Abstract
This study evaluated the efficacy and safety of stellate ganglion block (SGB) combined with trioxygen autologous blood retransfusion therapy (TABRT) in treating postherpetic neuralgia (PHN) of the head and face in elderly patients. A total of 190 patients (aged ≥ 60 years) with PHN were randomly assigned to receive either drug treatment alone (Group D, n = 40), drug treatment with SGB (Group DS, n = 52), drug treatment with TABRT (Group DT, n = 53), or drug combined SGB with TABRT (Group DST, n = 45). Key outcomes included pain visual analogue scale (VAS) scores and anxiety levels at baseline, 7 days, and 15 days post-treatment, the need for salvage analgesics, and complication rates assessed. All groups showed significant improvements in pain and anxiety, with greater reductions in the DS, DT, and DST groups compared to the drug-only group, and the combined therapy (DST) showing the most pronounced benefits. The DST group also had the highest proportion of patients not requiring rescue analgesics and the highest complete remission rate. Overall, the combination of SGB and TABRT was found to be effective and safe, offering superior therapeutic outcomes compared to single therapies for elderly patients with PHN of the head and face.
Similar content being viewed by others
Introduction
Postherpetic neuralgia (PHN) is the most common chronic complication of Herpes zoster1 and manifests as severe refractory neuropathic pain2,3,4,5. Herpes zoster involving the head and face has an incidence rate of approximately 20%. PHN develops in 9–34% of cases following acute herpesvirus infection, with the rate rising significantly to 65–73% among individuals over 60 years old. Furthermore, 30–50% of patients experience symptoms lasting longer than one year, with some enduring pain for more than a decade. Predominantly affecting older adults, PHN severely6 impairs quality of life by causing intense pain, prolonged disease duration, emotional anxiety, poor sleep quality, and high treatment costs with often limited efficacy7,8. As the global population continues to age, the prevalence of PHN is expected to rise, highlighting the urgent need for improved preventive measures, effective therapies, and comprehensive management strategies.
Conventional anti-neuropathic drugs combined with early interventional treatment are considered the best approach3,9, but their effectiveness is often limited, and treatment failure is particularly high in cases of craniofacial PHN. Patients with herpes zoster affecting the facial and upper limb regions are particularly vulnerable to severe pain and the subsequent development of PHN due to nerve damage10. The etiology and mechanisms behind PHN remain elusive, and no consistently effective treatments are available. The complex anatomy and the specific nature of pain in these regions further complicate treatment, leading to high failure rates and limited options11. As a result, there is an urgent need for more effective treatment methods12, prompting pain specialists to explore innovative approaches, such as adjusting treatment parameters or combining various therapies8.
Stellate ganglion block (SGB) is a method used to treat various conditions by blocking the stellate ganglia. Its primary mechanism involves regulating autonomic nerve function, aiming to modulate and restore balance within the autonomic nervous system. It is a well-studied modality in chronic pain management, especially for craniofacial pain. It is indicated for complex regional pain syndrome, postherpetic neuralgia, cancer pain, and head and face pain13,14. Clinical practice and literature have demonstrated that SGB is safe and effective for PHN15. However, some patients do not experience satisfactory pain relief with SGB alone, prompting the consideration of combined therapies. Although there is limited literature on this, some studies have shown that SGB combined with other treatments, like shock wave therapy, can significantly improve pain symptoms in PHN patients16. Additionally, trioxygen autologous blood retransfusion therapy (TABRT) combined with radiofrequency has been effective in relieving thoracic PHN in elderly patients17.
