Abstract
Antimicrobial-resistant bacteria (ARBs) are serious global threat because they make it difficult to treat infections with antibiotics. Recently, it has been demonstrated that ARBs are isolated from the oral cavities of elderly individuals in long-term care facilities. Because oral ARBs can cause systemic diseases such as bacteraemia and aspiration pneumonia, more attention must be given to protect the overall health of elderly people. To understand the prevalence of oral ARBs, more studies are needed in addition to previous studies. In this study, we investigated oral ARBs in elderly people receiving home health care (HHC) who had different lifestyles as residents in long-term care facilities. Among 98 HHC participants, Staphylococcus aureus, including 8 methicillin-resistant S. aureus (MRSA) strains, was isolated from 31 participants (31.7%), and 3rd-generation cephalosporin-resistant gram-negative bacteria (GNARB) were isolated from 18 participants (17.8%). An analysis of the relationship between oral ARBs and clinical status revealed that S. aureus/MRSA isolation was correlated with denture condition, while GNARB isolation was correlated with tube feeding. This study is the first comprehensive analysis of ARB carriage in the oral cavities of elderly people in HHCs. These results demonstrate the potential risk of oral ARB carriage and the importance of infection control in HHCs.
Similar content being viewed by others
Introduction
Antimicrobial-resistant bacteria (ARBs) increase the difficulty of treating infections with antibiotics. The spread of ARBs poses many challenges to societal infection control and public health. In particular, elderly people need to pay more attention to infectious diseases because they have weakened immunity to pathogens and often have systemic diseases. In addition, because elderly individuals are more likely to receive antimicrobial drugs, they may have a greater prevalence of ARBs1,2. Many antimicrobial agents are currently used to treat infections; as a result, many resistant bacteria have emerged. Among the many antimicrobial agents, β-lactams are among the most frequently used3, resulting in the emergence of β-lactam-resistant bacteria in many bacterial species. Among β-lactam-resistant gram-positive bacteria, methicillin-resistant Staphylococcus aureus (MRSA) is highly prevalent and problematic worldwide4. It is a major cause of nosocomial infections and tends to be detected in communities5,6. For β-lactam-resistant gram-negative bacteria, extended-spectrum β-lactamase (ESBL)-producing bacteria, including Acinetobacter, Pseudomonas, Escherichia and Klebsiella, which are resistant to β-lactam antibiotics, especially 3rd-generation cephalosporins, have emerged7,8,9.Carbapenems are effective against ESBL-producing bacteria, but carbapenem-resistant Enterobacteriaceae (CRE), Pseudomonas and Acinetobacter have recently emerged and have spread worldwide10. This increased prevalence of resistance makes antimicrobial selection for infections more complex and difficult. In addition, as these bacteria are isolated from not only human subjects, including blood, urea and stool, but also the environment, such as floors and toilet seats in hospitals, infection control against these bacteria is sometimes difficult.
Recently, these gram-negative resistant bacteria have been isolated from the oral cavity11,12,13. In addition, MRSA has also been isolated from the oral cavity14,15,16 The oral cavity is frequent the entry point for human-to-human or human-to-environment bacterial transmission (17). When considering the prevention of nosocomial ARB infection, we need to pay more attention to the presence of ARBs in the oral cavity. Furthermore, oral bacteria sometimes cause systemic diseases such as bacteraemia and pneumonia17.To prevent and treat oral ARB infections, it is important to understand the carriage of ARBs in the oral cavity.
On the basis of these findings, we previously isolated ARB from the oral cavities of residents in long-term-care facilities (LTCFs) and identified both GN-ARB and MRSA strains15,16. However, these studies were not sufficient for understanding ARB carriage status in elderly people because no information is available on the oral carriage of ARBs in people who live their daily lives at home. Therefore, this study focused on elderly individuals receiving home health care (HHC). We attempted to isolate 3rd-cephalosporine/carbapenem-resistant GN-ARB and MRSA strains from the oral cavity of HHC participants and analysed the relationship between ARB isolation and the clinical status of the participants.
Results
Participant characteristics
In this study, samples were collected by swabbing teeth and oral mucosa from 91 day-care rehabilitation users (DCRs) and 10 home visit rehabilitation users (HVRs). Medical information was obtained from the participants, including sex, age, presence of comorbidities, oral health assessment tool–Japanese version (OHAT-J), use of dentures, status of remaining teeth and functional oral intake scale (FOIS) score. Three participants were excluded from the study because no medical information was available. Ultimately, 98 participants were included in the study (89 DCR participants and 9 HVR participants). (Fig. S1) For all participants, the mean age was 84.7 years (range: 66–104 years) (Table S1). Of these, 38 (38.8%) were male. The OHAT-J of 98 participants had mean values of 0.05 to 0.51 for each score. As higher scores indicate a worse condition, relatively low values for each of the items in this study indicate relatively good oral hygiene.Two participants (2.0%) used tube feeding as per the FOIS survey. The most common preexisting diseases, in order, were dementia (47.0%), hypertension (41.8%), cerebrovascular disease (28.6%), cardiovascular disease (24.5%), diabetes (21.4%), fracture (21.4%), hyperlipaemia (12.2%) and osteoporosis (12.2%). There were no statistically significant differences between DCRs and HVRs regarding the medical information obtained in this study.
Isolation of oral antibiotic-resistant bacteria
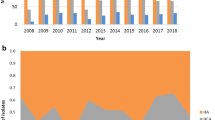
Staphylococcus aureus was isolated from 31 participants (31.6%) among 98 participants (Fig. 1a). This included 23 methicillin-susceptible Staphylococcus aureus (MSSA) isolates (23.5%) and 8 methicillin-resistant Staphylococcus aureus (MRSA) isolates (8.2%). Concerning the isolation rates of S. aureus by facility, the HVR participants had lower isolation rates (11.1%) than did the DCRs (33.7%), but there were no significant differences between them. The DCR had isolates from three facilities, and there were no significant differences in the isolation rates for both MSSA and MRSA between these facilities. For MRSA, no isolates were obtained from HVRs.
