Abstract
Dyspnea is a prominent symptom in patients with long COVID due to its high prevalence and significant clinical impact. However, the influence of commonly used medications in critically ill patients on long-term dyspnea remains unclear. This study aimed to identify risk factors and assess the impacts associated with moderate to severe dyspnea in COVID-19 survivors. This study evaluated patients admitted to a university hospital between April 2020 and April 2021. Data were collected on clinical preconditions, hospital and ICU stays, and the use of corticosteroids, neuroleptics, neuromuscular blockers, midazolam, fentanyl, and noradrenaline. Post-discharge evaluations were conducted at 1 and 12 months, assessing dyspnea, frailty, quality of life, functional capacity, anxiety, and depression. Descriptive statistics, including frequencies and percentages, were used, and logistic regression analysis was performed to identify factors associated with moderate to severe dyspnea at 1 and 12 months post-discharge. Statistical significance was defined as P < 0.05. A total of 100 patients were prospectively included in the study; all underwent the 1-month evaluation, and 63 completed the 12-month evaluation. Limiting dyspnea, defined as an mMRC score > 1, was observed in 56.6% of patients at 1 month and 33.9% at 12 months post-discharge. Independent factors associated with limiting dyspnea at 1 month included the total dose of neuroleptics administered during hospitalization and the presence of pre-existing comorbidities. The use of corticosteroids, neuromuscular blockers, midazolam, fentanyl, and noradrenaline showed no significant association with limiting dyspnea. Dyspnea at 1 month post-discharge was an independent risk factor for the persistence of limiting dyspnea at 12 months. Patients with limiting dyspnea at 12 months exhibited higher levels of depression, anxiety, and frailty, alongside reduced quality of life and functionality. Patients with severe COVID-19 exhibit a high prevalence of limiting dyspnea in the long term. The total dose of neuroleptics administered during hospitalization and the presence of comorbidities were independently associated with limiting dyspnea after discharge. At 12 months post-discharge, individuals with persistent limiting dyspnea frequently demonstrated additional physical and mental health impairments, underscoring the need for comprehensive evaluation and management to mitigate the burden of long-term disabilities.
Similar content being viewed by others
Background
First identified in China in late 2019 and declared a pandemic in March 2020, COVID-19 has resulted in millions of deaths globally, including in Brazil, and has caused high rates of dysfunction among recovering patients. The World Health Organization (WHO) recommends that patients with confirmed or suspected COVID-19 have access to follow-up care if persistent symptoms are present1.
Long COVID, defined as symptoms persisting or emerging more than four weeks after acute COVID-19, has been associated with a range of dysfunctions2. Dyspnea, one of the most prevalent long-term symptoms, is a multifactorial and patient-centered concern. It has been observed in high proportions during early evaluations after hospital discharge and remains persistent in some patients even after two years of follow-up3.
The mechanisms underlying long-term complications of COVID-19 may include direct viral tissue damage to the respiratory system, central nervous system, and other organs4,5, as well as the severity of the inflammatory response6. In patients with acute respiratory distress syndrome (ARDS), respiratory mechanics have been associated with respiratory dysfunction and mortality in both the acute phase7 and the long term8. Similarly, in COVID-19, respiratory mechanics have been linked to acute outcomes9. During the critical care of severely ill patients, medications are often administered at high doses and for prolonged durations, but their long-term effects remain unclear.
A critical need exists to better understand the risk factors and mechanisms underlying post-COVID dyspnea. While inconsistent findings have been reported for several risk factors, no studies have specifically focused on the role of medications used during hospitalization10.
This study aimed to investigate factors associated with limiting dyspnea after hospital discharge, with a particular focus on the use of medications in the context of severe COVID-19. Additionally, it sought to identify the potential long-term impacts of limiting dyspnea.
Methods
We conducted a one-year follow-up study among patients admitted to referral hospitals for SARS-CoV-2 infection between April 2020 and April 202111. Following hospital discharge, the patients were evaluated at two time points: one month and twelve months post-discharge. The study was approved by the Ethics Committee for the Analysis of Research Projects of HCFMUSP (approval number: 31942020.0.0000.0068). We confirm that all methods were performed in accordance with relevant guidelines and regulations.
