Abstract
To explore the additional value of shear wave elastography (SWE) in chronic obstructive pulmonary disease (COPD) patients. Ultrasound elastography of the rectus femoris and patellar tendon was performed to determine the mean elasticity index (SWEmean) of the rectus femoris (SWERF) and patellar tendon (SWEPT) in 56 patients with COPD and 53 healthy controls. Clinical tests included the COPD Assessment Test (CAT), the dyspnea index score (modified British Medical Research Council (mMRC)score), the Five-Repetition Sit-to-Stand Test(5STS) and the Six-Minute Walk Test (6MWT). We compared differences in SWEmean between healthy controls and COPD patients while describing the correlation between SWEmean and clinical tests in COPD patients. Both the intra-observer and inter-observer repeatability of SWE performance were excellent (all correlation coefficients > 0.75; p < 0.05). There was a statistically significant difference between healthy controls and COPD patients in the SWERF and SWEPT between healthy controls and COPD patients (p < 0.001). The COPD patients had smaller SWERF and larger SWEPT than healthy controls. The SWERF was positively correlated with the 6MWT (r = 0.591, p < 0.001), and negatively related to the mMRC (r = − 0.794, p < 0.001), CAT (r = − 0.894, p < 0.001) and 5STS (r = − 0.928, p < 0.001). But the SWEPT was positively related to the 6MWT (r = 0.269, p < 0.05), mMRC (r = 0.398, p < 0.05), CAT (r = 0.377, p < 0.05) and 5STS (r = 0.332, p < 0.05). SWEmean of COPD patients was statisticant, different from that of healthy controls, and associated with clinical tests. SWE was a simple and feasible tool for reflecting the lower limb dysfunction in patients with COPD.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable condition characterized by persistent respiratory symptoms and progressive airflow obstruction1. Quadriceps dysfunction was demonstrable in one-third of COPD patients2 and negatively affected the quality of life, morbidity, and mortality3. Previous biochemical and histological studies of the quadriceps femoris muscle in COPD patients had shown that its dysfunction was caused by oxidative stress, metabolic derangements, and changes in the type of muscle fibers4. Various clinical tests, including the Six-Minute Walk Test (6MWT), the Five-Repetition Sit-to-Stand Test (5STS), the COPD Assessment Test (CAT), and the modified British Medical Research Council score (mMRC), were performed to reflect the skeletal muscle dysfunction of COPD patients. Previous studies3 have shown that skeletal muscle dysfunction can increase the patient’s respiratory distress index score [modified Medical Research Council (mMRC) score], decreased exercise tolerance, decreased exercise ability, and reduced activity. Therefore, early identification and intervention of skeletal muscle dysfunction in COPD patients is essential for improving their quality of life and disease prognosis.
SWE is a simple and novel ultrasonic technique that obtains the SWE value by transmitting and tracking shear waves, reflecting the stiffness of the test tissue5. Our previous study6 applied SWE to the stiffness of the quadriceps in COPD patients, representing its clinical application potential in COPD patients. Anatomically, the patellar tendon is attached directly to the quadriceps femoris, jointly completing functions such as maintaining joint stability and knee extension movement. Among the four muscles of the quadriceps femoris, the rectus femoris plays a major role in performing related functions. Previous studies7,8 have shown that the patellar tendon mechanical properties and quadriceps femoris muscle strength were closely related and interacted.
In this study, SWE was introduced to explore the changes in SWE values of rectus femoris and patellar tendon between healthy controls and COPD patients. Meanwhile, the potential value of SWE in clinical parctice was explored by comparing SWE values with clinical tests.
Materials and methods
Participants
From August 2021 to February 2022, 56 COPD patients from the Department of Respiratory of the Chengdu First People’s Hospital were recruited as the COPD group, and 53 healthy people from health management center of the Chengdu First People’s Hospital were matched as the healthy controls. The inclusion criterion was a diagnosis of stable COPD based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria1. The exclusion criteria were described below: Patients with bronchial asthma, bronchiectasis, pulmonary tuberculosis, interstitial lung disease, lung cancer, pulmonary embolism and other lung lesions; Patients suffering from stroke, heart failure, coronary heart disease, hyperthyroidism or hypothyroidism, myasthenia gravis, malignant tumors and other conditions that may affect lower limb function; Patients with a history of acute COPD episodes or glucocorticoid use within 6 months; Patients with history of lower limb trauma or surgery; Athletes or chronic manual workers. This study was approved by the Research Ethics Committee of The Chengdu First People’s Hospital (2022,YNYJ,014).
