Abstract
This case–control study aimed to investigate the association between family history of pelvic organ prolapse (POP) and its development, combined with known clinical risk factors, in Japanese women. Participants included patients aged ≥ 40 years with and without POP. Self-reported questionnaires assessed delivery methods, disease history, and family history until third-degree relatives. Overall, 305 patients with POP and 338 healthy controls were included. After age-matching, a good balance was achieved between the groups (n = 129 each), with a mean age of 67.7 ± 8.3 years in the POP group and 67.4 ± 8.3 years in the control group. Multivariable logistic regression analysis revealed that the POP group had a significantly higher odds ratio for family history of POP (3.06 [1.09–8.56]; p = 0.03), body mass index (BMI) (1.12 [1.03–1.22]; p = 0.01), and parity (1.51 [1.20–1.89]; p = 0.001). An area under the curve of 0.693 was achieved with a family history of POP, BMI ≥ 23.1 kg/m2, and parity ≥ 3 for differentiation between the POP and control groups. This suggests that family history of POP combined with BMI and parity may be useful predictors for POP development in Japanese women.
Similar content being viewed by others
Introduction
Pelvic organ prolapse (POP), characterized by the descent of pelvic organs into the vagina, is a prevalent condition in middle-aged and older women, significantly impacting their quality of life owing to bladder, bowel, and sexual dysfunction 1. While the prevalence of symptomatic POP is reported to be approximately 3–6%, vaginal examinations reveal a much higher prevalence, reaching up to 41–50% 2. In Japan, stage II or greater POP, utilizing POP-quantification (POP-Q), has been shown to affect 17.1% of the women 3. The management of mild POP often requires nonsurgical approaches, including pelvic floor muscle training, pessary, and lifestyle modifications to prevent further progression. However, advanced stages (stage ≥ III) typically require surgical interventions. Therefore, prediction based on distinct acquired risk factors is necessary to prevent the development of advanced POP.
The etiology of POP is likely multifactorial, including mainly acquired risk factors, such as aging, parity, and obesity 4. Accumulating evidence from a systematic review/meta-analysis of family history of POP 5, a twin study on heritability 6, single-nucleotide polymorphism (SNP) analyses 7,8,9,10, and a genome-wide association study (GWAS) 11 have also suggested the potential genetic risk of POP. Epidemiological studies on POP are more frequently reported from Europe than from Asia; thus, a national survey on risk factors for POP, taking into account differences in race and lifestyle, is needed. In line with this, our recent study identified an association between specific SNPs in lysyl oxidase-like 4 (LOXL4), an enzyme essential for extracellular matrix remodeling, and POP occurrence in Japanese women for the first time 7. Therefore, we hypothesized that family history could be useful to predict risk factors for POP.
To this end, this case–control study aimed to investigate the association between a family history of POP and development of POP in Japanese women, in addition to established acquired risk factors for POP.
Results
Characteristics of the study participants
Matching achieved good balance between groups (n = 129 each), with a mean age of 67.7 ± 8.3 years in the POP group and 67.4 ± 8.3 years in control group (Fig. 1).
Recruitment flowchart of the study participants. A total of 299 patients with POP were recruited from outpatients at multiple institutes in Okinawa, Japan. Healthy women aged ≥ 40 years were recruited from 1148 participants at community- and institution-based health check-ups. Of the 1148 participants, 344 volunteered and answered the questionnaires (30.0% response rate). Considering the 6 newly diagnosed cases, a total of 305 patients in the POP group and 338 participants in the control group were included. Age-matching was achieved in the POP and control groups (n = 129 each) in the final analysis. POP pelvic organ prolapse.
Among the baseline characteristics (Table 1), body mass index (BMI), parity, and cases of hypertension and breast cancer history were significantly higher in the POP group than in the control group. In contrast, cases of prior smoking history and clerical jobs were lower in the POP group.
