Abstract
Stroke is the second leading cause of death globally. Oxidative stress plays a critical role in the development of stroke. The Oxidative Balance Score (OBS) is a tool used to assess the combined impact of diet and lifestyle on the body’s antioxidant capacity. The study included stroke survivors from the National Health and Nutrition Examination Survey (1999–2018), with a total of 1,781 participants and a median follow-up duration of 6.5 years, during which 786 participants (39.59%) died. The relationship between OBS and all-cause mortality was assessed using the Cox proportional hazards model. The results indicated that individuals in higher OBS quartiles had lower mortality rates. Specifically, patients in the fourth quartile had a 41% reduced risk of all-cause mortality compared to those in the first quartile (HR = 0.59, 95% CI = 0.42–0.84, p = 0.003). Restricted cubic spline analysis revealed a linear inverse relationship between OBS and all-cause mortality. Subgroup analysis further demonstrated that the inverse association persisted across various population subgroups. Overall, our study suggests that higher levels of OBS can reduce the risk of all-cause mortality in stroke survivors and provides new evidence for their diet and lifestyle.
Similar content being viewed by others
Introduction
Stroke is an acute cerebrovascular disease clinically characterized by a sudden onset and rapid development of localized or diffuse neurological deficits1. Stroke is a disease with high incidence, disability, and mortality rates, making it the second leading cause of death worldwide2. Research indicates that in 2019, approximately 12.2 million stroke cases occurred globally, leading to 6.6 million deaths, with over 101 million people having a history of stroke3. Furthermore, cohort study indicates that the average age of adults hospitalized due to a first-time stroke is 73 years4. The life expectancy of patients with acute stroke is approximately 5.5 years shorter than that of the general population4. Stroke has become a major global public health challenge, and researchers are continuously striving to improve outcomes by studying its risk factors.
The pathophysiology of stroke is extremely complex, and as research advances, growing evidence suggests that the occurrence and progression of stroke involve various pathophysiological processes such as excitotoxicity5, oxidative stress6, mitochondrial dysfunction7, inflammatory responses8, and blood-brain barrier damage9. Despite significant progress in understanding the underlying mechanisms of stroke, current pharmacological interventions and treatments still have limitations10. Oxidative stress is considered a key driver of aging and various chronic diseases, including stroke. Studies have shown that the balance between oxidation and antioxidant systems in the body is crucial for lifespan, when oxidative stress levels increase, they may lead to cell damage, DNA mutations, and protein dysfunction, thereby accelerating tissue aging and shortening lifespan11.Given the critical role of oxidative stress in stroke and lifespan, increasing attention has been directed toward enhancing the body’s antioxidant capacity to improve stroke outcomes12.
Traditional methods of measuring oxidative stress typically rely on single biomarkers, such as 8-hydroxy2’-deoxyguanosine (8-OHdG)13 and malondialdehyde(MDA)14, to assess oxidative stress levels. These methods often only reflect short-term oxidative stress and may be influenced by individual differences and environmental factors. Furthermore, many traditional methods require invasive blood sampling. Due to the limitations of traditional methods for measuring oxidative stress and the urgent need for a new measurement approach, the Oxidative Balance Score (OBS) was developed. The OBS consists of 20 components, calculated based on the antioxidant and pro-oxidant components in diet and lifestyle, serving as a comprehensive indicator for evaluating an individual’s redox balance15. Generally, a higher OBS value indicates stronger antioxidant activity, while a lower OBS value suggests greater pro-oxidant activity. Compared to traditional measurement methods, the OBS provides a more accurate reflection of an individual’s long-term oxidative stress levels by considering long-term lifestyle and dietary patterns. Moreover, since the OBS does not involve invasive procedures, it is particularly suitable for long-term monitoring and repeated measurements. The OBS has been widely used to assess relationships with other chronic diseases, including metabolic-associated fatty liver disease16, cancer17, and depression18. Recent studies indicate that a higher OBS is associated with a lower risk of mortality in the general population19.However, research on the relationship between OBS and stroke remains limited.
The National Health and Nutrition Examination Survey (NHANES) is a national, multi-stage, large-scale study organized by the National Center for Health Statistics (NCHS), primarily collecting data on the nutrition and health of the U.S. population.
