Abstract
To investigate the current situation of hearing loss and the associations of occupational noise exposure with hearing loss in petrochemical enterprise workers. This was a cross-sectional study that employed cluster sampling methods, and 951 workers aged 20–59 years from a petrochemical enterprise were included between June and December 2022. The subjects underwent health status surveys and occupational health examinations. To assess the associations between noise level and hearing loss, a logistic regression model was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs). A total of 951 participants (837 male and 114 female) were included in this study. And 68.3% of workers had a noise exposure level greater than ≥ 80 dB (A). The prevalence of speech frequency hearing loss, high-frequency hearing loss, and bilateral hearing loss among participants was 2.3% (22/951), 10.2% (97/951), and 10.3% (98/951), respectively. The prevalences of high-frequency hearing loss and binaural hearing loss were compared among subjects grouped by gender, age, family history of hyperlipidaemia, smoking status, systolic blood pressure, diastolic blood pressure, duration of noise exposure, and level of occupational noise exposure, and all differences were statistically significant (all P < 0.01). Compared with that of participants with noise levels < 80 dB(A), the risk of speech frequency hearing loss was significantly greater in the ≥ 90 dB(A) noise exposure group (OR: 5.33). The noise exposure level 80–89 dB(A) group (OR: 2.75) and the noise exposure level ≥ 90 dB(A) group (OR: 2.16) were both associated with a higher prevalence of high-frequency hearing loss. The noise hazards in petrochemical enterprises are severe. Long-term exposure to occupational noise environments significantly increases the risk of hearing loss among workers. Therefore, it is essential to strengthen noise control and enhance hearing protection efforts to effectively prevent excessive occupational noise exposure, thereby reducing the risk of hearing loss in workers.
Similar content being viewed by others
Introduction
Occupational noise is one of the most common occupational hazards in the workplace worldwide1, with more than 32.6 million workers exposed to hazardous noise levels in 2020 in China2. Hearing loss is the primary adverse health effect caused by occupational noise exposure3. Noise-induced hearing loss is also regarded as a serious problem and one of the most common occupational disorders worldwide, accounting for 7 to 21% of hearing loss cases4. The World Health Organization (WHO) estimated that 16% of hearing loss in adults was attributable to occupational noise exposure in 20215. In the U.S., nearly 25% of adults aged 20–69 years experienced noise-induced hearing loss in 20176. A recent study revealed that occupational noise exposure above 85 decibels [dB(A)] caused 7–21% hearing loss, with the lowest incidence in industrialized countries and the highest in developing countries3. Moreover, occupational noise-induced deafness has become the third most common occupational disease, accounting for 16.7% of the total occupational diseases in China7. Thus, hearing loss is a significant occupational health concern in workers exposed to noise8.
The prevalence of occupational hearing loss in developing countries (23%) is greater than that in developed countries (16%)3. Especially in China, monitoring results of the induction of occupational diseases revealed that the noise intensity in ten manufacturing categories, including the petrochemical industry, is relatively high. Numerous surveys indicated that noise hazards in petrochemical enterprises are more severe and that the prevalence of hearing loss among populations exposed to noise is relatively high. Hearing loss in the workplace is a significant health problem with economic consequences and accounts for 60% of all reported work-related diseases9. A cohort study conducted by foreign scholars over a period of 10 years revealed that the prevalence of hearing loss among workers in the petroleum industry is 14%10, whereas the prevalence of hearing loss among production workers in a certain petrochemical enterprise in China is as high as 37.8%11. The petrochemical industry plays an irreplaceable role in the national economy, with many people exposed to noise. However, information on the prevalence of hearing loss among employees caused by occupational noise in petrochemical enterprises is limited. This is a neglected public health issue that requires urgent implementation of policies and regulations.
Therefore, in this study, an epidemiological investigation of noise workers in a Chinese petrochemical enterprise was conducted to further understand the hazard status of occupational noise in petrochemical enterprises and the epidemiological characteristics of the effects of noise exposure on hearing damage.