Measurements of the SWE value
A 4-15MHZ linear array transducer and the Aixplorer ultrasound scanning system(SuperSonic Imagine, France), which is equipped with conventional two-dimensional ultrasonic function and SWE function, were used in this study. Ultrasonography was performed according to the methods of previous studies6. Conventional two-dimensional ultrasound was used to determine the course of muscles and tendons and to locate the rectus femoris and patellar tendons. Then, the SWE function was performed to measure the SWE value of the rectus femoris and patellar tendon (Fig. 1). Repeated measures five times to take the average for further analysis.
Measurement of the SWE value of rectus femoris and patellar tendon between healthy controls and COPD patients. (A) Conventional two-dimensional ultrasound image of the quadriceps femoris. (B) Measurement of the SWE value of rectus femoris in healthy controls. (C) Measurement of the SWE value of rectus femoris in COPD patients. (D) Conventional two-dimensional ultrasound image of patellar tendon. (E) Measurement of the SWE value of patellar tendon in healthy controls. (F) Measurement of the SWE value of patellar tendon in COPD patients.
Assessment of physical performance (clinical tests)
-
1.
The Assessment of Dyspnea Index Score (Modified British Medical Research Council (mMRC) Score)
Applying the modified Chinese mMRC scale9, according to the condition under which the patient developed dyspnea symptoms, the degree of dyspnea in COPD patients was divided into five grades. From grade 0 to 4, the degree of dyspnea worsened.
-
2.
COPD Assessment Test (CAT)
According to the Chinese version of the COPD assessment test10, the severity of the disease and the health status of the patient were reflected by assessing the patient’s cough, expectoration, chest tightness, difficulty climbing mountains/stairs, limited home activity, confidence in going out, sleep, and energy.
-
3.
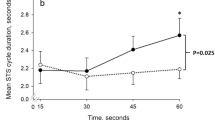
Five-Repetition Sit-to-Stand Test (5STS)
All COPD patients were participated in the 5STS and performed according to the method11. And recorded the time required to complete the experiment. The participant had a one-minute break between each test. Each test was repeated three times and the average of the three times was calculated.
-
4.
Six-Minute Walk Test (6MWT)
COPD patients should undergo 6MWT according to the American Thoracic Society (ATS)12 guidelines. They can slow down or stop to rest when they have shortness of breath, chest pain, or dizziness. If the above symptoms are aggravated and not relieved after rest, the test should be stopped immediately. After the test, the total walking distance of the tester was recorded in meters.
Statistical analyses
The rank sum test was used to compare the differences of SWE values between healthy controls and COPD patients, and p < 0.05 was considered statistically significant. Spearman correlation coefficiens was used to analyze the correlations between SWE value and physical performance in COPD patients. Intraclass correlation coefficient (ICC) test and Bland–Altman Plot were used to calculate intra-and inter-observer reliability. ICC was explained based on relevant guidelines: < 0.40, poor reliability; 0.40–0.75, for fair to good reliability; and > 0.75 for excellent reliability13.
Results
Basic characteristics
In this study introduced 56 COPD patients and 53 matched healthy people. None of the participants had hypertension, diabetes mellitus, stroke, heart failure, coronary heart disease, hyperthyroidism or hypothyroidism, myasthenia gravis, or malignant tumors, nor had a history of lower limb trauma or surgery. Patients in the COPD group were free of exacerbations in the previous six months. There was no significant difference in gender, age, height, weight and BMI between COPD patients and healthy controls, and the results are shown in Table 1.
Reliability and repeatability levels of SWE measurements
The intra-examiner and inter-examiner reliability of SWE in assessing rectus femoris and patellar tendon stiffness was excellent in 56 COPD patients and 53 controls (ICC > 0.75), as shown in Table 2 and Fig. 2.
Inter-examiner and intra-examiner concordance analysis of rectus femoris and patellar tendon in COPD patients. (A) Inter-examiner concordance analysis in rectus femoris in COPD patients. (B) Intra-examiner concordance analysis in rectus femoris in COPD patients. (C) Inter-examiner concordance analysis in patellar tendon in COPD patients. (D) Intra-examiner concordance analysis in patellar tendon in COPD patients.
