Abstract
Background End-of-life (EOL) care aims to facilitate good death and fulfill the patient’s final desires. Despite the known benefits of palliative consultations, emergency physicians encounter challenges in decision-making due to limited palliative resources. Previous studies primarily focus on non-emergency settings; thus, we aimed to develop a practical prediction score for 7-day mortality for palliative patients in the emergency department (ED). Methods This retrospective cohort study, conducted at a tertiary-level university hospital in Thailand between June 2022 and May 2023, evaluated adult palliative patients who declined life-sustaining treatments. Variables associated with 7-day mortality were analyzed using univariable and multivariable logistic regression. Results Of 499 ED visits, 152 patients (30.46%) died within seven days. Six predictors were identified: solid malignancy, respiratory with mandibular movement, systolic blood pressure < 100 mmHg, lymphopenia, thrombocytopenia, and a blood urea nitrogen to creatinine ratio > 20. These factors were used to develop the Ramathibodi End-of-life (RAMA-EOL) score, demonstrating an AuROC curve of 80.46% (95% CI: 76.15–84.77). Patients with a score ≥ 3 had a positive likelihood ratio of 2.92 (95% CI: 2.38–3.57) for 7-day mortality. Conclusion The RAMA-EOL score reliably predicts 7-day mortality in palliative ED patients, facilitating timely palliative care interventions for high-risk individuals.
Similar content being viewed by others
Introduction
‘End-of-life (EOL) care’ refers to care given to patients with life-limiting illnesses as their conditions progressively deteriorate and they eventually die, typically within a year1. The main objectives of EOL care are to alleviate patients’ suffering symptoms, improve the quality of life, and fulfill both patients and their families’ psychosocial and spiritual needs, including arranging for a proper place of death1,2. Even though up to one-third of the population visited an emergency department (ED) in the final month of their life3, only 18% of palliative patients had documented advanced care planning, and as many as 23% of them, unfortunately, died in the ED4. Numerous prior studies have established the benefits of attending palliative specialists and transferring patients to hospice wards5,6,7. However, due to the increasing patient volume, lack of palliative providers, and limited number of hospice beds, appropriate ED consultations and dispositions remain a significant concern.
Currently, there is no standard prediction tool for anticipating the timing of a patient’s death, and several studies have shown that clinician intuition is an unreliable approach8,9,10,11. Most validated clinical predictors of imminent death were based on subjective assessment and required experiences in palliative care (e.g., death rattle, inability to close eyelids, and terminal delirium)12,13,14,15. Although some studies demonstrated the correlation between objective parameters and short-term death (e.g., lower systolic blood pressure, decreased lymphocyte percentage, and elevated blood urea nitrogen level)16,17,18,19, they were studied in specific populations and outside the hectic setting of an ED20. Therefore, this study aimed to investigate relevant 7-day mortality prognostic factors in the ED and develop a user-friendly predictive score that could assist ED-based physicians in making decisions regarding the management and disposition of palliative patients.
Method
Study design and setting (source of data)
Between June 2022 and May 2023, we conducted a retrospective single-center observational study of 574 palliative patients at the 42,000-visit-annually-sized ED of a tertiary-level university hospital in Thailand. In our ED, the patient’s goal of care and their perception regarding life-sustaining treatments will be determined after initial evaluation by emergency physicians. After patients or their families decide to decline life-sustaining treatments, they sign a consent document. After emergency physicians consult the palliative care team, they offer patients consulting services to manage their symptoms, as well as personalized psychosocial and spiritual aspects. They also operate the 6-bed palliative care and hospice ward called “Ramathibodi Palliative Care Unit (RPU).” Concerning the limited availability of the ward, we aim to admit patients during the last seven days of their life.
Participants
The study included all adult patients aged 18 years or older who visited the ED throughout the study period and signed the consent document to decline life-sustaining treatments, including cardiopulmonary resuscitation (CPR), endotracheal intubation, mechanical ventilation, and hemodialysis21. The patients who subsequently underwent life-sustaining treatments, those who were dead upon arrival or within ten minutes of triage, those who were pregnant, and trauma patients were all excluded.
