Abstract
Sleep irregularity has been linked to multiple deleterious consequences in clinical populations or community adults and adolescents, but little is known about young adults. In this study, we explored the relationships between two measures of sleep regularity and a wide range of factors (lifestyle behaviors, subjective sleep, clinical outcomes, and academic performance) in a sample of female, university students in the United Arab Emirates. A total of 176 participants were recruited. Objective estimates of sleep–wake patterns were obtained using seven-day wrist actigraphy and data were used to calculate daily sleep regularity with the Sleep Regularity Index (SRI) and weekly sleep regularity with the social jetlag (SJL). Subjective sleep measures were also acquired using the Pittsburgh Sleep Quality Index (PSQI), Dysfunctional Beliefs and Attitudes about Sleep (DBAS), and daytime napping frequency. Self-reported night-time technology use frequency was ascertained using the Technology Use Questionnaire (TUQ). Psychological health was assessed using the Hospital Anxiety and Depression Scale. Objective physical health measurements for body mass index, fasting blood glucose and blood pressure were obtained. No significant associations emerged between sleep regularity and psychological physical health, or academic performance. However, significant relationships were detected between SRI and daytime napping frequency (p-value = 0.0017), PSQI (p-value = 0.0337), and DBAS (p-value = 0.0176), suggesting that daily irregular sleep patterns are associated with more frequent daytime napping, greater dysfunctional sleep beliefs, and poorer subjective sleep quality. Conversely, SJL was significantly associated with the DBAS (p-value = 0.0253), and the TUQ (p-value = 0.0208), indicating that weekly irregular sleep patterns are linked to greater dysfunctional sleep beliefs and increased nighttime technology use. In conclusion, efforts to educate and cultivate sustainable and consistent sleep–wake patterns amongst university students are needed, which can be achieved by raising awareness, promoting good sleep health habits, and minimizing excessive bedtime technology.
Similar content being viewed by others
Introduction
Preserved sleep–wake homeostasis is a central precept for optimal health, performance, and wellbeing. Whilst much effort has been made to understand the adverse consequences of sleep deprivation and poor sleep quality, sleep extends far beyond these two measures. Sleep is a multi-dimensional construct as well as a fluctuating behavior. Recent studies have explored links between intra-individual sleep irregularity and a range of outcomes including inflammation1, psychological health2,3,4, cognition4,5, performance6,7, obesity8,9, metabolic health10,11,12,13, brain function14, fatigue15, cardiac autonomic modulation16 as well as mortality17. This preliminary, yet extensive evidence-based suggests that irregular sleep–wake behaviors may result in multiple deleterious consequences, although most of these findings focused on clinical populations, adults, or adolescents. Despite the Sleep Regularity Index (SRI) being first applied to a small sample of undergraduate students6 very little is known about young, emerging adults, particularly in Middle Eastern populations. Moreover, whilst recent evidence has revealed gender differences in nocturnal sleep patterns and sleep variability across the lifespan18, little effort has been made to investigate daily/weekly sleep regularity in young, adult females and non-Western populations. Given its collectivist culture, this population is important to target, as sociocultural differences will likely influence sleep habits.
Evidence surrounding sleep irregularity and attendant outcomes has been investigated across different age groups and populations. Nevertheless young, emerging adults are likely to be at a higher risk of engaging in more variable sleep–wake patterns. For example, ample evidence suggests poor sleep habits are common among university students19,20. In addition, poor sleep hygiene practices may be particularly propelled by dysfunctional sleep beliefs and foster markedly irregular sleep patterns20. This implies that university students may not prioritize sleep health, thereby resulting in more sleep–wake variability with possible downstream consequences, as shown by Phillips et al.6. Furthermore, social jetlag (SJL), a biological-social clock discrepancy21,22, is another common sleep irregularity phenomenon that has been previously linked to several undesirable consequences21,22,23,24,25,26,27.
Gender and ethnic differences have also been detected in sleep amongst a large US national sample28. Similarly, another recent study revealed age and gender differences using objective estimates of sleep in Japanese adults29. The authors concluded that their observations, which included women having poorer and shorter sleep duration than men, were likely driven by socio-cultural and socio-familial factors29. This warrants further investigation in other non-Western populations, focusing on women’s sleep.
The determinants of sleep irregularity, such as fluctuations to sleep–wake timings, are currently unknown, although recent efforts have been made to identify the possible underlying physiological mechanisms30. A combination of internal (beliefs, cognition) and external factors (screen time exposure, lifestyle behaviors, social activities) are, however, likely to play a role in irregular sleep–wake behaviors. We hypothesized that sleep irregularity would be associated with negative or impairment in clinical, lifestyle, and performance-related outcomes. Accordingly, we aimed to comprehensively examine the potential relationships between sleep regularity and a range of different factors (lifestyle behaviors, clinical outcomes, sleep beliefs, and academic performance) in a sample of female, university students in the United Arab Emirates (UAE), a country where little is known about sleep habits. To achieve this goal, we obtained sleep–wake patterns using seven-day wrist actigraphy and subsequently calculated the SRI and SJL for each participant. The SRI quantifies the daily consistency in sleep/wake patterns, thus accounting for variations in daily sleep regularity arising from fragmented sleep, daytime napping, and variable sleep onset and offset sleep timing6,17,31,32. Conversely, SJL quantifies the difference in average sleep timing between workdays and free days, thus accounting for weekly rather than daily sleep regularity21,22,23,31.
