Abstract
Locally advanced gastric cancer (LAGC) poses a significant surgical challenge. While laparoscopic gastrectomy (LG) offers potential advantages, its cost-effectiveness relative to open gastrectomy (OG) in China remains uncertain. To compare the cost-effectiveness of LG and OG for LAGC in China. A Markov model compared the cost-effectiveness of LG and OG for LAGC. Probabilities and utilities were derived from published literature. Direct medical costs were obtained from the First Hospital of Lanzhou University. The primary outcome was the incremental cost-effectiveness ratio (ICER), expressed as the cost per quality-adjusted life-year (QALY) gained, using a willingness-to-pay threshold of ¥268,074/QALY. Sensitivity analyses assessed model robustness. Across 1-, 3-, and 5-year time horizons, OG had lower total costs and greater effectiveness than LG for LAGC. At 5 years, OG had a total cost of ¥128,259 and 7.20 QALYs versus LG’s ¥136,668 and 7.18 QALYs; the ICER for OG was -¥474,758/QALY. OG dominated at the ¥268,074 willingness-to-pay threshold. Sensitivity analysis indicated that variations in LG and OG costs minimally influenced the cost-effectiveness. Probabilistic sensitivity analysis, performed across 10,000 iterations, consistently identified OG as the optimal strategy (100% of iterations). From a Chinese health economics perspective—a framework essential for informing national healthcare resource allocation—OG consistently demonstrated a superior cost-effectiveness compared with LG for LAGC across 1, 3, and 5 years. This longitudinal observation of sustained cost-effectiveness persisted despite the statistically insignificant differences in overall costs and effectiveness between the two procedures.
Similar content being viewed by others
Gastric cancer (GC) represents a significant global health burden, ranking as the fifth most prevalent malignancy and cause of cancer-related mortality1. China has a particularly high prevalence of GC, with a substantial burden of locally advanced gastric cancer (LAGC), which presents significant surgical management challenges.
Standard treatment for LAGC involves radical gastrectomy with lymphadenectomy via open gastrectomy (OG) or laparoscopic gastrectomy (LG). While OG has been the traditional approach2, LG, a less invasive alternative, may offer benefits such as reduced postoperative complications and shorter hospital stays. Though LG has demonstrated safety and efficacy in early-stage GC3,4,5, achieving cure rates exceeding 90%, particularly those located in the middle or lower third of the stomach6,7. However, its role in LAGC remains debated due to increased tumor size and lymph node metastasis risk, which raise concerns about long-term efficacy and safety. Multicenter trials8,9, including the CLASS-01 study in China10, suggest LG may offer non-inferior outcomes compared with OG; however, LG costs are expected to be higher due to longer operating times and surgical materials or disposables. Furthermore, some studies report limited cost and effectiveness differences between LG and OG11. Hence, the clinical benefit of LG has not been proven so far in China, which necessitates a dedicated cost-effectiveness analysis between the two procedures.
The cost-effectiveness of LG versus OG for LAGC in China remains unclear. Robust data on the cost-effectiveness of LG and OG with patient-reported outcomes are limited in China. Although three observational cohort studies have compared the cost-effectiveness of LG and OG11,12,13, variations in healthcare cost structures, patient baselines, and clinical practices necessitate a tailored cost-effectiveness analysis for China. Existing analyses11,12, assessing quality of life (QoL) and costs one year post-surgery in patients with resectable gastric adenocarcinoma, may not fully capture long-term survival and cost impacts14. Given comparable 5-year recurrence-free survival rates between LG and OG (75.7% vs. 73.9%)8, with approximately one-third of patients experiencing recurrence within three years, a longer follow-up is needed for a comprehensive long-term assessment. Currently, published cost-effectiveness analyses of LG and OG for LAGC are lacking. Establishing cost-effective and sustainable treatment strategies for GC in China is a priority.