These characteristics were applicable to the overall cases and controls prior to age-matching (Supplementary Table S1), in whom diabetes mellitus and history of hysterectomy were also higher in the POP group, compared with the control group. In addition, the overall cases and controls showed that vaginal delivery rates and birth weights were significantly higher in the POP group than in the control group until the fourth child (Supplementary Table S2).
Characteristics of lower urinary tract symptoms (LUTS)
All participants completed the Overactive Bladder Symptom Score (OABSS) questionnaire. Overactive bladder (OAB) was defined as an OABSS total score of ≥ 3, with a score of ≥ 2 for Question 3 12. Table 2 demonstrates significantly higher total OABSS scores, particularly for Questions 1 (day-time frequency), 3 (urgency) and 4 (urgency incontinence), in the POP group compared to that in the control group. In Question 2 (night-time frequency), there was no significant difference between the groups. The prevalences of OAB in the control and POP groups were 18.1% and 57.0%, respectively (p < 0.0001).
Multivariable analysis for POP risk factors
Table 3 shows multivariable conditional logistic regression analysis after age adjustment. In addition to BMI and parity, the POP group had a significantly higher odds ratio for family history of POP (3.06 [95% CI, 1.09–8.56]; p = 0.03) and hypertension (1.95 [95% CI, 0.03–3.70]; p = 0.04).
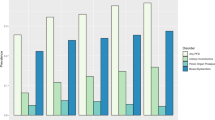
Receiver operating characteristic (ROC) curves for BMI, parity, and family history
Multivariable analysis revealed that BMI, parity, hypertension, and family history of POP in third-degree relatives were independent risk factors for POP incidence. ROC curve analysis (Fig. 2) was performed for the three risk factors: BMI, parity, and family history of POP. The area under the curve (AUC) for BMI was 0.644 (95% CI, 0.576–0.711) with a best cutoff value of 23.1 kg/m2, resulting in a sensitivity and specificity of 0.713 and 0.543, respectively (Fig. 2A). The AUC for parity was 0.643 (95% CI, 0.576–0.710) with a best cutoff value of 3.0, resulting in a sensitivity and specificity of 0.705 and 0.524, respectively (Fig. 2B). Finally, the AUC after combining these cutoff values with or without a family history of POP was 0.693, with a sensitivity and specificity of 0.535 and 0.771, respectively (Fig. 2C).
ROC curve analysis for predicting the risk of POP. (A) POP risk for BMI with continuous variable: The AUC is 0.644 (95% CI 0.576–0.711), and the best cut off value is 23.1 kg/m2; sensitivity and specificity are 0.713 and 0.543, respectively. (B) POP risk for parity with continuous variable: The AUC is 0.643 (95% CI 0.576–0.710), and the best cut off value is 3.0; sensitivity and specificity are 0.705 and 0.524, respectively. (C) POP risk for combined cutoff value of BMI and parity and POP family history with categorical variables: The AUC is 0.693; sensitivity and specificity are 0.535 and 0.771, respectively. ROC receiver operating characteristic, POP pelvic organ prolapse, AUC area under the curve, BMI body mass index.
Discussion
The key findings of this case–control study were as follows. First, a family history of POP, including within the third-degree relatives, was more frequent in the POP group, which is a novel finding in the Japanese population. Second, age, BMI, parity, and hypertension were also more prevalent in the POP group than in the control group as previously reported 4,13. Third, ROC analysis revealed a combined AUC of 0.693 using three criteria (BMI ≥ 23.1 kg/m2, parity number ≥ 3, and family history of POP), obtaining a sensitivity of 0.533 for differentiating POP cases. Fourth, OAB prevalence was significantly higher (57.0%) in the POP group than in the control group. Last, among healthy participants from community- and institution-based health check-ups, approximately 1.7% were newly diagnosed with POP.