Therefore, this study utilizes data from the NHANES to evaluate the relationship between OBS and all-cause mortality among stroke survivors in the United States.
Materials and methods
The National Health and Nutrition Examination Survey (NHANES), sponsored by the National Center for Health Statistics (NCHS), is a nationally representative survey designed to assess the health and nutritional status of the U.S. population. NHANES employs a complex, stratified, multistage sampling design to ensure the selection of a representative sample from the population. Data collection methods include structured household interviews, mobile examination center visits, and laboratory tests.
Study design and population
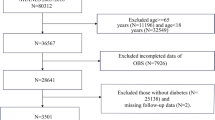
Data were extracted from NHANES, covering ten cycles from 1999 to 2018. The exclusion criteria in this study were as follows: (1) participants with incomplete stroke data (n = 46,311); (2) participants without a diagnosed stroke (n = 52,740); (3) participants with missing information on other relevant variables (n = 483); (4) participants without follow-up data (n = 1). Finally, 1,781 participants were included in our study (Fig. 1). We used the deletion method to handle missing data.
Definition of stroke
Stroke was determined based on self-reported prior diagnoses by a physician during face-to-face interviews. Individuals who responded affirmatively to the question, “Has a doctor or other health professional ever told you that you had a stroke?” were considered to have had a stroke. The diagnosis of such questionnaire-based self-reported illnesses has been shown to have good agreement and has been widely used in NHANES-related epidemiologic studies20,21.
Evaluation of oxidative balance score22
The calculation of the OBS is based on 16 dietary nutrients and 4 lifestyle factors, including 15 antioxidant components and 5 pro-oxidant components. These 16 nutrients were derived from the first dietary recall interview and include dietary fiber, carotenoids, riboflavin, niacin, vitamin B6, total folate, vitamin B12, vitamin C, vitamin E, calcium, magnesium, zinc, copper, selenium, total fat, and iron. The 4 lifestyle factors are physical activity, body mass index (BMI), alcohol consumption, and smoking, with the level of smoking evaluated based on cotinine levels. The 15 antioxidant components include dietary fiber, carotenoids, riboflavin, niacin, vitamin B6, total folate, vitamin B12, vitamin C, vitamin E, calcium, magnesium, zinc, copper, selenium, and physical activity. The 5 pro-oxidant components include total fat, iron, body mass index, alcohol consumption, and cotinine, while the remaining factors are classified as antioxidant factors. Each component is stratified by sex and scored based on tertiles. For antioxidant components, the scores are assigned as 0, 1, and 2 for the lowest, middle, and highest tertiles, respectively. In contrast, the scores for pro-oxidant components are inversely related to their tertiles, with the highest tertile receiving 0 points and the lowest tertile receiving 2 points. The overall OBS is the sum of the scores of each component, with a total score range of 3 to 36. The specific distribution criteria of OBS components are in Supplementary Table S123.
Assessment of mortality
To determine the mortality status in the follow-up population, we utilized the NHANES public-use linked mortality file, updated as of December 31, 2019. This file underwent linkage with the National Death Index (NDI) by the NCHS using a probability matching algorithm20,24.
Covariates
In this study, we considered several covariates which could potentially confound the outcomes16,25. These variables encompassed demographic characteristics, dietary confounding factors, and risk factors associated with stroke. The demographic characteristics included (1) age; (2) sex (male and female); (3) race (Mexican American, White, Black, and other races); and (4) education level (below high school, high school, and more than high school). Dietary confounding factors consisted of total energy intake and Healthy Eating Index-2015 score (HEI-2015 score)26 to eliminate the effect of energy intake and diet quality. As for the risk factors related to stroke, we accounted for diabetes (yes/no), hypertension (yes/no), and hyperlipidemia (yes/no). Additionally, BMI was also adjusted for in the analysis to ensure their influence on the outcomes was appropriately considered. Details of all these variables, including measurement methods, questionnaire data, and variables list, are available on the official NHANES website (www.cdc.gov/nchs/nhanes/).
