Abstract
Long-term changes in health-related quality of life (HrQoL) after SARS-CoV-2 infection are common, but their causes and consequences are poorly understood. This prospective, population-based study examined associations between HrQoL and 49 demographic and clinical variables. HrQoL was assessed using the European Quality-of-Life-5-Dimensions-5-Level-Version in 3,475 participants (56% female; aged 18–88 years) approximately 9 months (baseline) and 26 months (follow-up) after their initial infection. Results were compared with the demographic and clinical variables using recursive feature elimination and random forest regression analyses. A statistically significant improvement in HrQoL was observed during the observation period. At baseline, 39% of the variance in HrQoL was explained by fatigue, muscle pain, number of remaining symptoms (RS), perceived stress, and age. At follow-up, fatigue, RS, perceived stress, muscle and joint pain, and age explained 54% of the variance in HrQoL. Changes in HrQoL were associated with changes in fatigue, RS, and perceived stress, meaning that if these decreased from baseline to follow-up, then HrQoL was improved. However, it was not possible to predict whether an individual’s HrQoL would improve or worsen 1 year later based on baseline variable scores. The aforementioned symptoms are specifically associated with impairment in the population’s usual activities.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has caused more than 777 million infections and more than 7 million infection-related deaths worldwide as of December 20241. The average recovery time from acute SARS-CoV-2 infection is two to four weeks2, and any severe persistence of symptoms for more than 12 weeks is referred to as “post-COVID Syndrome” (PCS)3,4 or sometimes as “Long COVID”5. The prevalence of PCS in the USA is 14%, and up to 31% of COVID-19 patients developed PCS6. Since a large number of people were infected with SARS-CoV-2, these circumstances resulted in a large number of people suffering from PCS, which has since been recognized as a pressing public health issue. Not surprisingly, health-related quality of life (HrQoL) has been found to be reduced in PCS patients7. This is also associated with a loss of ability to work, which has economic consequences8,9. Although the course of HrQoL in relation to PCS is not well understood, it is likely to be particularly related to fatigue and perceived stress10,11. But there is also a wide variety of symptoms that can occur with PCS, including common signs of infection; dermatologic, gastrointestinal, neurologic, and throat disorders; various types of pain; chemosensory deficits; and exercise intolerance3.
Fatigue is defined as the depletion of energy reserves combined with an increased need for rest disproportionate to the previous exertion12. It appears to be a complex distortion of the physical, mental, cognitive, emotional, motivational, and social states of an individual, resulting in decreased functioning13,14. Fatigue has been found to be significantly associated with a decrease in quality of life in many diseases, including multiple sclerosis, cancer, and chronic obstructive pulmonary disease15,16,17. Fatigue is also one of the most commonly reported symptoms of PCS18, affecting 71% of patients19. Fatigue in the context of PCS has been associated with distinct structural and functional brain changes20,21,22. Depression and anxiety were also shown to be risk factors for prolonged fatigue after SARS-CoV-2 infection23. The relationship between HrQoL and perceived stress has been shown in other lung diseases, such as asthma24. In the case of SARS-CoV-2, people who had increased perceived stress before infection were more likely to report PCS symptoms that interfered with daily life after infection25. Thus, higher perceived stress may be a risk factor for the maintenance of PCS symptoms. In addition, PCS patients with symptoms such as fatigue, weakness, dyspnea, shortness of breath, palpitations, forgetfulness, numbness, sleep disturbance, cough, chest pain, muscle pain, joint pain, headache, anosmia, hair loss, taste loss, and many others have significantly lower HrQoL26,27,28. However, studies disagree on which symptoms actually significantly worsen HrQoL, and it is also largely unclear how much a given symptom worsens HrQoL and in what constellation it does so.
In summary, psychological and psychosocial factors, as well as physical symptoms, play a role in the well-being of former SARS-CoV-2 patients. There are an overwhelming number of symptoms that can occur in PCS, in different combinations and with different degrees of severity. However, to the best of our knowledge, there is no literature on which symptoms in combination are affecting HrQoL the most. The question is which symptoms are most detrimental to HrQoL and whether there are any symptoms that have no detrimental effect on HrQoL at all. This information would be essential to prioritize certain aspects of patients in the most efficient way for multimodal therapy approaches. This study aims to examine a large number of factors and symptoms in an exploratory way to determine which are most strongly associated with reduced HrQoL and the intensity with which they affect the HrQoL. To our knowledge, this is the first large-scale prospective study of the effect of demographic and clinical variables on HrQoL in individuals with and without PCS.
Methods
Study cohort
COVIDOM is a prospective, longitudinal, multicenter, population-based study of the long-term sequelae of COVID-19, carried out in Kiel, Berlin, and Wuerzburg under the umbrella of the German National Pandemic Cohort Network (NAPKON). Details about COVIDOM (aka NAPKON-POP) have been published before25,29,30, including study protocol, recruitment scheme, cohort characteristics, and non-responder analyses. Briefly, COVIDOM includes individuals aged 18 years or older, resident in Schleswig-Holstein (Kiel region), Berlin-Neukoelln, or Lower Franconia, Germany, and diagnosed SARS-CoV-2 positive by way of a PCR test. Public health authorities supported recruitment into COVIDOM by mailing appropriate invitations to potential participants. The main exclusion criterion was an acute re-infection at the scheduled study site visit. The first assessment (baseline) took place at least 6 months after infection, followed by a second assessment (follow-up) at least 18 months after infection. The present study included COVIDOM participants who underwent a baseline assessment between November 16, 2020, and May 17, 2023, and whose follow-up assessment took place between May 10, 2022, and September 28, 2023. All of the participants were invited to follow-up, but at the time of the data analysis, this had not yet taken place for all of them. In accordance with the Declaration of Helsinki, written informed consent was obtained from all COVIDOM participants. The study has received ethical approval from the respective Ethics Committees (for further information, see the patient consent and ethics approval section of this paper). COVIDOM was registered in the German Registry of Clinical Studies (DRKS00023742) and in ClinicalTrials.gov (NCT04679584).