TABRT involves drawing a small sample of the patient’s blood, treating it with ozone, and reinfusing it back into the patient. Studies have shown that this procedure can enhance tissue oxygenation18, improve microcirculation, promote nerve repair, and alleviate pain19,20 by reducing factors such as NADH21, interleukin, tumor necrosis factor-α, and so on. Additionally, TABRT generates reactive oxygen species (ROS) and lipid oxidation products (LOPs)22, which activate nuclear transcription factors and interact directly or indirectly with transmembrane proteins, contributing to its therapeutic effects in pain management. TABRT when combined with pharmacological therapy, has been shown to be superior to isolated pharmacological therapy in PHN patients, providing an effective and safe method for pain relief12,23 However, literature on the use of TABRT for PHN, particularly in combination with other therapies, is sparse. Therefore, we considered TABRT combined with SGB therapy to treat head and facial PHN in the elderly. We aimed to evaluate the effectiveness and safety of combining SGB and TABRT for treating PHN in elderly patients with head and face involvement, comparing this combination therapy to the individual treatments.
Materials and methods
Patients
The research protocol was approved by the Ethics Committee of the First Affiliated Hospital of Xiamen University and all methods were performed in accordance with the relevant guidelines and regulations. From January 2017 to December 2022, elderly (over 60 years old) patients with head and face PHN were recruited from the First Affiliated Hospital of Xiamen University. A total of 648 cases were initially included in the study. However, 425 cases were excluded for various reasons: 43 patients were unwilling to participate, and 382 did not meet the inclusion criteria. The reasons for non-compliance were as follows: abnormal coagulation function (n = 13), hyperthyroidism (n = 65), arrhythmia (n = 23), mental abnormality or use of psychotropic drugs other than the plan (n = 28), difficulty in accurate VAS scoring due to communication issues (n = 42), data incomplete data collection (n = 211), discontinuation of participation (n = 13) due to failure to complete the 15-day treatment plan, stopping treatment midway, or using other treatment methods such as local injection, acupuncture, red light irradiation, or laser treatment. Ultimately, 190 patients completed the study (Fig. 1). Written informed consent was obtained from each participant.
Research flowchart. The D group received only standard drug treatment. The DS group received stellate ganglion block therapy in addition to drug treatment. The DT group received trioxygen autologous blood retransfusion therapy alongside drug treatment. The DST group received both stellate ganglion block therapy and trioxygen autologous blood retransfusion therapy in combination with drug treatment. D drug therapy, DS drug combined stellate ganglion block therapy, DT drug combined trioxygen autologous blood retransfusion therapy, DST drug combined stellate ganglion block and trioxygen autologous blood retransfusion therapy.
Patient composition and follow-up
Patients were randomly assigned to one of four groups using a random drawing method with four differently colored balls, ensuring no statistically significant differences in baseline characteristics among the groups before treatment. Group 1 (D Group) received drug treatment only; Group 2 (DS Group) received drug treatment combined with SGB; Group 3 (DT Group) received drug treatment combined with TABRT; and Group 4 (DST Group) received drug treatment combined with both SGB and TABRT. All treatments were conducted by the same team of doctors and nurses, while follow-up visits were performed by a designated nurse who was not involved in other aspects of the study (Fig. 1).
Equipment and drugs
The equipment used in this study includes GE Ultrasound Instruments (VENUE 50 GE Healthcare, Chicago, IL), Trioxygen therapy apparatus (HYPER-MEDOZON comfort, Hermann Equipment Manufacturing GmbH, Germany).
The drugs used here are Tramadol (Beijing Menti Pharmaceutical Co., Ltd., Beijing, China), Pregabalin (Puyuelin, Ningbo Menova Tiankang Pharmaceutical, Ningbo, China), Lidocaine (Hunan Kelun Pharmaceutical Co., Ltd., Hunan, China), Saline (Yangzhou Zhongbao Pharmaceutical, Jiangsu, China), Heparin sodium (Hebei Changshan Biochemical Pharmaceutical Co., Ltd., Hebei, China).
Medication
Patients in all four groups received drug treatment, consisting of oral pregabalin administered at a dosage of one tablet two times daily (150 mg/day). Patients reporting a pain visual analog scale (VAS) score of ≥ 4 were administered oral tramadol and pregabalin as rescue analgesia.