Statistical analyses
To ensure that the data are representative of the U.S. population, we applied the weights recommended by the NCHS. Baseline characteristics were represented by the quartiles of the OBS. Continuous variables were expressed as mean ± standard deviation, and categorical variables as frequency and percentage. Continuous variables were compared using analysis of variance (ANOVA), and categorical variables were compared using chi-square tests. We used multivariable Cox regression models to assess the relationship between OBS and all-cause mortality, with results presented as regression coefficients and 95% confidence intervals (CIs). The original model was unadjusted, and Model 1 adjusted for age, gender, race, and education level. The original model was unadjusted, and Model 1 adjusted for age, gender, race, and education level. Model 2 further adjusted for energy intake and the 2015 Healthy Eating Index (HEI-2015) on top of Model (1) Model 3 further adjusted for BMI, diabetes, hypertension, and hyperlipidemia on top of Model (2) To compare survival probabilities, we performed Kaplan-Meier (KM) survival analysis. To visually depict the relationship between OBS and all-cause mortality in stroke survivors, we constructed a restricted cubic spline (RCS) model based on the fully adjusted model. Furthermore, we conducted subgroup analyses based on the fully adjusted model to explore the relationship between OBS and all-cause mortality across different subgroups. A p-value of less than 0.05 was considered statistically significant. All analyses were performed using R software, version 4.2.4.
Results
Baseline characteristics of the study population
Table 1 provides a comprehensive overview of the survey-weighted characteristics of the study population, showing the baseline characteristics of participants based on OBS quartiles. A total of 1,781 stroke survivors were included in the study, of whom 893 (56.32%) were female, and 905 (69.84%) were non-Hispanic white, with a mean age of 63.71 years. During a median follow-up of 6.5 years (interquartile range = 37–124 months), 786 participants (39.59%) died. Significant differences (p < 0.05) were observed across OBS quartiles in terms of age (p = 0.01), race (p < 0.0001), education level (p < 0.0001), BMI (p = 0.02), total energy intake (p < 0.0001), and HEI-2015 score (p < 0.0001). Compared to participants with lower OBS scores (Q1), those with higher OBS scores exhibited higher total energy intake, higher HEI-2015 score, and lower BMI. These high-scoring participants tended to be non-Hispanic whites with higher education levels. There were significant differences in all-cause mortality across OBS quartiles, with higher OBS scores associated with lower mortality rates.
Associations between OBS and all-cause mortality
Table 2 shows the results of the Cox regression analysis assessing the relationship between OBS and all-cause mortality in stroke survivors. As a continuous variable, in the unadjusted model, each one-unit increase in OBS was associated with a 2% reduction in all-cause mortality (hazard ratios (HR) = 0.98, 95% CI = 0.97–0.99, p = 0.004). After multivariable adjustments, the results remained robust and statistically significant in Model 1 (HR = 0.98, 95% CI = 0.97–0.99, p = 0.001), Model 2 (HR = 0.98, 95% CI = 0.97–0.99, p = 0.01), and Model 3 (HR = 0.98, 95% CI = 0.97–0.99, p = 0.004). As a quartile variable, in the model3 adjusting for all covariates, compared with participants inQ1, multivariate HRs for all-cause mortality were 0.70(95% CI = 0.55–0.89, p = 0.004) for Q2, 0.75(95% CI = 0.58–0.96, p = 0.02)for Q3, and 0.59(95% CI = 0.58–0.96, p = 0.003)for Q4 (p for trend = 0.007).
The Kaplan-Meier survival curves based on OBS quartiles are shown in Fig. 2. The Kaplan-Meier analysis revealed significant differences in all-cause mortality across different OBS levels (p = 0.002). Participants with higher OBS scores had significantly improved survival rates compared to those with lower OBS scores. Moreover, we used the RCS model to divide the data into smaller intervals to effectively evaluate the nonlinear relationships (Fig. 3). This model revealed a linear relationship between OBS and all-cause mortality (p = 0.0038).