A total of 27 isolates of gram-negative 3rd-generation cephalosporin/carbapenem-resistant bacteria (GNARB) were isolated from 18 participants (Fig. 1b). Some participants had multiple strains isolated from a single isolation. The breakdown included 11 participants with only one isolate, five with two isolates, two with three isolates (Table. S2). Stenotrophomonas maltophilia was the most common isolate from 8 participants. Acinetobacter sp. was isolated from 11 participants and included three strains of Acinetobacter baumannii. Other isolates included two strains of Pantoea septica, two strains of Klebsiella pneumoniae, one each of Achromobacter xylosoxidans, Pseudomonas rhodesiae and Neisseria sp. A comparison of GNARB isolation rates by facility revealed isolation from 20.2% of DCRs but not from HVRs.
The association between GNARBs and S. aureus carriage was also investigated. (Table 1). For S. aureus and MSSA, participants who had GNARB strain were more likely to be carriers than those without (S. aureus, p = 0.024) (MSSA, p = 0.0305). On the other hand, when looking at the number of GNARB held, S. aureus and MSSA were predominantly found in groups holding only one share (S. aureus, p = 0.0038) (MSSA, p = 0.0185), but no correlation was found in groups holding two or three shares. When restricted to participants with two or more GNARB strains, there was no difference in retention. For MRSA, no association was found, irrespective of the number of GNARB strains carried.
Relationship between participant information and isolation of antibiotic-resistant bacteria
A statistical analysis was conducted to determine the relationship between isolated ARBs and the medical information collected. The isolation of S. aureus and MRSA (Table 2) was significantly correlated with the OHAT-J denture score (S. aureus, p = 0.0046) (MRSA, p = 0.0178). The denture score is a measure of denture fracture, breakage and availability. Score 1 means the denture is damaged in one place or can only be used for 1–2 h; score 2 means the denture is damaged in several places or is difficult to wear without denture adhesive. In addition, a higher score (> 8 points) on the OHAT-J total score was positively correlated with S. aureus isolation (p = 0.0296). No associations of S. aureus isolation with other items were found.
The isolation of GNARB (Table 3) was significantly correlated with FOIS levels: participants with FOIS levels 1–3 (routinely used tube feeding) were significantly more isolated than those with FOIS levels 4–7 (p = 0.0322). No associations of GNARB isolation with other items were found.
Characterization of the isolated antibiotic-resistant bacteria
Staphylococcus aureus and MRSA
Multilocus sequence typing (MLST) and phylogenetic tree analysis
After obtaining the whole-genome sequencing data, multilocus sequence typing (MLST) and phylogenetic tree analysis were performed (Fig. 2). Thirty-one S. aureus isolates were classified into 18 STs. The most frequent ST was ST8 (n = 6, 19.4%), followed by ST15 (n = 5, 16.1%), ST1 (n = 4, 12.9%) and ST97 (n = 2, 6.5%). Specifically, for MRSA, there were 3 strains of ST1, 2 strains of ST8 and 1 strain each of ST2725, ST380 and ST121. Phylogenetic tree analysis revealed that strains of ST1 and ST8 tended to have more AMR genes, while strains of ST15 and ST97 had fewer AMR genes.
Antimicrobial resistance (AMR) genes and susceptibility to antimicrobial agents
The AMR genes of the isolates are listed in the phylogenetic tree (Fig. 2). The most frequently identified AMR gene was blaZ (n = 22, 71.0%). Among these isolates, 8 also harboured mecA. Among the genes for resistance to macrolides, lincosamide and streptogramin B (MLSb) were detected in 12 isolates harbouring erm(A) (38.7%), and erm(C) was detected in 1 isolate (3.2%). The gene most frequently identified as acquiring resistance to aminoglycoside antimicrobials was ant(9)-la, which was harboured by 12 isolates (38.7%). The next most common gene was aac(6’)-aph(2’’), which was carried by 8 isolates (25.0%). Point mutations in gyrA and grlA, which are involved in quinolone resistance, were identified in 10 isolates (32.2%).
The minimum inhibitory concentrations (MICs) of the isolates for the 12 antimicrobial agents were determined by the microdilution method (Fig. 2). The association between the determined AMR and AMR gene retention was tested. The AMR gene carriage tended to be associated with resistance to relevant antimicrobial agents. (Fig. S2) BlaZ-positive MSSA strains were resistant to PCG and ABPC but susceptible to MPIPC CFDR and IPM, while MRSA strains (mecA- and blaZ-positive) were resistant to PCG, ABPC, MPIPC and CFDR (except one strain) and showed intermediate or strong susceptibility to IPM. ermA-positive strains, including MRSA and MSSA, showed resistance or intermediate resistance to erythromycin. All aac(6’)-aph(2”) positive strains showed resistance to GM, while all positive strains except one MRSA strain showed susceptibility or intermediate resistance to ABK. The point mutation of gyrA/grlA resulted in resistance to LVFX.
Virulence factors
Thirty virulence factors were identified (Fig. 2). Among the 31 isolates, the plasminogen activator protein staphylokinase (sak) was identified in 21 strains. Staphylococcal complement inhibitor (SCN) was found in 24 strains. Aureolysin (Aur), which activates serine protease (SspA), was detected in all the isolates. Serine protease-like proteins A–F (SplA–F), a group of serine proteases, were isolated from 28 SplA isolates, 22 SplB isolates and 22 SplE isolates. The expression of the gamma-haemolysin locus (hlg), a pore-forming toxin, was confirmed in all the isolates for hlgA and hlgB. HlgC was confirmed in all but one isolate. Leukocidin (luk), a pore-forming toxin, was present in 29 strains. No strains without pore-forming toxins were identified. Enterotoxin was detected in 16 strains, and 14 genotypes were identified. The tst gene encoding toxic shock syndrome toxin-1 (TSST-1) was isolated from only two strains. For the epidermal differentiation factor (EDIN), one strain each harboured edinA and edinB. There was no significant correlation between the distribution of virulence factors and STs.