Materials and methods
Study design and participants
In June 2022, a cross-sectional survey was conducted, and 951 occupationally noise-exposed workers employed in the petrochemical enterprise were enrolled in Danzhou city, Hainan Province, China. The subjects had occupational noise exposure for more than one year, and the intensity of noise exposure was ≥ 80 dB(A) (LEX, 8 h). Those who declined to participate, provided incomplete information, or experienced difficulties in communication were excluded from the current research. A health status questionnaire designed by the research team was used to collect basic information about the study participants, and the Chinese version of the effort-reward imbalance (ERI) scale was used to assess the level of occupational stress. Data were collected face-to-face via a structured questionnaire administered by trained professional physicians. The information in the questionnaire included demographic characteristics [gender, age, family history, body mass index (BMI), etc.], health habits (physical activity, smoking, alcohol consumption, etc.) and exposure to occupational hazards (heat, dust, occupational stress, noise, etc.). The working model: regular day shift refers to workers working in different shifts for 24 h without stopping; shift work refers to workers working on a fixed day shift. Physical activity: Physical activity was defined as exercise frequency of > 3 times per week for > 30 min. Smoking: Smoking was defined as having 6 months or more of continuous or cumulative smoking with at least 1 cigarette per day. Alcohol use: those who consumed alcohol at least once a week in the past year were defined as alcohol use. Occupational stress: An ERI > 1 indicates occupational stress, and an ERI ≤ 1 indicates no occupational stress. This study was approved by the Ethics Committee of Hainan Medical University (HYLL-2022–247). All participants provided written informed consent.
Classification of exposure to occupational hazards
Information on occupational exposure, including the name of the occupational hazard and duration of exposure, was obtained from the participants’ companies according to the occupational health monitoring reports provided by certified occupational health inspection organizations. The data from the occupational health monitoring reports were measured in June 2022. In this study, occupational hazard exposure included occupational noise exposure, dust exposure, and high-temperature exposure. Noise levels were measured according to GBZ/T 189.8–2007 "Measurement of Physical Factors in the Workplace Part 8: Noise" . The testing indicators were evaluated according to the limit values stipulated in GBZ 2.2–2007 Limits of Occupational Exposure to Harmful Factors in the Workplace Part 2: Physical Factors. Occupational noise exposure was defined as working in the presence of sound harmful to health, with an equivalent sound level of at least 80 dB(A) during an 8-h workday or 40-h workweek. Occupational dust exposure was defined as working in the presence of industrial dust, including inorganic dust, organic dust, and mixed dust. Occupational high-temperature exposure was defined as working at sites where the wet bulb-globe temperature (WGBT) index was ≥ 25 °C.
Blood pressure measurement and hypertension definition
Blood pressure (BP) was measured via electronic sphygmomanometers, and the participants were in a seated position after a 5-min rest before examination. All measurements and medical examinations were performed by trained medical personnel. Each participant’s BP was measured three times, and the average BP was calculated. Individuals were defined as having hypertension if they met one of the following standards: self-reported current use of antihypertensive medication; mean value of SBP above 140 mmHg; and/or DBP above 90 mmHg measured during a medical examination. Each individual was diagnosed with hypertension after three resting BPs were measured in this study.
Ascertainment of hearing loss
Speech frequencies are generally defined as a range of frequencies that are closely related to everyday language comprehension, focusing mainly on 0.5 kHz, 1.0 kHz and 2.0 kHz. These frequencies are used to assess speech frequency hearing loss and reflect the extent to which everyday communication skills are affected. The high frequency range is often closely associated with noise exposure and age-related hearing loss (senile deafness). In this study, the analysis of high-frequency hearing loss focused on 3.0 kHz, 4.0 kHz, and 6.0 kHz because these frequencies are more sensitive to noise exposure.
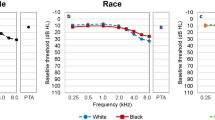
According to the diagnostic criteria (GB 49–2014). Professional medical technicians conduct pure-tone audiometry on the subjects in soundproof rooms in the hearing testing centers of medical institutions. The hearing test equipment passed the calibration of the National Institute of Measurement and Testing Technology, and the error between the equipment was controlled within 3%. The workers were free from the occupational noise exposure workplace and rested for at least 24 h. Air conduction thresholds were determined for each ear at 0.5, 1, 2, 3, 4, and 6 kHz over an intensity range of -10 to 120 dB(A). After the measurement results were adjusted for age and gender, judgements of speech frequency hearing loss and high-frequency hearing loss were made: any ear with an adjusted average hearing threshold at speech frequencies of 0.5, 1.0, and 2.0 kHz ≥ 25.0 dB(A) was considered to have speech frequency hearing loss, and any ear with an adjusted average hearing threshold at high frequencies of 3.0, 4.0, and 6.0 kHz ≥ 25.0 dB(A) was considered to have high-frequency hearing loss. Hearing thresholds ≥ 25.0 dB(A) at 0.5, 1.0, 2.0, 3.0, 4.0, and 6.0 kHz in either ear were defined as hearing loss at that frequency. Binaural hearing loss was defined as a pure-tone average ≥ 25.0 dB(A) in either ear in accordance with the definition of the WHO, including unilateral and bilateral hearing loss, and was based on the arithmetic mean of hearing thresholds (in decibels) at speech frequency (0.5, 1, and 2 kHz) or high frequency (3, 4, and 6 kHz)12.