Subgroup analyses
Subgroup analyses were stratified by age, sex, race, education level, diabetes, hypertension, and hyperlipidemia. When treating OBS as a continuous variable, the association between OBS and all-cause mortality remained consistent and reliable, with no significant interactions, as shown in the forest plot in Fig. 4. A statistically significant negative association between OBS and all-cause mortality was observed in participants over 60 years old (HR = 0.98, 95% CI = 0.96–0.99), females (HR = 0.97, 95% CI = 0.95–0.99), non-Hispanic white participants (HR = 0.97, 95% CI = 0.96–0.99), Mexican participants (HR = 0.96, 95% CI = 0.92–1.00), participants with below high school education (HR = 0.98, 95% CI = 0.96–1.00), participants with diabetes (HR = 0.97, 95% CI = 0.95–1.00), participants with hypertension (HR = 0.98, 95% CI = 0.96–0.99), and participants with hyperlipidemia (HR = 0.98, 95% CI = 0.96–0.99).
Discussion
In this study, by analyzing a representative sample of stroke survivors from the NHANES database, we found that the OBS was negatively correlated with all-cause mortality. Patients in the highest OBS quartile had a significantly lower risk of all-cause mortality compared to those in the lowest quartile. To our knowledge, this is the first study to explore the relationship between OBS and all-cause mortality in stroke survivors. In view of the negative correlation between OBS and all-cause mortality, improving OBS of stroke survivors may be a promising intervention goal. In the future, we can consider using dietary antioxidants or making personalized lifestyle adjustment programs to improve patients’ OBS scores, thus improving their survival rate and quality of life.
Our study found that in the unadjusted model, for each additional unit of OBS is associated with a 2% reduction in the all-cause mortality rate among stroke survivors. This suggests that a higher OBS is associated with a lower all-cause mortality rate, indicating its potential significance and positive impact in preventing all-cause mortality among stroke survivors.
In our study, the average age of stroke survivors was greater than 60 years, which is consistent with the findings of other studies27. Additionally, our study revealed that older stroke survivors had poorer prognoses. This may be related to the increased likelihood of complications in elderly individuals following a stroke. Furthermore, we also observed that the inclusion of different confounding factors (models 1, 2, and 3) did not significantly affect the results in our study. Possible reasons include firstly, although these confounding factors are generally associated with outcomes in stroke survivors, their impact on the results in this study may be relatively small; secondly, there may be strong correlations among these confounding factors, which makes it difficult to distinguish their independent effects, thereby preventing any significant impact on the results.
Stroke is the second leading cause of death worldwide, following ischemic heart disease2. However, current pharmacological treatments for stroke still have certain limitations10. In contrast, oxidative stress treatment is considered a potentially effective strategy for preventing and treating stroke, with significant clinical prospects. In terms of diet, unhealthy dietary habits, such as high cholesterol and high-fat diets, can exacerbate chronic inflammation and promote stroke development21. Conversely, high-quality dietary patterns, such as the Mediterranean diet and the DASH diet (Dietary Approaches to Stop Hypertension), have been shown to have protective effects against stroke28,29,30. The Mediterranean diet has been extensively studied for its role in stroke prevention. This diet is characterized by the consumption of a variety of fruits, vegetables, and whole grains, along with legumes, nuts, low-fat dairy, olive oil, and fish, while limiting the intake of red meat, salt, and carbohydrates31. A case-control study conducted in Iran found that adherence to the MIND diet was inversely associated with stroke incidence32. In additional, study has shown that increasing the intake of antioxidant bioactive compounds, such as vitamin A, vitamin C, and carotenoids, helps improve stroke prognosis12,29,33. This is consistent with our findings. Moreover, numerous studies have shown that physical activity is inversely associated with stroke risk. This association is observed not only in individuals who engage in vigorous physical activity but also in those who maintain light to moderate levels of exercise. To put it simply, different types, frequencies, and intensities of physical activity can provide significant benefits in the prevention and treatment of stroke34,35. Conversely, pro-oxidant factors such as smoking increase the production of ROS. Studies have shown that smoking reduces the generation of nitric oxide and elevates oxidative stress levels, leading to endothelial dysfunction and promoting the early development of atherosclerosis36. This is consistent with our findings. In our study, the comprehensive inclusion of antioxidants and pro-oxidants from dietary and lifestyle sources enables a more thorough and complete assessment of oxidative stress through the OBS.
