Abstract
How professionals communicate during medical procedures may have a significant impact on children and adolescents’ pain. Rel@x is a manualized training program designed to develop hypnosis-derived communication skills to mitigate childhood pain and distress. The study aimed to evaluate if this training was associated with an improvement and maintenance in communication skills over time, and measure associations between changes and participants’ characteristics. A 9-hour training in hypnosis-derived communication was offered to 78 volunteer healthcare professionals from a tertiary pediatric hospital, and 58 participated in the evaluative study. Participants were evaluated at baseline, immediately after training, and 5 months later (39 ± 10 yrs, 52 women, 54 nurses). We used a video-recorded standardized simulation protocol of blood draw and coded the participants’ interactions with the pre-validated Sainte-Justine Hypnotic Communication Assessment Scale (SJ-HCAS) assessing relational, technical, and total skills. We modeled pre-post-follow-up changes over time with latent growth curve models. Satisfaction with Rel@x was consistently excellent (97%). Across the 3 domains, we observed significant improvements of total (+ 61%, 95% CI 53–69%), relational (+ 27%, 95% CI 20–34%), and technical skills (+ 124%, 95% CI 08–140%). Post-training competence levels were 73–91% across domains. A large proportion of acquired skills were maintained at 5 months (55–75%) suggesting a significant effect of the training. Sensitivity analyses confirmed these results (best-case/worst-case skill maintenance ratio: 59–79%/49–73%). Larger improvements in technical skills were associated with younger age and lower baseline skills of participants. The Rel@x training is associated with improved skills in hypnotic communication post-training and at follow-up. This simulation study paves the way for future efficacy studies to examine the effect of hypnotic communication on real patients’ pain and distress.
Similar content being viewed by others
Introduction
Procedural pain management has been recognized as a significant issue in paediatrics1. The exposure to painful procedures, especially when repeated, has a major impact on the quality of life of youth during treatment2,3 and in the long term4,5. Distressing and painful medical experiences may lead to fear and anxiety towards future medical care6, and thus contribute to avoidance and even loss of follow-up as youth transition into the adult health care system, with increased potential risk for adverse events5.
To deal with procedural pain, paediatric healthcare teams can use pharmacological interventions such as local anesthetics7, as well as non-pharmacological strategies such as distraction8,9. In addition, the way healthcare providers (HCPs) communicate with youth and their caregivers may be key to the global experience of procedural pain10. Hypnosis-derived communication (HC) typically involves guided imagery combined with verbal suggestion and calls for a set of simple and concrete principles to be applied when performing a painful procedure11,12. The practice of HC is supported by a body of empirical studies suggesting beneficial effects of clinical hypnosis on pain13,14,15,16,17,18,19,20 and is easily applicable within care (see clinical illustration of the Magic Glove technique21). As compared to other non-pharmacological strategies, HC is transportable, easily applicable in varied and unplanned contexts, mainly using the child’s imagination and the language of an HCP without requiring any additional support material or the intervention of another professional22,23,24.
Recent advances in this field include the measurement of HC25 and successful feasibility tests of training professionals in hematology-oncology clinics26. Researchers have also collected encouraging data suggesting that professionals’ HC behaviors could benefit patients27. In line with guidelines on the development of behavioral interventions28, this led to a define-refine study of a manualized training, designed to train HCPs to use hypnotic communication skills while performing a painful procedure: the Rel@x training29.
The aim of this study was to evaluate the ability of the Rel@x training program to develop HC competences in paediatric healthcare professionals. We addressed these specific questions: (1) Do HC communication skills significantly improve with Rel@x? (2) If so, is this improvement maintained over time? (3) Are improvements associated with baseline levels, the selected technique and professional individual descriptors? Finally, participants’ satisfaction with the training was assessed.
Methods
Study design
A pre-post intervention study was conducted to evaluate Rel@x that was offered to HCPs practicing at a large, university- affiliated, tertiary care pediatric Canadian hospital (Phase IIb ORBIT28). Ethical approval was granted by the CHU Sainte-Justine Research Ethics Board (#2019–2205) and the research was conducted according to the principles expressed in the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardian(s). The reporting of this study is compliant with the TREND Statement30. Clinical trial number: not applicable.
Participants
To be included in this study, HCPs were required to (1) work primarily at the study pediatric hospital site, (2) volunteer to register to the Rel@x training, (3) have a routine clinical activity involving venipunctures with children or be comfortable in performing a venipuncture. We excluded participants with previous training in hypnosis-derived techniques. No other exclusion criteria were established. We advertised the training among nurses but included all HCPs interested in the training.
Procedure
Professionals were approached in three departments of the hospital: hematology-oncology, emergency, general pediatrics. Yet, to encourage uptake for future projects we decided to accept participants from other departments who heard about the training from word-of-mouth (Fig. 1). We presented the project in staff meetings, in several ad hoc meetings with the nursing management and physicians, and advertised the project in the hospital nurse journal (this was also used three times to regularly inform HCPs on the progress of the study). Interested individuals were asked to contact the study coordinator (ER) to get full information on the training and the evaluation procedure. Participants were asked to select one of two techniques of their choice (see training). Participants were then directed to an electronic consent form and a short online sociodemographic questionnaire. Those who consented were then put on a waitlist until a group was ready to be trained and dates were set for the two Rel@x sessions.