Methods
Participants and settings
Zayed University has one campus in Abu Dhabi with two sections, segregated according to gender. Most registered students are female, and therefore all participants were recruited from the female campus at Zayed University between September 2017 and March 2020. The percentages of data collected during the hot season (summer, April–October) and the warm season (winter, November–March) in the UAE are 61.6% and 38.4%, respectively. Inclusion criteria for study participation was: (1) registered student at Zayed University; (2) female; (3) aged 18–50 years; (4) able to provide written informed consent; (5) fluent in English language. Individuals were excluded from participation if they: (1) were taking prescribed sleep medication at the time of study participation; (2) had a physician-diagnosed psychiatric condition(s); (3) had a physician-diagnosed sleep disorder(s); and/or (4) were pregnant.
Measurements
Wrist actigraphy
Participants were asked to wear wrist actigraphy (GT3X + BT; The ActiGraph, Pensacola, FL, USA) on their non-dominant wrist for seven consecutive days and nights. Participants were also asked to complete a seven-day sleep diary concurrent with the days/nights during which they wore the actigraph. When the sleep diary and actigraph were returned, the device data were downloaded and auto-scored using ActiLife software, based on Cole-Kripke algorithms33. Discrepancies between the actigraphy data and sleep diaries were resolved with each participant, and data from all sleep–wake timings and daytime naps were adjusted during the participant’s second study visit. For each sleep period of each participant, the following variables were derived from the adjusted actigraphy data: in bed date and time, out of bed date and time, onset date and time, sleep onset latency (SOL), total sleep time (TST), number of awakenings (Nawakening), and wake after sleep onset (WASO). A small number of devices malfunctioned or had battery loss and therefore collected data for less than seven days. In this regard, participants with ≥ 30 h of actigraphy data missing, as well as subjects with less than five days of actigraphy data were excluded from subsequent analyses.
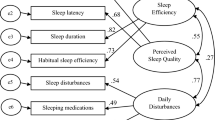
Subjective sleep quality
Sleep quality was assessed using the 19-item self-reported scale, Pittsburgh Sleep Quality Index (PSQI)34. The scale asks participants to estimate various sleep behaviors in the previous one-month period. It contains seven sub-components and items pertaining to each component are added to derive a global PSQI score ranging 0–21 where higher scores represent poorer overall sleep quality. The PSQI has previously demonstrated good internal consistency and sensitivity34.
Sleep beliefs
The Dysfunctional Beliefs and Attitudes about Sleep (DBAS) scale was employed to assess sleep beliefs. Participants were asked to rate each of the 16 statements using a Likert scale where 0 = strongly disagree and 10 = strongly agree. The total score was derived by summing responses then dividing by 16 to calculate the mean total score. Higher scores represent greater dysfunctional sleep beliefs. The DBAS has good internal consistency35 and good test–retest reliability.
Lifestyle behaviors and academic performance
All lifestyle factors were subjectively estimated. Daytime napping was assessed by asking the question “Do you usually nap during the day?” with response options of “yes” or “no”. Those who answered ‘yes’ were then further asked to estimate nap frequency with the following options: “ < 1 per week”, “1–3 per week”, “4–6 per week” or “daily”. These questions and response options were based on the Guangzhou Biobank Cohort Study36. Participants were also asked if they engaged in regular exercise (yes/no) and those who answered ‘yes’ were asked to self-report their weekly frequency using the same response options as daytime napping frequency (“ < 1 per week”, “1–3 per week”, “4–6 per week” or “daily”). Self-rated health status and dietary habits were assessed with response options of ‘very good’, ‘good’, ‘poor’, or ‘very poor’. The self-rated health question and response options were also based on the Guangzhou Biobank Cohort Study36. Participants cumulative grade point average (CGPA) was obtained at the time of study participation from the Zayed University database to determine objective academic performance.
The Technology Use Questionnaire (TUQ), previously developed for a cohort study37, was used to determine frequency of night-time electronic device use. Participants were asked about their use of different technologies (mobile telephone, video gaming, laptop/computer for studying, social media, tablets for reading, television) in the two hours before they went to bed at night and/or whilst in bed. Response options were “never = 0”; “sometimes = 1”; “usually = 2”; “always = 3”. Responses were summed to derive a total score (0–21) where higher scores represented greater night-time technology use. The TUQ has been previously validated against seven-day technology use diary information in a large sample of adolescents38.
Mental health & clinical measurements
Mental health was assessed using the Hospital Anxiety Depression Scale (HADS) which is a 14-item instrument used to determine symptoms and severity of anxiety and depression. The tool contains seven items pertaining to anxiety and the remaining seven to depression. Responses to each item are totaled for each of the two conditions and higher scores indicate greater symptom severity. The HADS has been extensively assessed for validity and reliability and has demonstrated good psychometric properties39.