Several studies have reported on the genetic risk factors for POP 5,6,7,11,14,15. A large population-based study on twin sisters in Sweden reported the influence of environmental and genetic factors on POP occurrence 6. Similarly, a systematic review and meta-analysis showed that a positive family history of POP increased the risk of POP by 2.3–2.7 times 5. Consistent with previous reports, the present study revealed an odds ratio of 3.06 for a family history of POP 5,6,14,15. To the best of our knowledge, this is the first report within a Japanese population, which underscores the importance of our findings. The synthesis and metabolism abnormalities of extracellular matrix (ECM) in pelvic floor such as collagen or elastin have been considered the cause of POP, so the SNPs associated the ECM components and metabolic enzyme have been studied widely 8. Thus, our recent study linked POP occurrence in Japanese women with SNPs in LOXL4 (odds ratio, 3.8–4.5), an enzyme involved in collagen and elastin fiber maturation, which is essential for extracellular matrix remodeling 7. In addition, a GWAS identified 19 novel loci as potential risk factors for POP 11. This report also demonstrated the potential of combining the polygenic risk score (PRS) with established clinical risk factors to improve POP prediction. Given that genomic backgrounds vary significantly across races and regions, conducting genetic research in Asian populations is crucial. As such, it is worth noting that family history of POP in the Japanese women of the present study is as an early and easy predictor for POP, especially in young females in the absence of social and lifestyle factors. In addition, combination of our proposed cutoff levels for two identified clinical factors (BMI ≥ 23.1 kg/m2 and parity ≥ 3) could serve as a valuable tool for evaluating POP risk.
Aging, obesity, and vaginal delivery are well-established risk factors of POP occurrence and recurrence postoperatively 4,16,17,18,19,20. These were also supported by our findings. The combined AUC for BMI, parity and hereditary risk factors exceeded that of the individual factors. Consistent with previous research 4, vaginal delivery emerged as a risk factor for POP, while cesarean section showed a protective effect (Supplementary Table S2). Moreover, the POP group displayed significantly higher birth weights than the control group. The association with delivery method and birth weight likely reflects damage to the pelvic floor structure during childbirth, potentially leading to POP after menopause.
Lifestyle characteristics are known to contribute to POP development 21. Comorbidities, such as hypertension and diabetes mellitus, have been established as risk factors for POP 22. In our study, a positive association between BMI, hypertension, and POP was observed, suggesting that lifestyle-related diseases might be a role in POP development. Regarding pulmonary conditions, increased intra-abdominal pressure owing to smoking and asthma may contribute to POP 21. Heart disease was also reported as a risk factor for POP, particularly as cardiac valve prolapse of collagen-associated disorders 23,24. Although our study showed a higher incidence of smoking history in the control group, neither smoking history nor pulmonary disease demonstrated a significant association with POP in the multivariable analysis. Heavy lifting jobs have also been linked to POP 25. In our present study, clerical jobs were less frequent in the POP group, but no association was found with occupations that would increase abdominal pressure. Clerical job is generally considered desk jobs, and non-heavy lifting jobs, which are occupations that do not chronically increase intra-abdominal pressure, might be a protective factor for POP. Collectively, these findings emphasize the need for large cohort studies or systematic reviews that encompass these factors to elucidate the mechanisms underlying POP.
Despite numerous studies on POP, epidemiological data on the natural history, occurrence, and prevalence of POP, particularly among healthy populations, remain scarce 2,3,16. Our study recruited healthy volunteers with a mean age of 57.5 years from community- and institution-based health checkups. Among the 344 participants, only 6 (1.7%) were newly diagnosed with POP based on Question 3 of the Pelvic Organ Prolapse Distress Inventory with six items (POPDI-6) in the Japanese Pelvic Floor Distress Inventory (J-PFDI-20) 26. The POP prevalence of 1.7% in our study may have been lower than that in previous reports: 17.1% in a single-center study by Kato et al. in Japan 3, and 30.8% and 37%, respectively, in Sweden and United States 16,27. Discrepancies between these studies are probably due to the following reasons. We used the POPDI-6 as a tool to exclude POP in healthy participants without vaginal examination, and most stage II patients were asymptomatic, potentially underestimating asymptomatic POP diagnosis in the present study. This highlights the necessity of precise questionnaires and standardized POP-Q grading to accurately determine the natural history and prevalence of POP.