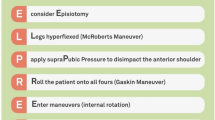
Training
The Rel@x training consists of a two-half-day, in-person, training for a total of 9 h including competence assessment. Full details on the training are available publicly29,31. In brief, the first session is centered on relational skills and aims to provide an accurate knowledge of HC based on the evidence and clinical practice. Also, strategies for synchronizing the professional-patient relationship, reframing the verbal content, and suggesting direct and metaphorical medical content, are reviewed12. The session ends with the HCP being presented the two evidence-based techniques to practice: (1) A pleasant place the youth imagines visiting using their five senses32 and (2) A magic glove the youth imagines using to protect their arm32,33,34. The second session focuses on the technique previously chosen by the participant (i.e. Magic Glove or Pleasant Place). It begins one to two weeks after the first session. The session is centered on learning to use simple language derived from clinical hypnosis and detecting desired changes in the child to monitor communication during the encounter. This session further provides an opportunity to learn, practice, and apply the chosen technique. Scripts are offered, which HCPs are encouraged to adapt in their own words for future use. These techniques standardize the HC method during medical procedures. At the end of the second session, a link is provided to an e-learning module to help review and reinforce the principles and illustrate the techniques with additional videos. Rel@x is available in French and English31. The training is designed to be provided by an HCP with advanced training in clinical hypnosis and an assistant clinician. The Rel@x training is also accredited for continuing education by the Quebec Professional Nurse Board (Ordre des Infirmières et Infirmiers du Québec, OIIQ).
In the present study, we trained 13 groups of HCPs (n = 3–10, median = 6 participants/group), from May 13, 2021 to March 23, 2023. Session #2 took place a median of 14 days after session #1. All groups were trained in-person in a meeting room of the hematology-oncology clinic. For the present study, nurse participants were compensated overtime for their participation (9 h). Training was provided by a certified psychologist and hypnotherapist (DO) and an assistant with hypnosis training (JA), both with a PhD in psychology.
Evaluation procedure
We video-recorded encounters of professionals performing a venipuncture in a simulation situation involving an actor equipped with a standard venipuncture arm (Limbs and Things®) (Fig. 2, see declaration ‘Consent to publish’ at the end of the manuscript). The videos were acquired in a dedicated room at the hematology-oncology clinic, at three time points: T1 pre-training, T2 post-training and T3 at 5 months follow-up. T1 took place before the first training session (on the same day), with participants being instructed to show up earlier for the baseline evaluation activity. T2 took place right in the minutes following the second session, and T3 was an appointment scheduled approximately 5 months after T2 (median 5.1 months, IQR 4.40–5.55). Although we had planned to organize T3 at 3 months, the burden of the Covid-19 pandemic on HCPs prevented us from respecting this timeline. Participants were compensated $CDN 50 by means of a voucher to be used in a local store after completing T3 evaluations.
The simulation protocol (e.g. a young adolescent girl remembering a picnic in a park with her family, see S1 Appendix35) was developed with two patient partners with experience of procedural pain. Although the context entailed a stressful and fearful patient, the simulation protocol allowed participants to practice their newly acquired skills with an actor reacting positively to the professionals’ behaviors. Actors were selected among psychology undergraduates and trained to strictly follow the simulation protocol. In a subset of 11 participants in the waitlist, we were able to collect an additional one-week baseline point before training using the exact same procedure (see complementary results subsection). During simulations, we played recorded noise from the ward to mimic a busy outpatient clinic, following suggestions provided by participants in a previous qualitative study29.
Measures
Online sociodemographic questionnaire
This questionnaire was completed after consenting. It included the following data: Age, gender, highest level of education, profession, years of practice, years of practice in pediatrics, current department, previous training in communication to mitigate pain.
Primary outcome
The primary outcome was the Sainte-Justine Hypnotic Communication Assessment Scale (SJ-HCAS). This scale was used to assess communication behaviors in video-recorded nurse-patient encounters25. It is based on 11 core items of hypnosis-derived communication to prevent pain and distress in children. For each item, independent raters evaluated whether the behavior was present (1) or absent (0). Two count scores were computed, one on the quality of the relationship (Relation subscore, range 0 to 5) and one on the quality of the communication technique (Technique subscore, range 0 to 6). We used versions of the scale adapted to the Pleasant Place and the Magic Glove techniques (S2 Appendix). A total score was computed by adding all 11 items (Total score, range 0–11). The score can be transformed into a percentage to reflect overall competence. A sample item for the Relation score is: “Language: an effort is made to use a language adapted to the level and life context of the child or adolescent”. A sample item for the Technical score is: “Use of various senses, sensory modalities among sight, hearing, taste, touch, smell: Uses multisensory descriptions and technique-specific images”. In the present study, two independent lay raters blinded to the assessment time-points used the SJ-HCAS to evaluate communication behaviors in HCPs. Raters were undergraduate students completing a research internship. They were trained to use the scale for 2 h using pre-existing recordings from a prior study. They had only basic knowledge on the study objectives and were unaware of the training stage of recordings. We found excellent inter-rater reliability for the Total (ICC = 0.893) and the Technique scores (ICC = 0.938), and fair reliability for the Relation score (ICC = 0.640). The final scores considered for analysis were averaged between raters. A total of n = 168 encounters (T1, T2, and T3) were coded for this project with a limited number of missing data (T2: n = 1, T3: n = 5).
Satisfaction questionnaire
We used an ad hoc satisfaction questionnaire composed of 15 items, each to be answered on a 1 (very little)-4 (very much) scale (S3 Appendix). Sample items are: “The objectives were well defined” and “Teaching methods promoted learning”. The questionnaire was answered in-person (paper-pencil format) after the second training session. The questionnaire was filled once training was completed and handed to the study coordinator, independently from the trainers. In the present project consistency was excellent across satisfaction items with α = 0.783, mean coefficient of variation = 0.07.