Procedure of SGB treatment
The patient’s identity is verified upon entering the room, and they are placed in an upper-lateral position on the affected side. Vital signs are monitored, and the skin is disinfected with povidone iodide. An ultrasound scan, using a linear transducer with a short-axis view, starts at the supraclavicular plane and moves along the trachea. When the ultrasound image shows the annular hypoechoic trachea, the probe is moved outward and slid up and down to locate the C7 transverse process, confirmed by the disappearance of the anterior transverse nodule. Using the intraplanar mode, the injection needle is percutaneously punctured, with the tip positioned anterior to the long neck muscle and posterior to the internal carotid and jugular vein. Then, 10 ml of 0.8% lidocaine is injected after confirming no blood or fluid is pulled back. The patient reports no discomfort during the procedure and is observed for 30 min. The affected side is treated with an SGB once daily for 15 days (Supplementary Fig. S1).
TABRT treatment procedure
The patient’s identity is verified upon entering the room. Vital signs are monitored, and the skin is prepared with iodization. A vein is accessed, and 150 ml of blood is drawn slowly under negative pressure. Then, 50 ml trioxygen with a concentration of 30 µg/ml is added and mixed evenly with the blood for 3–5 min23. The blood is then slowly infused back into the patient. This procedure is repeated three times consecutively. At the end of the treatment, the intravenous needle is removed, and local compression is applied. There is no bleeding or collection of pathological specimens during the treatment. The patient experiences no discomfort, and vital signs remain stable. The patient is observed for 15 min post-procedure and is advised to drink more water, rest, eat, and exercise moderately. The patient receives TABRT every other day for 15 days (supplementary Fig. S2).
Characterization of patients before treatment
Baseline characteristics of the four groups were recorded before treatment. The parameter contains age, gender, course of disease and side of herpes onset, history of cardiovascular and cerebrovascular diseases (CCD), diabetes mellitus (DM), and tumor and hematologic disorders (THD). Additionally, the Visual Analog Scale (VAS) score, anxiety self-rating index, Pittsburgh Sleep Quality Index (PSQI) score, and Thirty-six Item Short Form Health Survey (SF-36) score were assessed.
VAS score and anxiety self-rating index
The VAS score and anxiety self-rating index were evaluated before treatment and on Day 7 and Day 15 after operation.
Rate of complete remission
The rate of complete remission was assessed by the proportion of patients achieving a VAS score of 0 on Day 15.
Ratio of patients who do not receive analgesic
Patients with a VAS score of ≥ 4 received oral tramadol and pregabalin as rescue analgesics. The proportions of patients who did not require analgesics were recorded.
Complications and side effects
Any side effects during treatment, including hematoma24, tachycardia, infection, nausea/vomiting, local anesthetic toxicity, oral medication-related adverse reactions, pneumothorax, puncture injury allergic were recorded post-treatment.
Statistical analysis
Statistical analyses were conducted using GraphPad Prism 8 (GraphPad Software, Inc., La Jolla, CA, USA) and SPSS 25 (IBM Corporation, Armonk, NY, USA) statistical software. Quantitative data are presented as median (interquartile range, IQR) and were compared using Kruskal–Wallis tests. Qualitative data are presented as percentages and were analyzed using Fisher’s exact tests. A P-value < 0.05 was considered a statistically significant difference.
Results
Patient characteristics
The patients were divided into four groups: 54 in the D group, 48 in the DS group, 43 in the DT group, and 52 in the DST group. There were no statistically significant differences in baseline characteristics between the treatment groups (Table 1).
VAS score in four groups
As shown in Fig. 2 and Table S1, the VAS scores at each post-treatment time point in all four groups were lower than the preoperative scores (p < 0.05). Notably, the VAS on Day 15 (V15) was significantly lower than the initial pre-treatment VAS score (V1) (p < 0.0001). This indicated that the post-herpetic neuralgia of the four groups of patients significantly improved after fifteen days of treatment, with some patients even achieving recovery.
VAS scores in four groups before and after treatment. Violin-whiskers plots demonstrated the VAS scores on Day 1, 7 and 15. Median values was showed by solid line and the interquartile range was presented by dotted line. The VAS scores at each post-treatment time point in all four groups were lower than the preoperative scores (p < 0.01). The VAS on Day 15 was significantly lower than the initial pre-treatment VAS score (p < 0.0001). D drug therapy, DS drug combined stellate ganglion block therapy, DT drug combined trioxygen autologous blood retransfusion therapy, DST drug combined stellate ganglion block and trioxygen autologous blood retransfusion therapy.