Participants were asked to remove their shoes and height (cm) was measured using a portable Seca 213 stadiometer which was regularly calibrated. Body weight (kg) was assessed in light indoor clothing using a calibrated body weighing scale. Height and weight records were subsequently used to calculate body mass index (BMI) using the standard equation (kg/m2). Blood pressure (BP) was measured using a portable Omron M2 monitor. BP was taken after the participant had been seated and at rest for approximately 15 min after completing the questionnaires. Participants were instructed to be silent during the reading and to have both feet placed flat on the floor. Diastolic and systolic BP were recorded for each participant. Fasting blood glucose (FBG) was taken after an overnight fast using a portable monitoring system with compatible testing strips (Accu-Chek Instant).
Procedure
This work has been carried out according to the Declaration of Helsinki. Ethical approval for the study was granted by the Research Ethics Committee at Zayed University (ZU17_037_F). Summary details of the study were placed around the campus in poster format to recruit participants, as well as communicated through word-of-mouth approaches. Interested students contacted the Principal Investigator (TA) and were sent detailed information about the study and participation requirements. Those who expressed an interest in taking part in the study were asked to attend the first study visit at a mutually convenient time and date. During the first visit, participants arrived fasted from the night before. Participants provided written informed consent and then completed a series of researcher-led questionnaires in English as well as several, objective clinical measurements. English versions of all questionnaires were used as all courses at Zayed University are taught in English and students must obtain a relatively high standard of English proficiency for entrance to all majors. Moreover, our inclusion criteria also required participants to be fluent in English. Participants were then administered with wrist actigraphy and requested to wear it for seven consecutive days and nights. The researcher explained how to complete the seven-day sleep diary which they were instructed to complete alongside wearing the actigraph. An appointment was made for study visit two which was completed seven days after study visit one. At visit two, participants returned the wrist actigraphy and sleep diary and discrepancies between these two sleep measures were resolved with the researcher. Participants were debriefed at the end of visit two, and a copy of their actigraphy report was provided to them. Participants did not receive any financial incentive for participation, but they did receive one-hour of volunteer services to log in their student profile.
Sleep regularity index (SRI)
For each participant and based on all the reported periods of actigraphy-scored sleep, a binary sleep–wake signal was first obtained (see section 1 of the Supplementary Material). Based on the sleep/wake signal, the SRI measures the similarity of an individual’s sleep–wake patterns across consecutive days. Specifically, SRI calculates the percentage probability of an individual remaining in the same state (i.e., either sleep or wake) at any two time points (in our case, 1-min epochs) separated by 24 h. This percentage is then averaged over the given period. In this study, the SRI was computed using the following equation6:
where L is the total number of 1-min epochs, M is the number of 1-min epochs per day, and \(\delta ({s}_{i},{s}_{i+M}\)) is equal to one, when the sleep–wake signal is the same 24 h apart (\({s}_{i}= {s}_{i+M}\)), otherwise zero. The metric is defined in a manner that allows for a fair comparison between individuals who exhibit the same standard deviation in midsleep time but differ in their overall sleep durations (e.g., 4 h vs. 8 h). Consequently, these individuals will yield approximately equivalent SRI scores. An SRI value of 100 signifies that the sleep–wake patterns remain identical across consecutive days, while an SRI score of 0 indicates a complete absence of overlap between consecutive sleep–wake periods. Accordingly, participants were classified as regular (n = 53), normal (n = 52), or irregular (n = 53) sleepers if they were in the upper (SRI ≥ 72.1), middle (61.0 ≤ SRI < 72.1), or lower (SRI < 61.0) tertile based on their SRI score, respectively. This stratification allows us to discern distinct patterns of daily sleep regularity among the study participants, facilitating a comprehensive analysis of the data.
Social jetlag (SJL)
As actigraphy records contain both nighttime and daytime (i.e., naps) sleep periods, and considering that SJL measures the mismatch in average nighttime midsleep timing between workdays and free days, we have first obtained a nighttime sleep period for each day of recording of each participant (see section 2 of the Supplementary Material). For each participant and based on these nighttime sleep periods, SJL is extracted as the difference between midsleep time on free days (MSF) and midsleep time on workdays (MSW)21,31:
where MSF and MSW represent the midpoint between the onset time and offset time of each nighttime sleep period on free days and workdays, respectively. At the time of data collection, class days in the Zayed University of the UAE were on Sunday, Monday, Wednesday, and Thursday, so we considered evenings of Saturday, Sunday, Tuesday, and Wednesday as workdays and evenings of Monday, Thursday, and Friday as free days. An SJL value closer to zero indicates a more regular weekly sleep pattern. As with SRI, participants were also classified as regular (n = 53), normal (n = 52), or irregular (n = 53) sleepers if they were in the lower (SJL < 1.00), middle (1.00 ≤ SJL < 2.09), or upper (SJL ≥ 2.09) tertile based on their SJL score, respectively.
Study size
To calculate the minimum sample size needed to assess the association between sleep regularity measures and continuous outcome variables (i.e., lifestyle behaviors, clinical outcomes, sleep beliefs, and academic performance), as well as to assess the differences between sleep regularity measures and categorical outcome variables (i.e., self-rated health, self-reported diet, self-reported nap and nap frequency, and self-reported exercise and exercise frequency), independent statistical analyses were performed. We considered: (i) the probability of Type I error (i.e., α) should be 0.05; (ii) the power of the test (i.e., 1-β) should be 0.95; and (iii) the effect size should be of 0.3 (i.e., medium effects). With this information, it has been estimated that the total sample size should be 128 or large. Thus, the available data in this study (n = 158) provides enough statistical power. For replicability, these analyses were performed using the G*Power 3.1.9.7 software.