Comparison of SWE values of rectus femoris and patellar tendon between COPD group and healthy control group
Compare with healthy controls, the COPD patients had smaller SWE values in the rectus femoris and larger SWE values in the patellar tendon (Fig. 3), and the difference is statistically significant (p < 0.05) (Table 3).
Correlation between physical performance and SWE values of retus femoris and patellar tendon in COPD group
According to Table 4, in COPD patients, the SWERF was positively correlated with 6MWT (r = 0.591, p < 0.001), and negatively related to mMRC (r = − 0.794, p < 0.001), CAT (r = − 0.894, p < 0.001) and 5STS (r = − 0.928, p < 0.001), and the SWEPT was positively related to 6MWT (r = 0.269, p < 0.05), mMRC (r = 0.398, p < 0.05), CAT (r = 0.377, p < 0.05) and 5STS (r = 0.332, p < 0.05) (Fig. 4).
Correlation between physical performance and SWERF, SWEPT in COPD patients. (A) Correlation between CAT and SWERF. (B) Correlation between mMRC and SWERF. (C) Correlation between 5STS and SWERF. (D) Correlation between 6MWT and SWERF. (E) Correlation between CAT and SWEPT. (F) Correlation between mMRC and SWEPT. (G) Correlation between 5STS and SWEPT (H) Correlation between 6MWT and SWEPT (SWERF, SWE value of rectus femoris; SWEPT, SWE value of patellar tendon; mMRC, Modified British Medical Research Council Score; CAT, COPD assessment test; 6MWT, six-minute walk test; 5STS, five-repetition sit-to-stand test).
Discussion
COPD can cause limb muscle dysfunction, which is closely related to physical activity, exercise endurance, quality of life, and even survival14. As one of the vital muscle groups in the human body, the quadriceps femoris (especially rectus femoris) plays an crucial role in knee extension, maintaining upright posture, and other functions. Patellar tendon is closely related to the rectus femoris in anatomy and function. Therefore, rectus femoris and patellar tendon were considered study subjects this time.
The SWE was chosen for this study because it has recently been increasingly used in soft-tissue15, tendons16 and musculoskeletal system17 and can reflect real-time visualization of muscle stiffness distribution18. We first tested the reliability and repeatability levels of SWE measurements, and results showed good between healthy controls and COPD patients, consistent with previous studies19. Therefore, SWE can be a reliable and reproducible tool for measuring the rectus femoris and patellar tendon stiffness.
Results of this study showed that compared with healthy controls, the SWERF in COPD patients was decreased, and the SWEPT was increased, which performed the same trend in muscle and tendon stiffness of disease associated with lower limb dysfunction such as GNE-related myopathy20, idiopathic inflammatory myopathies21, myositis22, Parkinson’s disease23, patellar tendinopathy 24,25 and so on. In this study, the rectus femoris and patellar tendon were regarded as a musculoarticular system to explore whether changes in SWE of the lower limb musculoarticular system in COPD patients reflect lower limb dysfunction. To our knowledge, no previous studies have investigated the changes in the SWE value of the musculoarticular system in COPD patients using SWE, highlighting the importance of our work.
Some clinical tests were used to reflect the physical performance of COPD patients. The patient’s muscular endurance was assessed by 6MWT26, the muscle strength was reflected by 5STS27, and mMRC and CAT28 evaluated the patient’s overall health condition. Results of this study showed that the SWERF of COPD patients was positively correlated with 6MWT and negatively related to mMRC, CAT, and 5STS. Still, the SWEPT was negatively correlated with 6MWT and positively related to mMRC, CAT, and 5STS. Patients with COPD had smaller SWERF and larger SWEPT than healthy controls. In other words, When lower limb muscle function is reduced, the 6MWT distance decreases, and the required time of 5STS, the CAT, and the mMRC scores increase, which is the same trend as the clinical experimental results caused by SWE changes in the rectus femoris and patellar tendon in this study. We believe that the changes in SWE value in the musculoarticular system observed in the current work provide novel insights into the comprehension and interpretation of motor dysfunctions associated with COPD. That means SWE changes in the musculoarticular system in COPD patients can reflect lower limb dysfunction.