Questionnaires & assessments
HrQoL was assessed using the European Quality-of-Life-5-Dimensions-5-Level-Version (EQ-5D-5L)31. With this tool, HrQoL is rated along the five dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension provides five response options: no problems, slight problems, moderate problems, major problems, and extreme problems. Each response contributes to a quality-of-life index between 0 and 1, with 1 representing the best condition and 0 representing the worst condition.
The Functional Assessment of Chronic Fatigue Illness – Fatigue Subscore (FACIT-Fatigue Scale) questionnaire was used to assess fatigue32. The FACIT-Fatigue Scale comprises 13 items measuring fatigue symptoms over the previous seven days. A 5-point Likert scale is used to rate the severity of fatigue symptoms as “not at all”, “a little”, “moderate”, “quite”, or “very”. The overall score ranges from 0 to 52, with lower scores indicating more severe symptoms and scores ≤ 30 considered clinically relevant fatigue33.
The 10-item Perceived Stress Scale (PSS-10) was used to measure perceived stress, defined as the degree to which life was experienced as unpredictable, uncontrollable and overwhelming34. A 5-point Likert scale is used to rate the frequency with which an item was experienced in the past month as “never”, “almost never”, “sometimes”, “fairly often”, or “very often”. The total score ranges from 0 to 40, with higher scores indicating higher levels of perceived stress.
Sociodemographic information was collected using standardized questionnaires. Height and weight were measured at the study site visit. In a general standardized clinical interview, patients were also asked what symptoms they had during their SARS-CoV-2 infection, which of these symptoms persisted to the time of the assessment, what pre-diagnosed diseases they had before their SARS-CoV-2 infection, their vaccination status, their employment status, and whether they were treated during their SARS-CoV-2 infection (at home, in hospital, in intensive care, and/or on mechanical ventilation). In an additional neurology-specific standardized clinical interview, participants were asked whether they subjectively felt cognitively impaired since the infection (i.e., word-finding disorder).
The Montreal Cognitive Assessment (MoCA) was administered to assess global cognition. According to the manual, a score < 26 is considered an indication of cognitive impairment35. The MoCA includes information on whether they have > 12 years of education.
Statistical analysis
R software version 4.3.236 was used for data visualization and statistical analysis. Participants with a missing value or answer “don’t know” for at least one of a pre-specified set of (relevant) variables were excluded from the respective analysis. Details about all variables included in the statistical analysis are provided in Supplementary Table S1.
Recursive feature elimination (RFE)
Regression modeling of the HrQoL of participants was performed separately for the baseline and follow-up data. Prior to each regression, Recursive Feature Elimination (RFE) served to determine the most efficient number of independent variables to be included in the final modeling. To this end, interim models were computed using a 10-fold cross-validation method implemented in R package caret37. RFE starts with a full model and iteratively reduces the number of independent variables by one. The advantage of this method is that it takes into account the interaction of variables in any possible constellation. Models were evaluated exploratory by their associated root-mean-square error (RMSE) to determine, by visual inspection of the RMSE plot, the best compromise between model fit and the number of independent variables included. The selected variables were then included in the final random forest regression analysis. Because we don’t know in advance which variables will be selected by RFE, the following analyses are exploratory, as we made no assumptions about possible effects.
Random forest regression
Random forest regression analysis was performed to quantify the association between HrQoL, measured by EQ-5D-5L, and the RFE-selected independent variables. Random forest regression is suitable for large datasets with complex interactions and is robust to noisy data and outliers38,39. The number of independent variables randomly sampled as candidates at each split was set to two, and the number of trees to be grown was set to 2000. Data were divided randomly into a training set, comprising 70% of the data, and a test set, comprising 30%. The random forest regression models were trained with R package randomForest40, and each resulting model was validated on the test set. The coefficient of determination (R2) and RMSE of the final model were used to estimate the amount of variance of EQ-5D-5L explained and the goodness of fit of each model. The mean decrease in accuracy (MDA) of the variables in the final model was used to quantify the overall importance of each independent variable for the model. Accumulated local effects (ALE) plots were used to illustrate the value-specific effects of each independent variable on EQ-5D-5L.
Additional analyses
To ensure that the amount of variance explained and the relevance of the selected variables were not due to psychiatric conditions present in the cohort prior to the pandemic, the procedure described above was repeated in subsets of the data that included only participants with or without a pre-diagnosis of anxiety or depression. The final random forest regression analysis was also repeated with each dimension of the EQ-5D-5L, respectively. In addition, RFE and random forest regression analyses were performed to determine whether a particular combination of independent variables at baseline could predict HrQoL at follow-up. Selected relevant variables were further analyzed by defining the change in each variable as a new independent variable and treating the difference in EQ-5D-5L between baseline and follow-up as the outcome. Spearman rank correlation coefficients served to quantify the relationships between variables. A two-tailed Wilcoxon signed-rank test for paired samples was used to assess whether EQ-5D-5L changed significantly over time. The resulting effect sizes were interpreted following Cohen41. P-values < 0.05 were considered statistically significant.