Data analyses
We conducted preliminary analyses to ascertain distribution variability in outcomes across time-points using boxplots and calculated the average T1-T2%change and T1-T3%change with their 95%CIs. Following recommendations when missing data are limited (here 3.4%), we used the full-information maximum likelihood estimation method (FIML) to deal with missing data, allowing us to retain all participants36. For the main analyses, we used latent growth curve models (LGCMs)37 to examine changes over time as these are recommended for interventions with sample sizes as small as n = 5038,39. Each LGCM included an intercept and its variance (i.e., the average initial level of the score and inter-individual variations around this average initial level) and a slope and its variance (i.e., the average amount of change across all participants and inter-individual variations around this average level of change).
In the first step of the analysis, we compared two models for each outcome variable (i.e., Total, Relation, Technique). (1) A linear model was estimated, where linear change was expected in the outcome variable over time. (2) A non-linear model was estimated, where a non-linear change was expected in the outcome variable over time. In this model, the first time point was constrained to be 0, the second time point was constrained to be 1, and the third time point was freely estimated. This way, the slope reflected the total amount of change that occurred between T1 and T2, while the freely estimated time point (T3) reflected how much change occurred in T3 compared to the initial change level (T1-T2).
Next, in the second step of the analysis, we added time-invariant predictors of the intercept and the slope (i.e., age, gender, highest level of education, profession, years of practice, years of practice in pediatrics, current department, and technique trained) to examine their potential effect on the initial scores of the outcomes as well as on their change over time. Age, years of practice, years of practice in pediatrics were used as continuous variables, while gender, highest level of education, profession, and current department, were used as categorical variables in the analyses.
Models were evaluated using sample-size independent goodness-of-fit indices: Comparative Fit Index (CFI; ≥ 0.90 adequate; ≥ 0.95 excellent), Tucker-Lewis Index (TLI; ≥ 0.90 adequate; ≥ 0.95 excellent), and Root-Mean-Square Error of Approximation with its 90% confidence interval (RMSEA; ≤ 0.10 acceptable; ≤ 0.08 adequate; ≤ 0.06 excellent)40,41,42. Given the slightly non-normal distribution of the data (i.e., skewness values for the Total, Relation, and Technique variables ranged − 1.35 and 0.08, and the kurtosis values ranged between − 1.02 and 1.61), the robust maximum likelihood (MLR) estimator was used for all LGCMs.
Finally, we tested the robustness of these results in sensitivity analyses with best-case worst-case imputations43. Worst-case rules were T2 = T1 and T3 = T1. Best-case rules were T2 = T1 + mean difference of the sample at time point, and T3 = T2. For objective 1, we set the success criteria to reaching a 70% total skill mastery level in 75% of the sample, as was formulated in our initial project accepted by the grant agency (Date: 2019-12-03)35. LGCM were performed in Mplus 8.744. Other statistics were performed in SPSS v24 and Excel 365 2023. For inference, we set the significance level at 0.05. The repository link to access data and syntax during peer review is available here: https://osf.io/rdbe4.
Results
Characteristics of participants
A total of 127 professionals were approached, among which 98 (77%) logged in and signed the e-consent form. Among those who signed electronically, 78/98 (79%) followed the training in full. Since a subset of 20 professionals did not practice blood draws and thus could not be evaluated by the standardized simulation situation (e.g., respiratory therapists, educators, and a certified child life specialist), the final study sample was of 58 HCPs who were assessed with the standardized simulation scenarios. Of those, 50 (86%) participants chose to train in the Pleasant Place and 8 (14%) in the Magic Glove (Fig. 1). The majority (52/58, 90%) of these participants were women, and their mean age was 39 ± 10 years. Participants were mainly nurses (54/58, 93%) with a few physicians (4/58, 7%) and altogether had an average of 16 ± 10 years of clinical practice. More than half of participants (31/58) came from the hematology-oncology department, 13/58 (22%) from the emergency department and 14/58 (24%) from other departments including general pediatrics, critical care, and dermatology.
Preliminary analyses
Satisfaction with the training was excellent with a mean score of 3.91/4 ± 0.27 (97%). The coefficient of variation was very low (7%), showing a strong consistency of satisfaction across the sample. When exploring duration of encounters across timepoints, we found encounters to last a median 2:55 min (IQR = 1:09) at T1, 4:31 min (IQR = 1:36) at T2, 3:14 min (IQR = 1:57) at T3.
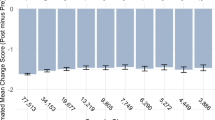
A description of outcomes with boxplots suggested a global trend toward an increase of skills at T2 and a slight decrease at T3, in all three scores Total, Relation, and Technique (Supplementary Fig. 1). Interestingly, boxplots also indicated that variability tended to increase at T3 showing T1-T2-T3 inter-quartile ranges (IQR) of 1.62-1.50-3.00 (Total), 1.50-1.00-1.50 (Relation), 1.00-1.00-2.50 (Technique). This suggested higher variability in skill retention (T3) in comparison to the other time points. Finally, the boxplots also suggested reduced room for improvement in the Relation subscale (high baseline scores).
A comparison of raw differences in non-imputed data across time-points suggested significant T1-T2 improvements in all three scores, with the Total score improving by 3.40 points (95%CI 2.93–3.88), the Relation score by 0.99 (95%CI 0.74–1.24), and the Technique score by 2.40 (95%CI 2.07–2.73). This translated into %change in skills of: Total + 62% (53–70%), Relation + 28% (21–35%), Technique + 123% (106–140%).
These raw results also suggested a maintenance of skills at T3 follow-up with T1-T3 differences showing increases in the Total score by 2.40 (95%CI 1.89–2.92), the Relation score by 0.52 (95%CI 0.24–0.80), and the Technique score by 1.88 (95%CI 1.54–2.22). This translated into %changes at T3 of: Total + 44% (34–53%), Relation + 15% (7–22%), Technique + 96% (79–113%).