Limitations of this study include: Firstly, previous studies29,30 have shown that knee joint angle can affect SWE values of the lower limb musculoarticular system, but the SWE values were measured only at a fixed knee angle. In future studies on SWE of the lower limb musculoarticular system, measurement of SWE values at different knee angles is needed as a study subject. Secondly, our study did not include a gold standard approach to measuring lower limb muscle strength, which would allow direct comparison to SWE value. Thirdly, referring to methods of previous research31,32, SWE values of the patellar tendon were measured only at one point in this study. The consistency of SWE values of patellar tendons in different parts has not been determined, and further investigation is needed to address this issue. Fourthly, this study has several methodological limitations requiring acknowledgment. The primary constraints include limited sample size and demographic homogeneity, with the cohort predominantly comprising clinically stable COPD patients aged approximately 60 years. Furthermore, potential measurement variability in outcome assessments may introduce cumulative error propagation. These combined methodological factors could amplify observed correlation coefficients between SWERF and other clinical parameters. To address these limitations, we will further validate the experimental findings by expanding the sample size, performing balanced matching of the included population, and exploring the correlations in COPD patients at different stages.
Conclusion
Changes in SWE values of the lower limb musculoarticular system in COPD patients can reflect lower limb dysfunction.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- SWE:
-
Shear wave elastography
- COPD:
-
Chronic obstructive pulmonary disease
- SWEmean:
-
The mean elasticity inde
- SWERF :
-
SWE value of rectus femoris
- SWEPT :
-
SWE value of patellar tendon
- mMRC:
-
Modified British Medical Research Council Score
- CAT:
-
COPD assessment test
- 6MWT:
-
Six-minute walk test
- 5STS:
-
Five-repetition sit-to-stand test
References
Labaki, W. W. & Rosenberg, S. R. Chronic obstructive pulmonary disease. Ann. Intern. Med. 173(3), 17–32 (2020).
Seymour, J. M. et al. The prevalence of quadriceps weakness in COPD and the relationship with disease severity. Eur. Respir. J. 36(1), 81–88 (2010).
Abdulai, R. M. et al. Deterioration of limb muscle function during acute exacerbation of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 197(4), 433–449 (2018).
Barreiro, E. & Gea, J. Molecular and biological pathways of skeletal muscle dysfunction in chronic obstructive pulmonary disease. Chronic Respir. Dis. 13(3), 297–311 (2016).
Creze, M. et al. Shear wave sonoelastography of skeletal muscle: Basic principles, biomechanical concepts, clinical applications, and future perspectives. Skelet. Radiol. 47(4), 457–471 (2018).
Niu, Y. et al. SWEmean of quadriceps, a potential index of complication evaluation to patients with chronic obstructive pulmonary disease. Int. J. Chronic Obstruct. Pulm. Dis. 17, 1921–1928 (2022).
Massey, G. J., Balshaw, T. G., Maden-Wilkinson, T. M., Tillin, N. A. & Folland, J. P. The influence of patellar tendon and muscle-tendon unit stiffness on quadriceps explosive strength in man. Exp. Physiol. 102(4), 448–461 (2017).
Tas, S. et al. Patellar tendon mechanical properties change with gender, body mass index and quadriceps femoris muscle strength. Acta Orthop. Traumatol. Turc. 51(1), 54–59 (2017).
Cui, L. et al. Role of inspiratory capacity on dyspnea evaluation in COPD with or without emphysematous lesions: A pilot study. Int. J. Chronic Obstruct. Pulm. Dis. 12, 2823–2830 (2017).
Zhou, Q. T. et al. Chronic obstructive pulmonary disease assessment test score correlated with dyspnea score in a large sample of Chinese patients. Chin. Med. J (Engl.) 126(1), 11–15 (2013).
Jones, S. E. et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax. 68(11), 1015–1020 (2013).
Laboratories ACoPSfCPF. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 166, 111–117 (2002).
Fleiss PESaJL. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 86, 420–428 (1979).
Maltais, F. et al. An official American Thoracic Society/European Respiratory Society statement: Update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 189(9), e15-62 (2014).
Arda, K., Ciledag, N., Aktas, E., Aribas, B. K. & Kose, K. Quantitative assessment of normal soft-tissue elasticity using shear-wave ultrasound elastography. AJR Am. J. Roentgenol. 197(3), 532–536 (2011).
Cortes, D. H., Suydam, S. M., Silbernagel, K. G., Buchanan, T. S. & Elliott, D. M. Continuous shear wave elastography: A new method to measure viscoelastic properties of tendons in vivo. Ultrasound Med. Biol. 41(6), 1518–1529 (2015).