Statistical analysis
Continuous demographic and actigraphy data were presented as mean ± standard deviation (SD) and compared among sleep irregularity groups using analysis of variance (ANOVA). To assess the differences between sleep regularity measures and categorical outcome variables (self-rated health, self-reported diet, self-reported nap and nap frequency, and self-reported exercise and exercise frequency), we used the analysis of covariance (ANCOVA) controlling for the following covariates: age, BMI, season of the year in which the actigraphy recording was collected, number of recording days (Nrec), number of free and workdays in the recording, per-subject TST, per-subject Nawakening, per-subject SOL, and per-subject WASO. These covariates were used to ensure that the statistically significant differences are due to the SJL and/or SRI rather than to demographics or other actigraphy measures. Based on all the reported sleep periods, the total per-subject values for TST, WASO, SOL, and Nawakening were calculated by summing the respective values across all sleep periods. These total values were then normalized by dividing each per-subject TST, WASO, SOL, and Nawakening by the total duration in days (Nrec) of the actigraphy data.
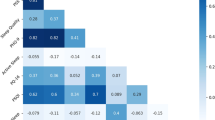
In addition to analyses among groups, we utilized Pearson’s linear and partial correlations (adjusted for the same covariates) to assess the relationship between continuous outcome variables (PSQI, DBAS, TUQ, CGPA, HADS scores, diastolic and systolic BP, and FBG) and sleep regularity measures (SJL and SRI). The same covariates used in the ANCOVA were included in the partial correlation analysis to ensure that the statistically significant associations are due to the SJL and/or SRI rather than to demographics or other actigraphy measures. Based on observed non-normality in variable distributions, BMI, TST, WASO, Nawakening, and SRI were transformed using Box-Cox method to perform associations40. The data were analyzed using our own codes and base functions in Python 3.8.8 (the Python Software Foundation, Wilmington, DE, USA). In all analyses, p-value < 0.05 was considered significant.
Results
Participants and actigraphy measures
A total of 176 female undergraduate university students were recruited to the study. Of these participants, 18 were excluded due to one of the following reasons: (i) two participants had missing actigraphy data; (ii) ten participants had ≥ 30 h elapsed between consecutive sleep periods; (iii) six participants had less than five days of actigraphy data17. Table 1 shows the patient demographics and actigraphy-derived parameters of the 158 participants. Although our inclusion age range was 18–50 years, the vast majority of our sample were aged 18–25 years (n = 152 (96.2%)). This table also shows a comparison of subject characteristics among regular, normal, and irregular SJL- and SRI-derived groups. No statistically significant differences were found in either age, BMI, TST, WASO, SOL, or Nawakening across the SJL- and SRI-derived sub-groups.
Daily sleep regularity: sleep regularity index
Table 2 presents the results of the partial correlation analysis, showing the association between SRI and continuous outcome variables (lifestyle behaviors, clinical outcomes, sleep beliefs, and academic performance), controlling for demographic and actigraphy covariates. Of note, SRI was significantly associated with the global PSQI score (ρ = − 0.1747, p-value = 0.0337) and the DBAS total score (ρ = − 0.1989, p-value = 0.0176). The scatterplots displayed in Fig. 1 also demonstrate lower SRI values observed with increased global PSQI and total DBAS scores. Conversely, there were no statistically significant correlations between SRI and other variables assessed (all p-values > 0.05). For the sake of completeness of the analysis, supplementary material also includes a replication of the proposed methodology using an additional sleep regularity measure, known as interdaily stability (IS, section 3), an assessment of the influence of WASO and the Nawakening in the SRI (SRIWASO-Nawak, section 4). Interestingly, IS (see Supplemental Table 2) and SRIWASO-Nawak (see Supplemental Table 5) were also only significantly associated with PSQI and DBAS scores and were not significantly correlated with other continuous variables.
Table 3 shows the comparisons of SRI measurements among groups of categorical variables derived from questionnaires, controlling for clinical covariates. Patients with self-reported naps had a significantly lower SRI (p-value < 0.001). From those patients, significantly lower values were obtained in SRI as the number of self-reported naps increased (p-value = 0.0017). These tendencies can be also observed in the boxplots displayed in Fig. 2. Conversely, there were no differences in SRI among groups of the remaining categorical variables. Supplemental Table 3 and Supplemental Table 6 show the ANCOVA analysis for IS and SRIWASO-Nawak, respectively. As in the case of SRI, significantly lower values were obtained in IS and SRIWASO-Nawak in patients with self-reported nap as well as when the number of self-reported naps increased. IS was also significantly associated with exercise (p-value = 0.0393), whereas SRI association with exercise showed a p-value in the 0.05–0.10 range. Conversely, there were no differences in IS and SRIWASO-Nawak among groups of the remaining categorical variables.
