Abstract
To evaluate the therapeutic efficacy of bone-disc-bone osteotomy (BDBO) via a posterior approach in combination with biomimetic bone grafting and pedicle screw implantation for the treatment of Kümmell disease complicated with kyphosis. Between March 2012 and June 2020, we retrospectively analyzed 22 patients who had Kümmell disease complicated with kyphosis and underwent BDBO in combination with biomimetic bone grafting and pedicle screw implantation. The kyphotic Cobb angle, visual analog scale (VAS), Oswestry Disability Index (ODI), and American Spinal Injury Association (ASIA) Impairment Scale were used to evaluate the effects of surgery. In addition, surgical conditions, including duration of surgery, intraoperative blood loss, and surgical complications, were recorded. The mean follow-up time was 32.86 months (range, 28.27 to 36.67). The mean operative time was 176.68 ± 25.96 min and the mean intraoperative blood loss was 281.24 ± 43.26 mL. The VAS, ODI, and kyphotic Cobb angles were significantly improved 1 week after surgery compared with preoperative assessments and remained well maintained at final follow-up. Eight patients (36.4%) had mild neurologic impairment before surgery, and their neurologic function normalized at final follow-up. The rate of intervertebral fusion at the final follow-up was 100%. One patient (4.5%) had an infected incision that healed after debridement. There was no case of instrumentation failure. BDBO in combination with biomimetic bone grafting and pedicle screw implantation is a novel, safe, effective and elective treatment strategy for patients who experienced Kümmell disease complicated by kyphosis.
Similar content being viewed by others
Introduction
Kümmell disease, also known as delayed post-traumatic vertebral collapse, was first described in 1895 by the German surgeon Hermann Kummell1 and occurs mainly in middle-aged and elderly patients with osteoporosis2,3. Patients develop delayed vertebral collapse and thoracolumbar kyphosis months to years after minor spinal trauma. Clinical symptoms of Kümmell disease include persistent back pain, limited daily activities and even neurological dysfunction, which severely limit patients’ independence and quality of life4,5. The disease differs from common osteoporotic vertebral compression fractures. Due to the presence of necrotic bone in the injured vertebrae of patients with Kümmell disease, conservative treatment is usually ineffective and requires surgical intervention to restore vertebral height, restore sagittal plane balance of the spine, maintain normal spinal biomechanics and relieve spinal cord compression6.
Regarding the treatment of Kümmell disease, both anterior reconstruction and posterior osteotomy could improve pain, neurological dysfunction and imaging outcomes. However, serious comorbidities, multilevel corpectomies and/or severe osteoporosis highly required PO7. Furthermore, patients without kyphosis and with an intact posterior wall of the vertebral body can be treated with PVP and PKP to relieve pain and restore spinal stability8; however, patients with kyphosis usually require spinal osteotomies for correction, including Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), bone-disc-bone osteotomy (BDBO) and vertebral column resection (VCR), in order of increasing correction rates and complexity9. With the SPO technique, a correction of 9.3° to 10.7° can be achieved through a single segment. However, this technique is not able to remove necrotic lesions in vertebrae with Kümmell disease10. The PSO technique results in an average correction of 31.7°, but has a high incidence of pseudoarthrosis formation of up to 29%, which can be particularly high in patients with Kümmell disease10. VCR is indicated for rigid multiplanar deformities, severely angulated deformities, hemivertebra resections, resectable spinal tumors, post-traumatic deformities and spondyloptosis. It is important to note that the sagittal imbalance was corrected by an average of 87%. However, the average operating time was over 12 h, the average blood loss was 5500 ml and there were a total of 31 complications11.
Currently, the optimal treatment of Kümmell disease, which is usually associated with a kyphosis of more than 30°, is still controversial and unclear6. One of the problems in the treatment of patients with Kümmell disease in combination with kyphosis is the selection of an osteotomy technique that provides adequate sagittal correction while minimizing surgical trauma. The BDBO is an osteotomy that is performed both above and below a disc level, with the resection including the disc with the adjacent endplate(s). A BDBO typically provides correction rates in the range of 35° to 60° and has less surgical trauma than VCR osteotomy. The other difficulty is reconstructing the stability of the spine to achieve bone fusion. The traditional approach is to implant a titanium cage filled with bone particles, but there is a risk that the bone non-healing and sinking of the cage. With advances in medical research on bionic materials, scientists have found that cages made of bionic bone materials have similar properties to the elastic modulus of human bone and promote osseointegration.