To fill this evidence gap, this study aims to assess the cost-effectiveness of LG versus OG for LAGC from a Chinese healthcare system perspective, using a Markov model with 1-, 3-, and 5-year time horizons and actual Chinese medical cost data. The model was designed to more accurately simulate disease progression and overcome limitations of insufficient time horizons in previous research. Model parameters were informed by the latest Japanese randomized controlled trial data, which closely represents the Chinese population.
Methods
Base-case patient
Given that gastric cancer incidence is relatively low before age 50, but increases sharply with age thereafter, peaking at 55–80 years, and is approximately twice as high in males as in females15,16,17,18, the base-case patient was defined as a hypothetical 50-year-old male diagnosed with stage III gastric adenocarcinoma, classified as locally advanced according to the Japanese Classification10,19. The tumor, confirmed by preoperative evaluation and gastroscopy biopsy, was located in the lower or middle third of the stomach. No nodal or distant metastasis or prior gastrectomy was present. The base-case analysis assumed a 5-year follow-up period for both LG and open OG, both including D2 lymphadenectomy.
Treatment characteristics and strategies
GC management adhered to guidelines from organizations such as the Chinese Society of Clinical Oncology20,21. Due to the lack of standardized chemotherapy regimens in advanced GC, such as chemotherapy cycles for patients experiencing metastasis or recurrence following gastrectomy, the model simulated conservative scenarios for both LG and OG treatments. Following two cycles of neoadjuvant chemotherapy, patients underwent either OG or LG, followed by four cycles of adjuvant chemotherapy20. Perioperative chemotherapy regimens included XELOX (oxaliplatin + capecitabine), and SOX (tegafur + oxaliplatin)21,22.
For stable disease, routine postoperative follow-up occurred every 3 months for the first 2 years and every 6 months for the next 3 years21. Follow-up included physical examination, blood testing, abdominal computed tomographic scans with tumor markers (every 3 months for the first 2 years, then every 6 months). Gastroscopy was performed annually for 5 years; abdominopelvic CT or ultrasound was alternatively performed21.
Local recurrence prompted a radical gastrectomy, followed by six cycles of adjuvant chemotherapy (XELOX, SOX)21. Distant metastasis was treated with six cycles of palliative chemotherapy (TC: Carboplatin + Paclitaxel, FP: Cisplatin + 5-FU, XP: Cisplatin + Capecitabine)21,23.
Positron emission tomography-computed tomography was used for suspected recurrence, identified via medical history, physical examination, imaging, and, if feasible, cytology or tissue biopsy10. Postoperative complications were assumed to be of Grade III-IV.
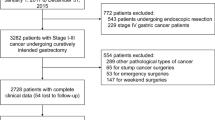
Markov model
A Markov model, constructed using TreeAge Software Pro version 2022, compared the long-term cost-effectiveness of LG and OG. The Markov model included nodes representing transitions to new health states: stability of disease after OG/LG; local recurrence after OG/LG requiring resection (including primary tumor growth or development of regional lymph node metastases); metastasis after OG/LG; operative complications; and death. The model used a 6-month cycle length and a 5-year time horizon, reflecting that most (60%) disease recurrences occur within 2 years of resection or treatment and over 90% occur within 5 years14 (Fig. 1).
Model parameters
Costs, obtained from the First Affiliated Hospital of Lanzhou University, included direct costs for gastrectomy, outpatient visits, laboratory tests, gastroscopy, and abdominal contrast-enhanced CT scans. Reference case values and ranges are presented in Table 1.
Effectiveness was measured in quality-adjusted life years (QALYs), calculated as health utility multiplied by time. Health utility values, ranging from 0 (death) to 1 (perfect health), were obtained from published literature11. Table 1shows utility scores by health state, with the stable disease value from reference11. Utility values for recurrence after LG and OG were set at half the stable disease value (0.4095 and 0.4145, respectively), assuming equivalence between recurrence and metastasis. Sensitivity analyses addressed the uncertainty of these assumptions using wide ranges for variables.
Local recurrence, metastasis and death probabilities were determined from the literature (Table 1)8. Surgical complication rates after LG and OG were derived from relevant studies8. Cost and QALYs were discounted at a rate of 3%.