Gram-negative 3rd-generation cephalosporin/carbapenem-resistant bacteria
Multilocus sequence typing (MLST)
MLST was performed on A. xylosoxidans, A. baumannii, K. pneumoniae and S. maltophilia, for which existing classifications were established by MLST 2.0 (Center for Genomic Epidemiology) or pubMLST (Table. S3) A. xylosoxidans HASPN41 was newly identified as ST583. The three A. baumannii strains were all ST1431. The two K. pneumoniae strains were both ST268. S. maltophilia was the most common ST249, with 6 strains, and the other strains were ST5, ST29, ST1156, and ST1157, with one each. ST1156 and ST1157 were registered as new STs.
β-Lactamase genes and susceptibility to antimicrobial agents
Among the ESBL genes, only two strains of K. pneumoniae possessed blaCTX−M15 and blaTEM−1B, and the other carried blaCTX−M15, blaTEM−1B and blaOXA−1. Among the CPase genes, all 3 A. baumannii strains harboured blaOXA−98, and all 10 S. maltophilia strains harboured blaL1. In addition, β-lactamases were detected in one A. xylosoxidans strain (blaOXA114g), 3 A. baumannii strains (blaADC25) and 2 K. pneumoniae strains (blaSHV−11). (Table. S3)
The susceptibilities of all the isolates were evaluated. (Table. S4) K. pneumoniae strains are resistant to 3rd- or 4th-generation cephalosporins but are susceptible to IPM and antimicrobial agents other than ST. S. maltophilia strains exhibit multiple resistance to cephalosporins, carbapenems, and AMK. Other bacterial species showed resistance or intermediate resistance to CTX, a 3rd-generation cephalosporine, but were mostly susceptible to other antimicrobial agents.
Transmission of antibiotic-resistant bacteria between facilities
The isolates were investigated for possible intrafacility transmission (Fig. S3). For S. aureus, a group of strains with the same MLST was selected for pairwise distance analysis. The strains in the ST1 (n = 2), ST8 (n = 5), ST15 (n = 3) and ST97 (n = 2) groups were analysed. As a result, only one pair in ST97 had a pairwise distance of less than 40 SNPs (6 SNPs). Because isolate pairs with SNP differences less than the threshold of 40 SNPs are suspected to belong to the same strain18,19,20, this pair was suspected to have resulted from intrafacility transmission.
For GNARB, groups of strains that were the same species or had the same MLST were selected for pairwise distance analysis. The results showed that one pair of S. maltophilia strains (4 SNPs) and one pair of P. septica strains (0 SNPs) were suspected of exhibiting intrafacility transmission.
Comparison of oral antibiotic-resistant bacteria carriage in home health care (HHC) participants and residents of long-term-care facilities (LTCFs).
We previously studied the prevalence of oral ARBs, including 3rd -generation cephalosporin/carbapenem-resistant gram-negative bacteria and S. aureus/MRSA, in residents of long-term-care facilities (LTCFs)15,16. Participant information and the prevalence of oral ARBs were compared shown in Table S5. The participant status between HHC and LTCF was different in oral environment and comorbidities.
For S. aureus (Fig. 3.a, b), MRSA was isolated more often in LTCFs than in HHCs (17.1% vs. 8.2%, p = 0.0558). We found a similar trend in the distribution of MLST types, with the most abundant MLST types in both groups being ST8, ST15 and ST1, in that order. We also compared the SCCmec type of MRSA. Among the HHC participants, types IV (87%) and V (13%) were identified, while types IV (68%), I (28%) and II (4%) were identified in the LTCFs. Intrafacility transmission was more frequent in LTCFs than in HHCs (LTCFs: 4 pairs vs. HHCs: 1 pair) (Fig.S3).
For GNARB, there were 29 (29.6%) isolates in 98 HHC participants and 30 (20.5%) in 146 LTCF participants (shown in Fig. 3). The percentage of S. maltophilia in HHCs (35%) was significantly greater than that in LTCFs (3%), while the percentages of Enterobacterales (34%) and Pseudomonas (23%) in LTCFs were significantly greater than those in HHCs (Enterobacterales [14%] and Pseudomonas [3%]). ESBL-producing Enterobacterales were more frequently detected in LTCFs than in HHCs (6.8% vs. 2.0%, p = 0.1306). Acinetobacter sp. was frequently isolated from HHCs (35%) and LTCFs (27%). Regarding intrafacility transmission, one pair was suspected at the LTCFs, and two pairs were suspected at the HHCs, with different species of bacteria (LTCFs: P. aeruginosa, HHCs: S. maltophilia, P. septica). (Fig.S3)
Materials and methods
Experimental conditions and participants
We isolated S. aureus, including MRSA, and gram-negative antibiotic-resistant bacteria by swabbing the teeth and oral mucosa of participants who were day-care service users or house call clinic users. A total of 101 people participated in the study, 91 of whom were from three day-care facilities and 10 of whom were from a home visiting facility (Facility on DCR1 with 45, DCR2 with 28, DCR3 with 18 and HVR1 with 10). Samples were collected from August 2022 to January 2023. Medical information was obtained from the participants. Information on sex, age, functional oral intake scale (FOIS) score, and systemic history was obtained from medical records. The Oral Health Assessment Tool–Japanese edition (OHAT-J), denture use, and remaining tooth status were collected on-site by the dentist at the time of specimen collection. The OHAT-J is a tool for evaluating the oral condition of people21,22. In this method, visual examination of the lips, tongue, gingiva, mucosa, saliva, remaining teeth, oral cleaning status, toothache, and denture fracture and fit was performed. Each item is rated on a scale from 0 to 4. Higher scores indicate lower oral hygiene (https://www.ohcw-tmd.com/research). The FOIS is commonly used to measure dysphagia23. Higher FOIS scores indicate poorer oral hygiene.