Theoretically, BDBO can adequately correct the posterior convex deformity and biomimetic bone grafting with pedicle screw implantation can reconstruct the anterior column support and increase the incidence of bony fusion, which is an intuitive technique for the treatment of Kümmell disease complicated by kyphosis. However, the use of this technique in the treatment of this disease has rarely been reported. Therefore, we retrospectively investigated BDBO in combination with biomimetic bone grafting for Kümmell disease with kyphosis.
Materials and methods
Patient population
The study was approved by the Institutional Review Board of Zhengzhou Orthopaedics Hospital (No. 20240206), and informed consent was obtained from all participants and/or their legal guardians. Furthermore, we confirm that this study was performed in accordance with relevant guidelines and regulations and in compliance with the Declaration of Helsinki. Between March 2012 and June 2020, we studied 22 patients with Kümmell disease combined with kyphosis who underwent BDBO and biomimetic bone grafting and pedicle screw implantation. Inclusion criteria as follows: (1) patients with a history of trauma; (2) patients with a time interval between trauma and hospitalization of ≥ 3 months who had not undergone strict bracing during this period; (3) patients with thoracolumbar segmental kyphosis deformity; (4) patients who had undergone conservative treatments such as bed brakes and thoracolumbar braces before hospitalization, but their effect was not obvious; (5) patients with severe back pain leading to limited mobility, with and without neurological dysfunction at the time of admission; (6) CT scan with intravertebral vacuum cleft and intact subvertebral endplates; (7) MRI with osteonecrosis with fluid signal; (8) bone density was measured by DEXA in all patients and showed osteoporosis (T score < -2.5). The exclusion criteria include: (1) patients with multiple vertebral fractures; (2) patients with a previous fracture of the same vertebra or adjacent vertebrae above and below; (3) patients who had previously undergone spinal surgery and vertebroplasty; (4) patients who have severe multi-organ dysfunction at the time of admission; (5) The patient underwent a three-segment pedicle screw fixation on either the cranial or caudal side of the injured vertebra, or used bone cement reinforced screws.
General information
The characteristics of the patients are shown in Table 1. The study included 6 men and 16 women, with a mean age of 66.50 ± 6.26 years. The course of disease ranged from 3 to 11 months, with an average of 5.35 ± 2.27 months. All patients had a history of minor back trauma, and the affected segment was T11 in 2 cases, T12 in 13 cases, L1 in 4 cases, and L2 in 3 cases. The mean T-score of bone mineral density was − 3.15 ± 0.81. The internal fixation materials were posterior pedicle screw-rod system (Weihai Weigao Company, Shandong Province, China) and nano-based apatite bionic cage (Sichuan Guona Technology Co., Ltd., China).
Surgical technique
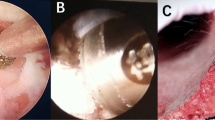
After the general anesthesia had taken effect, the patient was placed in a posteriorly extended prone position. C-arm fluoroscopy was used to confirm the fractured vertebrae. Pedicle screws were inserted into two segments of the injured vertebrae on the cranial and caudal sides, respectively. After the paraspinal muscles were detached, the lamina and the transverse processes of the fractured vertebra as well as the articular processes of the cranial vertebrae of the injured vertebra were removed with the ultrasonic bone knife. If the injured vertebra is a thoracic vertebra, the corresponding proximal ribs are also severed. Carefully separate and ligate the intercostal nerves. The soft tissues around the injured vertebra are then dissected and pushed aside to expose the intervertebral space above the injured vertebra. A titanium rod is inserted on one side for temporary fixation. We used a bone chisel to remove a portion of the cranial pedicle and vertebrae. Necrotic cancellous bone, collapsed superior endplates and fragmented endplates were removed from the injured vertebral body with nucleus pulposus forceps, followed by cleaning of the disk tissue and removal of the inferior endplates of the adjacent vertebral body on the head side with a curette. Depending on the angle of the patient’s kyphosis, the rods were alternately exchanged on both sides to gradually correct the kyphosis until the deformity was satisfactorily corrected radiographically. The resected vertebral plates and ribs were crushed into bone particles and densely filled with 1 ~ 2 nanomimetic cages (manufactured by Sichuan Guona Technology Co., Ltd.) of appropriate length. Then the cage was implanted into the intervertebral space, the titanium rods were pressurized and the screws were tightened, and the good position was confirmed under fluoroscopy (Fig. 1).