Ethics
Ethical approval for this study was obtained from the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University, granted on Jan 3, 2024 (IRB COA. MURA2024/4). The Institutional Review Boards in Mahidol University is in full compliance with the International Guidelines for Human Research Protection, including the Declaration of Helsinki, The Belmont Report, CIOMS Guidelines, and the International Conference on Harmonization in Good Clinical Practice (ICH-GCP). All personal identification was removed and replaced with study IDs. Given the study’s retrospective nature, the requirement for obtaining informed consent from individual patients was waived and approved by the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University.
Data collection (predictors and outcome)
Based on a literature review of previously published studies, clinical variables and biological markers of imminent death were thoroughly chosen as potential predictors for 7-day mortality4,12,13,14,15,16,17,18,19,20,22,23,24,25,26,27. All parameters were manually retrieved from the Ramathibodi Electronic Medical Record (RAMA EMR). The demographic data encompassed age, sex, and nursing home residency. Information about the illness and the course of treatment included the patient’s past medical history (e.g., underlying diseases and the age combined-Charlson comorbidities index (CA-CCI)28), the ED length of stay (hours), Emergency Severity Index (ESI) triage categories29, arrival modes, palliative care services (e.g., palliative consultations during ED stays), ED therapies (e.g., oxygen support and opioid usage), ED disposition destination, and main attending specialties. Clinical and laboratory parameters, including vital signs, the level of consciousness, respiratory with mandibular movement (RMM), and lab results (e.g., lymphocyte (x109/L), platelet (x109/L), hemoglobin level (g/dL), serum albumin (g/L), blood urea nitrogen (mg/dL), and creatinine (mg/dL)) were all recorded in the nearest time after the patients gave the agreement to decline life-sustaining treatments. RMM is an objective clinical sign characterized by an abnormal respiratory pattern accompanied by periodic mandibular jaw movements13,23,30, routinely recorded in the ED. The main outcome is the mortality within seven days after a patient’s permission to decline life-sustaining treatments. Mortality outcomes were determined using the RAMA EMR, cross-referencing with the national mortality database to ensure consistency and accuracy of death events. For non-admitted patients, outcomes were linked to the national database, while for admitted patients, they were documented in both the RAMA EMR and the national database. Survival durations were recorded in days.
Sample size estimation
The sample size of this study was calculated based on statistical data from the study on palliative care needs of advanced cancer patients in the ED at the end of life: an observational cohort study by Verhoef et al.31 The calculation was based on the variable main symptom at the ED: Dyspnea (Hazard ratio 1.48). The researchers used STATA version 17.0 and applied Two-sample comparisons of the survivor function, Log-rank test, and Freedman method using the following assumptions: Alpha = 0.05 (two sides), Power = 0.8, and N2/N1 = 0.30 (1:3.3 of the case: control). A total sample size of 238 people, divided into a group that survived after 7 days (N1) 183 people and a group that died within 7 days (N2) 55 people (N2/N1 = 0.301).
Missing data
In our study, 16 observations (3.21%) of some laboratory test results were missing because patients or their families refused blood testing. The missing data were classified as missing not at random (MNAR). We employed complete case analysis in multivariable logistic regression analysis, which involves including only cases with complete data for all variables in the analysis. While this approach ensures simplicity in handling missing data, it may introduce bias if the excluded cases differ systematically from those with complete data, particularly given the non-random nature of the missingness. Thus, potential limitations related to this method should be considered when interpreting the results.
Statistical analysis methods
All analyses were performed using STATA 17.0 software (StataCorp LLC, College Station, TX, USA). Subdivided by the outcome, all eligible patients were categorized into two groups: the study group (patients who died within seven days since the consent to decline life-sustaining treatments) and the control group (patients who survived after seven days). Categorical data are presented as frequency and percentage. The means (standard deviation, SD) and median (interquartile range, IQR) are used to report normally distributed or non-normally distributed continuous data, respectively. The data distribution will be determined using a histogram and plot. To assess statistically significant differences, two-tailed with a p-value < 0.05, between the study group and the control group, the Fisher exact probability test was used for categorical variables, and an independent T-test was used for normal distributions. In the case of non-normal distributions, the Mann-Whitney U test and Wilcoxon rank-sum test were employed.