Self-rating of anxiety in four groups
As shown in Fig. 3 and Table S2, after 7 days of treatment, the self-rating anxiety scores in three groups, excluding the drug-only group (Group D), were significantly lower than the baseline scores (p < 0.05). However, after 15 days of treatment, the self-rating anxiety score (J15) in all groups were significantly lower, compared to the pre-treatment scores (J1) (p < 0.0001). This indicated that the level of anxiety was substantially reduced in all four groups after 15 days of treatment.
Self-ratings of anxiety in the four groups. Violin-whiskers plots demonstrated the anxiety scores on Day 1, 7 and 15. Median values was showed by solid line and the interquartile range was presented by dotted line. After 7 days of treatment, the self-rating anxiety scores in three groups, except for the Group D, were significantly lower than the baseline scores (p < 0.05). However, after 15 days of treatment, the self-rating anxiety score in all groups were significantly lower, compared to the pre-treatment scores (p < 0.0001). D drug therapy, DS drug combined stellate ganglion block therapy, DT drug combined trioxygen autologous blood retransfusion therapy, DST drug combined stellate ganglion block and trioxygen autologous blood retransfusion therapy.
Difference in VAS scores and self-rating anxiety scores on Day 1 and Day 15 of the four groups
To compare the efficacy of different treatments, the difference in VAS scores and self-rating anxiety scores on Day 1 and Day 15 of the four groups were calculated and designated as DV and DJ respectively. As shown in Fig. 4A and Table S3, statistical analysis revealed that the DV value in the DS Group was significantly higher compared to the D Group (p < 0.05). The DV values in the DT Group and DST Group were even more significantly elevated compared to the D Group (p < 0.001), with the DST Group showing the largest increase (p < 0.0001). No significant difference was observed between the DV values of the DS Group and DT Group (p > 0.05), but both were significantly lower than the DV value of the DST Group when compared individually (p < 0.05). These findings indicated that the combination treatment provides the most substantial improvement in pain relief, followed by the SGB and TABRT methods, with the Drug treatment (D Group) showing the least effect.
DV and DJ values in the four groups. The scores were demonstrated by violin-whiskers plots, with the median values was showed by solid line and the interquartile range was presented by dotted line. (A) DV value in the four groups. The DV value in the DS Group was significantly higher compared to the D Group (p < 0.05). The DV values in the DT Group and DST Group were even more significantly elevated compared to the D Group (p < 0.001), with the DST Group showing the largest increase (p < 0.0001). No significant difference was observed between the DV values of the DS Group and DT Group (p > 0.05), but both were significantly lower than the DV value of the DST Group when compared individually (p < 0.05). (B) DJ value in the four groups. The DJ value in the DS Group was significantly higher than in the D Group (p < 0.05). The DJ values in the DT Group and DST Group were significantly greater than in the D Group (p < 0.001), with the DST Group showing the most substantial increase (p < 0.0001). No significant difference was found between the DJ values of DS and DT Groups (p > 0.05). However, when compared to the DST Group, the DJ value in the DS Group was significantly lower (p < 0.001), and the DJ value in the DT group was slightly smaller than that in the DST Group (p < 0.05). D drug therapy, DS drug combined stellate ganglion block therapy, DT drug combined trioxygen autologous blood retransfusion therapy, DST drug combined stellate ganglion block and trioxygen autologous blood retransfusion therapy. DV and DJ represent the difference of VAS scores and self-rating anxiety scores between Day 1 and Day 15 respectively.