Main analyses
The results indicated that the non-linear LGCM models fit the data better in the case of all outcome variables compared to the linear models (Supplementary Table 1). Therefore, the non-linear models were retained for further analyses. It should be noted that the CFI value for the non-linear LGCM for the technique variable was slightly below the acceptable cut-off, but the TLI and RMSEA values were excellent. Therefore, we retained this model for further analyses as well. Parameter estimates for each retained model are reported in Table 1.
Total score
Overall, T2 levels approximated 81% (8.92/11) in the 11 skills assessed on the SJ-HCAS, with 3.4% (T1), 77.6% (T2), 50% (T3) of interactions being scored above the pre-determined success criteria of 70%, i.e. at least 8 out of 11 skills being deployed in simulations (Fig. 3 panel A). On a descriptive level, the findings suggest that there was an increase of scores by 3.394 points (95%CI: 2.948–3.841) (+ 61%) from pre-intervention (T1) to post-intervention (T2). At follow-up (T3), although participants’ total scores decreased compared to post-intervention (T2), they still reported significantly higher total scores than at pre-intervention (T1) with 70% of the change (that was present between T1-T2) still being observed at T3. Results from LGCM showed significant variation in baseline levels (intercept) and the trajectory (slope) (Table 1). The intercept and slope had a negative association (unstandardized r = -1.305, p < .001; standardized r = − .73, p < .001), suggesting that the change in the Total score over time was smaller among those with higher T1 scores. When exploring contributors to the variability of the intercept and slope (i.e., adding the time-invariant predictors to the model described in the statistical analyses section), only gender was significantly related to the intercept (all other predictors’ ps > 0.166). Women had higher initial Total scores than men (B = -1.061, p = .015), but the change over time was unrelated to gender (p = .534).
Relation
T2 levels approximated 91% (4.57/5) in the 5 skills assessed on the SJ-HCAS (Fig. 3, panel B). On a descriptive level, the findings suggest that there was an increase of the Relation scores by 0.972 points (95%CI: 0.730–1.213) (+ 27%) from pre-intervention (T1) to post-intervention (T2). After 5 months (T3), although participants’ Relation scores decreased compared to post-intervention (T2), they were still significantly higher than pre-intervention (T1) with 55% of the change (that was present between T1-T2) still being observed at T3. The results of LGCM showed significant variability in baseline levels of Relation (intercept) but not in the trajectory (slope) (Table 1). The intercept and slope did not have a significant association based on the unstandardized estimates (unstandardized r = -.220, p = .131; standardized r = − .64, p = .001), suggesting that the change over time was not related to participants’ T1 scores. When exploring contributors to the variability of the intercept and slope (i.e., adding the time-invariant predictors to the model described in the statistical analyses section), none of the predictors were significantly associated either with the intercept or the slope (all ps > 0.052).
Technique
T2 levels approximated 73% (4.36/6) in the 6 skills assessed on the SJ-HCAS (Fig. 3 panel C). On a descriptive level, the findings suggest that there was an important increase of the Technique scores by 2.416 points (95%CI: 2.110–2.721) (+ 124%) from pre-intervention (T1) to post-intervention (T2). At follow-up (T3), although participants’ Technique scores decreased compared to post-intervention (T2), they were still significantly higher than at pre-intervention (T1) with 75% of the change (that was present between T1-T2) still being observed at T3. Results from LGCM showed significant variation in baseline levels (intercept) and the trajectory (slope) (Table 1). The intercept and slope had a negative association (unstandardized r = -.479, p = .001; standardized r = − .64, p < .001), suggesting that the change in the Technique score over time was smaller among those with higher T1 scores. When exploring contributors to the variability of the intercept and slope (i.e., adding the time-invariant predictors to the model described in the statistical analyses section), only gender and age were significantly related either to the intercept or the slope (all other predictors ps > 0.060). Women had higher initial Technique scores than men (B = -0.593, p = .029), but the change over time was unrelated to gender (p = .399). In addition, even though the intercept was not significantly related to the slope (p = .873), the change over time in the Technique scores was greater for younger participants (B = -0.035, p = .024).
Sensitivity analyses
The results from the sensitivity analyses supported results computed with the FIML strategy (see Supplementary Table 1 and Table 1). Best-case scenario: We observed a significant increase of skills following training (Total + 61%, Relation + 28%, and Technique + 123%). Skills decreased at follow-up, but a significant portion of change was maintained (Total 74%, Relation 59%, Technique 79%). Worst-case scenario: We observed a significant increase of skills following training (Total + 60%, Relation + 27%, and Technique + 121%). Skills decreased at follow-up, but a significant portion of change was maintained (Total 65%, Relation 49%, Technique 73%). Full syntax and data are available in the study repository35.
Complementary analyses
In a subset of n = 11 on the waitlist, we were able to collect a pre-baseline measure one week before training. In this subset, T1-T3 trends appear graphically similar to what was previously described in the larger group. In contrast, pre-baseline T0 levels show an absolute stability with T1 in the absence of training (Total: ICC = 0.915, Relation: ICC = 0.862, Technique: ICC = 0.864) (Supplementary Fig. 235). These results suggest no change in HC skills was observed in absence of training. Finally, to better understand the source of change in the main analysis we compared frequencies for each skill over the three timepoints with a Cochrane Q test (Fig. 4). The results showed that 6 out of 11 skills were more frequent after training: Synchronicity or adapted pace (Q = 16.083, p < .001), Rhythm, slowing and calming down (Q = 24.056, p < .001), Using sensory modalities (Q = 65.636, p < .001), Using a secure/relaxing language (Q = 24.074, p < .001), Including the procedure in imagery (Q = 39.793, p < .001), Patient concentrated and slowed (Q = 64.791, p < .001). Except for Synchronicity, all these skills were still significantly more frequent at follow-up than at baseline (post-hoc McNemar, Fig. 4).