Multivariable logistic regression analysis with backward elimination was used to identify independent factors associated with the 7-day mortality of palliative patients in the ED. The prediction score was calculated by dividing the regression coefficients of each potential factor by the lowest coefficient and rounding the result. The Area under the ROC (AuROC) curve was used to illustrate the score’s predictive potential. Subsequently, based on this score, we categorized patients into two groups to determine a proper cut point for decision-making in the ED. This prediction model’s sensitivity, specificity, positive predictive value, negative predictive value, and positive likelihood ratio were computed to manifest the power of the test.
Results
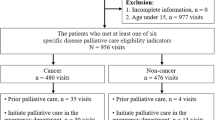
Regarding participants, among the 574 ED visits of palliative adult patients who consented to decline life-sustaining treatments, 64 patients eventually received life-sustaining treatments. This group included 35 patients who were intubated, 6 patients who underwent CPR, and 23 tracheostomy patients who required mechanical ventilation. Additionally, 8 patients presented with trauma-related injuries, and 3 patients died within 10 min of arrival. After exclusion, 499 visits (86.93%) were eligible for our analysis. Of these visits, 152 patients (30.46%) died within seven days. The study flow was shown in the Supplementary (Fig. 1). The median survival time of individuals who died within seven days were 2.5 days (IQR 1–4), while those who survived were 51.5 days (IQR 21–155).
For model development, the univariable analysis of baseline characteristics, clinical parameters, laboratory parameters, and healthcare service measures are listed in Tables 1 and 2. The mean age of patients who died within seven days was less than those who survived, 72.65\(\:\pm\:\)15.33 years and 78.16\(\:\pm\:\)13.94 years, respectively (p<0.001). The sex, nursing home residents, and the combined age-Charlson comorbidity index (CA-CCI) were not statistically different between the two groups. Regarding the underlying diseases, individuals with solid malignancy (59.87% vs. 40.35%, p<0.001) and liver diseases (22.37% vs. 11.82%, p=0.004) significantly tended to die within seven days. On the contrary, patients with stroke (15.79% vs. 37.75%, p < 0.001) and those who were bedridden (50.66% vs. 65.71%, p = 0.002) were more likely to survive after seven days.
Regarding clinical parameters, RMM was significantly associated with 7-day mortality (23.03% vs. 2.88%, p < 0.001). The median survival time of patients with RMM was 19.75 hours (IQR 7.02–87.32, p < 0.001). A statistically significant correlation was also found between unresponsiveness (AVPU scale) and their death within seven days (13.16% vs. 3.75%, p < 0.001). Additionally, many vital signs were correlated with 7-day death, including lower systolic blood pressure (115.02\(\:\pm\:\)28.09 mmHg vs. 130.30\(\:\pm\:\)27.02 mmHg, p<0.001), increased respiratory rate (27.38\(\:\pm\:\)7.73 breaths per minute vs. 24.48\(\:\pm\:\)6.26 breaths per minute, p<0.001), and lower oxygen saturation (96.04\(\:\pm\:\)5.83% vs. 97.92\(\:\pm\:\)2.69% p < 0.001).
According to the laboratory parameters of patients who died within seven days, the neutrophil counts slightly increased; conversely, there were significant drops in the median lymphocyte counts (0.66 (0.32–0.97) x109/L vs. 0.92 (0.53–1.39) x109/L, p < 0.001) and platelet counts (189 (102–308) x109/L vs. 234.5 (170–321.5) x109/L, p = 0.001). Both serum hemoglobin (9.59\(\:\pm\:\)2.24 g/dL vs. 10.43\(\:\pm\:\)2.44 g/dL, p<0.001) and serum albumin (23.55\(\:\pm\:\)6.20 g/L vs. 26.70\(\:\pm\:\)6.72 g/L, p<0.001) were also declined, while liver markers (aspartate transaminase and alanine transaminase) tended to increase. We also found that the elevated median blood urea nitrogen (BUN) and blood urea nitrogen to creatinine (BUN/Cr) ratio were also substantially associated with death within seven days (33 (21–54) mg/dL vs. 23 (15–43.5) mg/dL, p < 0.001) and (28.28 (20.78–40) vs. 23.20 (16.50–32.70), p < 0.001), respectively.