Statistical analysis
Continuous variables are expressed as the mean ± standard deviation (SD) for normally distributed data. Categorical variables are expressed as frequencies (%). Continuous data were evaluated via univariate analysis of variance and Student’s t tests, and qualitative data were analysed via Pearson χ2 contingency tables. The prevalence of hearing loss at each frequency, speech frequency, and high frequency were estimated for the participants. Three logistic regression models were constructed to assess the associations between occupational noise exposure levels and speech frequency hearing loss, high-frequency hearing loss, and bilateral hearing loss. Model 1 was unadjusted. Model 2 was adjusted for age and gender. All variables with a p value ≤ 0.05 in the univariate analysis of Table 1 were adjusted in Model 3. All of the statistical analyses were performed using SPSS 26.0 software. The statistical tests were two-sided, and significance was set at P < 0.05.
Results
Characteristics of participants
A total of 951 workers (837 male and 114 female) were included in this study. The mean age of the participants was 30.6 ± 8.1 years. A total of 31.7% of the participants were exposed to noise for less than 80 dB(A), 38.4% were in the range of 80–89 dB(A), and 29.9% had a noise exposure level of greater than ≥ 90 dB(A). The prevalence of hypertension in the subjects was 6.3% (60/951). The prevalence of hearing loss at frequencies of 0.5, 1.0, 2.0, 3.0, 4.0, and 6.0 kHz was 2.0% (19/951), 0.9% (9/951), 2.7% (26/951), 6.1% (58/951), 10.9% (104/951), and 12.9% (123/951), respectively. The prevalence of speech frequency hearing loss, high-frequency hearing loss, and bilateral hearing loss among the participants was 2.3% (22/951), 10.2% (97/951), and 10.3% (98/951), respectively. We observed significant differences in the prevalence of hearing loss according to demographic characteristics. The prevalence of speech frequency hearing loss was significantly greater among individuals characterized by advanced age, shift work, a family history of hyperlipidaemia, BMI, longer occupational noise exposure duration and higher occupational noise exposure levels (all P < 0.05). The prevalences of high-frequency hearing loss and binaural hearing loss were compared among subjects grouped by gender, age, family history of hyperlipidaemia, smoking status, systolic blood pressure, diastolic blood pressure, duration of noise exposure, and level of occupational noise exposure, and all differences were statistically significant (all P < 0.01).
Associations between occupational noise exposure levels and hearing loss at a frequency of 3,4 and 6 kHz
Table 2 shows the OR values and 95% confidence intervals (95% CIs) for the associations between occupational noise exposure levels and hearing loss at a frequency of 3 kHz. Compared with participants with noise exposure levels < 80 dB(A), after adjusting for potential confounding factors, the risk of hearing loss was significantly greater in the 80–89 dB(A) noise exposure group (OR: 3.09, 95% CI: 1.33–7.18). However, the association with the ≥ 90 dB(A) group was not significant. Compared with individuals with noise exposure levels < 80 dB(A), after adjusting for potential confounding factors, both the 80–89 dB(A) noise exposure group (OR: 2.03, 95% CI: 1.11–3.73) and the ≥ 90 dB(A) noise exposure group (OR: 1.95, 95% CI: 1.04–3.62) had significantly higher prevalence rates of hearing loss (Table 3). At a frequency of 6 kHz, compared with individuals with noise exposure levels < 80 dB(A), the risk of hearing loss was significantly greater in the 80–89 dB(A) noise exposure group (OR: 1.88, 95% CI: 1.10–3.22). However, the association with the ≥ 90 dB(A) group was not significant (Table 4).