Base-case analysis
Expected costs and utilities for each treatment option were calculated by multiplying each outcome’s cost and utility by its probability. Each strategy generated separate costs and discounted lifetime QALYs, which were used to calculate the incremental cost-effectiveness ratio (ICER) using the formula: (cost of LG – cost of OG) / (QALYs for LG – QALYs for OG). A strategy was considered “cost-saving” if it was both less costly and more effective (i.e., it dominated the competing strategy). A strategy was deemed cost-effective if its ICER was below the willingness-to-pay threshold of ¥268,074 per QALY.
Sensitivity analysis
Sensitivity analyses explored the variability of results across a plausible range. One-way sensitivity analyses assessed the impact of individual parameters (probabilities, costs, and utilities). In univariable sensitivity analysis, transformation probabilities, health utility values, and costs varied by ± 20%, ± 10%, and ± 25%, respectively; the discount rate ranged from 1 to 5% (Supplementary Table 1).
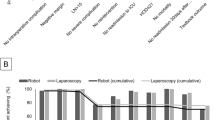
Multivariate sensitivity analysis was used to systematically evaluate the impact of simultaneous variations in multiple input parameters on model outputs, thereby elucidating the sources and extent of model uncertainty. Unlike univariate analysis, which assesses single-parameter effects, multivariate analysis identifies key parameters significantly influencing model outcomes and quantifies overall model robustness. Because model outputs are influenced by the interaction of multiple parameters, univariate analysis may not capture these effects, potentially leading to partial interpretations of model behavior. Thus, multivariate sensitivity analysis was used to assess the model’s overall sensitivity to input parameter uncertainties. Tornado diagrams present results of multivariate sensitivity analyses (Fig. 2).
Probabilistic sensitivity analyses explored uncertainties around model inputs by varying them simultaneously using Monte Carlo simulations (1,000 iterations) with different distributions based on previously published literature as well as other peer-reviewed cost-effectiveness analyses24. Beta distributions were used for health utilities and probabilities; normal distributions, for costs data. Table 1 shows parameter ranges and distributions used. Scatter plots present the results of probabilistic sensitivity analyses (Fig. 3).
Results
Base-case
In the base case scenario, modeling a 5-year follow-up for both LG and OG in middle-aged patients, OG was less costly (¥128,259) and more effective (7.20 QALYs) than LG (¥136,668; 7.18 QALYs). The resulting ICER for OG was -¥474,758/QALY gained. At a willingness-to-pay threshold of ¥268,074/QALY, OG was deemed more cost-effective than LG (Table 2).
Similar trends were observed in 1- and 3-year follow-up analyses. OG was associated with lower costs (¥95,151 and ¥113,112, respectively) and increased effectiveness (2.37 and 5.02 QALYs, respectively) relative to LG (¥103,838 and 2.34 QALYs; ¥121,575 and 4.99 QALYs). The corresponding ICERs for OG in the 1- and 3-year models were -¥368,236/QALY and -¥279,590/QALY, respectively, and were below the willingness-to-pay threshold, indicating OG’s cost-effectiveness (Table 2).
Sensitivity analysis
One-way sensitivity analysis (Supplemental Table 1) showed that the ICER varied most when parameters were assessed across their full range. Treatment costs for LG and OG, probability of postoperative metastasis, and the utility value of disease progression were key factors influencing study conclusions.
Multivariate sensitivity analyses (Fig. 2) showed that variations in metastasis rates for LG and OG did not change the primary conclusion that OG remained cost-effective. Despite varying these parameters, positive incremental effectiveness and ICERs persisted, confirming OG’s cost-effectiveness or cost-saving potential. However, treatment costs associated with LG and OG had a moderate influence on the study conclusions, while other factors had less effect.
Probabilistic sensitivity analyses, consistent with the base-case analysis, showed that 100% of 1000 bootstrap iterations, displayed in the cost-effectiveness plane (Fig. 3), indicated lower costs and higher effectiveness for OG, thus demonstrating its cost-effectiveness.
