minor head injury: the multicenter STIC-S100 French study. Clin. Chem. Lab. Med. 52 (4), 527–536 (2014).
Oris, C. et al. S100B, actor and biomarker of mild traumatic brain Injury. Int. J. Mol. Sci. 24, 6602 (2023).
Oris, C. et al. Predictive performance of blood S100B in the management of patients over 65 years old with mild traumatic brain Injury. J. Gerontol. Biol. Sci. Med. Sci. 76, 1471–1479 (2021).
Mercaldo, N. D., Lau, K. F. & Zhou, X. H. Confidence intervals for predictive values with an emphasis to case-control studies. Stat. Med. 26, 2170–2183 (2007).
Weil, Z. M., Corrigan, J. D. & Karelina, K. Alcohol Use Disorder and Traumatic Brain Injury. Alcohol Res. 39, 171–180 (2018).
Janigro, D. et al. GFAP and S100B: what you always wanted to Know and Never dared to ask. Front. Neurol. 13, 835597 (2022).
Ohrt-Nissen, S. et al. How does extracerebral trauma affect the clinical value of S100B measurements? Emerg. Med. J. 28, 941–944 (2011).
De Carvalho, H. et al. Stroke with delayed visit to the Emergency Department: the Next Public Crisis? J. Emerg. Med. 60, e147–e148. https://doi.org/10.1016/j.jemermed.2020.12.027 (2021).
Holper, S., Loveland, P., Churilov, L., Italiano, D. & Watson, R. Yassi, N. Blood astrocyte biomarkers in Alzheimer Disease: a systematic review and Meta-analysis. Neurology 103, e209537 (2024).
Torres, V. B. L. et al. Sepsis-Associated outcomes in critically ill patients with malignancies. Ann. Am. Thorac. Soc. 12, 1185–1192 (2015).
Mocellin, S., Zavagno, G. & Nitti, D. The prognostic value of serum S100B in patients with cutaneous melanoma: a meta-analysis. Int. J. Cancer. 123, 2370–2376 (2008).
Aleksovska, K. et al. Systematic review and Meta-analysis of circulating S100B blood levels in Schizophrenia. PLoS One. 9, e106342 (2014).
Ye, H. et al. Serum S100B levels may be associated with cerebral infarction: a meta-analysis. J. Neurol. Sci. 348, 81–88 (2015).
Author information
Authors and Affiliations
Contributions
Hugo De Carvalho (HDC) and Paul André Poislane (PAP) conceived the study. HDC and Quentin Lebastard (QLB) developed the analysis plan. HDC, PAP collected the clinical data and Damien MASSON (DM) collected the S100B results. HDC, QLB and Mathilde Papin (MP) undertook the main analysis. HDC, PAP, QLB and MP wrote the first draft of the paper. Arthur David (AD) Nicolas Goffinet (NG) and DM reviewed and corrected the manuscript making important critical revisions. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Poislane, PA., Papin, M., Masson, D. et al. Diagnostic performance of S100B assay for intracranial hemorrhage detection in patients with mild traumatic brain injury under antiplatelet or anticoagulant therapy. Sci Rep 15, 5741 (2025). https://doi.org/10.1038/s41598-025-89927-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89927-9