Association between occupational noise exposure levels and speech frequency hearing loss, high-frequency hearing loss, and bilateral hearing loss
The ORs and 95% CIs for the associations of occupational noise exposure level with speech frequency hearing loss are shown in Table 5. Compared with that of participants with noise exposure levels < 80 dB(A), the risk of hearing loss was significantly greater in those with noise exposure levels ≥ 90 dB(A) (OR: 5.33, 95% CI: 1.14–24.93) after adjusting for potential confounders. However, the association was not significant for the noise exposure level of 80–89 dB (A). The ORs and 95% CIs for the associations of occupational noise exposure level with high-frequency hearing loss are shown in Table 6. After adjusting for potential confounders, individuals exposed to occupational noise levels of 80–89 dB(A) and ≥ 90 dB(A) presented a significantly greater prevalence of hearing loss than did those exposed to noise levels below 80 dB(A), with odds ratios of 2.75 (95% CI: 1.46–5.17) and 2.16 (95% CI: 1.12–4.17), respectively. The ORs and 95% CIs for the associations between occupational noise exposure and bilateral hearing loss are presented in Table 7. Compared with individuals with noise exposure levels below 80 dB(A), those in the 80–89 dB(A) exposure group (OR: 2.75, 95% CI: 1.46–5.17) and the ≥ 90 dB(A) exposure group (OR: 2.24, 95% CI: 1.16–4.32) presented a greater prevalence of hearing loss.
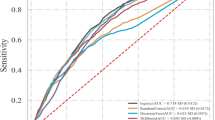
Furthermore, we also assessed the risk of hearing loss in different occupational noise exposure groups (Fig. 1). High levels of occupational noise exposure were associated with increased hearing loss. In particular, hearing loss was more pronounced in the 4 kHz frequency, high-frequency, and bilateral groups, with both the 80–89 dB (A) noise-exposed group and the ≥ 90 dB (A) group having a significantly increased risk of hearing loss, with ORs > 1, compared to participants with noise exposure levels < 80 dB (A). At 3 kHz and 6 kHz frequencies, compared to individuals with noise exposure levels of < 80 dB (A), the risk of hearing loss was significantly increased in the 80–89 dB (A) noise exposure group. However, the correlation with the ≥ 90 dB (A) group was not significant. In addition, the relationship between occupational noise exposure levels and speech frequency hearing loss showed that the correlation between noise exposure levels in the 80–89 dB (A) group was not significant compared to participants with noise exposure levels < 80 dB (A).
Discussion
Hearing loss was ranked as the fourth leading disease in both 2013 and 201513, higher than many other chronic diseases, such as diabetes and chronic obstructive pulmonary disease. However, limited research and public awareness have been conducted on hearing loss. It is estimated that one-third of all cases of hearing loss are attributed to noise exposure, and occupational exposure to noise makes up a great proportion of these cases, which makes hearing loss the most prevalent occupational disease in the USA8. The World Health Assembly noted that hearing loss can be prevented in half of all cases, especially hearing loss in the workplace, which is irreversible but can be entirely prevented. Thus, early detection and intervention are critical for the prevention of this condition14.
The present study estimated the hearing loss conditions of workers in petrochemical enterprises in Hainan, China, in the range of 0.5 to 6 kHz, which indicated that 2.3% of those workers had speech frequency hearing loss, 10.2% had high-frequency hearing loss, and 10.3% had bilateral hearing loss. These prevalences were lower than that in the U.S. population aged 20 to 69 years, in which 16.1% had speech frequency hearing loss and 31% had high-frequency hearing loss15. Dan Kuang et al16. showed that the prevalence of high-frequency hearing loss among employees at a certain automobile factory in China was 7.0%. In addition, Zhou et al17. reported that noise workers in Chinese petrochemical enterprises had more severe hearing loss, with speech frequency and high-frequency hearing loss rates of 3.7% and 30.6%, respectively, and Lawson et al10. reported that the detection rate of hearing loss in petrochemical enterprise workers was 14.0% in a 10-year cohort study. This may be related to factors such as the age of the target population, the duration of exposure to noise, and other conditions that could lead to hearing loss, such as exposure to environmental noise or other ear-related diseases.
Our results indicated that individuals with speech frequency hearing loss were more likely to be older, work shifts, and have a family history of hyperlipidaemia than those with a normal hearing level. Study shows that, Older age might result in the loss of neurons and their density and a decrease in cochlear blood flow, increasing their vulnerability to noise damage16. Similarly, studies have shown that a key factor contributing to the development of occupational noise-induced hearing loss is age18. Owing to the particularity of petrochemical enterprises, some employees need to work in shifts, they may be exposed to noise for a longer time, which could lead to hearing damage. Hyperlipidaemia can lead to damage to vascular endothelial cells, causing vascular diseases such as atherosclerosis. These vascular changes may affect the microcirculation of the inner ear, reducing the blood supply to the auditory nerves and hair cells and thereby impairing hearing.