Discussion
This analysis aimed to determine the cost-effectiveness of LG versus OG for patients with LAGC in China. Results indicated that OG was consistently more cost-effective than LG across 1-, 3-, and 5-year time horizons, incurring lower costs and greater effectiveness.
While this analysis suggests OG’s cost-effectiveness for LAGC, a prior decision tree model found LG more cost-effective12. That study included patients with pathological stage I GC, whose QoL values were based on trials of early-stage cancer. Over 10% of cases initially classified as clinical T3-T4 GC are later found to be pathological stage I25, and the KLASS-02 trial reported over 35% in LAGC9. This heterogeneity presents a challenge to isolating the impact of early-stage cancer on study outcomes. To mitigate this, we used probability values from a Japanese multicenter, prospective, randomized controlled trial involving 507 patients with LAGC8. This larger cohort, with standardized, high-quality laparoscopic surgical procedures, may provide a more precise evaluation of surgical outcomes and LG quality in East Asia8.
The QALY gains up to 1, 3, and 5 years postoperatively were 0.03, 0.03, and 0.02, respectively, and were lower in the laparoscopic group compared with the open group. These findings consistent with the LOGICA trial11. While QALYs constitute an important metric, treatment cost remains a critical consideration in the decision-making process. Despite the observed minimal differences in QALYs between the two surgical approaches, the laparoscopic group exhibited higher costs relative to the open group. Specifically, cost differentials at 1, 3, and 5 years were ¥8,687, ¥8,463, and ¥8,409, respectively. Based on our analysis, open gastrectomy (OG) appears to be more cost-effective. This is likely due to lower complication rates, shorter post-operative hospital stays, and reduced post-operative hospitalization costs in the laparoscopic group offsetting the higher initial surgical costs.
This study’s cost estimates for LG and OG differed from those of three non-randomized observational studies: a Japanese national database($21,510 vs. $21,024)26, a US medical center database ($40,633 vs. $41,326)27, and a Dutch single-center study ($7,320 vs. $6,554)11. These discrepancies, identified through comparison with literature review, may stem from variations in healthcare costs across regions and our focus on direct medical costs, which excluded indirect costs. Additionally, the analysis incorporated neoadjuvant and adjuvant chemotherapy costs, assuming consistent regimens for both groups.
Post-recurrence utility values of 0.4095 and 0.4145 were assumed for LG and OG, respectively. These assumptions require careful consideration because of a lack of high-quality studies specifically investigating QoL in locally LAGC and the psychological and physical distress from disease progression. Distress arises not only from cancer and treatment but also from fear of losing control and of death28. A study of advanced GC showed declining QoL with disease progression29, and a prospective study of solid tumors supports this28. These findings suggest that disease progression is associated with a deterioration in health-related QoL28. Despite the potential simplifications, the assumed utility values may be considered reasonable. Therefore, to assess the impact of these utility values on study outcomes, we conducted a sensitivity analysis. Sensitivity analysis demonstrated that the ICER remained below the willingness-to-pay threshold (¥268,074/QALY) across the plausible range of utility values, indicating the robustness of the study’s primary findings. Multivariate sensitivity analysis showed that treatment costs for LG and OG exerted a degree of influence on study conclusions, because of the composite and variable nature of total surgical costs (including surgical, hospitalization, medication, examination, complication, and follow-up expenses) and cost heterogeneity across hospitals, regions, and patients. These findings underscore the need for clinicians to consider patient-specific factors and treatment costs when developing strategies and choosing surgical modalities in GC to enhance clinical decision-making reliability.