From the perspective of self-rating anxiety, as illustrated in Fig. 4B and Table S3, the DJ value in the DS Group was significantly higher than in the D Group (p < 0.05). The DJ values in the DT Group and DST Group were significantly greater than in the D Group (p < 0.001), with the DST Group showing the most substantial increase (p < 0.0001). No significant difference was found between the DJ values of DS and DT Groups (p > 0.05). However, when compared to the DST Group, the DJ value in the DS Group was significantly lower (p < 0.001), and the DJ value in the DT group was slightly smaller than that in the DST Group (p < 0.05). These results suggested that the Combination treatment provides the most effective anxiety relief, followed by the TABRT and SGB methods, with the Drug treatment showing minimal impact.
Rate of complete remission
Complete remission (CR), defined as a VAS score of 0, indicates that the patient no longer requires medication. As shown is Fig. 5A and Table S4, the rate of complete pain remission was higher in the combined treatment group compared to other three treatment modalities (p < 0.01), especially compared with Group D and Group DS (p < 0.0001). Additionally, Group DT showed a significantly greater remission rate than both the Group D and DS (p < 0.01 for both comparisons). No significant difference was observed between Group D and Group DS (p > 0.05). These findings underscored the superior efficacy of the combined treatment approach in achieving complete pain remission.
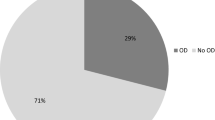
Comparison of complete pain remission, no rescue medication and complication rate in the four groups. (A) Rate of complete remission (CR). The rate of complete pain remission was significantly higher in the DST group compared to other three treatment modalities (p < 0.01). Additionally, Group DT showed a significantly greater remission rate than both the Group D and DS (p < 0.01 for both comparisons). No significant difference was observed between Group D and Group DS (p > 0.05). (B) Rate of no rescue medication (NRM). The rate of NRM in Group DST was significantly higher than in Groups D and DS (p < 0.001). The NRM rate in Group D was significantly lower compared to Group DT (p < 0.01). No significant differences were observed between Group D and Group DS, Group DS and Group DT, or Group DT and Group DST (p > 0.05). (C) Complication rate of four groups. The complication rates in all groups were below 3%, No significant difference was found between four groups (p > 0.05). D drug therapy, DS drug combined stellate ganglion block therapy, DT drug combined trioxygen autologous blood retransfusion therapy, DST drug combined stellate ganglion block and trioxygen autologous blood retransfusion therapy, CR complete remission, NRM no rescue medication.
Rate of no rescue medication in the four groups
The number of patients who did not require emergency medication during the treatment was recorded in each group, and the rate of those not needing rescue medication was calculated. As shown in Fig. 5B and Table S5, the proportion of patients who did not use emergency medication was lowest in Group D (70.0%), followed by Group DS (78.8%) and group DT (92.5%). Notably, no patients in the Group DST required emergency medication, achieving a 100% rate of no rescue medication use. The rate of no rescue medication (NRM) in Group DST was significantly higher than in Groups D and DS (p < 0.001), indicating a superior outcome for the DST group. Meanwhile, the NRM rate in Group D was significantly lower compared to Group DT (p < 0.01). No significant differences were observed between Group D and Group DS, Group DS and Group DT, or Group DS and Group DST (p > 0.05). These findings further support the conclusion that the combination treatment offered the most effective performance in reducing the need for rescue medication.
Complication rate
The number of patients who developed any complications during treatment was recorded. The results showed that the complication rates in all four groups were below 3% (Fig. 5C and Table S6), which reflected that the methods we adopted were safe.
Discussion
In this study, we explored four treatment approaches for PHN in the head and face among elderly patients: simple drug therapy, drug therapy combined with SGB, drug therapy combined with TABRT, and a combination of all three methods. All four treatment methods significantly reduced VAS and anxiety, with SGB25, TABRT, and especially their combination being more effective than drug therapy alone. While there was no significant difference between SGB and TABRT in terms of anxiety relief, the combination therapy was superior, suggesting that a multi-modal approach may provide the most comprehensive benefit. The proportion of patients achieving complete remission was significantly higher in the DT group compared to the drug therapy and DS groups. This finding underscores the superior efficacy of TABRT in pain management and suggests that TABRT, whether used alone or in conjunction with SGB and drug therapy, may be particularly beneficial for treating PHN. The combined treatment group demonstrated the highest rates of both rescue analgesic avoidance and complete remission, further emphasizing the advantages of a comprehensive treatment strategy.