Eligibility criteria for participation included being at least 18 years of age, agreeing to participate in the study, and signing the informed consent form. Additionally, patients must have been admitted to the hospital with a confirmed diagnosis of COVID-19. Pregnant patients were excluded.
Participants underwent an initial evaluation, which included an interview to collect personal and sociodemographic data (e.g., name, age, date of birth, sex, race, marital status, education level, telephone, and address), medical history (Charlson Comorbidity Index, prior frailty, and EQ-5D-3 L questionnaire), and disease progression details (e.g., symptom onset, initial symptoms, history of hospitalization, and the need for respiratory support and oxygen therapy).
Dyspnea was assessed using the modified British Medical Research Council (mMRC) Dyspnea Scale12. This scale allows patients to report the extent to which breathlessness affects their mobility. It is graded on a 0–4 scale to establish clinical levels of breathlessness. Patients who scored 2, 3, or 4 were classified as having moderate to severely disabling post-COVID dyspnea.
Frailty was evaluated using the Clinical Frailty Scale, which comprises nine clinical criteria. Patients were classified as frail, pre-frail, or non-frail based on observations made by healthcare professionals and patient-reported information13. Anxiety and depressive symptoms were assessed using the Hospital Anxiety and Depression Scale (HADS). The HADS-Anxiety and HADS-Depression subscales each contain seven items scored on a 4-point Likert scale (0–3), with a maximum score of 21 per subscale. A cut-off score of ≥ 8 was applied to identify anxiety or depressive symptoms, based on established sensitivity and specificity thresholds14.
Quality of life was measured using the EQ-5D, a standardized and simple health instrument. The EQ-5D-3 L descriptive system evaluates five dimensions of health: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is rated using a 3-level verbal scale (1 = no problems, 2 = some problems, 3 = extreme problems), generating a single-digit score per dimension15.
The Medical Research Council (MRC) Sum Score was used to evaluate global muscle strength. Strength in six muscle groups (shoulder abduction, elbow flexion, wrist extension, hip flexion, knee extension, and ankle dorsiflexion) was assessed bilaterally using the MRC scale. The total score ranges from 0 to 60, with scores below 48 indicating significant weakness and scores below 36 identifying severe weakness16.
The one-minute sit-to-stand test was also conducted, recording baseline heart rate, blood pressure, respiratory rate, and SpO2 using a standard-height chair positioned next to a wall, as previously described17. Participants were instructed to stand and sit as many times as possible within one minute at a comfortable pace without using their arms for support. Desaturation nadirs, post-exercise heart rate, and respiratory rate were monitored until values returned to baseline.
Pulmonary function testing (PFT) was performed 1 month after discharge using the MedGraphics Cardiorespiratory Diagnostic System (Medical Graphics Corporation, USA). All tests were done according to Brazilian guidelines and reference ranges were calculated based on statistics formulated from the Brazilian population.
Potential risk factors for dyspnea at one and twelve months post-discharge were evaluated, including sex, age, pre-COVID frailty, Charlson Comorbidity Index, ICU and hospital length of stay, total corticosteroid doses (converted to dexamethasone equivalents and categorized into quartiles)18, total neuroleptic doses (converted to quetiapine equivalents and categorized into quartiles)19, and duration of midazolam, fentanyl, muscle relaxant, and norepinephrine use. For dyspnea at twelve months, additional factors included frailty and dyspnea status at one month post-discharge.
Demographic characteristics and long-term COVID-19 outcomes were presented as medians (interquartile ranges) for continuous variables and as absolute values with percentages for categorical variables. The Wilcoxon signed-rank test was used to compare frailty, health-related quality of life (HRQoL), clinical functionality, muscle weakness, and HADS scores for anxiety and depression between patients with and without limiting dyspnea. Associations between moderate to severe dyspnea and pre-selected risk factors—including sex, age, Charlson Comorbidity Index, pre-COVID frailty, cumulative corticosteroid dose (quartiles), cumulative neuroleptic dose, duration of neuromuscular blockade, fentanyl days, midazolam days, noradrenaline days, duration of mechanical ventilation, length of ICU stay, length of hospital stay, forced vital capacity (FVC, % of predicted) one month post-discharge, dyspnea one month post-discharge, and frailty one month post-discharge—were analyzed at one and twelve months post-discharge. Initially, a univariate analysis was conducted for all the specified parameters, followed by a multivariate logistic regression model incorporating only those parameters that demonstrated statistical significance in the univariate analysis.