Weekly sleep regularity: social jetlag
Table 4 presents the results of the partial correlation analysis, showing the association between SJL and continuous outcome variables (lifestyle behaviors, clinical outcomes, sleep beliefs, and academic performance), controlling for demographic and actigraphy covariates. Similarly, Table 5 shows the comparisons of SJL measurements among groups of categorical variables derived from questionnaires, controlling for clinical covariates. Of note, SJL was significantly associated with the global DBAS (ρ = − 0.1877, p-value = 0.0253) and the TUQ total (ρ = − 0.1898, p-value = 0.0208) scores, whose scatter plots are displayed in Fig. 3. Conversely, there were no statistically significant correlations between SJL and other variables assessed (all p-values > 0.05). For the sake of completeness of the analysis, supplementary material also includes an assessment of the influence of earlier sleep midpoint on weekends in the SJL (SJLADMW, section 5). As in the case of SJL, SJLADMW (see Supplemental Table 8 and Supplemental Table 9) were also significantly associated with DBAS. Conversely, it was not significantly associated with TUQ and the remaining outcomes variables, which supports the use of SJL.
Discussion
The present study is the first to comprehensively examine a range of factors in relation to two sleep regularity measures in young female university students in a country where very little is known about sleep behaviors. Our findings revealed significant negative linear relationships between the SRI and subjective sleep quality (PSQI) and sleep beliefs (DBAS), as well as significant positive correlations between the SJL and night-time technology (TUQ). Moreover, we observed that those who reported daytime napping had more daily irregular sleep (i.e., lower SRI), and more frequent daytime napping was associated with greater daily sleep irregularity. We did not detect any significant relationships with other variables assessed such as clinical outcomes (fasting blood glucose, blood pressure), mental health, other lifestyle behaviors (diet, self-rated health, exercise), or academic performance.
Contemporary society offers demands and distractions that compete for attention during wakefulness. These may, unintentionally, result in extended wakefulness and sleep hinderance, thus creating a sleep–wake imbalance and greater irregularity. Availability and accessibility of technology is abundant and recent evidence has suggested a possible causal relationship between evening social media use and delayed sleep onset (time taken to initiate sleep)41. Similarly, a high frequency of binge TV viewers exhibit poorer sleep quality, as well as other adverse consequences42. Moreover, frequent use of electronic devices at night-time has been associated with poor sleep quality, increased sleep onset latency and excessive daytime sleepiness43. Whilst sleep quality, and several indicators of this sleep feature, are clearly affected by night-time technology use, nothing is currently known about the potential relationship between sleep irregularity and electronic device use at night-time amongst university students.
Our study findings revealed a linear relationship, suggesting that more frequent night-time technology use was significantly associated with SJL but not the SRI. Whilst we cannot draw causal inferences from our observation, there are at least three possible explanations. First, irregular sleep–wake behavior is likely to disrupt natural sleep cycle rhythms, potentially exacerbating daytime sleepiness. Subsequent daytime napping behavior may ensue with later consequential bedtimes particularly on weekends, as shown by our findings and others. This, in turn, could leave individuals with more opportunities to use technology given accessibility is 24 h a day for most. Notably, we found more daily irregular sleep amongst those who napped versus those who did not. Moreover, a dose-dependent relationship was found with napping frequency and daily sleep regularity with those reporting more frequent napping having higher levels of daily sleep irregularity, thus providing further support for this explanation. Second, frequent night-time technology use may contribute to irregular sleep habits. There is some evidence to suggest that individuals encounter distorted time perception and lose track of time when engaging with technology44. In turn, this may result in delayed sleep onset and/or alterations to sleep–wake timings and, therefore, greater sleep irregularity, particularly at the weekends. Another study found that individuals who had a higher frequency of binge TV viewing also had poorer sleep quality, an observation which was mediated by cognitive pre-sleep arousal42. This could, however, vary depending on the type of technology and activity the user is engaged with. We did not acquire this level of detail in our study and therefore suggest that future research sets out to comprehensively investigate this issue, as well as complete longitudinal assessments to determine potential cause-effect associations. Third, participants had later bedtimes on weekends than weekdays which contributes to social jetlag. A recent study showed that teenagers engage more in bedtime technology on free nights versus school nights, which predicts later sleep timings45. Another study revealed that bedtime technology users had a later sleep midpoint at weekends than those who did not use technology46. These studies are relevant to our findings given that night-time technology use was significantly associated with SJL (weekday versus weekend sleep regularity) but not the SRI (daily sleep regularity).
Our previous work has shown that poor subjective sleep quality is high amongst university students in the UAE47. This high level of poor subjective sleep quality is similar to that reported amongst university students in other Gulf states. Interestingly, one predictor of poor sleep quality in this study was the use of pre-bedtime technology48. Poor sleep quality could also be a cause or consequence of irregular sleep patterns as well as dysfunctional sleep beliefs. We observed a significant linear relationship between both SRI and SJL and the DBAS, suggesting that greater dysfunctional sleep beliefs were related to greater sleep irregularity. Although our study does not determine temporal associations, it is possible that dysfunctional sleep beliefs may contribute to irregular sleep–wake behaviors. For example, individuals with inflexible sleep beliefs about sleep need may result in heightened pre-sleep cognitive arousal states which may subsequently delay sleep initiation49, possibly resulting in irregular sleep patterns. Second, irregular sleep may underpin dysfunctional beliefs. For example, those with irregular sleep habits may adopt negative beliefs about sleep self-efficacy. To our knowledge, this is the first study to assess the relationship between dysfunctional sleep beliefs and sleep irregularity, but others have explored associations between sleep beliefs, sleep hygiene, and sleep quality in university students20. The results of this study found a high level of poor subjective sleep quality (60.4%) with poor sleep hygiene being the only significant predictor, after adjustment. It is worth considering that sleep hygiene practices are likely to be motivated by accurate and healthy sleep beliefs as opposed to dysfunctional ones, thus there is the possibility of a mediating effect, although this was not explored or reported in the study. It is, however, also important to emphasize that sleep beliefs may not translate into actual sleep behavior. For example, university students in particular tend to have more limited daily requirements (apart from class attendance) as well as poor sleep hygiene, yet they may be equipped with knowledge pertaining to sleep-enhancing behaviors such as minimizing caffeine intake and screen-time, as well as taking regular exercise.