In terms of healthcare service measures, the median length of ED stays of those who died within seven days was 22.07 hours (IQR 6.77–52.83), which was significantly shorter than that of those who survived: 69.45 hours (IQR 31.92–116.8), p < 0.001. The ESI triage level 1 and death within seven days were also statistically associated (51.32% vs. 38.90%, p = 0.011). On the contrary, the mode of ED arrival, prior ED presentation, and prior admission in the previous six months showed no difference between groups. Regarding palliative care services, patients who died within seven days had a higher presence of pre-existing palliative-care consultations (48.03% vs. 31.12%, p < 0.001), as well as advanced care planning (44.08% vs. 25.94%, p < 0.001). During the ED stay, the palliative team provided the consultation service for 92.11% of those who died within seven days. In contrast, only 48.41% of surviving patients received palliative services (p < 0.001). In addition, a substantial portion of patients who died within seven days were prescribed intravenous opioids to relieve their symptoms, which was significantly higher than the control group (85.53% vs. 42.36%, p < 0.001). Emergency physicians also provided oxygen support for 92.11% of those who died within seven days (63.82% with low-flow oxygen therapies and 28.29% with positive-pressure ventilation). On the other hand, vasopressors were administered to only 6.58% and 3.46% of patients in the study group and the control group, consequently (p = 0.153). The patients who died within seven days were most frequently discharged to the RPU (40.79%), followed by home (25.66%) and ED death (23.03%). Accordingly, they were discharged from the ED by palliative care physicians (80.92%).
For multivariable logistic regression and prediction score analysis in model specification, Table 3 demonstrated the results to determine the predictors of 7-day mortality in ED palliative patients. The following parameters were included in the prediction scores: the presence of solid malignancy, RMM, systolic blood pressure (SBP) < 100 mmHg, lymphopenia (lymphocyte count < 1 × 109/L), thrombocytopenia (platelet count < 150 × 109/L), and elevated BUN/Cr ratio (BUN/Cr > 20). The mortality prediction score was named the “RAMA-EOL” score. The AuROC of the prognostic prediction score showed a predictive power of 80.46 (95% CI, 76.15–84.77) for 7-day mortality in model performance (Fig. 1). We categorized our score into two groups: the low-risk group (score < 3) and the high-risk group (score\(\:\ge\:\)3). Compared to those who survived after seven days (1.92\(\:\pm\:\)1.17), the mean score of patients who died in 7 days was substantially greater at 3.38\(\:\pm\:\)1.41, p<0.001. The predictive validity of the high-risk group was as follows (Table 4): 75.5% sensitivity, 74.1% specificity, 54.1% positive predictive value, 88.2% negative predictive value, and 2.92 positive likelihood ratio. The median survival time of those in the high-risk group was 6 days (2–27), which was significantly shorter than the low-risk group, 43 days (14–156), p<0.001. Additionally, the calibration of the prediction score is depicted, showing the observed risk and predicted risk in palliative patients (Fig. 2).
Discussion
The objective of this study was to explore predictive factors and formulate a predictive model that could anticipate the likelihood of 7-day mortality of palliative patients in the ED. The performance of the RAMA-EOL score showed an AuROC of 80.46, which represented a strong correlation of the six variables (presence of solid malignancy, RMM, SBP < 100 mmHg, lymphopenia (lymphocyte < 1 × 109/L), thrombocytopenia (platelet < 150 × 109/L), BUN/Cr ratio > 20) and the prediction of death within seven days. Compared to past literature, this study is distinctive in that we selected potential predictors based on the practical usage in the ED, which are non-subjective, easily accessible, and simple to use.