This study revealed that both speech frequency and high-frequency hearing loss were significantly associated with noise exposure time. Workers with a noise exposure duration of ≥ 10 years had a greater prevalence of hearing loss. Additionally, a long-term follow-up study by the National Institutes of Health (NIH) revealed that the incidence of speech frequency hearing loss among workers exposed to high noise levels for a long period of time is much greater than that in the general population. Research suggests that long-term or high-intensity noise exposure is one of the main causes of high-frequency hearing loss16. Therefore, it is particularly important for individuals frequently exposed to high-noise environments to take necessary protective measures. Our results are consistent with those of previous studies, which revealed that nonoccupational characteristics, such as gender, smoking, and high systolic and diastolic blood pressure, are associated with high-frequency hearing loss and bilateral hearing loss19,20. Additionally, some studies have reported that gender is a risk factor for occupational noise-induced hearing loss, with the risk being greater in males than in females17,21. This difference may be due to the significant variation in noise intensity at work between men and women. Compared with female workers, male workers are usually exposed to greater noise intensity in their workplace16. Another possible explanation may be the physiological differences induced by hormones between sexes. Relevant studies have shown that oestrogen and its signalling pathways may protect women from hearing loss21.
In this study, we observed that smokers had a significantly greater risk of high-frequency hearing loss. Smoking was found to be associated with an increased risk for hearing loss22. Wang D et al23. also reported that smoking was an independent risk factor for NIHL, and there was a dose‒response relationship between smoking and NIHL risk. However, the specific pathogenic mechanisms underlying how smoking increases the risk of hearing loss are not well understood. Available evidence has revealed that smoking may damage cochlear hair cells and cause hearing loss by increasing carboxyhaemoglobin and reducing cochlear blood flow to the cochlea. Therefore, quitting smoking may help prevent hearing loss. Many previous studies have investigated the associations between hearing loss and blood pressure as well as hypertension. However, the results have been inconsistent. Ni CH et al. reported that the SBP and DBP in a high-frequency hearing loss group were significantly greater than those in a normal hearing group among 618 noise-exposed workers24. Another study reported that hearing loss at high frequency (4 kHz) is significantly associated with mean blood pressure and hypertension among 119 black male workers25. Our findings are consistent with those of the aforementioned study, which revealed that high-frequency hearing loss and bilateral hearing loss are associated with increased risks of SBP and DBP. However, a cross-sectional study involving 790 aircraft-manufacturing workers revealed that SBP and DBP were not significantly different among those affected by hearing loss in that study26. The reason for the inconsistency between this study and our findings may be related to the age of the target population, the severity and type of hearing loss, and other potential confounders such as lifestyle, diet, and exercise. Therefore, for more accurate conclusions, future studies need to control and analyse these aspects more meticulously.
Our study indicates that occupational noise exposure among petrochemical enterprise employees is positively correlated with the risk of hearing loss. This finding is consistent with the findings of other studies10,11. Research has indicated that, after controlling for other factors, occupational noise exposure is an independent factor leading to speech frequency hearing loss and high-frequency hearing loss. At frequencies of 3000 Hz, 4000 Hz, and 6000 Hz, compared with participants with noise exposure levels < 80 dB(A), after adjusting for potential confounding factors, the hearing loss risk was significantly greater in the 80–89 dB(A) noise exposure group. However, the results revealed that, compared with participants with noise exposure levels < 80 dB(A), the group with noise exposure levels ≥ 90 dB(A) was associated with a greater prevalence of speech frequency, high frequency, and bilateral hearing loss. These findings indicate that long-term exposure to high-intensity occupational noise significantly increases the risk of hearing loss among workers. Therefore, strengthening noise control and improving hearing protection measures are crucial for effectively preventing excessive occupational noise exposure, thereby reducing the risk of hearing loss in workers.
In summary, the noise hazards in this petrochemical enterprise are quite serious. Long-term exposure to occupational noise significantly increases the risk of hearing loss among workers. Therefore, taking effective hearing protection measures is crucial to reduce the risk of hearing loss among employees. Enterprises need to provide professional noise-reducing earplugs or earmuffs to isolate external noise and maintain the hearing health of employees. Moreover, it is necessary to arrange employees’ work and rest time reasonably, avoid being in a noisy environment for a long time, and conduct regular hearing examinations to detect and address hearing problems in a timely manner. In addition, it is important to strengthen noise pollution management and control at the social and environmental levels.