Results
Study sample
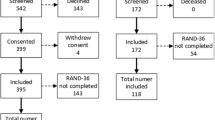
There were 3,475 participants at baseline and 2,510 at follow-up. The median age of the participants was 44 years (quartiles: 32; 57). The median time since initial infection was 299 days (quartiles: 165; 361) at baseline and 744 days (quartiles: 657; 835) at follow-up. Eleven percent of participants reported a previous diagnosis of depression, and 3% suffered from an anxiety disorder prior to their SARS-CoV-2 infection. Twenty percent had clinically relevant fatigue at baseline and 18% at follow-up. Additional sociodemographic and clinical details of the study sample, separated by whether clinically relevant fatigue was found according to FACIT-F, are shown in Table 1, and extended cohort characteristics are shown in Supplementary Table S2.
After excluding participants with missing data on any of the 50 variables, baseline data were available for the RFE for 2,174 of the 3,475 participants. Of these, 1,579 also had follow-up data, leaving 1,519 participants after exclusion of cases with missing data (Supplementary Fig. S3), which were used for the prediction analysis. For the RFE at follow-up, data were available for 2,350 of the 2,510 participants after excluding participants with missing data on any of the 29 variables.
Variables associated with HrQoL
The RMSE plots of all models that were computed in the RFE steps of the analysis (S4 – S9), and the MDA values of the variables that were included in each final model (S10 – S15) are provided in the Supplementary Information. Details of the final random forest regression models are provided in Supplementary Table S16.
Baseline
RFE identified the following five variables as relevant for inclusion in the final regression analysis of EQ-5D-5L (in descending order, starting with the most relevant variable): Fatigue (FACIT-Fatigue Scale), muscle pain (yes/no), Number of symptoms remaining from initial SARS-CoV-2 infection (RS), perceived stress (PSS), and Age (years). The final regression model could be calculated with 3,117 participants, and it achieved an R2 value of 0.39 (RMSE = 0.11), meaning that 39% of the variance in the EQ-5D-5L could be explained by the model through the five independent variables.
In the ALE plots of the variables selected for the analysis (Fig. 1), FACIT-Fatigue Scale ≤ 30, presence of muscle pain, RS > 1, PSS > 28, and age > 50 years were all independently associated with a lower than average EQ-5D-5L index.
Accumulated local effects (ALE) plots of the independent variables included in the random forest regression analysis of EQ-5D-5L at baseline. The x-axis is the scale of the respective variable, whereas the y-axis measures the average difference between the value-specific and the overall impact of the respective independent variable upon the outcome variable (EQ-5D-5L). Each dot corresponds to a value of the respective independent variable that was observed at least once in the study sample. EQ-5D-5L, European Quality-of-Life-5-Dimensions-5-Level-Version; FACIT-Fatigue Scale, Functional Assessment of Chronic Fatigue Illness – Fatigue Subscore; PSS, Perceived Stress Scale.
In participants without pre-diagnosed depression or anxiety, the same five independent variables were selected by RFE, and the final model accounted for 35% of the variance in EQ-5D-5L (RMSE = 0.09). In terms of their relative importance, as measured by MDA, muscle pain moved from the second to the fifth place. In participants with pre-diagnosed depression or anxiety, fatigue, RS and PSS were sufficient to explain 30% of the variance in EQ-5D-5L (RMSE = 0.15).
Regression models in Supplementary Table S17 using the individual dimension of the EQ-5D-5L instead of the index showed that the selected variables had a similar but slightly lower R2 value in the mobility (R2 = 29%) and anxiety/depression (R2 = 29%) dimensions. With the selected variables, most variance could be explained in the usual activities dimension (R2 = 47%), while the self-care dimension had a small R2 value (R2 = 4%).
Follow-up
RFE identified the following six variables as most important in explaining EQ-5D-5L at follow-up: Fatigue, RS, PSS, muscle pain, oint pain, and Age. The final regression model could be calculated with 2,350 participants, and it explained 54% of the variance of EQ-5D-5L (RMSE = 0.10). The ALE plots (Fig. 2) revealed that FACIT-Fatigue Scale < 35, RS > 3, PSS > 30, the presence of muscle pain or joint pain, and age > 50 were all independently associated with lower than average EQ-5D-5L.
Accumulated local effects (ALE) plots of the independent variables included in the random forest regression analysis of EQ-5D-5L at follow-up. For details, see legend to Fig. 1
Among participants without pre-diagnosed depression or anxiety, the corresponding model explained 43% of the variance in EQ-5D-5L (RMSE = 0.09), compared to 53% for participants with pre-diagnosed depression or anxiety (RMSE = 0.15). In the final models of both subsets, the same six variables were selected as in the full data set. Age had more weight after the data were separated. In the subgroup with pre-diagnosed depression or anxiety, RS (rank 5) had less weight.