Regarding six predictive variables, two studies with mixed populations showed an association between the presence of malignancy and short-term mortality, while most previous research included only the cancer population4,24. Many previous studies also showed that RMM and other respiration abnormalities (e.g., apnea period) were highly specific for predicting imminent death, especially within 72 hours12,15,22. Additionally, our results aligned with the study by S. Bruera et al.16, manifesting a significant drop in systolic blood pressure, diastolic blood pressure, and oxygen saturation in the last three days of life. The study by S. Mercadante et al.17. also stated the correlation of SBP < 100 mmHg and 10-day mortality. Concerning biological markers associated with mortality, as demonstrated in previous studies, lymphopenia, low albumin levels, thrombocytopenia, and elevated BUN levels are also associated with short-term mortality in end-of-life patients18,19,24,26,27,32,33. Besides, a low percentage of lymphocytes is one of the scoring items in the Palliative Prognostic Score (PaP), a validated short-term mortality prediction score34,35.
The palliative team’s high engagement in patients’ end-of-life period was also demonstrated in this study. Patients who died within seven days tended to have preexisting advanced care planning and prior palliative care consultations. Furthermore, emergency physicians were more likely to consult the palliative team and offer palliative patients opioids for symptom management and oxygen support, as reported by Sweeny, A.L. et al.20and Monsomboon A. et al.4. This also implied that emergency physicians may be able to prognosticate a patient’s imminent death36. In addition, the ESI triage level 1 was also significantly associated with death, reflecting the quality of this triage tool in predicting the outcomes of the patients20.
Despite being irrelevant in other studies, younger patients tended to die within seven days in our studies because of the mixed population. The higher presence of malignancy is reported in the younger group, while the older group reported being associated with bedridden status and underlying stroke. Moreover, the lower death trend among bedridden and stroke patients reflected a higher percentage of declining life-sustaining treatments among these patients and indicated the uncertainty in the prediction of death by emergency physicians in this population.
The RAMA-EOL score has high sensitivity and specificity for predicting 7-day mortality. Regarding the results, even though more than half of the palliative patients who died within seven days were sent to the hospice ward or back to their homes per their request, 23% of the patients inappropriately died in the ED. Therefore, the RAMA-EOL score facilitates emergency physicians in making decisions regarding palliative consultations and precise ED disposition. Since most variables were objective and the signs of RMM were recorded as emergency physicians and nurses noticed, the RAMA-EOL score does not require specialization in palliative care. We proposed that if patients were classified into the high-risk group (score\(\:\ge\:\)3), they would have a higher likelihood of death within seven days, with a positive likelihood ratio of 2.92. Therefore, emergency physicians should promptly discuss the goal of care and the location of death with patients and their families and make a shared decision regarding emergency care for their quality of life.
Limitations
Firstly, due to its single-center design, the study’s generalizability to other populations or demographics may be limited. Thus, additional external validation of our predictive score using independently obtained patient data from different hospital systems is required to validate the model. Moreover, considering the retrospective study’s design, it is challenging to account for confounding variables and demonstrate a causal association between the discovered outcomes. Multi-center prospective research may be conducted to enhance generalizability and causal relationships.
Secondly, the selection bias of the study population is based on physicians’ awareness and recognition of the end-of-life period and palliative care requirement. The system for enrolling this study population has been established by the inclusion criterion of declining life-sustaining treatments and completing the consent document. Further studies with specific indications to identify EOL palliative-eligible patients would help diminish this bias.
Lastly, although most previous studies have primarily focused on a particular type of illness trajectory toward the end of life, our study included all populations with various trajectories. In fact, we believed that the variety of disease subgroups that visited the ED during the study period represented the actual difficulties that emergency physicians faced with the detection of imminent death in the last seven days.
Conclusion
The RAMA-EOL score predicts the 7-day mortality of the palliative patients in the ED. Since the high-risk group (score\(\:\ge\:\)3) has a higher likelihood of death within seven days, the shared decision regarding emergency care for the quality of life, including the preferred place of death, should be discussed for the goal of care. Moreover, this prediction score can be implemented effortlessly in the ED because no prior clinical palliative knowledge or experience is required. The clinical use of this score in the actual emergency setting still requires further study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RMM:
-
Respiratory with mandibular movement
- SBP:
-
Systolic blood pressure
- BUN/Cr:
-
Blood urea nitrogen/creatinine
References
Crawford, G. B. et al. Care of the adult cancer patient at the end of life: ESMO Clinical Practice guidelines. ESMO Open.6 (4), 100225 (2021).