This study has several advantages. First, we discuss the current situation of workers’ hearing loss, including frequencies from 0.5–6 kHz, speech frequencies, and high frequencies, which is comprehensive. Second, we employed precise hearing test techniques to enhance the reliability of the data. We also analyzed the potential impact of different ages and genders on hearing loss, which adds a richer dimension to the research findings. However, this study also has several limitations. First, the present study was conducted in Hainan Province and may not represent the national level; however, because Hainan Province is an important city of economic development, it is significant for estimating the prevalence of hearing loss among working professionals. Second, this study was based on a cross-sectional survey, which cannot reveal causal relationships and cannot appropriately assess associations. Prospective cohort studies are needed to verify these results in the future. Third, we did not collect information on the use of earplugs by employees or nonoccupational noise exposures, which may have affected the research results. In our future research, we will pay more attention to collecting the above data, which can make our research more convincing.
Data availability
“The datasets generated and/or analyzed during the current study are not publicly available because the data involve personal information of occupational workers. However, they are available from the corresponding author upon reasonable request.”
References
Tak, S. et al. Exposure to hazardous workplace noise and use of hearing protection devices among US workers–NHANES, 1999–2004. Am. J. Ind. Med. 52(5), 358–371. https://doi.org/10.1002/ajim.20690 (2009).
Li, X. et al. Epidemiological characteristics of hearing loss among noise-exposed workers in Chinese industrial enterprises in 2020. Chin. J. Dis. Control. Prev. 26(08), 882–887 (2022) ((in chinese)).
Lie, A. et al. Occupational noise exposure and hearing: a systematic review. Int. Arch. Occup. Environ. Health 89(3), 351–372. https://doi.org/10.1007/s00420-015-1083-5 (2016).
Dobie, R. A. The burdens of age-related and occupational noise-induced hearing loss in the United States. Ear Hear. 29(4), 565–577. https://doi.org/10.1097/AUD.0b013e31817349ec (2008).
Chadha, S., Kamenov, K. & Cieza, A. The world report on hearing, 2021. Bull. World Health Organ. 99(4), 242-242A. https://doi.org/10.2471/BLT.21.285643 (2021).
Carroll, Y. et al. Vital Signs: Noise-induced hearing loss among adults - United States 2011–2012. MMWR. Morbidity & mortal. Wkly. rep. 66(5), 139–144. https://doi.org/10.15585/mmwr.mm6605e3 (2017).
Yu S. F. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi = Chinese journal of industrial hygiene and occupational diseases 34 12 881–883. (2016)
Basner, M. et al. Auditory and non-auditory effects of noise on health. Lancet (London, England) 383(9925), 1325–1332. https://doi.org/10.1016/S0140-6736(13)61613-X (2014).
Samant, Y., Parker, D., Wergeland, E. & Wannag, A. The norwegian labour inspectorate’s registry for work-related diseases: data from 2006. Int. J. Occup. Environ. Health 14(4), 272–279. https://doi.org/10.1179/oeh.2008.14.4.272 (2008).
Lawson, S. M., Masterson, E. A. & Azman, A. S. Prevalence of hearing loss among noise-exposed workers within the mining and oil and gas extraction sectors, 2006–2015. Am. J. Ind. Med. 62(10), 826–837. https://doi.org/10.1002/ajim.23031 (2019).
Wanhai, C. Investigation and analysis of noise hazards at a petrochemical enterprise worksite. Ind. Saf. & Environ. Prot. 45(12), 100–102 (2019).
WHO. Prevention of deafness and hearing impaired grades of hearing impairment. http://www.who.int/pbd/deafness/hearing_ impairment_grades/en/index.html Accessed date 25 Aug 2018
Wilson, B. S., Tucci, D. L., Merson, M. H. & O’Donoghue, G. M. Global hearing health care: new findings and perspectives. Lancet (London, England) 390(10111), 2503–2515. https://doi.org/10.1016/S0140-6736(17)31073-5 (2017).
Mirza, R., Kirchner, D. B., Dobie, R. A. & Crawford, J. ACOEM task force on occupational hearing loss occupational noise-induced hearing loss. J. Occup. & Environ. Med. 60(9), e498–e501 (2018).