Previous research has demonstrated that combining TABRT with drug therapy effectively reduced PHN symptoms, with the VAS score decreasing by more than 50% without an increase in adverse reactions23. This study evaluated treatment outcomes using a 50% efficacy rate, which provides a relatively broad and generalized view. In contrast, our research adopted a more detailed approach, assessing efficacy through complete remission rates and the proportion of patients who avoided the need for rescue medication. Our study statistical results not only highlight the effectiveness of treatment for mild pain but also demonstrate the timeliness of interventions for severe pain. Additionally, ultrasound-guided SGB has been reported to achieve favorable outcomes in treating PHN affecting the head, face, neck, and upper limbs26. Previous studies primarily focused on pregabalin at a dosage of 150 mg twice daily (bid) or did not include oral anti-neuralgia drugs9,24. In our study, every patient received pregabalin at 75 mg bid as background medication. This approach balances the initial analgesic effects of oral drugs while minimizing the potential interference of high doses with the observation of treatment efficacy. On the other hand, our study exclusively evaluates improvements in pain and anxiety to present the results more concisely. This approach represents a novel observational perspective not explored in previous studies.
Clinical guidelines typically recommend drug therapy, nerve blocks, and radiofrequency therapy for the treatment of postherpetic neuralgia (PHN), yet only 40–50% of patients achieve satisfactory outcomes27. Previous studies have shown that the efficacy of pulsed radiofrequency (PRF) in treating PHN is only 52%11. Another study reported that the success rate of remission in the PRF combined with ozone autohemotherapy group was significantly higher at 68.8%, compared to 51.4% in the PRF group alone17. Based on our data and these previous findings, we can speculate that the TABRT therapy and the combined treatment may become recommended options in future guidelines, providing an additional therapeutic approach for the clinical management of PHN.
Low complication rate is an essential consideration for clinical practice, particularly when treating elderly patients who may be more susceptible to adverse effects. While complications associated with drug therapy, SGB, and TABRT therapy have been reported in the literature6,24, our study found these events to be rare and generally mild. With strict monitoring and timely intervention, these treatments can be administered safely.
This study is limited by its single-center design and small sample size. The observation period was only 15 days, with no long-term follow-up data available. Long-term efficacy is an important consideration, and the positive outcomes observed within the 15-day period suggest a promising potential for sustained benefits. However, to fully address the generalizability of our results, further research with extended follow-up periods will be essential to evaluate the long-term impact, including any delayed effects or changes in efficacy over time. These future studies will help to better understand how TABRT and SGB combination treatment compares to standard therapies in terms of both immediate and long-term benefits. Additionally, combining TABRT, SGB, and other approaches, such as radiofrequency ablation, could be explored through comparative or combination studies. Follow-up research could take experimental or clinical forms, focusing on areas such as biochemistry, physiology, or clinical outcomes. The current treatment frequency is based on empirical guidance, with no clear rationale identified in the literature. Future studies could investigate the underlying principles of frequency selection or compare different treatment frequency protocols to optimize outcomes.
In summary, our study provides compelling evidence that SGB and TABRT, either alone or in combination, are effective and safe for treating PHN in the head and face of elderly patients with the combined application has the best effect. This approach may represent a valuable addition to clinical practice, offering improved pain management and better quality of life for patients suffering from PHN. Our study also introduces a new idea for treating PHN and offers a reference point for future large-scale clinical research and exploration of underlying mechanisms.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Saxena, A. K. et al. Modulation of mRNA expression of IL-6 and mTORC1 and efficacy and feasibility of an integrated approach encompassing cognitive behavioral therapy along with Pregabalin for management of neuropathic pain in postherpetic neuralgia: A pilot study. Pain Med. 22, 2276–2282. https://doi.org/10.1093/pm/pnab142 (2021).