Sample collection and culture conditions
Two swabs were used to collect specimens from the dentition and oral mucosa of all participants. One swab was plated on Staphylococcus medium No. 110 “Nissui” medium plates (Shimadzu Diagnostics Corporation, Japan) (No. 110 medium plate). The other was plated on CHROMagar ESBL medium plates (Kanto Chemical, Japan) and CHROMagar mSuper CARBA medium plates (Kanto Chemical, Japan), in that order. CHROMagar ESBL medium plates and CHROMagar mSuper CARBA medium plates are used for rapid and presumptive identification of ESBL-producing enterobacteria24. No. 110 medium plates were incubated at 37 °C for 24 h and then incubated at room temperature for 24 h. Among the positive colonies, no more than 4 yellow colonies were picked and grown on No. 110 medium plates at 37 °C for 48 h. A small sample of bacterial cells was harvested from each colony and suspended in 100 µL of CS buffer (100 mM Tris-HCl [pH 7.5], 150 mM NaCl, and 10 mM EDTA) containing 10 µg of lysostaphin (Sigma‒Aldrich). The bacterial suspensions were incubated at 37 °C for 15 min. The samples were then heated at 95 °C for 10 min. After centrifugation at 10,000 × g for 5 min, the supernatant was used as template DNA for PCR. PCR was performed using specific primers (R: 3’TATCACCATCAATCGCT5’, F: 3’GTTGTAGTTTCAAGTCTAAG5’) for S. aureus identification. The resulting S. aureus isolates were stored in a freezer (− 80 °C) prior to use. S. aureus was cultured in trypticase soy broth (Becton, Dickinson and Company) at 37 °C under aerobic conditions. MRSA was defined as positive for the mecA gene using genomic data from each isolate. CHROMagar ESBL medium plates and CHROMagar mSuper CARBA medium plates were incubated at 37 °C for 48 h. Positive colonies were grown on CHROMagar ESBL medium plates, CHROMagar mSuper CARBA medium plates, and Candida GE Agar (Shimadzu Diagnostics Corporation, Japan) at 37 °C for 24 h. The colonies cultured on Candida GE agar were determined to be Candida spp. and were excluded from the study. The bacterial species of each isolate were determined from the genomic data.
Genome sequencing of isolated bacterial strains
To determine the DNA sequence, DNA was extracted from each isolate. For Staphylococcus aureus, bacterial cells (1.5 mL) cultured overnight were centrifuged at 10,000 × g for 5 min, and the bacteria were suspended in 500 µL of CS buffer containing 1.5 µL of lysostaphin (5 mg/mL) and 1 µL of RNase (10 mg/mL). After incubation at 37 °C for 60 min, 50 µL of 10% SDS and 15 µL of proteinase K (5 mg/mL) were added and incubated at 55 °C for 3 h. An equal volume of Tris-saturated phenol (pH 8.0) was added, the mixture was centrifuged at 10,000 × g for 5 min after immersion, and the supernatant was collected. Phenol‒chloroform solution was added, and the samples were immersed. Then, the samples were centrifuged at 10,000 × g for 5 min, after which the supernatant was collected. Finally, the DNA was precipitated with ethanol. After centrifugation, the DNA was washed with 70% ethanol and dissolved in 100 µL of TE buffer.
For gram-negative drug-resistant bacteria, bacterial cells (2.0 mL) were centrifuged at 10,000 × g for 5 min, and the bacteria were mixed with 564 µL of TE buffer. Thirty microlitres of 10% SDS and 6 µL of proteinase K (10 mg/mL) were added, and the mixture was incubated at 37 °C for 30 min. Then, 100 µL of 5 M NaCl solution, 80 µL of CTAB/NaCl solution (10% CTAB, 0.7 M NaCl), and equal volumes of chloroform/isoamyl alcohol were added. The sample was centrifuged at 10,000 × g for 20 min, after which the supernatant was collected. An equal volume of phenol/chloroform/isoamyl alcohol was added, the mixture was centrifuged at 10,000 × g for 10 min, and the supernatant was collected. Then, 0.6 volumes of 2-propanol were added and allowed to permeate, and the mixture was centrifuged at 10,000 × g for several tens of seconds. The supernatant was removed, and finally, the DNA was precipitated with ethanol. After centrifugation, the DNA was washed with 70% ethanol and dissolved in 100 µL of TE buffer. Subsequently, DNA libraries were constructed and paired-end sequenced (2 × 150 bp) using the Illumina HiSeq X Five platform (Macrogen Japan Corporation). The Illumina read data for each isolate were used for de novo assembly using Shovill v1.1.0 Seemann T. Shovill: faster SPAdes assembly of Illumina 2018 (available from https://github.com/tseemann/shovill).
Genomic sequence data analyses
Bacterial species were identified from the genome library sequences using Kmer Finder 3.2 (Center for Genomic Epidemiology: https://cge.food.dtu.dk/services/KmerFinder/)25,26,27. Genes associated with antimicrobial resistance were analysed using ResFinder 4.4.2 (Center for Genomic Epidemiology)28,29,30. Virulence factors were analysed using VirulenceFinder 2.0 (Center for Genomic Epidemiology)25,30,31,32. MLST analysis was performed using MLST 2.0 (Center for Genomic Epidemiology) or pubMLST (https://pubmlst.org). Sequence type (ST) profiles not previously deposited were submitted to pubMLST (https://pubmlst.org) and received new designations. SCCmec typing was performed using SCCmecFinder 1.2 (Center for Genomic Epidemiology)30,33,34. S. aureus isolates were annotated using Prokka35, and the resulting gff files were used to obtain a linked core genome alignment via the Panaroo pipeline36. A maximum-likelihood tree was then created using RAxML version 8.2.1037. iTOL38 was used to construct the tree and metadata. S. aureus isolates with the same MLST were subjected to pairwise distance analysis to examine the possibility of intrafacility transmission. Isolate pairs with SNP differences less than the threshold of 40 SNPs and originating from different individuals within the same facility were considered to have the potential for intrafacility transmission18,19,20. To compare the number of SNPs in S. aureus and GNARB between HHCs and LTCFs, whole-genome sequence data for each LTCF isolate deposited in the NCBI database (BioProject accession nos.: S. aureus: PRJDB16315; GNARB: PRJDB14068 and PRJDB12075) were used.