Agrawal, Y., Platz, E. A. & Niparko, J. K. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the national health and nutrition examination survey, 1999–2004. Arch. Intern. Med. 168(14), 1522–1530. https://doi.org/10.1001/archinte.168.14.1522 (2008).
Kuang, D., Yu, Y. Y. & Tu, C. Bilateral high-frequency hearing loss is associated with elevated blood pressure and increased hypertension risk in occupational noise exposed workers. PLoS ONE 14(9), e0222135. https://doi.org/10.1371/journal.pone.0222135 (2019).
Zhou, J., Shi, Z., Zhou, L., Hu, Y. & Zhang, M. Occupational noise-induced hearing loss in China: a systematic review and meta-analysis. BMJ open 10(9), e039576. https://doi.org/10.1136/bmjopen-2020-039576 (2020).
Nyarubeli, I. P., Tungu, A. M., Moen, B. E. & Bråtveit, M. Prevalence of noise-induced hearing loss among tanzanian iron and steel workers: A cross-sectional study. Int. J. environ. Res. & public health 16(8), 1367. https://doi.org/10.3390/ijerph16081367 (2019).
Bento, R. F. & Sousa, N. C. Hearing health: A Major concern for the 21 st century. Int. Arch. Otorhinolaryngol. 23(3), e254–e255. https://doi.org/10.1055/s-0039-1692980 (2019).
Toppila, E., Pyykkö, I., Starck, J., Kaksonen, R. & Ishizaki, H. Individual risk factors in the development of noise-induced hearing loss. Noise & Health 2(8), 59–70 (2000).
Shuster, B. Z., Depireux, D. A., Mong, J. A. & Hertzano, R. Sex differences in hearing: Probing the role of estrogen signaling. J. Acoust. Soc. Am. 145(6), 3656. https://doi.org/10.1121/1.5111870 (2019).
Hu, H. et al. Japan epidemiology collaboration on occupational health study group smoking, smoking cessation, and the risk of hearing loss: Japan epidemiology collaboration on occupational health study. Nicotine & Tob. Res. : Official J Soc. Res. Nicotine & Tob. 21(4), 481–488 (2019).
Wang, D. et al. The combined effect of cigarette smoking and occupational noise exposure on hearing loss: evidence from the dongfeng-tongji cohort study. Sci. rep. 7(1), 11142. https://doi.org/10.1038/s41598-017-11556-8 (2017).
Ni, C. H. et al. Associations of blood pressure and arterial compliance with occupational noise exposure in female workers of textile mill. Chinese med. J. 120(15), 1309–1313 (2007).
Tarter, S. K. & Robins, T. G. Chronic noise exposure, high-frequency hearing loss, and hypertension among automotive assembly workers. J. Occup. & Environ. Med. official publication of the Industrial Medical Association 32(8), 685–689 (1990).
Chang, T. et al. High-frequency hearing loss, occupational noise exposure and hypertension: a cross-sectional study in male workers. Environ. health a glob. access sci. source 10, 35. https://doi.org/10.1186/1476-069X-10-35 (2011).
Acknowledgements
The authors would like to thank all those who generously allocated their time to this study.
Funding
This project received support from High-level Talent Scientific Research Startup Fund of Hainan Medical University (XRC190011), 2023 Hainan Medical College Graduate Student Innovative Scientific Research Project (No. HYYB2023A3).
Author information
Authors and Affiliations
Contributions
Presentation of research ideas, analyze the data, and manuscript drafting: ZS and SF. Collected the data: Y H, SW, JP, CL, and NZ. Data analysis guidance: Q W, and B Z. Conceptualization: Y N, and J W. Supervised this study: S X, Z Y. Conceived and designed the research and, reviewed, and critically edited the final draft of the manuscript: J Z, DY. All authors read and approved the final manuscript to be submitted or published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Ethics Committee of Hainan Medical University (HYLL-2022–247). All methods were performed in accordance with the relevant institutional and local guidelines and regulations and were conducted per the Declaration of Helsinki (2010). A signed informed consent form was obtained from all the study participants, and all the participants voluntarily completed the questionnaire.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Su, Z., Fan, S., Niu, Y. et al. The association between occupational noise exposure and hearing loss among petrochemical enterprise workers in Hainan, South China. Sci Rep 15, 9447 (2025). https://doi.org/10.1038/s41598-025-90023-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90023-1