Regression models in Supplementary Table S17 using the individual dimensions of the EQ-5D-5L instead of the index showed that the selected variables had a low R2 value in the mobility (R2 = 23%) and self-care (R2 = 14%) dimensions. The pain/discomfort (R2 = 40%) and anxiety/depression (R2 = 43%) dimensions had a lower R2 value than the index but were still moderately high.
Changes of HrQoL and independent variables
A difference of 0.09 was observed between the median EQ-5D-5L at baseline (median = 0.91; quartiles = 0.89, 1.00) and follow-up (0.999; 0.91, 1.00; Fig. 3). The two-tailed Wilcoxon signed-rank test showed that this difference was significant, with a small effect size (r = 0.23). This indicates that HrQoL increased 1 year after the first assessment in this cohort. However, even when all 49 possible independent variables measured at baseline were considered, the RFE did not result in a regression model that explained more than 1% of the variance of the EQ-5D-5L at follow-up (RMSE = 0.13).
Box plots showing the longitudinal change in the EQ-5D-5L index by displaying median, quartiles, range, and data points for baseline and follow-up, with additional lines to visualize each participant’s trajectory, and violin plots to visualize the density of the respective data. EQ-5D-5L, European Quality-of-Life-5-Dimensions-5-Level-Version.
On the other hand, changes from baseline to follow-up in FACIT-Fatigue Scale (Spearman correlation coefficient r = 0.27, p < 0.001), RS (r = -0.23, p < 0.001), and PSS (r = -0.13, p < 0.001) were all significantly correlated with the corresponding change in EQ-5D-5L. A regression model including these three changes explained 11% of the variance in the change in EQ-5D-5L (RMSE = 0.12). Although it was not possible to predict which participants would experience a decrease in HrQoL, it is associated with a decrease in fatigue, remaining symptoms and perceived stress.
Discussion
This explorative large prospective observational study, covering a 2-year period after SARS-CoV-2 infection, found that the HrQoL of patients is notably affected initially, but improves over time. Fatigue, the number of symptoms remaining from the acute phase of COVID-19, perceived stress, muscle pain, and age were found to play a role in HrQoL at both the beginning and at the end of the observation period.
At approximately nine months after acute SARS-CoV-2 infection, 39% of the variance in HrQoL could be explained in the present study by just five variables. This is a remarkably strong relationship between HrQoL and fatigue, muscle pain, the number of symptoms remaining from the acute phase of COVID-19, perceived stress, and age. Notably, fatigue had the strongest association with HrQoL (both at baseline and follow-up). Specifically, participants with a FACIT-Fatigue ≤ 30 have below-average HrQoL, further supporting the cut-off used to diagnose clinically relevant fatigue. These results fit well with other studies that have identified fatigue as the most important variable for PCS. For example, a score has been developed to assess the severity of PCS, with fatigue being a symptom with the highest weight in the calculation of this score3. This PCS score also correlates with HrQoL. Although most studies agree that fatigue is the most common symptom in PCS26,27,28, none of them report the extent to which it affects HrQoL. The fact that fatigue appears to be the most common symptom and also the one that most affects HrQoL emphasizes the fact that the treatment of PCS consists primarily of the treatment of fatigue. But it is more complex than that, because treatment options that would be classically chosen for fatigue, such as physical activity42, may be contraindicated for people with muscle pain. Another study27 supports the notion that muscle pain is one of the strongest associations with HrQoL, as in this case.
Patients with at least two persistent symptoms appeared to suffer from reduced HrQoL at baseline. This suggests that even 9 months after the acute infection, the persistence of symptoms that occurred at that time had an influence on HrQoL. There is also likely to be an inverse effect: The lower the HrQoL prior to infection, the greater the likelihood of experiencing an increased number of symptoms that persist after infection. One indication of this is that people with no residual symptoms from the initial infection have an above-average HrQoL in this sample, even though they make up 55% of the sample (supplementary table S2). From a causal perspective, it is unlikely that the absence of residual symptoms would raise the HrQoL of individuals above the average; therefore it is possible that people with a high HrQoL are less likely to have symptoms up to 2 years after SARS-CoV-2 infection. This may indicate that healthy adults were less affected by the virus than those who already had some HrQoL-reducing conditions, as suggested in the literature43. The importance of perceived stress also makes sense because it may be a risk factor for an increased number of symptoms25, and having new symptoms may increase your perceived stress. Finally, it is also commonly reported that people of older age are more negatively affected by the infection44,45. We would suggest that people > 50 have a higher risk for decreased HrQoL.
To examine whether pre-existing depressive or anxiety disorder acted as a confounder of the above association with HrQoL, the analysis was stratified according to these conditions. The effect of the identified variables on HrQoL was found to be largely independent of whether or not patients had either disorder at the time of acute SARS-CoV-2 infection or not. All regression models explained at least a moderate amount of variance in HrQoL, and fatigue remained the most important variable. For participants with pre-diagnosed depression or anxiety, the importance of fatigue appears to be greater than the other variables by a greater margin than for those without (Supplementary Fig. S14). The co-occurrence of fatigue and depression is a known phenomenon and might explain this result46. This highlights these comorbidities as potential risk factors for fatigue progression, as suggested by other studies25.
Using the individual dimensions of the EQ-5D-5L, it was found that the selected variables were specifically associated with the Usual Activities dimension. Since chronic fatigue makes usual activities of daily living more difficult, it makes sense that fatigue (probably caused by the infection) would be the cause of the decline in HrQoL.