MICs of various antimicrobial agents
MICs were determined by the microdilution method previously described39. After culturing each isolated strain overnight, the optical density (OD660) at 660 nm in TSB was adjusted to 1.0 (1 × 109 cells/mL). Next, the culture medium was diluted 100-fold with trypsin soy broth (TSB), and 10 µl (105 cells) were added to each well of a 96-well plate (Thermo Fisher Scientific, Waltham, MA, USA). Two-fold serial dilutions of each antimicrobial agent were prepared. After 24 h of incubation at 37 °C, the MIC was evaluated. For S. aureus, penicillin G (PCG), ampicillin (ABPC), oxacillin (MPIPC), cefdinir (CFDN), gentamicin (GM), arbekacin (ABK), erythromycin (EM), minocycline (MINO), and vancomycin (VCM) were used. For gram-negative ARB, the Vitek-2 system (bioMérieux, France) was used to evaluate the MICs of ABPC, piperacillin (PIPC), cefazolin (CEZ), cefotiam (CTM), ceftazidime (CAZ), cefpodoxime (CPDX), cefotaxime (CTX), cefozopran (CZOP), cefmetazole (CMZ), flomoxef (FMOX), ampicillin/sulbactam (A/S), cefoperazone/sulbactam (C/S), IPM, meropenem (MEPM), tazobactam/piperacillin (T/P), amikacin (AMK), MINO, sulfamethoxazole (ST), ciprofloxacin (CPFX), and fosfomycin (FOM). The MIC results were calculated using the Performance Standards for Antimicrobial Susceptibility Testing, 33rd Edition (CLSI, Clinical and Laboratory Standards Institute, USA)40.
Statistical analyses
The associations between the clinical characteristics of the participants and the detection of S. aureus, MRSA, and extended spectrum β-lactamase (ESBL)-producing or third-generation cephalosporin-resistant Enterobacterales bacteria were analysed by univariate analysis with Fisher’s exact test (p < 0.05). Continuous non-normally distributed variables were analyzed by the Mann–Whitney U-test. Multiple logistic regression analysis was performed for factors with p values less than 0.05 in the univariate analysis and the corrected p-values are stated. All the statistical analyses were performed using JMP Pro version 16 (SAS Institute, Cary, NC, USA).
Discussion
This study investigated the oral carriage of Staphylococcus aureus, methicillin-resistant Staphylococcus aureus (MRSA) and third-generation cephalosporin-resistant gram-negative bacteria (GNARB) in elderly patients receiving home health care (HHC) and analysed their respective characteristics. Ninety-eight participants in HHC were included. S. aureus was isolated from 31.7%, MRSA from 7.9% and GNARB from 17.8% of the oral cavities (including dentition, tongue and oral mucosa) of 98 participants (Fig. 1).
Several reports of S. aureus and MRSA isolation from the oral cavity have been published. Koukos et al. previously detected S. aureus in dental plaque or on the surface of the tongue in 154 healthy adults attending a dental hospital in Greece. (average:46, 49 or 50 years) S. aureus was detected in 27 (18%) patients, with no MRSA11. Hirose et al. studied saliva samples from 332 healthy university students in Japan (aged 18–45 years, average:20.5 years); S. aureus was detected in 88 (26.5%), and MRSA was detected in 4 (1.2%)41. In a survey of elderly people living in nursing homes, Silva et al. reported the prevalence of S. aureus and MRSA in the nasal, oral and rectal cavities of 150 LTCF residents and 76 bedridden patients in Brazil42. The prevalence of S. aureus and MRSA in the oral cavity was 22.7% (n = 34) and 8% (n = 12), respectively. Kwetkat A et al. reported the prevalence of S. aureus (29.5%) and MRSA (1.1%) in nasopharyngeal or oropharyngeal swabs from 529 residents (aged 65–103 years, average: 84.5 years) of nursing homes in Germany43. These reports suggest that the carriage rate of S. aureus, and particularly MRSA, may increase with age, but it is difficult to make a consistent comparison because of differences in isolation methods. We also previously reported the isolation of S. aureus (33.6%) and MRSA (17.1%) from the oral cavities of 146 residents (average age: 88.0 years) of long-term-care facilities16 using the same protocol as this study, and it was possible to accurately compare the results of this study. As a result, the S. aureus isolation ratio (31.7%) in HHC participants was similar to the isolation ratio in healthy persons and elderly LTCFs. However, the MRSA isolation ratio (7.9%) in HHC participants was greater than that in healthy personsbut was lower than that in LTCF participants.
In this study, we found a correlation between S. aureus/MRSA isolation and denture score (Table 2). S. aureus has been reported to attach to denture surfaces44,45,46 Mechanically damaged or poorly fit dentures may be an environment in which S. aureus can easily attach itself due to increased contact with the fingers because of their frequent wearing and removal and the difficulty involved in cleaning dentures. Raghavendran et al. reported that S. aureus in the oral cavity, including in dentures, can cause systemic infections such as aspiration pneumonia47. Garbacz et al. showed that S. aureus in denture wearers may be characterized by a greater tendency to establish in the oral cavity than in denture nonwearers48 As the management of dentures is left to the individual, HHC users may overlook defective dentures, unlike LTCF residents, whose carers tend to manage their dentures. Therefore, denture problems are considered risk factors for S. aureus colonization in the oral cavity.
For MRSA isolation, the isolation rate of LTCFs tended to be greater than that of HHCs, although there was no significant difference between them (17.1% vs. 8.2%, p = 0.0558, χ2 test). Previously, we reported that tube feeding was a risk factor for the colonization of MRSA in the oral cavity. However, among HHC participants, the percentage of tube feeding among HHC participants (only 2 participants [2.0%]) was lower than that among LTCF participants [15.8%]). Additionally, it has been reported that MRSA is transmitted through contact with health care providers and carers46; as a result, residents of LTCFs with high contact with carers may have been strongly affected. Therefore, the factors involved in MRSA colonization are likely different.