Mental health issues can significantly disrupt women’s sleep–wake cycles, often leading to irregular and poorer quality sleep. Unlike findings from other studies2,10,11,13, we did not identify significant relationships between sleep regularity and psychological or physical health outcomes. A cultural factor influencing mental health in the UAE is the stigma associated with it, along with the belief that mental health issues are caused by the “Jinn” and a lack of awareness that these are real psychological conditions50. This could have introduced biases in responses to the HADS questionnaire, despite its strong validation and reliability. For the clinical health outcomes measured (fasting blood glucose, BMI and blood pressure), one possible explanation for these objective measures not being significantly associated with sleep regularity may be due to the young age of the participants. There tends to be less variability amongst these measures in younger age groups as compared to older adults, thus making it more difficult to detect differences.
Given the well-documented age, racial, and gender differences in sleep28,29, our study focused exclusively on young, female, Emirati adults, an extensively under-studied group. This specific population may have irregular sleep–wake patterns due to various socio-cultural factors. Given the collectivist and traditional Emirati culture, sleep regularity may be impaired in young, university-attending females who could be expected to care for younger siblings and aging parents and/or grandparents. Another known disruptor of female sleep is hormone fluctuations51. Biological drivers, such as menstrual cycle variability, also contribute to sleep quality51; thus, it is possible that the menstrual phase could have impacted sleep timing and regularity in our all-female sample. Additionally, academic demands may be met by using technology to fulfill study requirements, with weekends providing ample time for study and pleasure, resulting in later bedtimes compared to weekdays. Thus, the observation between SJL and TUQ is, perhaps, not surprising and could be further exacerbated by the aforementioned cultural family expectations.
Although this is the first study to explore a range of factors in relation to sleep irregularity using objective sleep estimates, and although we conducted our study in a relatively neglected population (UAE university students), we acknowledge some limitations. First, our sample size was relatively constrained, which hinders the feasibility of applying more complex methodological approaches such as latent profile analysis52. Nonetheless, considering the seven-day wrist actigraphy requirement, our cohort size is comparable with other studies of similar design6,53,54. Furthermore, the validity of our results is reinforced by obtaining similar findings using IS and SRIWASO-Nawak measures. A second limitation is that our results may not be generalizable to male university students or other university students outside of the UAE. Given our all-female sample, the menstrual phase is a potential confounder, which we did not obtain data for. Moreover, social-cultural factors previously discussed could have affected sleep, although information on these was not obtained. Other potential confounders with unobtained data are employment status and possible shift work. However, it is uncommon for young, Emirati females, registered as full-time university students, to also be employed whilst studying. Third, despite using validated and reliable tools/questions, we relied on self-reported measures for several outcomes such as mental health, sleep beliefs, bedtime technology use, and lifestyle behaviors. This could have resulted in a range of common biases such as recall, social desirability or others, which, in turn, could have influenced our overall findings. Fourth, we asked about the subjective frequency of night-time technology use and day-time napping but did not capture information pertaining to duration. Finally, our cross-sectional design does not determine cause-effect relationships, but it does provide key insights into sleep irregularity in an under-investigated population and has identified some key avenues for future studies in this area.
In conclusion, our study adds to the growing body of evidence surrounding sleep irregularity. Our findings are unique to female university students in a country where sleep habits have not been extensively explored. We show, for the first time, that sleep irregularity between weekdays and weekends is linked to greater use of night-time technology. Moreover, daily and weekly sleep irregularity were associated with dysfunctional sleep beliefs, while daily sleep irregularity was also significantly associated with poor sleep quality and more frequent daytime napping. We recommend that future studies unravel the precise contributions of daytime napping versus nocturnal sleep in relation to sleep regularity as well as technology use and sleep beliefs. Our study also needs to be replicated in other populations to either confirm or refute the findings. We also recommend carefully planned and well-designed studies to explore cause-effect associations so that university students, as well as other populations, can be educated about the significance of sustaining consistent and regular sleep–wake patterns.
Data availability
Actigraphy data are not publicly available but can be obtained upon reasonable request to the authors.
References
Okun, M. L. et al. Sleep variability, health-related practices and inflammatory markers in a community dwelling sample of older adults. Psychosom. Med. 73, 142 (2011).
Bernert, R. A., Hom, M. A., Iwata, N. G. & Joiner, T. E. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J. Clin. Psychiatry 78, 19738 (2017).
Doane, L. D., Gress-Smith, J. L. & Breitenstein, R. S. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J. Youth Adolesc. 44, 389–404 (2015).