Zhao, C. et al. PROCESS trial: effect of Duloxetine premedication for postherpetic neuralgia within 72 h of herpes Zoster reactivation: a randomized controlled trial. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciad714 (2023).
Wen, B., Wang, Y., Zhang, C., Xu, W. & Fu, Z. Efficacy of different interventions for the treatment of postherpetic neuralgia: a bayesian network meta-analysis. J. Int. Med. Res. 48, 300060520977416. https://doi.org/10.1177/0300060520977416 (2020).
Cui, J. Z. et al. Effect of single Intra-cutaneous injection for acute thoracic herpes Zoster and incidence of postherpetic neuralgia. Pain Manag. Nurs. 19, 186–194. https://doi.org/10.1016/j.pmn.2017.09.002 (2018).
van Hecke, O., Austin, S. K., Khan, R. A., Smith, B. H. & Torrance, N. Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain 155, 654–662. https://doi.org/10.1016/j.pain.2013.11.013 (2014).
Toman, H., Ozdemir, U., Kiraz, H. A. & Luleci, N. Severe headache following ozone therapy: pneumocephalus. Agri 29, 132–136. https://doi.org/10.5505/agri.2016.36024 (2017).
Wang, S., Wang, H., Wang, H., Zhang, D. & Nie, H. Comprehensive comparison of therapeutic efficacy of radiofrequency thermocoagulation and pulsed radiofrequency in treatment of elderly patients with thoracic postherpetic neuralgia. Med. Sci. Monit. 29, e942108. https://doi.org/10.12659/MSM.942108 (2023).
Tang, J., Zhang, Y., Liu, C., Zeng, A. & Song, L. Therapeutic strategies for postherpetic neuralgia: mechanisms, treatments, and perspectives. Curr. Pain Headache Rep. 27, 307–319. https://doi.org/10.1007/s11916-023-01146-x (2023).
Lin, C. S., Lin, Y. C., Lao, H. C. & Chen, C. C. Interventional treatments for postherpetic neuralgia: A systematic review. Pain Physician. 22, 209–228 (2019).
Ding, Y. et al. CT-Guided stellate ganglion pulsed radiofrequency stimulation for facial and upper limb postherpetic neuralgia. Front. Neurosci. 13, 170. https://doi.org/10.3389/fnins.2019.00170 (2019).
Ding, Y. et al. Efficacy and safety of computed tomography-guided pulsed radiofrequency modulation of thoracic dorsal root ganglion on herpes Zoster neuralgia. Neuromodulation 22, 108–114. https://doi.org/10.1111/ner.12858 (2019).
Masan, J., Sramka, M. & Rabarova, D. The possibilities of using the effects of ozone therapy in neurology. Neuro Endocrinol. Lett. 42, 13–21 (2021).
Luo, Q., Wen, S., Tan, X., Yi, X. & Cao, S. Stellate ganglion intervention for chronic pain: A review. Ibrain 8, 210–218. https://doi.org/10.1002/ibra.12047 (2022).
Jeon, Y. Therapeutic potential of stellate ganglion block in orofacial pain: a mini review. J. Dent. Anesth. Pain Med. 16, 159–163. https://doi.org/10.17245/jdapm.2016.16.3.159 (2016).
Fan, Z., Zheng, X., Li, D., Chen, H. & Li, L. Comparison of lidocaine and ropivacaine stellate ganglion blockade in treating upper limb postherpetic neuralgia. Med. (Baltim). 101, e29394. https://doi.org/10.1097/MD.0000000000029394 (2022).
Wang, C. et al. Ultrasound-Guided stellate ganglion block combined with extracorporeal shock wave therapy on postherpetic neuralgia. J. Healthc. Eng. 2022 (9808994). https://doi.org/10.1155/2022/9808994 (2022).
Li, X. R. et al. Ozonated autohemotherapy combined with pulsed radiofrequency in the treatment of thoracic postherpetic neuralgia in older adults: a retrospective study. Med. Gas Res. 14, 12–18. https://doi.org/10.4103/2045-9912.372666 (2024).