Women with POP frequently experience various LUTS, including urinary frequency, urinary urgency, stress incontinence, and voiding difficulty. The reported prevalence of OAB in women with POP was approximately 37% 28, compared to the prevalence of 11.0% among Japanese women aged > 40 years based on a national health survey 29. While our study observed a similar OAB prevalence in the control group (18.1%), the POP group demonstrated a significantly higher prevalence (57.0%) compared to that in previous studies. This may be attributed to the greater severity of POP in our participants, who had symptoms associated with secondary obstruction and more prominently LUTS.
Anatomically, POP is classified into three stages according to the DeLancy level theory of pelvic floor structure 30. Levels I, II, and III disorders cause uterine prolapse, cystocele and rectocele, and urethrocele, respectively. Moderate disarrangement of levels I–III (i.e., more than stage III POP) usually requires surgical interventions such as laparoscopic sacrocolpopexy, native tissue repair, or minimally invasive surgeries with or without mesh 31. Therefore, prediction based on distinct family history and acquired risk factors such as this study might be useful to prevent the development of advanced POP.
Despite the important findings in the present study, some limitations must be acknowledged. First, the participants in the control group, recruited from community- and institution-based health checkups, might have their health orientation and wellness level than that of the case group recruited from hospital outpatients. Second, the sample size of the control group was relatively small. Ideally, control groups should have a sample size three times larger than that of the case group. Third, all comparisons between both groups relied on self-reported questionnaires, and POP-Q grading was not evaluated using vaginal examinations in the control group. Nevertheless, POP screening was conducted using the PFDI6, which has an 81% positive predictive value for clinically significant POP 16,32. Fourth, the POP group in our study comprised women with POP-Q stages III–IV requiring surgery, whereas those with mild POP (POP-Q stages I–II) were not included. However, given that patients with mild POP are often asymptomatic, the present study objectively represents real-world data for clinically significant POP. Fifth, recall bias of the POP family history in the case group cannot be ruled out. Last, this study serves as an exploratory investigation for POP risk factors. The AUC of our model, which includes three variables, was not as high as 0.693; further large-scale studies are therefore required to validate our findings.
In conclusion, this case–control study demonstrated the utility of subjective questionnaires for POP risk prediction. Furthermore, this study is the first of its kind in Japan, providing valuable clinical and genomic insights into POP development. A family history of POP, in addition to BMI ≥ 23.1 kg/m2, parity ≥ 3, in Japanese women emerged as independent predictors for POP, emphasizing their utility for evaluating POP risk.
Materials and methods
Study design and participants
This was a case–control study conducted from April 2020 to March 2023. Female patients with POP were recruited consecutively from outpatients with a POP-Q stage III or IV at Ryukyu University Hospital, Okinawa Kyodo Hospital, and Chibana Clinic, Okinawa, Japan, and 299 participated as the POP group in this study. For the control group, healthy women aged ≥ 40 years were recruited from the community- and institution-based health checkups at Naha City Lifestyle Related Disease Medical Center, Yanbaru Kenshin, and Chubu Tokushukai Kenshin Center, Okinawa, Japan, during the study period. From the initial pool of 1148 individuals, 344 agreed to participate and respond to the questionnaires (30.0% response rate). Notably, six of these participants were newly diagnosed with POP based on Question 3 of the POPDI-6 in the J-PFDI-20 26: “Do you usually have a bulge or something falling out that you can see or feel in your vaginal area?” Individuals that answered “yes” to this question were confirmed to have POP via telephone follow-up. Thus, a total of 305 patients in the POP group and 338 individuals in the control group were included in the final analysis. To adjust for the potential confounding effect of age, 1:1 age-matching was employed, and matching analysis was performed as the main analysis. The R programming language (version 4.2.0; R Foundation for Statistical Computing, Vienna, Austria) with the "optmatch” package was used for optimization matching 33.