Discussion
In a pre-post follow-up study involving 58 pediatric HCPs, we found that enrollment in Rel@x improved short- and long-term hypnosis-derived communication skills designed to mitigate paediatric pain (61% of skills improvement, 70% of maintenance). This improvement was mostly attributable to the technical aspects of communication, and less to the cross-sectional relational skills. We observed significant variability in improvements, partly due to initial levels of skills mastery, as participants with lower initial competence benefitted more from the training. The improved mastery of technical skills was also larger in younger participants. These results are much in line with recently developed institutional policies to mitigate paediatric procedural pain such as those from the Canadian Paediatric Society45. Leading tertiary hospitals have emphasized the communication and non-pharmacological aspects of the relationship with patients and their families, including allowing comfort positioning and control over the procedure, positively supporting the patient, and diverting the patient’s attention from the procedure46,47.
We found that more than 77% of participants displayed 8 or more skills out of the 11 skills after training, which surpassed our pre-established success criterion of ¾ of the sample. This proportion is superior to that of a previous feasibility study in a limited number of hematology-oncology nurses26. Our results also suggested that Rel@x was associated with more pronounced improvements on HC technical skills when compared with more general relationship skills. This may be due to the differential effect of pre-existing participant experience on both domains. In fact, this study excluded participants with previous knowledge/training in HC, which translated to low baseline levels in technical skills in this matter, thus leaving larger room for learning new skills. This was not the case with more cross-sectional relational competences where baseline levels were already high. In this domain, Rel@x brought about learning of significant but limited new skills. It can be assumed that in such a tertiary hospital, many experienced HCPs had already developed supportive ways to interact with young people and their parents48. This is especially true for HCPs interested in participating in a communication training program such as Rel@x. So, self-selection inherent to this type of program might have increased this phenomenon. Such an observation is a traditional bias in communication training programs targeting HCPs49.
Nevertheless, relational and technical skills should not be considered as independent domains as one may reinforce the other. Indeed, relational skills have been recognized as a prerequisite for the development of technical skills when using hypnosis in paediatrics. The implementation of techniques may, in turn, reinforce cooperation and thus enhance the quality of the relationship50. It is interesting to note that changes observed on sub-scores in the present study were related to improvements on an array of individual skills tapping key components of hypnotic communication, such as adopting a slow and calm rhythm, using a secure and relaxing language to interact with patients, using multisensory imagery or suggesting analgesia. This is in line with the definition of this sort of communication and may serve as a validity element of the training content12,29,51.
It is notable that a majority of skills learned with Rel@x were maintained at follow-up. From 55 to 75% of new skills acquired were still displayed in simulations 5 months later. Although we did not collect this information, we may hypothesize that these skills were retained and applied in practice after training. Putting skills in practice is recognized as an essential element of retention when acquiring new competences in nursing education52. It is also possible that specific tools or components of the training may be of particular help, such as the e-training module and other practical tools31. Yet, seeing the glass as being half empty, we should recognize that 25–45% of the learned skills were not displayed at follow-up overtime. When comparing individual skills frequencies drop at follow-up, we observe a widespread 15–20% drop in almost all skills that were learned (Fig. 4). These figures are hardly comparable to any existing data in the field and could be due to a range of factors such as loss in skill competence, work overload or stress. They underline the need for booster sessions after the main training that should address the array of HC competences. This could take the form of a practical supervision provided by Rel@x instructors, or a community practice within groups or wards that have been trained. Future studies could focus on the effects of complementary sessions on maintaining hypnotic communication skills in clinical practice.
When exploring contributing factors to the progress after training, we first observed that participants with lower initial competence benefitted more from the program. This was true for technical but not relational skills that were limited by a ceiling effect and lower trajectory variability. The effect of baseline is a strong limitation to change in interventional research53 and is often observed in education research54. When exploring individual characteristics, younger participants acquired more technical skills than older participants. It is possible that younger HCPs are characterized by more motivation to learn new skills, flexibility, openness, or other abilities that would favor a better or quicker uptake of HC techniques, as assimilation is easier than accommodation55. If this is further corroborated in future studies, one could argue that younger participants (e.g. nursing trainees) could be a promising target group for future trials and HC implementation as they are likely to show the largest improvements with training, and these skills could impact the quality of care over their forthcoming career. It could also lend support to adapt HC training for older professionals, for instance by adjusting the program format, allowing more time for learning skills and allowing them to practice the skills between sessions. It is also possible that older participants hold to their communication strategies, which they may find effective on children’s pain. Finding supporting evidence for this would require a dedicated study. Future studies should compare the use of HC with other communication strategies, for instance using counting or respiratory techniques, which are widely taught in nursing school56. Interestingly, we did not find any effect of other potential contributors such as the technique trained (Pleasant Place or Magic Glove), level of education, profession, years of practice or department of practice, on learning. Although the study is not powered for comparison purposes, the results do not suggest that one technique is more difficult to train in than the other.
This study follows several important steps allowing to further test the use of HC. Previous research has enabled to define and measure HC by coding observed behaviours25, to demonstrate that it was feasible to train HCPs26, and that training was promising on patient and family outcomes27. Recently, the Rel@x training program was developed and refined with a qualitative study optimizing its pertinence, acceptability, and satisfaction levels29. Our study suggests that it is possible to train a large group of HCPs in a specialized setting and thus build capacity to intervene. Notably, professionals can use HC techniques while performing the painful procedure in practice, with no need of extra support from a pain specialist. The following step should be to demonstrate the impact of using such skills in practice on real patients’ procedural pain and distress. Following recommended steps on intervention optimization, this could take the form of a pilot study with a control group to compare interactions where the HCP was exposed vs. not exposed to HC training28. To avoid contamination, one could compare independent sites.