Vanderlind, W. M. et al. Sleep and sadness: Exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Med. 15, 144–149 (2014).
Kuula, L. et al. Naturally occurring circadian rhythm and sleep duration are related to executive functions in early adulthood. J. Sleep Res. 27, 113–119 (2018).
Phillips, A. J. K. et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci. Rep. 7, 3216 (2017).
McBean, A. L. & Montgomery-Downs, H. E. Timing and variability of postpartum sleep in relation to daytime performance. Physiol. Behav. 122, 134–139 (2013).
Morales-Ghinaglia, N. & Fernandez-Mendoza, J. Sleep variability and regularity as contributors to obesity and cardiometabolic health in adolescence. Obesity 31, 597–614 (2023).
Tsai, S.-Y., Tung, Y.-C., Huang, C.-M. & Lee, C.-C. Sleep and its variability in relation to behavioral outcomes in school-age children with overweight and obesity. Res. Nurs. Health (2023).
Spruyt, K., Molfese, D. L. & Gozal, D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics 127, e345–e352 (2011).
Chontong, S., Saetung, S. & Reutrakul, S. Higher sleep variability is associated with poorer glycaemic control in patients with type 1 diabetes. J. Sleep Res. 25, 438–444 (2016).
Patel, S. R. et al. The association between sleep patterns and obesity in older adults. Int. J. Obes. 38, 1159–1164 (2014).
Zhu, B., Kapella, M. C., Zhao, X. & Fritschi, C. Intra-individual variability in sleep is related to glycaemic control in adults with type 2 diabetes. J. Adv. Nurs. 76, 991–998 (2020).
Baker, A. E., Tashjian, S. M., Goldenberg, D. & Galván, A. Sleep variability over a 2-week period is associated with restfulness and intrinsic limbic network connectivity in adolescents. Sleep 46, zsac248 (2023).
Matos, M. G., Gaspar, T., Tomé, G. & Paiva, T. Sleep variability and fatigue in adolescents: Associations with school-related features. Int. J. Psychol. 51, 323–331 (2016).
Rodríguez-Colón, S. M. et al. Sleep variability and cardiac autonomic modulation in adolescents–Penn State Child Cohort (PSCC) study. Sleep Med. 16, 67–72 (2015).
Windred, D. P. et al. Sleep regularity is a stronger predictor of mortality risk than sleep duration: A prospective cohort study. Sleep zsad253 (2023).
Jonasdottir, S. S., Minor, K. & Lehmann, S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: A global-scale wearables study. Sleep 44 (2021).
Becker, S. P. et al. Sleep in a large, multi-university sample of college students: Sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4, 174–181 (2018).
Humphries, R. K., Bath, D. M. & Burton, N. W. Dysfunctional beliefs, sleep hygiene and sleep quality in university students. Health Promot. J. Aust. 33, 162–169 (2022).
Wittmann, M., Dinich, J., Merrow, M. & Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 23, 497–509 (2006).
Roenneberg, T., Pilz, L. K., Zerbini, G. & Winnebeck, E. C. Chronotype and social jetlag: A (self-) critical review. Biology (Basel) 8, 54 (2019).
Hand, A. J. et al. Measuring light regularity: Sleep regularity is associated with regularity of light exposure in adolescents. Sleep 46 (2023).
Koopman, A. D. M. et al. The association between social jetlag, the metabolic syndrome, and type 2 diabetes mellitus in the general population: The New Hoorn Study. J. Biol. Rhythm. 32, 359–368 (2017).
Zhu, H., Xu, Y., Lin, D., Wang, X. & Niu, B. Relationship between social jetlag and body mass index in nurses working shift schedules: A cross-sectional study. Sci. Rep. 14, 16911 (2024).
Mota, M. C. et al. Association between social jetlag food consumption and meal times in patients with obesity-related chronic diseases. PLoS One 14, e0212126 (2019).
Mathew, G. M., Li, X., Hale, L. & Chang, A.-M. Sleep duration and social jetlag are independently associated with anxious symptoms in adolescents. Chronobiol. Int. 36, 461–469 (2019).
Saelee, R., Haardörfer, R., Johnson, D. A., Gazmararian, J. A. & Suglia, S. F. Racial/ethnic and sex/gender differences in sleep duration trajectories from adolescence to adulthood in a US national sample. Am. J. Epidemiol. 192, 51–61 (2023).
Li, L., Nakamura, T., Hayano, J. & Yamamoto, Y. Age and gender differences in objective sleep properties using large-scale body acceleration data in a Japanese population. Sci. Rep. 11, 9970 (2021).
Bei, B., Seeman, T. E., Carroll, J. E. & Wiley, J. F. Sleep and physiological dysregulation: A closer look at sleep intraindividual variability. Sleep 40, zsx109 (2017).
Fischer, D., Klerman, E. B. & Phillips, A. J. K. Measuring sleep regularity: Theoretical properties and practical usage of existing metrics. Sleep 44, zsab103 (2021).
Halson, S. L. et al. Sleep regularity and predictors of sleep efficiency and sleep duration in elite team sport athletes. Sport. Med. 8, 1–10 (2022).