Under physiological conditions, a balance exists between the production of reactive oxygen species (ROS) and cellular antioxidant defense mechanisms37. When this balance is disrupted, leading to an overproduction of ROS, which in turn activates pathways such as IKK/NF-KB, JNK/SAPK, and PI3-K38,39.Although the exact mechanisms linking OBS with the mortality risk of stroke survivors are not fully understood, current research has revealed several potential biological pathways: (1) ROS promote cell proliferation by activating signaling pathways such as MAPK and NF-κB and enhance cancer cell survival by inhibiting apoptosis. Additionally, ROS can alter the tumor microenvironment, promoting tumor angiogenesis, inflammatory responses, and immune escape, all key drivers of tumor progression40. (2) ROS oxidize low-density lipoprotein (LDL) to form oxidized LDL (ox-LDL), which is then ingested by macrophages and converted into foam cells, promoting the formation of atherosclerotic plaques; oxidative stress further damages vascular endothelial cells, inhibits nitric oxide synthesis, and impairs vasodilation, thereby increasing the risk of hypertension41. (3) ROS damage pancreatic β-cells, inhibiting their insulin secretion function, leading to insulin deficiency and accelerating the onset of diabetes. Furthermore, oxidative stress is closely related to the formation of insulin resistance. ROS interfere with insulin receptor signaling, reducing cellular sensitivity to insulin and exacerbating metabolic abnormalities in diabetes. ROS also induce inflammatory responses and promote cell apoptosis, causing vascular dysfunction and tissue hypoxia, which in turn lead to diabetic complications, especially microvascular damage, such as diabetic retinopathy and nephropathy42. (4) ROS are associated with the loss of synaptic function and protein aggregation in neurons, and ROS-induced neuronal damage accelerates the progression of neurodegenerative diseases, resulting in a gradual decline in cognitive and motor functions43. (5) ROS accumulation is considered a primary driver of cellular aging and organ function deterioration, as it accelerates telomere shortening, leading to cellular senescence and a decline in tissue regenerative capacity44.
Our study has several strengths. First, this is the first large-scale observational study aimed at evaluating the relationship between OBS and all-cause mortality in stroke survivors. Second, we extensively adjusted for a variety of potential confounders, including demographic variables, dietary confounding factors, and comorbidities, and further confirmed the robustness of our results through subgroup analysis. Lastly, our study is based on a nationwide epidemiological survey, and we employed appropriate weighting methods to ensure that the sample is representative and reflects the characteristics of the general population, thereby ensuring the representativeness and generalizability of our findings.
This study has some notable limitations. Firstly, the study population primarily consists of Americans, which may limit the applicability of the results to different ethnicities and living environments. Further research is needed to validate whether our main findings are applicable to other countries. Secondly, the definition of stroke in NHANES relies on self-reported questionnaires rather than specific imaging examinations, which may limit the accuracy of stroke diagnosis. Therefore, future research should aim to reduce such biases by using more accurate stroke diagnostic methods, such as clinical evaluation or imaging confirmation. Thirdly, although we adjusted for various potential confounders, there are still some unknown factors that we could not control for. Therefore, prospective randomized controlled trials are needed in the future to validate our findings further.
Conclusion
In summary, we found a negative correlation between OBS and all-cause mortality in stroke survivors (based on self-reports to define the occurrence of stroke). A higher OBS score indicates greater exposure to antioxidant factors relative to pro-oxidant factors in diet and lifestyle, which is associated with lower all-cause mortality. Our study provides new evidence for the diet and lifestyle of stroke survivors. Furthermore, future longitudinal or interventional studies are needed to further validate and expand our findings.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
References
Mendelson, S. J. & Prabhakaran, S. Diagnosis and management of transient ischemic attack and acute ischemic stroke: A review. JAMA 325 (11), 1088–1098 (2021).
Virani, S. S. et al. Heart disease and stroke Statistics-2020 update: A report from the American heart association. Circulation 141 (9), e139–e596 (2020).
Collaborators, G. S. Global, regional, and National burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 20 (10), 795–820 (2021).
Peng, Y. et al. Stroke recurrence, and life expectancy after an acute stroke in Australia and new Zealand from 2008–2017: A Population-Wide cohort study. Stroke 53 (8), 2538–2548 (2022).
Lai, T. W., Zhang, S. & Wang, Y. T. Excitotoxicity and stroke: identifying novel targets for neuroprotection. Prog Neurobiol. 115, 157–188 (2014).