The study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the University of Ryukyus for Medical and Health Research Involving Human Subjects (#1653). All participants provided written informed consent. All data were collected using the Research Electronic Data Capture (REDCap) System (https://ruqcap.med.u-ryukyu.ac.jp/redcap/) and were managed at the Academic Research Organization and Clinical Research Support Center of Ryukyu University Hospital.
Birth information and POP-related questionnaires
Participants were instructed to complete questionnaires regarding parity, delivery method (normal vaginal delivery or caesarean section), and childbirth weight. Data on family history of POP were obtained for first-degree (parents and children), second-degree (siblings and grandparents), and third-degree relatives (aunts and nieces). Participants in the control group who responded positively to the POPDI-6 questions were further assessed to definitively rule out POP.
Urinary tract symptom questionnaire
The participants were evaluated for LUTS using the OABSS questionnaire 12 to investigate lower urinary tract symptoms.
Additional data collection
Data on age, sex, height, body weight, occupation, and self-reported medical history, including hysterectomy, smoking status, pulmonary disease, hypertension, collagen disease, diabetes mellitus, and breast cancer were also collected.
Statistical analysis
Normally distributed data are expressed as means and standard deviations, whereas non-normally distributed data as medians and interquartile ranges. Basic clinical characteristics were compared between the two groups using an unpaired t-test, Wilcoxon rank-sum test (Mann–Whitney U test), or chi-squared test. Logistic regression analysis was employed to calculate the odds ratio and 95% CI of each parameter. The variables were selected from those that showed a significant difference in Table 1 and those that have been reported to be clinically significant POP risk factors. Therefore, an ROC curve was calculated to assess the risk prediction abilities of three factors for POP incidence (BMI, parity, and family history of POP). All statistical analyses were performed using JMP® pro version 15.0.0 (SAS Institute Inc., Cary, NC, USA), and two-tailed p-values were considered significant at p < 0.05.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to [a license agreement with the Academic Research Organization and Clinical Research Support Center of Ryukyu University Hospital] but are available from the corresponding author on reasonable request.
References
Molina-Barea, R., Slim, M. & Calandre, E. P. Health-related quality of life and psychosocial variables in women with colorectal pelvic floor dysfunction: A cross-sectional study. Healthcare https://doi.org/10.3390/healthcare12060668 (2024).
Barber, M. D. & Maher, C. Epidemiology and outcome assessment of pelvic organ prolapse. Int. Urogynecol. J. 24, 1783–1790. https://doi.org/10.1007/s00192-013-2169-9 (2013).
Kato, J., Nagata, C., Miwa, K., Ito, N. & Morishige, K. I. Pelvic organ prolapse and Japanese lifestyle: prevalence and risk factors in Japan. Int. Urogynecol. J. 33, 47–51. https://doi.org/10.1007/s00192-021-04672-7 (2022).
Jelovsek, J. E., Maher, C. & Barber, M. D. Pelvic organ prolapse. The Lancet 369, 1027–1038. https://doi.org/10.1016/s0140-6736(07)60462-0 (2007).
Samimi, P., Jones, S. H. & Giri, A. Family history and pelvic organ prolapse: A systematic review and meta-analysis. Int. Urogynecol. J. 32, 759–774. https://doi.org/10.1007/s00192-020-04559-z (2021).
Altman, D., Forsman, M., Falconer, C. & Lichtenstein, P. Genetic influence on stress urinary incontinence and pelvic organ prolapse. Eur. Urol. 54, 918–922. https://doi.org/10.1016/j.eururo.2007.12.004 (2008).
Ashikari, A., Suda, T. & Miyazato, M. Collagen type 1A1, type 3A1, and LOXL1/4 polymorphisms as risk factors of pelvic organ prolapse. BMC Res .Notes 14, 15. https://doi.org/10.1186/s13104-020-05430-6 (2021).
Li, L. et al. Genetic polymorphisms in collagen-related genes are associated with pelvic organ prolapse. Menopause 27, 223–229. https://doi.org/10.1097/GME.0000000000001448 (2020).