Drakonaki, E. E., Allen, G. M. & Wilson, D. J. Ultrasound elastography for musculoskeletal applications. Br. J. Radiol. 85(1019), 1435–1445 (2012).
Shinohara, M., Sabra, K., Gennisson, J. L., Fink, M. & Tanter, M. Real-time visualization of muscle stiffness distribution with ultrasound shear wave imaging during muscle contraction. Muscle Nerve 42(3), 438–441 (2010).
Tas, S., Onur, M. R., Yilmaz, S., Soylu, A. R. & Korkusuz, F. Shear wave elastography is a reliable and repeatable method for measuring the elastic modulus of the rectus femoris muscle and patellar tendon. J. Ultrasound Med. 36(3), 565–570 (2017).
Carpenter, E. L., Lau, H. A., Kolodny, E. H. & Adler, R. S. Skeletal muscle in healthy subjects versus those with GNE-related myopathy: Evaluation with shear-wave US–A pilot study. J. Radiol. 277(2), 546–554 (2015).
Alfuraih, A. M. et al. Muscle shear wave elastography in idiopathic inflammatory myopathies: A case–control study with MRI correlation. Skelet. Radiol. 48(8), 1209–1219 (2019).
Botar-Jid, C. et al. The contribution of ultrasonography and sonoelastography in assessment of myositis. Med. Ultrason. 12(2), 120–126 (2010).
Gao, J. et al. Ultrasound strain elastography in assessment of resting biceps brachii muscle stiffness in patients with Parkinson’s disease: A primary observation. Clin. Imaging. 40(3), 440–444 (2016).
Zhang, C., Duan, L., Liu, Q. & Zhang, W. Application of shear wave elastography and B-mode ultrasound in patellar tendinopathy after extracorporeal shockwave therapy. J. Med. Ultrason. 47(3), 469–476 (2019).
Zhang, Z. J., Ng, G. Y., Lee, W. C. & Fu, S. N. Changes in morphological and elastic properties of patellar tendon in athletes with unilateral patellar tendinopathy and their relationships with pain and functional disability. PLoS One. 9(10), e108337 (2014).
Chen, S., Sierra, S., Shin, Y. & Goldman, M. D. Gait speed trajectory during the six-minute walk test in multiple sclerosis: A measure of walking endurance. Front. Neurol. 12, 698599 (2021).
Mentiplay, B. F., Clark, R. A., Bower, K. J., Williams, G. & Pua, Y. H. Five times sit-to-stand following stroke: Relationship with strength and balance. Gait Posture. 78, 35–39 (2020).
Jones, P. W. et al. Development and first validation of the COPD assessment test. Eur. Respir. J. 34(3), 648–654 (2009).
Kuervers, E. J., Firminger, C. R. & Edwards, W. B. Effect of knee angle and quadriceps muscle force on shear-wave elastography measurements at the patellar tendon. Ultrasound Med Biol. 47(8), 2167–2175 (2021).
Ebihara, B., Mutsuzaki, H. & Fukaya, T. Relationships between quadriceps tendon elasticity and knee flexion angle in young healthy adults. Medicina (Kaunas). 55(2), 53 (2019).
Dickson, D. M., Fawole, H. O., Newcombe, L., Smith, S. L. & Hendry, G. J. Reliability of ultrasound strain elastography in the assessment of the quadriceps and patellar tendon in healthy adults. Ultrasound. 27(4), 252–261 (2019).
Porta, F., Damjanov, N., Galluccio, F., Iagnocco, A. & Matucci-Cerinic, M. Ultrasound elastography is a reproducible and feasible tool for the evaluation of the patellar tendon in healthy subjects. Int. J. Rheum. Dis. 17(7), 762–766 (2014).
Acknowledgements
The authors express gratitude to all the participants of this study and to department of Respiratory and Health management of the Chengdu First people’s Hospital.
Funding
This work was supported by the Youth Innovation Project of Sichuan Medical Association 2024(Q23054).
Author information
Authors and Affiliations
Contributions
Concept and study design: C.C. Data collection and analyses: L.X and ZC.C. Draf preparation and revision: YY.Y, YF.N, W.T and ST. L. Draf review and editing: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yue, Y., Niu, Y., Tang, W. et al. Shear wave elastography, as a feasible tool, can be used to reflect the lower limb dysfunction in patients with chronic obstructive pulmonary disease?. Sci Rep 15, 6532 (2025). https://doi.org/10.1038/s41598-025-91082-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91082-0