Qin, C. et al. Signaling pathways involved in ischemic stroke: molecular mechanisms and therapeutic interventions. Signal. Transduct. Target. Ther. 7 (1), 215 (2022).
George, P. M. & Steinberg, G. K. Novel stroke therapeutics: unraveling stroke pathophysiology and its impact on clinical treatments. Neuron 87 (2), 297–309 (2015).
DeLong, J. H., Ohashi, S. N., O’Connor, K. C. & Sansing, L. H. Inflammatory responses after ischemic stroke. Semin Immunopathol. 44 (5), 625–648 (2022).
Abdullahi, W., Tripathi, D. & Ronaldson, P. T. Blood-brain barrier dysfunction in ischemic stroke: targeting tight junctions and transporters for vascular protection. Am. J. Physiol. Cell. Physiol. 315 (3), C343–C356 (2018).
Tsivgoulis, G. et al. Thrombolysis for acute ischaemic stroke: current status and future perspectives. Lancet Neurol. 22 (5), 418–429 (2023).
Wu, Z., Qu, J., Zhang, W. & Liu, G. H. Stress, epigenetics, and aging: unraveling the intricate crosstalk. Mol. Cell. 84 (1), 34–54 (2024).
Teng, T. Q. et al. Association of composite dietary antioxidant index with prevalence of stroke: insights from NHANES 1999–2018. Front. Immunol. 15, 1306059 (2024).
Graille, M. et al. Urinary 8-OHdG as a biomarker for oxidative stress: A systematic literature review and Meta-Analysis. Int. J. Mol. Sci. 21 (11), 3743 (2020).
Nielsen, F., Mikkelsen, B. B., Nielsen, J. B., Andersen, H. R. & Grandjean, P. Plasma malondialdehyde as biomarker for oxidative stress: reference interval and effects of life-style factors. Clin. Chem. 43 (7), 1209–1214 (1997).
Goodman, M., Bostick, R. M., Dash, C., Flanders, W. D. & Mandel, J. S. Hypothesis: oxidative stress score as a combined measure of pro-oxidant and antioxidant exposures. Ann. Epidemiol. 17 (5), 394–399 (2007).
Tan, Z. et al. Trends in oxidative balance score and prevalence of metabolic Dysfunction-Associated steatotic liver disease in the united States: National health and nutrition examination survey 2001 to 2018. Nutrients 15 (23), 4931 (2023).
Park, Y. M. et al. Dietary inflammatory potential, oxidative balance score, and risk of breast cancer: findings from the sister study. Int. J. Cancer. 149 (3), 615–626 (2021).
Liu, X. et al. Association between depression and oxidative balance score: National health and nutrition examination survey (NHANES) 2005–2018. J. Affect. Disord. 337, 57–65 (2023).
Wu, J. et al. The impact of oxidative balance on all-cause and cause-specific mortality in US adults and cancer survivors: evidence from NHANES 2001–2018. BMC Cancer. 25 (1), 133 (2025).
Yuan, J. et al. Association between C-reactive protein/albumin ratio and all-cause mortality in patients with stroke: evidence from NHANES cohort study. Nutr. Metab. Cardiovasc. Dis. : (2024). S0939-4753(24)00208-4 [pii].
Mao, Y. et al. Association between dietary inflammatory index and stroke in the US population: evidence from NHANES 1999–2018. BMC Public. Health. 24 (1), 50 (2024).
Xu, Z. et al. Association between the oxidative balance score and all-cause and cardiovascular mortality in patients with diabetes and prediabetes. Redox Biol. 76, 103327 (2024).
Zhang, W. et al. Association between the Oxidative Balance Score and Telomere Length from the National Health and Nutrition Examination Survey 1999–2002. Oxid Med Cell Longev. 2022: 1345071. (2022).
Yang, M., Miao, S., Hu, W. & Yan, J. Association between the dietary inflammatory index and all-cause and cardiovascular mortality in patients with atherosclerotic cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 34 (4), 1046–1053 (2024).
Chen, J. et al. Adherence to oxidative balance score is inversely associated with the prevalence of stroke: results from National health and nutrition examination survey 1999–2018. Front. Neurol. 15, 1348011 (2024).