Allen-Brady, K. et al. Systematic review and meta-analysis of genetic association studies of pelvic organ prolapse. Int. Urogynecol. J. 33, 67–82. https://doi.org/10.1007/s00192-021-04782-2 (2022).
Ward, R. M. et al. Genetic epidemiology of pelvic organ prolapse: A systematic review. Am. J. Obstet. Gynecol. 211, 326–335. https://doi.org/10.1016/j.ajog.2014.04.006 (2014).
Pujol-Gualdo, N. et al. Advancing our understanding of genetic risk factors and potential personalized strategies for pelvic organ prolapse. Nat. Commun. 13, 3584. https://doi.org/10.1038/s41467-022-31188-5 (2022).
Homma, Y. et al. Symptom assessment tool for overactive bladder syndrome–overactive bladder symptom score. Urology 68, 318–323. https://doi.org/10.1016/j.urology.2006.02.042 (2006).
Colombage, U. N. et al. Occurrence and impact of pelvic floor dysfunction in women with and without breast cancer: A cross-sectional study. Braz. J. Phys. Ther. 26, 100455. https://doi.org/10.1016/j.bjpt.2022.100455 (2022).
Alcalay, M., Stav, K. & Eisenberg, V. H. Family history associated with pelvic organ prolapse in young women. Int. Urogynecol. J. 26, 1773–1776. https://doi.org/10.1007/s00192-015-2779-5 (2015).
Allen-Brady, K., Norton, P. A., Hill, A. J., Rowe, K. & Cannon-Albright, L. A. Risk of pelvic organ prolapse treatment based on extended family history. Am. J. Obstet. Gynecol. 223, 105e101–105e108 (2020). https://doi.org/10.1016/j.ajog.2019.12.271.
Swift, S. et al. Pelvic Organ Support Study (POSST): The distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am. J. Obstet. Gynecol. 192, 795–806. https://doi.org/10.1016/j.ajog.2004.10.602 (2005).
Akter, F., Gartoulla, P., Oldroyd, J. & Islam, R. M. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in Rural Bangladesh: A cross-sectional survey study. Int. Urogynecol. J. 27, 1753–1759. https://doi.org/10.1007/s00192-016-3038-0 (2016).
Bradley, C. S., Zimmerman, M. B., Wang, Q. & Nygaard, I. E. Vaginal descent and pelvic floor symptoms in postmenopausal women: A longitudinal study. Obstet. Gynecol. 111, 1148–1153. https://doi.org/10.1097/AOG.0b013e31816a3b96 (2008).
Awwad, J., Sayegh, R., Yeretzian, J. & Deeb, M. E. Prevalence, risk factors, and predictors of pelvic organ prolapse: A community-based study. Menopause 19, 1235–1241. https://doi.org/10.1097/gme.0b013e31826d2d94 (2012).
Vergeldt, T. F., Weemhoff, M., IntHout, J. & Kluivers, K. B. Risk factors for pelvic organ prolapse and its recurrence: A systematic review. Int. Urogynecol. J. 26, 1559–1573. https://doi.org/10.1007/s00192-015-2695-8 (2015).
Fitz, F. F., Bortolini, M. A. T., Pereira, G. M. V., Salerno, G. R. F. & Castro, R. A. PEOPLE: Lifestyle and comorbidities as risk factors for pelvic organ prolapse-a systematic review and meta-analysis PEOPLE: PElvic Organ Prolapse Lifestyle comorbiditiEs. Int. Urogynecol. J. 34, 2007–2032. https://doi.org/10.1007/s00192-023-05569-3 (2023).
Isik, H. et al. Are hypertension and diabetes mellitus risk factors for pelvic organ prolapse?. Eur. J. Obstet. Gynecol. Reprod. Biol. 197, 59–62. https://doi.org/10.1016/j.ejogrb.2015.11.035 (2016).
Lammers, K. et al. Pelvic organ prolapse and collagen-associated disorders. Int. Urogynecol. J. 23, 313–319. https://doi.org/10.1007/s00192-011-1532-y (2012).