The MLST and SCCmec types of the MRSA isolates were compared between HHCs and LTCFs; SCCmec-IV was more commonly isolated in both HHCs and LTCFs (HHCs: 87%, LTCFs: 68%). Kaku et al. isolated 270 MRSA strains from blood cultures in 45 hospitals and reported that the main combination types were ST8-SCCmec-IV (30.7%) and ST1-SCCmec-IV (29.6%)49 Yamaguchi et al. analysed MRSA detected on skin or pus in 244 health care facilities and reported that the prevalence of SCCmec type IV was 75.8%, with an increasing trend50 Additionally, 51% of the SCCmecIV MRSA isolates were clonal complex 1 (CC1), which included 164 strains isolated from 13 hospitals located in Tokyo and surrounding prefectures51. The results of this and previous studies were similar to these trends.
In this study, oral GNARB was detected in 18 of 98 HHC participants (17.8%) (Fig. 1). We previously reported that it was 18.1% in dental outpatients (total 514 participants, average 69.5 years) and 17.1% in LTCF residents (total 146 residents; average age: 88.0 years)15,52,53. And Le MN et al. reported that 38% of residents (total 98 residents; average age: 83.3 years) had 3rd -generation cephalosporine/carbapenem-resistant gram-negative bacteria according to oropharyngeal swabs14. In three studies of these, similar to S. aureus colonization, tube feeding was significantly correlated with GNARB colonization. However, despite the low tube feeding rate of HHC participants (2.0%) compared to those in previous studies (6.1% [Le et al.], 12.9% [Kajihara et al.]), the GNARB isolation rate in HHC participants (17.8%) was similar to that in our previous study (17.1%), although its rate was lower than that in the study by Le et al. (38%). Therefore, other factors are involved in the colonization of GNARB in the oral cavity. Because the subjects of these studies were elderly individuals, it is speculated that complex factors such as antibiotic application history, oral and systemic immunity, and systemic diseases caused by ageing affect the colonization of ARBs. Notably, the detection rates for each isolate species differed between HHC and LTCF participants, with a high isolation rate of S. maltophilia and low isolation rate of Enterobacterales in HHCs. S. maltophilia was detected in 9.9% (n = 10) of HHCs and 0.7% (n = 1) of LTCFs (Fig. 3.c, d). Tada et al. isolated S. maltophilia from 10 participants (18.2%) in the oral cavities of 55 bedridden older people in hospitals and reported that all S. maltophilia-positive participants had dysphagia and speech disorders54. Therefore, dysphagia and speech disorders may be risk factors for oral carriage of S. maltophilia. However, the prevalence of these disturbances was quite low in our studies of HHCs and LTCFs. The prevalence of S. maltophilia could be influenced by complex oral factors, systemic independence and the living environment. S. maltophilia is an environmental bacterium of low virulence, but it is associated with high morbidity and mortality in susceptible hosts. There is concern that nosocomial and community-acquired infections will increase55. Prates et al. reported oral S. maltophilia infections in immunosuppressed, mechanically ventilated patients56. In addition, one of the HHC isolates in this study (ST1157) showed resistance to minocycline and trimethoprim-sulfamethoxazole, which are commonly used therapeutic agents (Table. S4). Therefore, S. maltophilia may represent a potential health risk in HHCs. Regarding the isolation of Enterobacterales, it is considered that differences in lifestyle, such as living independently, can affect the proportion of Enterobacteriaceae localized in the oral cavity.
In this study, a few cases of intrafacility transmission were suspected for S. aureus and GNARB (Fig.S3) For S.aureus, it is more likely to be transmitted in LTCFs than in HHCs. This may be due to the closer relationships and longer length of stay of residents in LTCFs than in HHCs. With regard to antimicrobial-resistant ESKAPE pathogens (E. faecium, S. aureus, K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter spp.) considered dangerous for nosocomial transmission57, P. aeruginosa was identified in only LTCFs, A. baumannii was identified in both facilities, and other species of ESKAPE were not found. Therefore, the transmission of these pathogens requires attention in HHCs as well as in LTCFs.
There is a limitation to this study. Because the study examined the possession of ARBs in participants at a single point in time, it is difficult to determine whether participants were continuous or transient carriers of the bacteria. To further validate the prevalence, it would be desirable to confirm the presence of ARBs over time.
To the best of our knowledge, this is the first comprehensive report on the prevalence and characteristics of S. aureus, MRSA, and GNARB in the oral cavities of HHCs. Our study investigated the prevalence, antibiotic susceptibility, medical information and their interrelationships in Japanese HHCs. We also identified unique trends in HHCs by comparing them with a survey of LTCFs. Our study highlights the potential risks of ARB retention in HHCs.
Statement of ethics
This study protocol was reviewed and approved by the Hiroshima University Hospital review board, approval number [E2022-0092]. This study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from the participants prior to their enrollment in the study.
Data availability
Genomic data for all isolates used in this study have been deposited in the DNA Data Bank of Japan (DDBJ)(https://www.ddbj.nig.ac.jp/index-e.html) under BioProject accession number PRJDB17936 (PSUB022776). Further inquiries can be addressed to the corresponding author.
References
Lu, N. et al. DNA microarray analysis reveals that antibiotic resistance-gene diversity in human gut microbiota is age related. Sci. Rep. 4, 4302 (2014).
Nys, S., van Merode, T., Bartelds, A. I. M. & Stobberingh, E. E. Antibiotic treatment and resistance of unselected uropathogens in the elderly. Int. J. Antimicrob. Agents. 27, 236–241 (2006).