Smith, R. A good death. An important aim for health services and for us all. Bmj 320 (7228), 129–130 (2000).
Elmer, J., Mikati, N., Arnold, R. M., Wallace, D. J. & Callaway, C. W. Death and end-of-Life Care in Emergency Departments in the US. JAMA Netw. Open. 5 (11), e2240399 (2022).
Monsomboon, A. et al. Characteristics and factors associated with mortality in palliative patients visiting the Emergency Department of a large tertiary hospital in Thailand. BMC Palliat. Care. 21 (1), 115 (2022).
Leung, K. K. et al. Can a good death and quality of life be achieved for patients with terminal cancer in a palliative care unit? J. Palliat. Med. 13 (12), 1433–1438 (2010).
Echteld, M. A., van Zuylen, L., Bannink, M., Witkamp, E. & Van der Rijt, C. C. Changes in and correlates of individual quality of life in advanced cancer patients admitted to an academic unit for palliative care. Palliat. Med. 21 (3), 199–205 (2007).
Bakitas, M. et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. Jama 302 (7), 741–749 (2009).
White, N., Reid, F., Harris, A., Harries, P. & Stone, P. A systematic review of predictions of Survival in Palliative Care: how accurate are clinicians and who are the experts? PLoS One. 11 (8), e0161407 (2016).
Glare, P. et al. A systematic review of physicians’ survival predictions in terminally ill cancer patients. Bmj 327 (7408), 195–198 (2003).
Hui, D. Prognostication of survival in patients with Advanced Cancer: Predicting the Unpredictable? Cancer Control. 22 (4), 489–497 (2015).
Christakis, N. A. & Lamont, E. B. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. Bmj 320 (7233), 469–472 (2000).
Hui, D. et al. Clinical signs of impending death in cancer patients. Oncologist 19 (6), 681–687 (2014).
Ijaopo, E. O., Zaw, K. M., Ijaopo, R. O. & Khawand-Azoulai, M. A review of clinical signs and symptoms of imminent end-of-life in individuals with Advanced Illness. Gerontol. Geriatric Med. 9, 23337214231183243 (2023).
Stone, P. et al. Prognostic evaluation in patients with advanced cancer in the last months of life: ESMO Clinical Practice Guideline. ESMO Open. 8 (2), 101195 (2023).
Hui, D. et al. Bedside clinical signs associated with impending death in patients with advanced cancer: preliminary findings of a prospective, longitudinal cohort study. Cancer 121 (6), 960–967 (2015).
Bruera, S. et al. Variations in vital signs in the last days of life in patients with advanced cancer. J. Pain Symptom Manage. 48 (4), 510–517 (2014).
Mercadante, S. et al. Prognostic factors of survival in patients with advanced cancer admitted to home care. J. Pain Symptom Manage. 45 (1), 56–62 (2013).
Kikuchi, N. et al. Survival prediction of patients with advanced cancer: the predictive accuracy of the model based on biological markers. J. Pain Symptom Manage. 34 (6), 600–606 (2007).
Chen, Y. T. et al. Objective palliative prognostic score among patients with advanced cancer. J. Pain Symptom Manage. 49 (4), 690–696 (2015).
Sweeny, A. L. et al. End-of-life care: a retrospective cohort study of older people who died within 48 hours of presentation to the emergency department. Emerg. Med. Australas 36(1), 13–23 (2024).
Salins, N. et al. Definition of terms used in limitation of treatment and providing Palliative Care at the end of life: the Indian Council of Medical Research Commission Report. Indian J. Crit. Care Med. 22 (4), 249–262 (2018).
Hosoi, T., Ozone, S., Hamano, J., Maruo, K. & Maeno, T. Prediction models for Impending Death using physical signs and Vital Signs in Noncancer patients: a prospective longitudinal observational study. Palliat. Med. Rep. 2 (1), 287–295 (2021).
Matsunami, K. et al. Physical signs and clinical findings before death in Ill Elderly patients. Am. J. Hosp. Palliat. Care. 35 (4), 712–717 (2018).
Christ, S. M. et al. Prevalence and predictors for 72-h mortality after transfer to acute palliative care unit. Support Care Cancer. 30 (8), 6623–6631 (2022).