Wang, K. et al. Associations of oxidative balance score with hyperuricemia and gout among American adults: a population-based study. Front. Endocrinol. (Lausanne). 15, 1354704 (2024).
Wang, W. et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide Population-Based survey of 480 687 adults. Circulation 135 (8), 759–771 (2017).
Hankey, G. J. Nutrition and the risk of stroke. Lancet Neurol. 11 (1), 66–81 (2012).
Spence, J. D. Nutrition and risk of stroke. Nutrients 11 (3), 647 (2019).
Song, Y. et al. Better adherence to the MIND diet is associated with lower risk of all-cause death and cardiovascular death in patients with atherosclerotic cardiovascular disease or stroke: a cohort study from NHANES analysis. Food Funct. 14 (3), 1740–1749 (2023).
Widmer, R. J., Flammer, A. J., Lerman, L. O. & Lerman, A. The mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 128 (3), 229–238 (2015).
Salari-Moghaddam, A. et al. The association between adherence to the MIND diet and stroke: a case-control study. Nutr. Neurosci. 25 (9), 1956–1961 (2022).
Farashi, S., Shahidi, S., Sarihi, A. & Zarei, M. Association of vitamin A and its organic compounds with stroke - a systematic review and meta-analysis. Nutr. Neurosci. 26 (10), 960–974 (2023).
Ghozy, S. et al. Physical activity level and stroke risk in US population: A matched case-control study of 102,578 individuals. Ann. Clin. Transl Neurol. 9 (3), 264–275 (2022).
Kyu, H. H. et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ 354, i3857 (2016).
Ambrose, J. A. & Barua, R. S. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J. Am. Coll. Cardiol. 43 (10), 1731–1737 (2004).
Turrens, J. F. & Boveris, A. Generation of superoxide anion by the NADH dehydrogenase of bovine heart mitochondria. Biochem. J. 191 (2), 421–427 (1980).
Houstis, N., Rosen, E. D. & Lander, E. S. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440 (7086), 944–948 (2006).
Samantha, H. & Walter, H. H. The etiology of oxidative stress in insulin resistance. Biomedical J. 40 (5), 257–262 (2017).
Hayes, J. D., Dinkova-Kostova, A. T. & Tew, K. D. Oxidative stress in Cancer. Cancer Cell. 38 (2), 167–197 (2020).
Vekic, J. et al. Oxidative stress, atherogenic dyslipidemia, and cardiovascular risk. Biomedicines 11 (11), 2897 (2023).
Singh, A., Kukreti, R., Saso, L. & Kukreti, S. Mechanistic insight into oxidative Stress-Triggered signaling pathways and type 2 diabetes. Molecules 27 (3), 950 (2022).
Dionísio, P. A., Amaral, J. D. & Rodrigues, C. Oxidative stress and regulated cell death in Parkinson’s disease. Ageing Res. Rev. 67, 101263 (2021).
Wu, Z., Qu, J. & Liu, G. H. Roles of chromatin and genome instability in cellular senescence and their relevance to ageing and related diseases. Nat. Rev. Mol. Cell. Biol. 25 (12), 979–1000 (2024).
Acknowledgements
The authors thank the staff and the participants of the NHANES study for their valuable contributions.
Funding
This work was sponsored by a major Research Project of National Clinical Key Specialties of Hunan Provincial Health Commission(Z2023127), Hunan Provincial Natural Science Foundation Regional Joint Fund(2023JJ50372), Research Project of Hunan Provincial Health Commission (D202303077684), Xiangnan University College-level Research Project (2022JX109), and Chenzhou Stroke Technology Research and Development Center.
Author information
Authors and Affiliations
Contributions
J.L., Z.L. and W.D. were involved in the experiment design. L.D., H.T., H.L., and H.H. performed the data analysis, and JL wrote the primary manuscript. Q.L., and H.L. reviewed and revised the manuscript. All the authors have approved the manuscript for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the NCHS Research Ethics Review Board (ERB). All participants provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lei, J., Liao, Z., Duan, W. et al. Association between oxidative balance score and all-cause mortality in stroke survivors. Sci Rep 15, 7628 (2025). https://doi.org/10.1038/s41598-025-91721-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91721-6