Artis, A. S., Aydogan, S. & Sahin, M. G. The effects of colorectally insufflated oxygen-ozone on red blood cell rheology in rabbits. Clin. Hemorheol. Microcirc. 45, 329–336. https://doi.org/10.3233/CH-2010-1316 (2010).
Bocci, V., Borrelli, E., Zanardi, I. & Travagli, V. The usefulness of ozone treatment in spinal pain. Drug Des. Dev. Ther. 9, 2677–2685. https://doi.org/10.2147/DDDT.S74518 (2015).
Muto, M., Giurazza, F., Silva, R. P. & Guarnieri, G. Rational approach, technique and selection criteria treating lumbar disk herniations by oxygen-ozone therapy. Interv. Neuroradiol. 22, 736–740. https://doi.org/10.1177/1591019916659266 (2016).
Aydos, T. R. et al. Effects of ozone therapy and taurine on ischemia/reperfusion-induced testicular injury in a rat testicular torsion model. Turk. J. Med. Sci. 44, 749–755. https://doi.org/10.3906/sag-1308-20 (2014).
Duricic, D., Valpotic, H. & Samardzija, M. Prophylaxis and therapeutic potential of ozone in buiatrics: current knowledge. Anim. Reprod. Sci. 159, 1–7. https://doi.org/10.1016/j.anireprosci.2015.05.017 (2015).
Hu, B., Zheng, J., Liu, Q., Yang, Y. & Zhang, Y. The effect and safety of ozone autohemotherapy combined with pharmacological therapy in postherpetic neuralgia. J. Pain Res. 11, 1637–1643. https://doi.org/10.2147/JPR.S154154 (2018).
Hirota, K. et al. Risk vessels of retropharyngeal hematoma during stellate ganglion block. Reg. Anesth. Pain Med. 42, 778–781. https://doi.org/10.1097/AAP.0000000000000644 (2017).
Jeong, S., Jeon, Y., Yeo, J. & Baek, W. The effects of stellate ganglion block on the electroencephalogram in rats. J. Anesth. 28, 601–605. https://doi.org/10.1007/s00540-013-1780-8 (2014).
Treggiari, M. M. et al. Cervical sympathetic block to reverse delayed ischemic neurological deficits after aneurysmal subarachnoid hemorrhage. Stroke 34, 961–967. https://doi.org/10.1161/01.STR.0000060893.72098.80 (2003).
Werner, R. N. et al. European consensus-based (S2k) guideline on the management of herpes Zoster - guided by the European dermatology forum (EDF) in Cooperation with the European academy of dermatology and venereology (EADV), part 1: diagnosis. J. Eur. Acad. Dermatol. Venereol. 31, 9–19. https://doi.org/10.1111/jdv.13995 (2017).
Funding
This work was supported by the Natural Science Foundation of China to Z.W. (No. 82072777) and to Y.G. (No. 32301023), the Fujian Provincial Clinical Research Center for Brain Diseases (No. 2021FJSLCYX01), the Xiamen Clinical Research Center for Neurological Diseases (No. 2021XMSLCYX01), the Project of Xiamen Cell Therapy Research, China to Z.W. (No.3502Z20214001) to Z.W., the Natural Science Foundation of Fujian Province (No. 2023J011624) and the Medical and Health Guiding Project of Xiamen (No. 3502Z20224ZD1026) to Y.Z. and the Natural Science Foundation of Fujian Province to Y. X. (No. 2023J05270).
Author information
Authors and Affiliations
Contributions
C.Z., Y.G. and Z.W. designed the study. C.Z., Y.X. and Y.Z. performed the experiments and analyzed data. C.Z., Y.G., Y.Z. and Z.W. wrote the manuscript. H. L., B.Z., S.C., W.H. and J.L. provided help with the experiments.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zheng, C., Xie, Y., Li, H. et al. Effectiveness and safety of stellate ganglion block with trioxygen autologous blood retransfusion therapy for facial postherpetic neuralgia in elderly patients. Sci Rep 15, 8025 (2025). https://doi.org/10.1038/s41598-025-91847-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91847-7