Lima, L. M., Silva, B. N. M., da, Barbosa, G. & Barreiro, E. J. β-lactam antibiotics: an overview from a medicinal chemistry perspective. Eur. J. Med. Chem. 208, 112829 (2020).
Lakhundi, S. & Zhang, K. Methicillin-Resistant Staphylococcus aureus: molecular characterization, evolution, and Epidemiology. Clin. Microbiol. Rev. 31(4), e00020-18 (2018).
Vandenesch, F. et al. Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine Leukocidin genes: Worldwide Emergence - 9, number 8—August 2003 - emerging infectious diseases journal - CDC. Emerg. Infect. Dis. 9, 978–984 (2003).
Ruhe, J. J., Smith, N., Bradsher, R. W. & Menon, A. Community-onset methicillin-resistant Staphylococcus aureus skin and soft-tissue infections: impact of antimicrobial therapy on outcome. Clin. Infect. Dis. 44, 777–784 (2007).
Chong, Y., Shimoda, S. & Shimono, N. Current epidemiology, genetic evolution and clinical impact of extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae. Infect. Genet. Evol. 61, 185–188 (2018).
Kawamura, K. et al. ESBL-producing Escherichia coli and its Rapid rise among healthy people. Food Saf. (Tokyo). 5, 122–150 (2017).
Husna, A. et al. Extended-spectrum β-Lactamases (ESBL): challenges and opportunities. Biomedicines 11, 2937 (2023).
Tompkins, K. & van Duin, D. Treatment for carbapenem-resistant Enterobacterales infections: Recent advances and future directions. Eur. J.Clin. Microbiol. Infect. Dis. 40, 2053–2068 (2021).
Koukos, G. et al. Prevalence of Staphylococcus aureus and methicillin resistant Staphylococcus aureus (MRSA) in the oral cavity. Arch. Oral Biol. 60, 1410–1415 (2015).
de Leão-Vasconcelos, L. S. N. Enterobacteriaceae isolates from the oral cavity of workers in a Brazilian oncology hospital. Rev. Inst. Med. Trop. Sao Paulo. 57, 121–127 (2015).
Katkowska, M. et al. High oral carriage of multidrug resistant gram-negative bacilli in adolescents: the SOPKARD-Junior study. Front. Cell. Infect. Microbiol. 13, 1265777 (2023).
Le, M. N. T. et al. Oral colonisation by antimicrobial-resistant Gram-negative bacteria among long-term care facility residents: prevalence, risk factors, and molecular epidemiology. Antimicrob. Resist. Infect. Control. 9, 45 (2020).
Haruta, A. et al. Disinfectant susceptibility of third-generation-cephalosporin/carbapenem-resistant gram-negative bacteria isolated from the oral cavity of residents of long-term-care facilities. Appl. Environ. Microbiol. 89 (2023).
Kusaka, S. et al. Oral and rectal colonization of methicillin-resistant Staphylococcus aureus in long-term care facility residents and their association with clinical status. Microbiol. Immunol. https://doi.org/10.1111/1348-0421.13111 (2024).
Rathbun, K. P., Bourgault, A. M. & Sole, M. Lou. Oral microbes in Hospital-Acquired Pneumonia: practice and Research implications. Crit. Care Nurse. 42, 47–54 (2022).
Long, S. W., Beres, S. B., Olsen, R. J. & Musser, J. M. Absence of patient-to-patient intrahospital transmission of Staphylococcus aureus as determined by whole-genome sequencing. mBio 5, e01692–e01614 (2014).
Price, J. R. et al. Whole-genome sequencing shows that patient-to-patient transmission rarely accounts for Acquisition of Staphylococcus aureus in an Intensive Care Unit. Clin. Infect. Dis. 58, 609–618 (2014).
Golubchik, T. et al. Within-host evolution of Staphylococcus aureus during Asymptomatic Carriage. PLoS One. 8, e61319 (2013).
Benjapornlert, P. et al. Reliability and validity of Japanese version of the oral Health Assessment Tool (OHAT-J). J. Jpn Soc. Disab Oral Health. 37, 1 (2016).
Chalmers, J. M., King, P. L., Spencer, A. J., Wright, F. A. C. & Carter, K. D. The oral health assessment tool–validity and reliability. Aust Dent. J. 50, 191–199 (2005).
Sallum, R. A. A., Duarte, A. F. & Cecconello, I. Analytic review of dysphagia scales. ABCD Arquivos Brasileiros De Cirurgia Digestiva (São Paulo). 25, 279–282 (2012).
Saito, R. et al. Evaluation of a chromogenic agar medium for the detection of extended-spectrum β‐lactamase‐producing Enterobacteriaceae. Lett. Appl. Microbiol. 51, 704–706 (2010).
Clausen, P. T. L. C., Aarestrup, F. M. & Lund, O. Rapid and precise alignment of raw reads against redundant databases with KMA. BMC Bioinform. 19, 1–8 (2018).
Hasman, H. et al. Rapid whole-genome sequencing for detection and characterization of microorganisms directly from clinical samples. J. Clin. Microbiol. 52, 139–146 (2014).
Larsen, M. V. et al. Benchmarking of methods for genomic taxonomy. J. Clin. Microbiol. 52, 1529–1539 (2014).
Bortolaia, V. et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 75, 3491–3500 (2020).
Zankari, E. et al. PointFinder: a novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J. Antimicrob. Chemother. 72, 2764–2768 (2017).
Camacho, C. et al. BLAST+: Architecture and applications. BMC Bioinform. 10, 1–9 (2009).
Tetzschner, A. M. M., Johnson, J. R., Johnston, B. D., Lund, O. & Scheutz, F. In Silico genotyping of Escherichia coli isolates for extraintestinal virulence genes by use of whole-genome sequencing data. J. Clin. Microbiol. 58 (2020).
Joensen, K. G. et al. Real-time whole-genome sequencing for routine typing, surveillance, and outbreak detection of verotoxigenic Escherichia coli. J. Clin. Microbiol. 52, 1501–1510 (2014).
Kondo, Y. et al. Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob. Agents Chemother. 51, 264–274 (2007).