We recognize the limitations of this research. As a preliminary remark, it did not demonstrate the efficacy of hypnotic communication on pain. Rather, it was designed to evaluate skill acquisition and retention in participants following a communication training. Although manualized, the Rel@x training is provided to groups. This inevitably introduces variability between trained groups. It is possible that interactions between members within groups either promoted or impeded learning, aspects that are not directly attributable to the training program and limit reproducibility. We did not include a control group. Consequently, it is not possible to attribute changes observed overtime to the training program. Yet, we observed no change in a small group on a waitlist, suggesting HC do not change “naturally”, without specific training. This should be replicated in a larger group. On another aspect, we found excellent satisfaction with training, but we should recognize that desirability or affiliation biases may have influenced participant’s ratings, as the satisfaction questionnaire was completed right after training. Limitations also pertains to the simulation protocol. Although healthcare professionals are used to being recorded, we cannot rule out the effect of being observed which could lead to a desire to perform better. It could have inflated the use of technical skills at baseline. Although the SJ-HCAS is reliable, we found lower reliability in the Relation sub-score. Results regarding this specific score should then be interpreted cautiously. Raters of this scale also probably figured out which video came from which stage of training, increasing the possibility of experimenter expectations biasing the results. To deal with this bias, it would be interesting in the future to complement the SJ-HCAS with more objective measures, such as word counts or micro-behavior coding, that do not need interpretation from the coder and can even be performed automatically. We also recognize that the external validity of the study is limited, as only one painful procedure (venipuncture) was simulated. Although participants reported they would use the techniques in different situations (Porth-A-Cath, dressing change, vaccination, lumbar puncture, etc.), we could not evaluate this in the present project. As for external validity, we should also recognize that nurse participants were compensated for their time. This was instrumental in enrolling participants in the hard times of the Covid-19 pandemic. Yet, it also came with a cost, as it limits the feasibility of the research in low-income environments. Finally, we should recognize the disturbances to the project due to the Covid-19 pandemic. We had initially planned to include patient outcomes as a second broad aim of the present research, but this was not feasible due to repeated shutdowns and work overload.
Conclusions
The present study reports the results of a standardized two half-day training in hypnotic communication designed to mitigate procedural pain and distress in pediatrics (Rel@x). Hypnotic communication includes aspects such as: slowing down the rate of speech, using positive, relaxing, and secure words, distracting the patient’s attention from the painful procedure, or using imagery and analgesia suggestions. We trained 78 professionals and coded 168 video-recorded simulated encounters across three time-points. The results suggested that the training was associated with a + 61% improved competence after training and 70% retention of acquired skills over a 5-month period. Almost 80% of the evaluated sample reached a pre-established desired level of competence after training. The results show that it is possible to train a large number of professionals with very good training efficacy. Future studies should now focus on testing if the use of HC techniques during treatment is associated with less pain and distress in young patients.
Data availability
Data and syntax used in this study are fully accessible in the Open Science Framework repository at the following link: https://osf.io/rdbe4.
References
Birnie, K. A. et al. Systematic review and meta-analysis of distraction and hypnosis for needle-related pain and distress in children and adolescents. J. Pediatr. Psychol. 39 (8), 783–808. https://doi.org/10.1093/jpepsy/jsu029 (2014).
Po, C. et al. The management of procedural pain at the Italian centers of pediatric hematology-oncology: state-of-the-art and future directions. Supportive care in cancer. 20 (10) 2407–2414.https://doi.org/10.1007/s00520-011-1347-x (2012).
McCarthy, A. M. & Kleiber, C. A conceptual model of factors influencing children’s responses to a painful procedure when parents are distraction coaches. J. Pedriatic Nurs. 21 (2), 88–98. https://doi.org/10.1016/j.pedn.2005.06.007 (2006).
Stuber, M. L., Christakis, D. A., Houskamp, B. & Kazak, A. E. Posttrauma symptoms in childhood leukemia survivors and their parents. Psychosomatics 37 (3), 254–261 (1996).
Pai, A. L. & Kazak, A. E. Pediatric medical traumatic stress in pediatric oncology: family systems interventions. Curr. Opin. Pediatr. 18 (5), 558–562. https://doi.org/10.1097/01.mop.0000245358.06326.e9 (2006).
Kleiber, C., Craft-Rosenberg, M. & Harper, D. C. Parents as distraction coaches during IV insertion: A randomized study. J. Pain Symptom Manag. 22 (4), 851–861 (2001).
Rogers, T. L. & Ostrow, C. L. The use of EMLA cream to decrease venipuncture pain in children. J. Pediatr. Nurs. 19 (1), 33–39. https://doi.org/10.1016/j.pedn.2003.09 (2004).
Şahiner, N. C., İnal, S. & Akbay, A. S. The effect of combined stimulation of external cold and vibration during immunization on pain and anxiety levels in children. J. PeriAnesth. Nurs. 30 (3), 228–235 (2015).
Koller, D. & Goldman, R. D. Distraction techniques for children undergoing procedures: A critical review of pediatric research. J. Pediatr. Nurs. 27 (6), 652–681. https://doi.org/10.1016/j.pedn.2011.08.001 (2012).
Hadjistavropoulos, T. et al. A biopsychosocial formulation of pain communication. Psychol. Bull. 137 (6), 910–939. https://doi.org/10.1037/a0023876 (2011).
Kaiser, P., Kohen, D., Brown, M., Kajander, R. & Barnes, A. Integrating pediatric hypnosis with complementary modalities: clinical perspectives on personalized treatment. Children 5 (8). https://doi.org/10.3390/children5080108 (2018).