Huang, Y. L., Alsaba, N., Brookes, G. & Crilly, J. Review article: end-of-life care for older people in the emergency department: a scoping review. Emerg. Med. Australas. 32 (1), 7–19 (2020).
Viganó, A. et al. Clinical survival predictors in patients with advanced cancer. Arch. Intern. Med. 160 (6), 861–868 (2000).
Maltoni, M. et al. Prognostic factors in advanced cancer patients: evidence-based clinical recommendations–a study by the Steering Committee of the European Association for Palliative Care. J. Clin. Oncol. 23 (25), 6240–6248 (2005).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40 (5), 373–383 (1987).
Gilboy, N. T. P., Travers, D. A., Rosenau, A. M. & Eitel, D. R. Emergency Severity Index, Version 4: Implementation Handbook (AHRQ Publication, 2005).
Kaneishi, K. et al. Epidemiology of respiration with Mandibular Movement in Advanced Cancer patients: a Multicenter prospective cohort study. J. Palliat. Med. 25 (3), 461–464 (2022).
Verhoef, M. J. et al. Palliative care needs of advanced cancer patients in the emergency department at the end of life: an observational cohort study. Support Care Cancer. 28 (3), 1097–1107 (2020).
Chiang, J. K., Cheng, Y. H., Koo, M., Kao, Y. H. & Chen, C. Y. A computer-assisted model for predicting probability of dying within 7 days of hospice admission in patients with terminal cancer. Jpn J. Clin. Oncol. 40 (5), 449–455 (2010).
Chiang, J. K., Lai, N. S., Wang, M. H., Chen, S. C. & Kao, Y. H. A proposed prognostic 7-day survival formula for patients with terminal cancer. BMC Public. Health. 9, 365 (2009).
Pirovano, M. et al. A new palliative prognostic score: a first step for the staging of terminally ill cancer patients. Italian Multicenter and Study Group on Palliative Care. J. Pain Symptom Manage. 17 (4), 231–239 (1999).
Scarpi, E., Nanni, O. & Maltoni, M. Development and validation of the PaP score Nomogram for terminally Ill Cancer patients. Cancers (Basel) 14 (10), 2510 (2022).
Stone, P. C. et al. The accuracy of clinician predictions of survival in the prognosis in palliative care study II (PiPS2): a prospective observational study. PLoS One. 17 (4), e0267050 (2022).
Author information
Authors and Affiliations
Contributions
TC and WT wrote the main manuscript, and we followed the TRIPOD Checklist for prediction model development research. TC and WT initiated the research question and completed the IRB submission. TC performed data collection and data analysis, made tables and figures, and wrote background, results, discussion, and limitations sections. WT performed data analysis, edited tables and figures, reviewed data, and addressed the corresponding author. CY and TP are associated professors and research advisors at Mahidol University, who provided revisions and guidance to the manuscript. CB and NP are physicians with expertise in family medicine and palliative care, who guided the manuscript discussion, and provided expert opinions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Ethical approval for this study was obtained from the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University, granted on Jan 3, 2024 (IRB COA. MURA2024/4). The Institutional Review Boards in Mahidol University is in full compliance with the International Guidelines for Human Research Protection including the Declaration of Helsinki, The Belmont Report, CIOMS Guidelines, and the International Conference on Harmonization in Good Clinical Practice (ICH-GCP). All personal identification was removed and replaced with study IDs. Given the study’s retrospective nature, the requirement for obtaining informed consent from individual patients was waived and approved by the Human Research Ethics Committee, Faculty of Medicine Ramathibodi Hospital, Mahidol University.
Using artificial intelligence chatbots
During the preparation of this work, the author (s) used Chat GPT 4.0 and Grammarly to check and correct grammatical errors during the manuscript writing process. After using this tool/service, the author (s) reviewed and edited the content as needed and take (s) full responsibility for the content publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Charascharungkiat, T., Tienpratarn, W., Yuksen, C. et al. Prognostic factors and development of the practical prediction score for 7-day mortality of palliative patients in the emergency department. Sci Rep 15, 6628 (2025). https://doi.org/10.1038/s41598-025-90593-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90593-0