Cole, R. J., Kripke, D. F., Gruen, W., Mullaney, D. J. & Gillin, J. C. Automatic sleep/wake identification from wrist activity. Sleep 15, 461–469 (1992).
Buysse, D. J., Reynolds, C. F. III., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Morin, C. M., Vallières, A. & Ivers, H. Dysfunctional beliefs and attitudes about sleep (DBAS): Validation of a brief version (DBAS-16). Sleep 30, 1547–1554 (2007).
Hubert Lam, K. et al. Napping is associated with increased risk of type 2 diabetes: The Guangzhou Biobank Cohort Study. Sleep 33, 402–407 (2010).
Ness, A. R. The Avon Longitudinal Study of Parents and Children (ALSPAC)–a resource for the study of the environmental determinants of childhood obesity. Eur. J. Endocrinol. 151, U141–U149 (2004).
Arora, T. et al. The complexity of obesity in UK adolescents: Relationships with quantity and type of technology, sleep duration and quality, academic performance and aspiration. Pediatr. Obes. 8, 358–366 (2013).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370 (1983).
Sakia, R. M. The Box-Cox transformation technique: A review. J. R. Stat. Soc. Ser. D Stat. 41, 169–178 (1992).
Meyerson, W. U. et al. The association between evening social media use and delayed sleep may be causal: Suggestive evidence from 120 million Reddit timestamps. Sleep Med. 107, 212–218 (2023).
Exelmans, L. & den Bulck, J. Binge viewing, sleep, and the role of pre-sleep arousal. J. Clin. Sleep Med. 13, 1001–1008 (2017).
AlShareef, S. M. The impact of bedtime technology use on sleep quality and excessive daytime sleepiness in adults. Sleep Sci. 15, 318 (2022).
Gonidis, L. & Sharma, D. Internet and Facebook related images affect the perception of time. J. Appl. Soc. Psychol. 47, 224–231 (2017).
Reardon, A., Lushington, K. & Agostini, A. Adolescent sleep, distress, and technology use: Weekday versus weekend. Child Adolesc. Ment. Health 28, 108–116 (2023).
Mireku, M. O. et al. Night-time screen-based media device use and adolescents’ sleep and health-related quality of life. Environ. Int. 124, 66–78 (2019).
Arora, T., Alhelali, E. & Grey, I. Poor sleep efficiency and daytime napping are risk factors of depersonalization disorder in female university students. Neurobiol. Sleep Circadian Rhythm. 9, 100059 (2020).
Albqoor, M. A. & Shaheen, A. M. Sleep quality, sleep latency, and sleep duration: A national comparative study of university students in Jordan. Sleep Breath. 25, 1147–1154 (2021).
Wuyts, J. et al. The influence of pre-sleep cognitive arousal on sleep onset processes. Int. J. Psychophysiol. 83, 8–15 (2012).
Ghubash, R. & Eapen, V. Postpartum mental illness: Perspectives from an Arabian Gulf population. Psychol. Rep. 105, 127–136 (2009).
Baker, F. C. & Lee, K. A. Menstrual cycle effects on sleep. Sleep Med. Clin. 17, 283–294 (2022).
Spurk, D., Hirschi, A., Wang, M., Valero, D. & Kauffeld, S. Latent profile analysis: A review and “how to” guide of its application within vocational behavior research. J. Vocat. Behav. 120, 103445 (2020).
Pillai, V., Steenburg, L. A., Ciesla, J. A., Roth, T. & Drake, C. L. A seven day actigraphy-based study of rumination and sleep disturbance among young adults with depressive symptoms. J. Psychosom. Res. 77, 70–75 (2014).
Zhang, X., Wang, F., Zou, L. & Lee, S.-Y. Depressive symptoms, sleep-wake features, and insomnia among female students: The role of rumination. J. Health Psychol. https://doi.org/10.1177/13591053241258252 (2024).
Acknowledgements
This project was funded by a start-up grant awarded to the Principal Investigator (TA) from Zayed University. This work was also supported by 'Ministerio de Ciencia e Innovación/Agencia Estatal de Investigación/10.13039/501100011033/', ERDF A way of making Europe, and NextGenerationEU/PRTR under projects PID2020-115468RB-I00 and PID2023-148895OB-I00, and by CIBER -Consorcio Centro de Investigación Biomédica en Red- (CB19/01/00012) through ‘Instituto de Salud Carlos III (ISCIII)’. F. Vaquerizo-Villar is supported by a “Sara Borrell” grant (CD23/00031) from the ISCIII cofounded by the ‘Fondo Social Europeo Plus (FSE +)’. D. Gozal is supported by National Institute on Aging grant AG061824.
Author information
Authors and Affiliations
Contributions
Data collection: TA; Study design TA, FV-V, RH, and DG. Implementation: FV-V. Data analysis: FV-V. Manuscript writing: TA, FV-V, RH, and DG. Manuscript review: TA, FV-V, RH, and DG. Funding acquisition: TA, FV-V, RH, and DG. All authors gave their final approval of this version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Arora, T., Vaquerizo-Villar, F., Hornero, R. et al. Sleep irregularity is associated with night-time technology, dysfunctional sleep beliefs and subjective sleep parameters amongst female university students. Sci Rep 15, 6374 (2025). https://doi.org/10.1038/s41598-025-90720-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90720-x