At 26 months, on average, fatigue was found to be a covariate of HrQoL with an even stronger association, i.e., fatigue becomes increasingly important in reducing HrQoL over time. This is probably the main reason why the amount of explained variance in HrQoL increased to 54% at follow-up, using only one more variable (joint pain). This again highlights the long-term role of fatigue in people after a SARS-CoV-2 infection, as HrQoL is mostly dependent on the intensity of this symptom. At follow-up, the effect of the remaining symptoms seems to be similar, but the decrease in HrQoL for participants with 2 or 3 symptoms became smaller. This could be explained by habituation to the few symptoms they have. The importance of muscle pain appears to be less than at baseline, which would be a positive message for patients that this symptom is less important to HrQoL over time.
The association of the selected variables with the anxiety/depression dimension increased at follow-up, suggesting that mental health becomes more affected over time. This makes sense because it is expected that worry, hopelessness, and social problems will increase the longer the illness lasts. Interestingly, the number of symptoms remaining from the acute phase of COVID-19 became remarkably less important in participants with pre-diagnosed depression or anxiety at follow-up. This further emphasizes that the course of PCS is different in patients with pre-diagnosed depression or anxiety. Treatment should be tailored to the individual pattern of illness. For example, although the majority of PCS patients would likely benefit from psychotherapy, patients with a pre-diagnosed psychiatric illness need a different approach than those without.
In the present study, HrQoL showed a significant improvement from baseline to follow-up. This change was also accompanied by improvements in fatigue, number of symptoms remaining from the acute phase of COVID-19, and perceived stress. However, the best-fitting regression model could not predict more than 1% of the variance in HrQoL improvement from the baseline values of its covariates. This means that the HrQoL at different stages of the recovery from COVID-19 is more dependent on a patient’s current health status than on their status at the onset of PCS. It can be concluded that, although predicting the degree of improvement in HrQoL is complex and requires further research, patients who experience fatigue, a high number of symptoms, stress, and muscle pain at 9 months after SARS-COV-2 infection can still expect their HrQoL to improve if these symptoms improve in the following months.
The study has the following limitations: Many participants had to be excluded due to missing data. Any participant with even one missing value was excluded to ensure a more robust analysis. Although the number of participants is still large enough, it cannot be completely excluded that participants with a higher number of symptoms have missing values, which could lead to bias. Furthermore, it is possible that the magnitude of the association is overestimated because it cannot be proven that all reported symptoms are directly attributable to SARS-CoV-2 infection. However, there is no doubt that they occurred in temporal association with the infection.
In conclusion, the present study showed that HrQoL improved significantly during the first 2 years after SARS-CoV-2 infection and that fatigue, perceived stress and number of remaining symptoms were the main determinants of poor HrQoL, followed by muscle pain, age and joint pain. To improve the HrQoL of PCS patients, future clinical research in this area should therefore focus on the prevention of chronic fatigue, which is the most debilitating and common symptom of PCS and currently has the fewest treatment options. In addition, depression and anxiety as comorbidities should also be taken seriously in the management of PCS patients, as they are important for the HrQoL of patients even 26 months after the initial SARS-CoV-2 infection.
Data availability
The datasets used and/or analysed during the current study available from uac@nukleus.netzwerk-universitaetsmedizin.de on reasonable request. More information is available on the NAPKON website (https://proskive.napkon.de/).
References
World Health Organization. WHO coronavirus (COVID-19) dashboard. https://data.who.int/dashboards/covid19/deaths (2024).
Bikbov, B. & Bikbov, A. Maximum incubation period for COVID-19 infection: Do we need to rethink the 14-day quarantine policy?. Travel Med. Infect. Dis. 40, 101976 (2021).
Bahmer, T. et al. Severity, predictors and clinical correlates of post-COVID syndrome (PCS) in germany: A prospective, multi-centre, population-based cohort study. EClinicalMedicine 51, 101549. https://doi.org/10.1016/j.eclinm.2022.101549 (2022).
Venkatesan, P. NICE guideline on long COVID. Lancet Respir. Med. 9, 129. https://doi.org/10.1016/S2213-2600(21)00031-X (2021).
Callard, F. & Perego, E. How and why patients made long covid. Soc. Sci. Med. 268, 113426. https://doi.org/10.1016/j.socscimed.2020.113426 (2021).
Cohen, J. & Rodgers, Y. V. D. M. Long COVID prevalence, disability, and accommodations: Analysis across demographic groups. J. Occup. Rehabil. 34, 335–349. https://doi.org/10.1007/s10926-024-10173-3 (2024).
AlRasheed, M. M. et al. Quality of life, fatigue, and physical symptoms post-COVID-19 condition: A Cross sectional comparative study. Healthcare 11, 1660. https://doi.org/10.3390/healthcare11111660 (2023).
Lemhoefer, C. et al. Gefuehlte und reale arbeitsfähigkeit von patient*innen mit post-COVID symptomatik nach mildem akutverlauf: Eine analyse des rehabilitation needs questionnaire (RehabNeQ). Phys. Med. Rehab. Kuror. 32, 151–158 (2022).
Ottiger, M., Poppele, I., Sperling, N., Schlesinger, T. & Mueller, K. Work ability and return-to work of patients with post-COVID-19: A systematic review and meta-analysis. BMC Public Health 24, 1811. https://doi.org/10.1186/s12889-024-19328-6 (2024).