All significance tests were two-sided, with a p-value < 0.05 considered statistically significant. Missing data were not imputed. All statistical analyses were performed using R, version 4.2.2.
Results
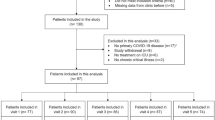
During the recruitment period (April 2020–July 2021), 108 patients were referred to the post-COVID service following hospital discharge. Of these, 100 patients were evaluated one month after discharge, and 63 patients were followed up 12 months after discharge (Fig. 1). No significant differences were observed between patients who completed the 12-month follow-up and those lost to follow-up in terms of sex, age, comorbidities, length of stay in the intensive care unit (ICU) or hospital, or use of mechanical ventilation.
Among the enrolled patients, 50 were male, and the median age was 59 years. A total of 89 patients had ICU stays exceeding 24 h, and 67 patients required mechanical ventilation for more than 24 h. Only three patients reported pre-existing pulmonary conditions: two had asthma, and one had bronchiectasis.
In terms of corticosteroid use, 46 patients received dexamethasone, 39 received methylprednisolone, and 48 received prednisone. After conversion to dexamethasone-equivalent doses, the median total dose of hospital-administered corticosteroids was 60 mg (range: 0–130.8 mg). Regarding neuroleptics, 60 patients received quetiapine, 9 received risperidone, and 23 received haloperidol. After conversion to quetiapine-equivalent doses, the median total dose of hospital-administered neuroleptics was 225 mg (range: 0–1158 mg). Midazolam was used for a median of 4 days (range: 0–7 days), fentanyl for 5 days (range: 0–10 days), muscle relaxants for 2 days (range: 0–5 days), and norepinephrine for 3 days (range: 0–7.5 days).
Dyspnea was assessed in 83 patients at 1 month and in 56 patients at 12 months. The prevalence of limiting dyspnea, defined as an mMRC score > 1, was 56.6% (47/83) at 1 month and 33.9% (19/56) at 12 months.
Baseline and hospitalization data for all patients, as well as for those who experienced limiting dyspnea at 1 and 12 months post-discharge, are summarized in Table 1.
Risk factors for dyspnea
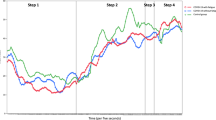
At 1 month post-discharge, univariate analysis identified the Charlson Comorbidity Index, ICU length of stay, hospital length of stay, cumulative corticosteroid dose, and cumulative neuroleptic dose as potential risk factors for dyspnea (Table 2). In multivariate analysis, significant risk factors included the Charlson Comorbidity Index (OR 1.27, 95% CI 1.02–1.63) and cumulative neuroleptic dose (OR 1.82, 95% CI 1.10–3.14) (Fig. 2).
At 12 months post-discharge, frailty at 1 month (P < 0.01) and dyspnea at 1 month (P < 0.01) were identified as significant risk factors in univariate analysis (Table 2). In multivariate analysis, dyspnea at 1 month post-discharge (OR 3.65, 95% CI 1.63–9.68) was the sole independent risk factor for dyspnea at 12 months (Fig. 3).
Impact of dyspnea at 12 months
Patients with dyspnea at 12 months exhibited greater frailty, poorer quality of life, increased mobility dysfunction, and higher levels of depression and anxiety compared to those without dyspnea (Table 3; Fig. 4).
Discussion
In evaluating limiting breathlessness among survivors of severe COVID-19 hospitalization, our study is the first to identify an independent association between the total dose of neuroleptics administered during hospitalization and the development of post-COVID dyspnea. This association persisted even after adjusting for other well-known risk factors for COVID-19 severity, including duration of mechanical ventilation, norepinephrine use, and length of ICU or hospital stay.