Ito, T. et al. Classification of staphylococcal cassette chromosome mec (SCCmec): guidelines for reporting novel SCCmec elements. Antimicrob. Agents Chemother. 53, 4961–4967 (2009).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Tonkin-Hill, G. et al. Producing polished prokaryotic pangenomes with the Panaroo pipeline. Genome Biol. 21 (2020).
Stamatakis, A. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 30, 1312 (2014).
Letunic, I. & Bork, P. Interactive tree of life (iTOL) v5: an online tool for phylogenetic tree display and annotation. Nucleic Acids Res. 49, W293 (2021).
Kawada-Matsuo et al. Involvement of the novel two-component NsrRS and LcrRS systems in distinct resistance pathways against nisin A and nukacin ISK-1 in Streptococcus mutans. Appl. Environ. Microbiol. 79, 4751–4755 (2013).
Clinical and Laboratory Standards Institute (CLSI). Performance standards for Antimicrobial susceptibility testing. CLSI Supplement M100. (2023).
Hirose, M. et al. Genetic characterization of Staphylococcus aureus, Staphylococcus argenteus, and coagulase-negative Staphylococci colonizing oral cavity and hand of healthy adults in Northern Japan. Pathogens 11 (2022).
Silva, L. P. et al. Molecular epidemiology of Staphylococcus aureus and MRSA in bedridden patients and residents of long-term care facilities. Antibiotics (Basel) 11 (2022).
Kwetkat, A. et al. Naso- and oropharyngeal bacterial carriage in nursing home residents: impact of multimorbidity and functional impairment. PLoS One. 13, e0190716 (2018).
Tawara, Y., Honma, K. & Naito, Y. Methicillin-resistant Staphylococcus aureus and Candida albicans on denture surfaces. Bull. Tokyo Dent. Coll. 37, 119–128 (1996).
Garbacz, K., Kwapisz, E. & Wierzbowska, M. Denture stomatitis associated with small-colony variants of Staphylococcus aureus: a case report. BMC Oral Health. 19, 219 (2019).
O’Donnell, L. E. et al. Dentures are a Reservoir for respiratory pathogens. J. Prosthodont. 25, 99–104 (2016).
Raghavendran, K., Mylotte, J. M. & Scannapieco, F. A. Nursing home-associated pneumonia, hospital-acquired pneumonia and ventilator-associated pneumonia: the contribution of dental biofilms and periodontal inflammation. Periodontology 2000. 44, 164–177 (2007).
Garbacz, K., Jarzembowski, T., Kwapisz, E., Daca, A. & Witkowski, J. Do the oral Staphylococcus aureus strains from denture wearers have a greater pathogenicity potential? J. Oral Microbiol. 11, 1536193 (2019).
Kaku, N., Sasaki, D., Ota, K., Miyazaki, T. & Yanagihara, K. Changing molecular epidemiology and characteristics of MRSA isolated from bloodstream infections: nationwide surveillance in Japan in 2019. J. Antimicrob. Chemother. 77, 2130–2141 (2022).
Yamaguchi, T. et al. Changes in the genotypic characteristics of community-acquired methicillin-resistant Staphylococcus aureus Collected in 244 medical facilities in Japan between 2010 and 2018: a Nationwide Surveillance. Microbiol. Spectr. 10, e0227221 (2022).
Ogura, K. et al. Predominance of ST8 and CC1/spa-t1784 methicillin-resistant Staphylococcus aureus isolates in Japan and their genomic characteristics. J. Glob Antimicrob. Resist. 28, 195–202 (2022).
Kajihara, T. et al. Oral and rectal colonization by Antimicrobial-Resistant Gram-Negative Bacteria and Their Association with death among residents of Long-Term Care facilities: a prospective, Multicenter, Observational, Cohort Study. Gerontology 69, 261–272 (2023).
Kawayanagi, T. et al. The oral cavity is a potential reservoir of gram-negative antimicrobial-resistant bacteria, which are correlated with ageing and the number of teeth. Heliyon 10, e39827 (2024).
Tada, A., Shiiba, M., Yokoe, H., Hanada, N. & Tanzawa, H. Relationship between oral motor dysfunction and oral bacteria in bedridden elderly. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 98, 184–188 (2004).
Brooke, J. S. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin. Microbiol. Rev. 25, 2–41 (2012).
Prates, M. et al. Oral infection caused by Stenotrophomonas maltophilia: A rare presentation of an emerging opportunistic pathogen. Case Rep. Infect. Dis. 6346120 (2020).
Pendleton, J. N., Gorman, S. P. & Gilmore, B. F. Clinical relevance of the ESKAPE pathogens. Expert Rev. Anti Infect. Ther. 11, 297–308 (2013).
Acknowledgements
We thank all the institutions and participants for their cooperation in this study and the colleagues who helped us with the survey.We acknowledge the contributions and support of Tomomi Nakamura at Nakamura Hospital, PIA Group Medical Corporation. We would also like to thank Junzo Hisatsune and Yo Sugawara for their technical assistance.
Funding
This study was supported by the Ministry of Health, Labour, and Welfare Japan (program Grant No. 21HA2009).
Author information
Authors and Affiliations
Contributions
MK, HO, MS, HS and HK contributed to designing and conceptualizing the study. SN, AF, AH, YH and MY isolated the strains. SN performed the susceptibility testing. SN, MNL, TK , MS and HK performed the identification of bacterial species and genome analyses. SN created the shown in Figures and tables. MK and MNL contributed to the majority of the experiments and participated in interpreting the data. SN and HK wrote the manuscript, and TK, TA, HO, MS and HS edited the manuscript. All the authors read and approved the final version of the manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nishihama, S., Kawada-Matsuo, M., Le, M.NT. et al. Oral colonization of antimicrobial-resistant bacteria in home health care participants and their association with oral and systemic status. Sci Rep 15, 5776 (2025). https://doi.org/10.1038/s41598-025-90037-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90037-9