Vélez-Santamaría, R. et al. Functionality, physical activity, fatigue and quality of life in patients with acute COVID-19 and Long COVID infection. Sci. Rep. 13, 19907. https://doi.org/10.1038/s41598023-47218-1 (2023).
Herrmann, J. et al. Prospective single-center study of health-related quality of life after COVID-19 in ICU and non-ICU patients. Sci. Rep. 13, 6785. https://doi.org/10.1038/s41598-02333783-y (2023).
Curt, G. A. et al. Impact of cancer related fatigue on the lives of patients: New findings from the fatigue coalition. Oncologist 5, 353–360. https://doi.org/10.1634/theoncologist.5-5-353 (2000).
Davies, K., Dures, E. & Ng, W.-F. Fatigue in inflammatory rheumatic diseases: Current knowledge and areas for future research. Nat. Rev. Rheumatol. 17, 651–664. https://doi.org/10.1038/s41584-021-00692-1 (2021).
Maetzler, W. et al. Fatigue-related changes of daily function: Most promising measures for the digital age. Digit. Biomark. 8, 30–39. https://doi.org/10.1159/000536568 (2024).
Flensner, G., Landtblom, A.-M., Soederhamn, O. & Ek, A.-C. Work capacity and health related quality of life among individuals with multiple sclerosis reduced by fatigue: A cross sectional study. BMC Public Health 13, 224. https://doi.org/10.1186/1471-2458-13-224 (2013).
McCabe, R. M., Grutsch, J. F., Braun, D. P. & Nutakki, S. B. Fatigue as a driver of overall quality of life in cancer patients. PLOS ONE 10, e0130023. https://doi.org/10.1371/journal.pone.0130023 (2015).
Yang, Q. et al. Smell-induced gamma oscillations in human olfactory cortex are required for accurate perception of odor identity. PLOS Biol. 20, e3001509. https://doi.org/10.1371/journal.pbio.3001509 (2022).
Hartung, T. J. et al. Fatigue and cognitive impairment after COVID-19: A prospective multicenter study. EClinicalMedicine 53, 101651. https://doi.org/10.1016/j.eclinm.2022.101651 (2022).
Lee, J.-S., Choi, Y., Joung, J.-Y. & Son, C.-G. Clinical and laboratory characteristics of fatigue dominant long-COVID subjects: A cross-sectional study. Am. J. Med. https://doi.org/10.1016/j.amjmed.2024.01.025 (2024).
Bungenberg, J. et al. Characteristic functional connectome related to Post-COVID-19 syndrome. Sci. Rep. 14, 4997. https://doi.org/10.1038/s41598-024-54554-3 (2024).
Chien, C. et al. Altered brain perfusion and oxygen levels relate to sleepiness and attention in post-COVID syndrome. Ann. Clin. Transl. Neurol. https://doi.org/10.1002/acn3.52121 (2024).
Heine, J. et al. Structural brain changes in patients with post-COVID fatigue: A prospective Observational study. eClinicalMedicine 58, 101874. https://doi.org/10.1016/j.eclinm.2023.101874 (2023).
Hartung, T. J. et al. Predictors of non recovery from fatigue and cognitive deficits after COVID-19: A prospective, longitudinal, population-based study. EClinicalMedicine 69, 102456. https://doi.org/10.1016/j.eclinm.2024.102456 (2024).
Kimura, T., Yokoyama, A., Kohno, N., Nakamura, H. & Eboshida, A. Perceived stress, severity of asthma, and quality of life in young adults with asthma. Allergol. Int. 58, 71–79. https://doi.org/10.2332/allergolint.O-07-531 (2009).
Wang, S. et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of Post–COVID-19 Conditions. JAMA Psychiatry 79, 1081. https://doi.org/10.1001/jamapsychiatry.2022.2640 (2022).
Dheeraj, K. P., Ashfaq, K. & Bindu, P. C. Post-covid symptoms and quality of life among covid-19 survivors. Nursing J. India CXV 3, 117–122. https://doi.org/10.48029/NJI.2024.CXV304 (2024).
Gursoy, E. & Eren, S. The burden of post-COVID-19 syndrome: A cross-sectional study of symptoms and quality of life in a Turkish Sample. Eurasian J. Family Med. 12(3), 159–166. https://doi.org/10.33880/ejfm.2023120307 (2023).
Yalcin-Colak, N., Kader, C., Eren-Gok, S. & Erbay, A. Long-term symptoms and quality of life in persons with COVID-19. Infect. Dis. Clin. Microbiol. 5(3), 212–220. https://doi.org/10.36519/idcm.2023.248 (2023).
Horn, A. et al. Long-term health sequelae and quality of life at least 6 months after infection with SARS-CoV-2: Design and rationale of the COVIDOM-study as part of the NAPKON population Based cohort platform (POP). Infection 49, 1277–1287. https://doi.org/10.1007/s15010-021-01707-5 (2021).
Schons, M. J. et al. The german national pandemic cohort network (NAPKON): Rationale, study Design and baseline characteristics. Eur. J. Epidemiol. 37, 849–870. https://doi.org/10.21203/rs.3.rs-1249111/v1 (2022).