Dyspnea is a complex, multifactorial, and subjective experience of breathing discomfort influenced by physiological, psychological, and environmental factors20, 21. It is inconsistently correlated with traditional measures of lung function or imaging findings22,23. Consistent with prior studies, we observed a high prevalence of dyspnea following severe COVID-193,4, suggesting that its etiology likely involves a combination of interrelated factors. By identifying neuroleptic use as a risk factor, our findings add an important dimension to this multifactorial puzzle.
Delirium rates in mechanically ventilated COVID-19 patients are notably high, comparable to those observed in patients with similar critical illness unrelated to COVID-1924. ICU admission, prolonged mechanical ventilation, and high sedation doses are key contributors to delirium, with possible additional contributions from direct neuronal injury caused by SARS-CoV-225. Our patient cohort was at high risk for delirium, as 89% had ICU stays and 67% required mechanical ventilation.
In this context, neuroleptics were frequently used, often at high doses, primarily during ICU stays. The adverse effects of anticholinergic medications in critically ill patients include short-term sedation, respiratory depression, QTc prolongation, and daytime sedation, all of which could contribute to the observed association with post-COVID dyspnea26,27. While further studies are needed to clarify this relationship, our findings support the growing evidence that alternative approaches to managing ICU delirium should be prioritized, given the limited efficacy of neuroleptics and their potential for adverse effects28.
The absence of an association between corticosteroid use and dyspnea in our study aligns with previous findings29. Similarly, no relationships were observed between dyspnea and the duration of medications typically used during critical illness, such as fentanyl, midazolam, norepinephrine, or neuromuscular blockers, which are commonly associated with COVID-19 severity.
Our findings suggest a potential link between neuroleptic use during COVID-19 hospitalization and dyspnea, as measured by the mMRC Scale. Future research should include additional assessments, such as diffusion capacity tests, imaging studies, and exercise tests, to evaluate the multidimensional nature of dyspnea and further investigate its underlying mechanisms.
Patients experiencing dyspnea 12 months post-COVID exhibit significant physical and mental health dysfunctions, which may contribute to and exacerbate their breathlessness. Reduced quality of life in post-COVID patients has been well-documented30, and our results suggest that dyspnea plays a significant role in this impairment. These findings underscore the importance of a patient-centered approach to identifying and treating comorbidities, such as anxiety, depression, and muscle weakness, that may alleviate dyspnea and improve overall outcomes. However, addressing these comorbidities was beyond the scope of this study.
The strengths of our study include its longitudinal design with a long follow-up period, comprehensive data collection during hospitalization, and a high proportion of patients admitted to the ICU.
However, several limitations must be acknowledged. First, the moderate response rate at 12 months could introduce selection bias. Nonetheless, no significant differences were observed between follow-up participants and those lost to follow-up in terms of key baseline and hospitalization parameters.
Second, delirium was not systematically measured during ICU stays, making it possible that the effect attributed to neuroleptics could be confounded by delirium. However, the dose-response relationship observed and the lack of association between dyspnea and other pharmacological risk factors for delirium, such as midazolam, suggest an independent effect of neuroleptics.
Third, this single-center study focused on patients hospitalized during the early stages of the pandemic. Thus, the findings may not fully extend to patients infected with later SARS-CoV-2 variants. Nonetheless, as the largest university hospital in Brazil, our center serves a diverse population of approximately 21 million people in the São Paulo metropolitan region, providing broad generalizability9.
Fourth, as with most post-COVID follow-up studies, self-reported comorbidities and health outcomes may introduce information bias.
Finally, we did not exclude patients with pre-existing pulmonary diseases, though only 3% of participants reported such conditions. While undiagnosed pulmonary diseases could potentially influence the results, their impact is likely negligible.
In conclusion, our study highlights an important association between neuroleptic use during COVID-19 hospitalization and the persistence of dyspnea in long-term survivors. These findings warrant further investigation and emphasize the importance of considering alternative treatments for ICU delirium to minimize potential adverse effects.