Hammond, D. C. Handbook of Hypnotic Suggestions and Metaphors. (WW Norton & Company, 1990).
Milling, L. S., Valentine, K. E., LoStimolo, L. M., Nett, A. M. & McCarley, H. S. Hypnosis and the alleviation of clinical pain: A comprehensive meta-analysis. Int. J. Clin. Exp. Hypn. 69 (3), 297–322. https://doi.org/10.1080/00207144.2021.1920330 (2021).
Thompson, T. et al. The effectiveness of hypnosis for pain relief: A systematic review and meta-analysis of 85 controlled experimental trials. Neurosci. Biobehav. Rev.. 99, 298–310. https://doi.org/10.1016/j.neubiorev.2019.02.013 (2019).
Langlois, P. et al. Hypnosis to manage musculoskeletal and neuropathic chronic pain: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 135, 104591. https://doi.org/10.1016/j.neubiorev.2022.104591 (2022).
Kuttner, L., Bowman, M. & Teasdale, M. Psychological treatment of distress, pain, and anxiety for young children with cancer. J. Dev. Behav. Pediatr. 9 (6), 374–382 (1988).
Liossi, C. & Hatira, P. Clinical hypnosis versus cognitive behavioral training for pain management with pediatric cancer patients undergoing bone marrow aspirations. Int. J. Clin. Exp. Hypn. 47 (2), 104–116 (1999).
Liossi, C. & Hatira, P. Clinical hypnosis in the alleviation of procedure-related pain in pediatric oncology patients. Int. J. Clin. Exp. Hypn. 51 (1), 4–28. https://doi.org/10.1076/iceh.51.1.4.14064 (2003).
Liossi, C., White, P. & Hatira, P. Randomized clinical trial of local anesthetic versus a combination of local anesthetic with self-hypnosis in the management of pediatric procedure-related pain. Health Psychol. 25 (3), 307–315. https://doi.org/10.1037/0278-6133.25.3.307 (2006).
Liossi, C., White, P. & Hatira, P. A randomized clinical trial of a brief hypnosis intervention to control venepuncture-related pain of paediatric cancer patients. Pain 142 (3), 255–263. https://doi.org/10.1016/j.pain.2009.01.017 (2009).
Kuttner, L. The Magic Glove: Using imagination and self hypnosis to help kids with pain. https://www.megfoundationforpain.org/2022/07/22/the-magic-glove-hypnotic-pain-management-for-children/ [Accessed 01 November 2023]. (2010).
Geagea, D. et al. Clinical hypnosis for procedural pain and distress in children: a scoping review. Pain Med. 24 (6), 661–702 (2023).
Kuttner, L. Pediatric hypnosis: pre-, peri‐, and post‐anesthesia. Pediatr. Anesth. 22 (6), 573–577 (2012).
Kuttner, L. A Child in Pain: What Health Professionals Can Do To Help. (Crown House Publishing, 2010).
Aramideh, J. et al. Development and inter-rater reliability of a tool assessing hypnotic communication behaviours adopted by nurses caring for children with cancer: the Sainte-Justine Hypnotic Communication Assessment Scale. Complement. Ther. Med. 37, 178–184 (2018).
Aramideh, J. et al. Do professionals change their communication behaviours following a training in hypnosis-derived communication? A feasibility study in pediatric oncology. Complement. Ther. Med. 52, 102426. https://doi.org/10.1016/j.ctim.2020.102426 (2020).
Ogez, D. et al. Does practising hypnosis-derived communication techniques by oncology nurses translate into reduced pain and distress in their patients? An exploratory study. Br. J. Pain 15 (2), 147–154. https://doi.org/10.1177/2049463720932949 (2021).
Czajkowski, S. M. et al. From Ideas to Efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 34 (10), 971–982. https://doi.org/10.1037/hea0000161 (2015).
Aramideh, J., Ogez, D., Rondeau, É., Duval, M. & Sultan, S. Development and refinement of Rel@x: A training in hypnosis-derived communication for pediatric nurses to prevent procedural pain. Br. J. Pain 16 (5), 546–559. https://doi.org/10.1177/20494637221103170 (2022).
Des Jarlais, D. C., Lyles, C., Crepaz, N. & the TG. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am. J. Public Health 94 (3), 361–366 (2004).
Sultan, S., Ogez, D., Rondeau, É., Duval, M. & Aramideh, J. Training material Rel@x: hypnotic communication training to prevent pain. https://doi.org/1866/25349. Montreal (Qc), Canada: Université de Montréal. [Accessed 01 November 2023]. (2021).
Kohen, D. P. & Olness, K. Hypnosis and Hypnotherapy With Children Fourth edn (Routledge, 2011).
Kuttner, L. Pediatric hypnosis: pre-, peri-, and post-anesthesia. Pediatr. Anesth. 22 (6), 573–577 (2012).
Kuttner, L. [cited November 2018]. http://pediatric-pain.ca/wp-content/uploads/2013/04/The_Magic_Glove12.pdf (2018).
Dataset and supporting files for the study: Training healthcare professionals in hypnosis-derived communication to mitigate procedural pain in children: skills acquisition and maintenance [Internet]. Open Sci. Framew. https://osf.io/rdbe4 (2025).
Newman, D. A. Missing data: five practical guidelines. Organ. Res. Methods 17 (4), 372–411 (2014).
Bollen, K. A. & Curran, P. J. Latent Curve Models: A Structural Equation Perspective (Wiley, 2006).
Hardy, S. & Thiels, C. Using latent growth curve modeling in clinical treatment research: comparing guided self-change and cognitive behavioral therapy treatments for bulimia nervosa. Eur. Psychiatry 22 (S1), S180–S (2007).