EuroQol Research Foundation. EQ-5D-5L user guide: Basic information on how to use the EQ-5D-5L instrument. https://euroqol.org/wp-content/uploads/2023/11/EQ-5D-5LUserguide-23-07.pdf (2019).
Yellen, S. B., Cella, D. F., Webster, K., Blendowski, C. & Kaplan, E. Measuring fatigue and other anemia-related symptoms with the functional assessment of cancer therapy (FACT) measurement system. J. Pain Symptom Manag. 13, 63–74. https://doi.org/10.1016/s0885-3924(96)00274-6 (1997).
Piper, B. F. & Cella, D. Cancer-related fatigue: Definitions and clinical subtypes. J. Natl. Compr. Cancer Netw. 8, 958–966. https://doi.org/10.6004/jnccn.2010.0070 (2010).
Klein, E. M. et al. The German version of the Perceived Stress Scale – psychometric characteristics in a representative German community sample. BMC Psychiatry 16, 159. https://doi.org/10.1186/s12888-016-0875-9 (2016).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment: MOCA: A BRIEF SCREENING TOOL FOR MCI. J. Am. Geriatr. Soc. 53, 695–699. https://doi.org/10.1111/j.15325415.2005.53221.x (2005).
R Core Team. R: A language and environment for statistical computing. https://www.R-project.org/ (2021).
Kuhn, M. Building predictive models in R using the caret package. J. Stat. Softw. 28, 1–26. https://doi.org/10.18637/jss.v028.i05 (2008).
Hastie, T., Tibshirani, R., Friedman, J. H. & Friedman, J. H. The Elements of Statistical Learning: Data Mining, Inference, and Prediction (Springer, 2009).
James, G., Witten, D., Hastie, T. & Tibshirani, R. An Introduction To Statistical Learning (Springer, 2013).
Liaw, A. & Wiener, M. Classification and regression by randomForest. R News 2, 18–22 (2002).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences (Routledge, 1988).
Yancey, J. R., Hospital, F. B. C. & Belvoir, F. Chronic fatigue syndrome: Diagnosis and treatment. Chronic Fatigue Syndrome 86(8), 741–746 (2012).
Eidininkienė, M., Cesarskaja, J., Talačkaitė, S., Traškaitė-Juškevičienė, V. & Macas, A. Mini review: Co-existing diseases and COVID-19—A one way ticket?. Int. J. Environ. Res. Public Health 19(8), 4738. https://doi.org/10.3390/ijerph19084738 (2022).
Al-Tai, F. & Al-Hamdany, M. The Correlation between Age and Coronavirus Infections. Int. J. Res. Med. Sci. Technol. 14(01), 57–68. https://doi.org/10.37648/ijrmst.v14i01.008 (2022).
CDC COVID-19 Response Team, CDC COVID-19 Response Team, Bialek, S., Boundy, E., Bowen, V., Chow, N., Cohn, A., Dowling, N., Ellington, S., Gierke, R., Hall, A., MacNeil, J., Patel, P., Peacock, G., Pilishvili, T., Razzaghi, H., Reed, N., Ritchey, M. & Sauber-Schatz, E. (2020). Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR. Morbidity and Mortality Weekly Report 69(12), 343–346. https://doi.org/10.15585/mmwr.mm6912e2
Corfield, E. C., Martin, N. G. & Nyholt, D. R. Co-occurrence and symptomatology of fatigue and depression. Compr. Psychiatry 71, 1–10. https://doi.org/10.1016/j.comppsych.2016.08.004 (2016).
Acknowledgements
The study was carried out using the clinical-scientific infrastructure of NAPKON (Nationales Pandemie Kohorten Netz, German National Pandemic Cohort Network) and NUKLEUS (NUM Klinische Epidemiologie- und Studienplattform, NUM Clinical Epidemiology and Study Platform) of the Network University Medicine (NUM), both funded by the Federal Ministry of Education and Research (BMBF). The NUM funding reference number is 01KX2121. We gratefully thank all NAPKON sites who contributed patient data and/or biosamples for this analysis. The representatives of NAPKON sites contributing at least 5 per mille to this analysis are (alphabetical order, representatives in brackets): Charité - Universitaetsmedizin Berlin, Berlin (Fricke J, Kretzler L, Steinbeis F, Treue D, Triller P, Witzenrath M, Zoller T), University Hospital Schleswig-Holstein, Kiel (Brummerloh C, Hermes A, Klamp I, Lehmann I, Meier S, Pape D, Reinke L, Siebert N, Stadler B, Tamminga T, Thomsen-Mascher R), University Hospital Wuerzburg, Wuerzburg (Frantz S, Hein G, Jahns R, Stoerk S, Weissbrich B). We gratefully thank all participating NAPKON infrastructures that contributed to this analysis. The representatives of these NAPKON infrastructures are (alphabetical order, representatives in brackets): University Hospital Cologne, Cologne (Brechtel M, Fiedler K, Lee C, Nunes de Miranda S, Seibel C, Vehreschild JJ), University Hospital Frankfurt, Frankfurt (Appel KS, Geisler R, Hagen M, Schneider J, Sikdar S, Vehreschild JJ, Weismantel C, Wolf L), University of Wuerzburg, Wuerzburg (Fiessler C, Guenther K, Jiru-Hillmann S, Haug F, Haug J, Miljukov O, Reese J-P), University Medicine Greifswald, Greifswald (Bahls T, Hoffmann W, Nauck M, Schaefer C, Schattschneider M, Stahl D, Valentin H), University Medicine Goettingen, Goettingen (Hanß S, Krefting D, Pape C, Rainers M, Schoneberg A, Weinert N), Helmholtz Center Munich, Munich (Kraus M, Lorenz-Depiereux B), Charité - Universitaetsmedizin Berlin, Berlin (Lorbeer R, Schaller J, Fricke J, Roennefarth M), University Hospital Schleswig-Holstein, Kiel (Hermes A, Tamminga T), University Hospital Wuerzburg, Wuerzburg (Kohls M). We gratefully thank the NAPKON Steering Committee: Bielefeld University, Bielefeld (Anton, G), University Hospital Frankfurt, Frankfurt (Ciesek S, Vehreschild M), University Hospital Giessen and Marburg, Giessen (Herold S), University of Wuerzburg, Wuerzburg (Heuschmann P), Charité - Universitaetsmedizin Berlin, Berlin (Heyder R, Witzenrath M), University Medicine Greifswald, Greifswald (Hoffmann W), Hannover Unified Biobank, Hannover Medical School, Hannover (Illig T), University Hospital Schleswig-Holstein, Kiel (Schreiber S), University Hospital Cologne and University Hospital Frankfurt, Cologne and Frankfurt (Vehreschild JJ).