Conclusions
Patients with long-term COVID exhibit a high prevalence of limiting dyspnea, which cannot be solely attributed to the severity of the acute illness. The total dose of neuroleptics administered during hospitalization was independently associated with the occurrence of dyspnea 1 month after discharge. At 12 months, patients who continued to experience dyspnea also presented with multiple physical and mental health disorders. These findings highlight the necessity of comprehensive evaluation and management strategies to address the burden of symptoms associated with long-term COVID and improve patient outcomes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
14 April 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41598-025-97754-1
Abbreviations
- mMRC:
-
Modified British Medical Research Council
- WHO:
-
World Health Organization
- ARDS:
-
Acute respiratory distress syndrome
- HCFMUSP:
-
Hospital das clínicas da Faculdade de Medicina da Universidade de São Paulo
- HADS:
-
Hospital Anxiety and Depression Scale
- SpO2:
-
Peripheral oxygen saturation
- IQR:
-
Interquartile range
- HRQoL:
-
Health-related quality of life
- ICU:
-
Intensive care unit
- OR:
-
Odds ratio
- CFS:
-
Clinical frailty scale
- VAS:
-
Visual analogue scale
- FVC:
-
Forced Vital Capacity
References
OMS. Living guidance for clinical management of COVID-19 [Internet]. www.who.int. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2
National Institute for Health and Care Excellence. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19. (2022). Available from: https://www.nice.org.uk/guidance/ng188/resources/covid19-rapid-guideline-managing-the-longterm-effects-of-covid19-pdf-51035515742
Huang, L. et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: A longitudinal cohort study. Lancet Respiratory Med. ; (2022).
Desai, A. D., Lavelle, M., Boursiquot, B. C. & Wan, E. Y. Long-term complications of COVID-19. Am. J. Physiology-Cell Physiol. 322 (1), C1–11 (2022).
Deana, C. et al. Insights into neurological dysfunction of critically ill COVID-19 patients. Trends Anaesth. Crit. Care. 36, 30–38 (2021).
Phetsouphanh, C. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 23 (2), 210–216 (2022).
Amato, M. B. P. et al. Driving pressure and survival in the acute respiratory distress syndrome. N. Engl. J. Med. 372 (8), 747–755 (2015).
Toufen Junior, C. et al. Driving pressure and long-term outcomes in moderate/severe acute respiratory distress syndrome. Ann. Intensiv. Care. ;8(1). (2018).
Ferreira, J. C. et al. Protective ventilation and outcomes of critically ill patients with COVID-19: A cohort study. Ann. Intensiv. Care. 11 (1), 92 (2021).
Zheng, B. et al. Prevalence, risk factors and treatments for post-COVID-19 breathlessness: A systematic review and meta-analysis. Eur. Respiratory Rev. 31 (166), 220071 (2022).
de Godoy, C. G. et al. e, da, Protocol for Functional Assessment of Adults and Older Adults after Hospitalization for COVID-19. Clinics. ;76:e3030. (2021).
Mahler, D. A. & Wells, C. K. Evaluation of clinical methods for rating dyspnea. Chest 93 (3), 580–586 (1988).
Rodrigues, M. K., Nunes Rodrigues, I., de Pinto, S. & Oliveira, J. M. Vasconcelos Gomes da Silva DJ, MF. Clinical Frailty Scale: translation and cultural adaptation into the Brazilian Portuguese language. Journal of Frailty & Aging. ;10(1):1–6. (2020).
Olssøn, I., Mykletun, A. & Dahl, A. A. The hospital anxiety and depression rating scale: A cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry ;5(1). (2005).
Xie, F., Gaebel, K., Perampaladas, K., Doble, B. & Pullenayegum, E. Comparing EQ-5D valuation studies. Med. Decis. Making. 34 (1), 8–20 (2013).
Turan, Z. et al. Medical Research Council-sumscore: A tool for evaluating muscle weakness in patients with post-intensive care syndrome. Critical Care. 24(1).,
The 1-minute sit-to-stand test to detect exercise-induced oxygen desaturation in patients with interstitial lung disease. Therapeutic Advances in Respiratory Disease. 2018;12:175346661879302. (2020)
Becker, D. E. Basic and clinical pharmacology of glucocorticosteroids. Anesth. Prog. 60 (1), 25–32 (2013).