Fan, X. Power of latent growth modeling for detecting group differences in linear growth trajectory parameters. Struct. Equ. Model. 10 (3), 380–400 (2003).
Kenny, D. A., Kaniskan, B. & McCoach, D. B. The performance of RMSEA in models with small degrees of freedom. Sociol. Methods Res. 44 (3), 486–507 (2015).
Schermelleh-Engel, K., Moosbrugger, H. & Müller, H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. Online 8 (2), 23–74 (2003).
Browne, M. W. & Cudeck, R. Alternative ways of assessing model fit. Sociol. Methods Res. 21 (2), 230–258 (1992).
Jakobsen, J. C., Gluud, C., Wetterslev, J. & Winkel, P. When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Med. Res. Methodol. 17 (1), 162. https://doi.org/10.1186/s12874-017-0442-1 (2017).
Muthén, L. K. & Muthén, B. O. MPlus User’s Guide. Eighth Edition. (Los Angeles, CA , 2022).
Trottier, É. D., Doré-Bergeron, M-J., Chauvin-Kimoff, L., Baerg, K. & Ali, S. Managing pain and distress in children undergoing brief diagnostic and therapeutic procedures. Paediatr. Child Health 24 (8), 509–521. https://doi.org/10.1093/pch/pxz026 (2019).
UCSF. The Comfort Promise at UCSF Benioff Children’s Hospitals The Regents of The University of California. https://www.ucsfbenioffchildrens.org/services/comfort-promise (2023).
CHU Sainte-Justine (Sainte-Justine University Health Centre). Tout Doux: Pour des soins en douceur 2022. https://www.chusj.org/soins-services/D/Douleur/Confort/Professionnels [Accessed 05 October 2023].
Thrane, S. E., Wanless, S., Cohen, S. M. & Danford, C. A. The assessment and non-pharmacologic treatment of procedural pain from infancy to school age through a developmental lens: A synthesis of evidence with recommendations. J. Pediatr. Nurs. 31 (1), e23–e32. https://doi.org/10.1016/j.pedn.2015.09.002 (2016).
Harnischfeger, N. et al. Effects of a communication training for oncologists on early addressing palliative and end-of-life care in advanced cancer care (PALLI-COM): a randomized, controlled trial. ESMO Open 7 (6), 100623. https://doi.org/10.1016/j.esmoop.2022.100623 (2022).
Wood, C. & Bioy, A. Hypnosis and pain in children. J. Pain Symptom Manag. 35 (4), 437–446. https://doi.org/10.1016/j.jpainsymman.2007.05.009 (2008).
Kohen, D. P. & Olness, K. Hypnosis and Hypnotherapy With Children 5th edn (Routledge, 2023).
Oermann, M. H., Kardong-Edgren, S. E. & Odom-Maryon, T. Effects of monthly practice on nursing students’ CPR psychomotor skill performance. Resuscitation 82 (4), 447–453. https://doi.org/10.1016/j.resuscitation.2010.11.022 (2011).
Powell, L. H., Kaufmann, P. G. & Freedland, K. E. Outcomes. In: (eds Powell, L. H., Freedland, K. E. & Kaufmann, P. G.) Behavioral Clinical Trials for Chronic Diseases: Scientific Foundations. 209–236. (Cham: Springer International Publishing, 2021).
Albanese, M. Problem-based learning: why curricula are likely to show little effect on knowledge and clinical skills. Med. Educ. 34 (9), 729–738 (2000).
Gegenfurtner, A. & Vauras, M. Age-related differences in the relation between motivation to learn and transfer of training in adult continuing education. Contemp. Educ. Psychol. 37 (1), 33–46. https://doi.org/10.1016/j.cedpsych.2011.09.003 (2012).
Pancekauskaitė, G. & Jankauskaitė, L. Paediatric pain medicine: pain differences, recognition and coping acute procedural pain in paediatric emergency room. Medicina 54 (6), 94. https://doi.org/10.3390/medicina54060094 (2018).
Acknowledgements
The research team is most grateful to the healthcare teams of the Centre Hospitalier Universitaire Sainte-Justine who facilitated access of their personnel to the training. We also deeply thank patient partners who helped us with data collection and interpretation: Ariane Lacoste-Julien, Mathias Tyo-Gomez. We thank Anne-Frédérique Tessier for helping in data collection. We are grateful to Andrea Laizner and Christian Dagenais for their help on writing sections of the initial grant application.
Funding
This study received support from the FRQs-Oncopole, Grant #302025 (year 2020). The funder had no specific role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conception: SS, MD, JA, ER, SLM, AM, CJB, AT, DO. Design: SS, MD, JA, ER, SLM, AM, CJB, AT, DO. Data acquisition and analysis: MD, ALatendresse, MB, ALévesque, ER, AM, MJDB, EDT, JG, DO. Interpretation of data: SS, MD, JA, BB, ALatendresse, MB, ALévesque, ER, SLM, AM, CJB, AT, MJDB, EDT, JG, DO. Drafting: SS, DO. Revision: SS, MD, JA, BB, ALatendresse, MB, ALévesque, ER, SLM, AM, CJB, AT, MJDB, EDT, JG, DO. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was granted by the CHU Sainte-Justine Research Ethics Board (#2019–2205) and the research was conducted according to the principles expressed in the Declaration of Helsinki. All participants provided written informed consent.
Consent to publish
Informed Consent for the publication of the individual image in Fig. 2 was obtained from the two individuals.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sultan, S., Duval, M., Aramideh, J. et al. Training healthcare professionals in hypnosis-derived communication to mitigate procedural pain in children. Sci Rep 15, 8266 (2025). https://doi.org/10.1038/s41598-025-91267-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91267-7