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was funded by the German Federal Ministry of Education and Research (BMBF) [Grant Number 01GM1908D].
Author information
Authors and Affiliations
Contributions
Christian Neumann, Tim Hartung, Walter Maetzler, and Carsten Finke contributed to the study conception and design. Material preparation was performed by Thomas Bahmer, Wolfgang Lieb, Stefan Schreiber, Michael Krawczak, Jan Heyckendorf, Karl Georg Haeusler, Matthias Endres, Peter Heuschmann, Thomas Keil, Lilian Krist, Caroline Morbach, Sein Schmidt, Stefan Stoerk, Walter Maetzler and Carsten Finke. Data collection was performed by Klara Boje, Christian Neumann, Katrin Franzpoetter, Sina M. Pütz, Tim Hartung, Irina Chaplinskaya-Sobol, Johanna Geritz, Corina Maetzler, Felipe Montellano, Carolin Nürnberger, Anne-Kathrin Russ, Lena Schmidbauer and Flo Steigerwald. Analysis was performed by Klara Boje, Christian Neumann and Julius Welzel. The first draft of the manuscript was written by Christian Neumann and Walter Maetzler. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
KGH reports speaker’s honoraria, consulting fees, lecture honoraria and/or study grants from Abbott, Amarin, AstraZeneca, Bayer Healthcare, Biotronik, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Edwards Lifesciences, Medronic, Pfizer, Portola, Premier Research, Sanofi, SUN Pharma, and W.L. Gore and Associates, all of which were unrelated to this work. ME reports grants from Bayer and fees paid to the Charité from Abbot, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, BMS, Daiichi Sankyo, GSK, Sanofi, Covidien, Novartis and Pfizer, all of which were unrelated to this work. TB reports consulting fees, lecture honoraria and/or study grants from AstraZeneca, Boehringer Ingelheim, Pfizer, GlaxoSmithKline, MSD, Chiesi, Novartis, and Roche all of which were unrelated to this work. JK reports consulting fees and salaries from Ababax.Health, all of which were unrelated to this work. CF is supported by EU, DFG and BMBF. WM reports funding from the European Union, the German Federal Ministry of Education of Research, German Research Council, Michael J. Fox Foundation, Robert Bosch Foundation, Neuroalliance, Lundbeck, Sivantos and Janssen, speaker honoraria from Abbvie, Bayer, BIAL, GlaxoSmithKline, Heel, Licher MT, Roelke Pharma, Takeda and UCB, was invited to Advisory Boards / Consultancies of Abbvie, Aptar Digital Health, Atheneum, Biogen, Kyowa Kirin, and Pfizer. The other authors have reported no potential conflicts of interest.
Patient consent and ethics approval
In accordance with the Declaration of Helsinki, written informed consent was obtained from all COVIDOM participants. The study has received ethical approval from the Ethics Committee of the Faculty of Medicine at the Christian Albrecht University in Kiel, Germany (reference numbers: Kiel D537/20, also valid for the Berlin site) and from the Ethics Committee of the Institute for Pharmacology and Toxicology of the Julius Maximilians University in Wuerzburg, Germany (236/20_z-am). COVIDOM was registered in the German Registry of Clinical Studies (DRKS00023742) and in ClinicalTrials.gov (NCT04679584).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Neumann, C., Hartung, T.J., Boje, K. et al. Factors associated with reduction in quality of life after SARS-CoV-2 infection. Sci Rep 15, 6833 (2025). https://doi.org/10.1038/s41598-025-91388-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91388-z
Keywords
This article is cited by
-
Health-related quality of life in COVID-19 patients: a systematic review and meta-analysis of EQ-5D studies
Health and Quality of Life Outcomes (2025)
-
Pre-pandemic disease trajectories and genetic insights into long COVID susceptibility
BMC Medicine (2025)
-
Post-Covid-19 symptoms, subjective work ability and sick leave 2 years after acute infection—results from a population-based long COVID study
BMC Public Health (2025)