Leucht, S. et al. Dose equivalents for Second-Generation antipsychotic drugs: the classical mean dose method. Schizophr. Bull. 41 (6), 1397–1402 (2015).
Laviolette, L. & Laveneziana, P. Dyspnoea: A multidimensional and multidisciplinary approach. Eur. Respir. J. 43 (6), 1750–1762 (2014).
Ribeiro Carvalho, C. R. et al. Long-term respiratory follow-up of ICU hospitalized COVID-19 patients: Prospective cohort study. Kou YR, editor. PLOS ONE. ;18(1):e0280567. (2023).
Carvalho, C. R. R. et al. Post-COVID-19 respiratory sequelae two years after hospitalization: An ambidirectional study. Lancet Reg. Health Americas. 33, 100733–100733 (2024).
Singh, S. et al. Respiratory sequelae of COVID-19: pulmonary and extrapulmonary origins, and approaches to clinical care and rehabilitation. Lancet Respiratory Med. (2023).
Bernard-Valnet, R. et al. Delirium in adults with COVID-19–Related acute respiratory distress syndrome. Neurology 99 (20), e2326–e2335 (2022).
Hawkins, M. et al. A rapid review of the pathoetiology, presentation, and management of delirium in adults with COVID-19. J. Psychosom. Res. 141, 110350 (2021).
Ostuzzi, G. et al. Pharmacological treatment of hyperactive delirium in people with COVID-19: Rethinking conventional approaches. Therapeutic Adv. Psychopharmacol. 10, 204512532094270 (2020).
Ostuzzi, G. et al. Safety of psychotropic medications in people with COVID-19: evidence review and practical recommendations. BMC Med. ;18(1). (2020).
Kim, M. S. et al. Comparative efficacy and acceptability of Pharmacological interventions for the treatment and prevention of delirium: A systematic review and network meta-analysis. J. Psychiatr. Res. 125, 164–176 (2020).
Chan Sui Ko, A. et al. No impact of corticosteroid use during the acute phase on persistent symptoms Post-COVID-19. Int. J. Gen. Med. 15, 6645–6651 (2022).
Deana, C. et al. Quality of life in COVID-Related ARDS patients one year after intensive care discharge (Odissea Study): A Multicenter Observational Study. J. Clin. Med. 12 (3), 1058–1058 (2023).
Acknowledgements
We are grateful for the assistance given by Luciana Cassimiro Nóbrega, Vinicius Iamonti, Vivian Vieira Tenorio Sales, Caroline Gil de Godoy, Erika Christina Gouveia e Silva, Danielle Brancolini de Oliveira in acquired the study data.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
CTJ designed the work, acquired, analyzed, interpreted the data for the work and drafted the work. GC designed the work, acquired, interpreted the data for the work and critically revised the work. JEP designed the work, acquired, interpreted the data for the work and critically revised the work. CRFC designed the work, acquired, interpreted the data for the work and critically revised the work. CRRC designed the work, interpreted the data for the work and critically revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved by the Ethics Committee for the Analysis of Research Projects of the HCFMUSP (approval number: 31942020.0.0000.0068). All individuals consent to participate in this study and sign the informed consent form.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in Affiliation 1, which was incorrectly given as ‘Division of Pulmonary Medicine, Heart Institute, Hospital das Clinicas HCFMUSP, Faculdade de medicina, Universidade de Sao Paulo, Sao Paulo, SP, Brazil’. The correct affiliation is listed here: Divisao de Pneumologia, Instituto do Coracao (InCor), Hospital das Clinicas HCFMUSP, Faculdade de medicina, Universidade de Sao Paulo, Sao Paulo, SP, Brazil.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Toufen, C., de Almeida, G.C., Pompeu, J.E. et al. Neuroleptics used in critical COVID associated with moderate-severe dyspnea after hospital discharge. Sci Rep 15, 6744 (2025). https://doi.org/10.1038/s41598-025-91010-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91010-2