Batista, N. C. et al. Collagen I and collagen III polymorphisms in women with pelvic organ prolapse. Neurourol. Urodyn. 39, 1977–1984. https://doi.org/10.1002/nau.24447 (2020).
Gillor, M., Saens, P. & Dietz, H. P. Demographic risk factors for pelvic organ prolapse: Do smoking, asthma, heavy lifting or family history matter?. Eur. J. Obstet. Gynecol. Reprod. Biol. 261, 25–28. https://doi.org/10.1016/j.ejogrb.2021.04.006 (2021).
Yoshida, M. et al. Reliability and validity of the Japanese version of the pelvic floor distress inventory-short form 20. Int. Urogynecol. J. 24, 1039–1046. https://doi.org/10.1007/s00192-012-1962-1 (2013).
Samuelsson, E. C., Victor, F. T., Tibblin, G. & Svärdsudd, K. F. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am. J. Obstet. Gynecol. 180, 299–305. https://doi.org/10.1016/s0002-9378(99)70203-6 (1999).
Lawrence, J. M., Lukacz, E. S., Nager, C. W., Hsu, J.-W.Y. & Luber, K. M. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet. Gynecol. 111, 678–685. https://doi.org/10.1097/AOG.0b013e3181660c1b (2008).
Mitsui, T. et al. Prevalence and impact on daily life of lower urinary tract symptoms in Japan: Results of the 2023 Japan Community Health Survey (JaCS 2023). Int. J. Urol. https://doi.org/10.1111/iju.15454 (2024).
DeLancey, J. O. Anatomic aspects of vaginal eversion after hysterectomy. Am. J. Obstet. Gynecol. 166, 1717–1724; (discussion 1724–1718). https://doi.org/10.1016/0002-9378(92)91562-o (1992).
Sahin, F., Ozdemir, S. & Dogan, O. Should sacrouterine plication be added to lateral suspension surgery? A prospective study. J. Obstet. Gynaecol. Res. 50, 1042–1050. https://doi.org/10.1111/jog.15941 (2024).
Murphy, A. M., Clark, C. B., Denisenko, A. A., D’Amico, M. J. & Vasavada, S. P. Surgical management of vaginal prolapse: Current surgical concepts. Can. J. Urol. 28, 22–26 (2021).
Hansen, B. B. & Klopfer, S. O. Optimal full matching and related designs via network flows. J. Comput. Graph. Stat. 15, 609–627. https://doi.org/10.1198/106186006x137047 (2006).
Acknowledgements
The authors would like to thank Yuki Hoshi, Keiko Higa, Masami Teruya, and Hitoshi Uehara for their data collection and management. We also thank Editage (www.editage.jp) for English language editing.
Funding
This work was supported by AMED Grant Number JP22gk0210025 and JSPS KAKENHI Grant Number 20K11158 and 24K20534.
Author information
Authors and Affiliations
Contributions
The contributions of each author are as follows. (1) Substantial contributions to the conception and design: A.A., A.T., H.I., Y.I., KOS.N., S.U., and M.M. (2) Data provision: K.K., S.N., N.M., and K.M. (3) Data analysis: A.A., A.T., H.I., S.U., and M.M. (4) Critical drafting and revision of the article for important intellectual content: A.A., K.K., A.T., H.I., S.N., N.M., Y.I., K.M., J.I., T.K., KOT.N., KOS.N., S.U., and M.M. All the authors have read and agreed to the published version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
All procedures involving human participants were conducted in accordance with the ethical standards of the institutional committee (Ethics Committee of the University of the Ryukyus, #20–1653-01–00-00, April 2020) and tenets of the 1975 Declaration of Helsinki, revised in 2013, or with comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ashikari, A., Kadekawa, K., Tokushige, A. et al. Family history and acquired risk factors for pelvic organ prolapse: a case–control study in Japan. Sci Rep 15, 5717 (2025). https://doi.org/10.1038/s41598-025-90202-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90202-0