This study has several limitations. First, utility values from international literature and probability values from East Asian cancer centers were used, without validated methods for adjustment to the Chinese population, which may limit generalizability. Larger, multicenter prospective studies are needed to determine cost-effectiveness within China. Second, the model assumed constant progression and metastasis rates regardless of age and sex, precluding subgroup analyses. Recent evidence suggests younger age30and male sex31 are associated with increased tumor progression, which could affect OG cost-effectiveness. Third, patient heterogeneity precluded collection of indirect cost data, potentially introducing bias. This study excluded indirect costs (e.g., productivity and wage losses), and while their inclusion could influence findings, their variability makes it difficult to ascertain the direction and magnitude of that influence. Finally, the model’s inherent limitations may have simplified clinical complexities, particularly regarding specific patient subgroups and future uncertainties.
This study’s strengths include being the first cost-effectiveness analysis of LG versus OG for LAGC in China. It also addresses prior studies’ short time horizons by evaluating short- and long-term outcomes using 1-, 3-, and 5-year simulations based on observed survival and recurrence patterns.
Conclusion
In conclusion, OG consistently demonstrated greater cost-effectiveness than LG for locally advanced gastric cancer in China across 1-, 3-, and 5-year time horizons. These findings support OG as an economically advantageous strategy for clinical and patient decision-making. Furthermore, for healthcare policy, wider OG adoption could alleviate the financial burden through optimized resource allocation.
Data availability
All data generated or analysed during this study are included in this article(Table and Supplement table).
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 74 (3), 229–263 (2024).
Al-Batran, S. E. et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet (London England). 393 (10184), 1948–1957 (2019).
Katai, H. et al. Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric cancer: Official J. Int. Gastric Cancer Association Japanese Gastric Cancer Association. 20 (4), 699–708 (2017).
Kim, H. H. et al. Effect of laparoscopic distal gastrectomy vs Open Distal Gastrectomy on Long-Term Survival among patients with stage I gastric Cancer: the KLASS-01 Randomized Clinical Trial. JAMA Oncol. 5 (4), 506–513 (2019).
Katai, H. et al. Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol. Hepatol. 5 (2), 142–151 (2020).
Japanese gastric cancer treatment guidelines (2014) (ver. 4). Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 20(1), 1–19 (2017)
Kim, W. et al. Decreased morbidity of laparoscopic distal gastrectomy compared with Open Distal Gastrectomy for Stage I gastric Cancer: short-term outcomes from a Multicenter Randomized Controlled Trial (KLASS-01). Ann. Surg. 263 (1), 28–35 (2016).
Etoh, T. et al. Five-year survival outcomes of Laparoscopy-assisted vs Open Distal Gastrectomy for Advanced Gastric Cancer: the JLSSG0901 Randomized Clinical Trial. JAMA Surg. 158 (5), 445–454 (2023).
Hyung, W. J. et al. Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric Cancer: the KLASS-02-RCT Randomized Clinical Trial. J. Clin. Oncology: Official J. Am. Soc. Clin. Oncol. 38 (28), 3304–3313 (2020).
Yu, J. et al. Effect of laparoscopic vs Open Distal Gastrectomy on 3-Year disease-free survival in patients with locally advanced gastric Cancer: the CLASS-01 Randomized Clinical Trial. Jama 321 (20), 1983–1992 (2019).
van der Veen, A. et al. Cost-effectiveness of laparoscopic vs Open Gastrectomy for gastric Cancer: an economic evaluation alongside a Randomized Clinical Trial. JAMA Surg. 158 (2), 120–128 (2023).
Gosselin-Tardif, A. et al. Laparoscopic versus open subtotal gastrectomy for gastric adenocarcinoma: cost-effectiveness analysis. BJS open. 4 (5), 830–839 (2020).
Tegels, J. J. et al. Introduction of laparoscopic gastrectomy for gastric cancer in a western tertiary referral centre: a prospective cost analysis during the learning curve. World J. Gastrointest. Oncol. 9 (5), 228–234 (2017).
Lai, J. F. et al. Prediction of recurrence of early gastric cancer after curative resection. Ann. Surg. Oncol. 16 (7), 1896–1902 (2009).
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: a cancer journal for clinicians. 71(3), 209–249 (2021).
Thrift, A. P. & El-Serag, H. B. Burden of gastric Cancer. Clin. Gastroenterol. Hepatology: Official Clin. Pract. J. Am. Gastroenterological Association. 18 (3), 534–542 (2020).
Xia, C. et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin. Med. J. 135 (5), 584–590 (2022).
[Chinese Guideline on Risk Management of Gastric Cancer in the General. Public(2023 Edition)]. Zhonghua Yi Xue Za Zhi. 103 (36), 2837–2849 (2023).
Japanese classification of gastric carcinoma: 3rd English edition. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 14(2), 101–112 (2011).
Wang, F. H. et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer, 2021. Cancer Commun. (London England). 41 (8), 747–795 (2021).
Wang, F. H. et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer, 2023. Cancer Commun. (London England). 44 (1), 127–172 (2024).
Xing, J. et al. Long-term outcomes of laparoscopic versus open distal gastrectomy for patients with advanced gastric cancer in North China: a multicenter randomized controlled trial. Surg. Endosc. 38 (9), 4976–4985 (2024).
Koizumi, W. et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 9 (3), 215–221 (2008).
Cui, C. L. et al. Cost effectiveness of Watch and wait Versus Resection in rectal Cancer patients with complete clinical response to Neoadjuvant Chemoradiation. Ann. Surg. Oncol. 29 (3), 1894–1907 (2022).
Fukagawa, T. et al. A prospective multi-institutional validity study to evaluate the accuracy of clinical diagnosis of pathological stage III gastric cancer (JCOG1302A). Gastric cancer: Official J. Int. Gastric Cancer Association Japanese Gastric Cancer Association. 21 (1), 68–73 (2018).
Yasunaga, H. et al. Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann. Surg. 257 (4), 640–646 (2013).
Glenn, J. A., Turaga, K. K., Gamblin, T. C., Hohmann, S. F. & Johnston, F. M. Minimally invasive gastrectomy for cancer: current utilization in US academic medical centers. Surg. Endosc. 29 (12), 3768–3775 (2015).
Marschner, N. et al. Association of Disease Progression with Health-Related quality of life among adults with breast, lung, pancreatic, and Colorectal Cancer. JAMA Netw. open. 3 (3), e200643 (2020).
Chau, I. et al. Association of quality of life with disease characteristics and treatment outcomes in patients with advanced gastric cancer: exploratory analysis of RAINBOW and REGARD phase III trials. Eur. J. cancer (Oxford England: 1990). 107, 115–123 (2019).
Qiu, W. W. et al. Postoperative follow-up for gastric cancer needs to be individualized according to age, tumour recurrence pattern, and recurrence time. Eur. J. Surg. Oncology: J. Eur. Soc. Surg. Oncol. Br. Association Surg. Oncol. 48 (8), 1790–1798 (2022).
Luan, X. et al. Sex disparity, prediagnosis lifestyle factors, and long-term survival of gastric cancer: a multi-center cohort study from China. BMC cancer. 24 (1), 1149 (2024).
Acknowledgements
We thank all authors for participating in this study.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 82260540, Project: Study on epigenetic regulation mechanism and clinical significance of NEK7-NLRP3 inflammasome) and the Gansu Provincial Health and Health Industry Scientific Research Program (Grant No. GSWSKY2022-19, Project: Risk factors and effects of HG during SPN after surgery for gastric cancer; a randomized controlled study of precise regulation of blood glucose by insulin).
Author information
Authors and Affiliations
Contributions
Lai Min, Li YanTing and Lan Ning collected data, analyzed the data. Lai Min and Li YanTing wrote the manuscript. Yuan Wenzhen approved the manuscript. All authors contributed to the article and approved the submitted version. The Min Lai and YanTing Li contributed to the work equllly and should be regarded as co-first authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived to prejudice the impartiality of the research reported.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lai, M., Li, Y., Lan, N. et al. Cost-effectiveness of open vs. laparoscopic gastrectomy for locally advanced gastric cancer in China. Sci Rep 15, 6714 (2025). https://doi.org/10.1038/s41598-025-91003-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91003-1