The illustration of bone-disc-bone osteotomy and internal fixation techniques used in this study. (A) Insertion of pedicle screws into the caudal and cranial vertebrae of the fractured vertebrae, followed by bone-disc-bone osteotomy; (B) after osteotomy, the posterior column was closed and (C) the anterior column was supported with a bionic bone cage.
A drainage tube was placed and the wound was irrigated with large amounts of saline solution and then sutured layer by layer. Intraoperatively removed necrotic tissue in the vertebral body was examined pathologically to rule out other diseases such as tumors or infectious lesions. A dural tear occurred in one patient, which was discovered intraoperatively and closed tightly with a 5 − 0 suture.
Postoperative treatment
All patients were asked to get out of bed 1 to 2 days after surgery and received rehabilitation exercises in the hospital for about 1 week. Physiotherapy such as electroacupuncture and acupuncture is performed for patients with residual postoperative neurological dysfunction. All patients received pharmacologic antiosteoporotic treatment after discharge from the hospital, including a standard daily dose of calcium (800 mg daily, by mouth), alfacalcidol vitamin D supplement (0.25 mg/bid, by mouth), and zoledronic acid (intravenous infusion of 5 mg, once a year). The patients were followed up at regular intervals.
Postoperative evaluation
Clinical and radiologic data were reviewed before surgery, 1 week after surgery, and at final follow-up. Positive and lateral radiographs were obtained at each follow-up, and the healing of the injured vertebrae was assessed by CT scans at the final follow-up. The Cobb angle was used to assess kyphosis using lateral radiographs. It was measured as the angle between the upper endplate of the uppermost vertebra and the lower endplate of the lowermost vertebra at the instrumented fusion levels. The VAS score and the ODI score were used to assess the improvement in the patient’s pain and functional outcome. The American Spinal Injury Association (ASIA) Impairment Scale was used to assess neurologic status preoperatively and at final follow-up. Surgical data, including operative time, intraoperative blood loss and complications were documented.
Statistical analysis
The statistical software SPSS 25.0 was used. Pre- and postoperative VAS scores, ODI scores, and Cobb angle measurements were normally distributed measures and expressed as expressed as \(\:\stackrel{-}{x\:}\) ± s. Comparisons of indicators at different time points were analyzed by repeated-measures analysis of variance (ANOVA), and multiple comparisons were performed using the Bonferroni method, with P < 0.05 considered statistically significant differences.
Results
The average duration of follow-up was 32.86 months (range from 28.27 to 36.67). The average hospital stay was 8.23 ± 2.41 days, the average duration of surgery was 176.68 ± 25.96 min and the average intraoperative blood loss was 281.24 ± 43.26 mL. Bony union of the injured vertebra was defined as obvious bridging trabeculae and bone formation on CT images and lateral radiographs, and there was no evidence of a vacuum or gap in the vertebral body.
Detailed clinical data on the patients in this report can be found in Table 1. Lasting pain relief and functional improvement was achieved in all cases. Mean VAS scores improved from 8.50 ± 2.06 preoperatively to 3.15 ± 1.15 1 week postoperatively and 1.50 ± 0.52 at final follow-up (all P values < 0.001). Mean ODI scores improved from 75.36 ± 15.96 preoperatively to 45.95 ± 14.37 one week postoperatively and 21.58 ± 5.85 at final follow-up (all P values < 0.001) (Tables 2 and 3).
The mean kyphotic Cobb angle was corrected from 41.52 ± 6.8 preoperatively to 12.27 ± 2.5 one week after surgery and remained at 14.09 ± 2.6 at the last follow-up (Table 3). The fractured vertebrae of all patients showed substantial bone union, which was confirmed by CT scans at the last follow-up (Fig. 2).
A 59-year-old female patient with Kummel’s disease. Her chief complaint was back pain with limited mobility for 6 months after a fall. (A) Preoperative frontal and (B) lateral radiographs of the spine show a kyphosis of the thoracolumbar segment and a compression fracture of L1; (C) preoperative sagittal CT scans show a vertebral collapse of L1 with kyphotic deformity; (D) preoperative T2-weighted MRI images show a linear high signal below the superior endplate of L1 surrounded by a low signal; (E) intraoperative clinical images show that the bionic bone cage was filled with autogenous bone particles; (F) postoperative lumbar frontal and (G) lateral X-rays of the lumbar spine show that the position of the pedicle screws is good and the kyphosis has been significantly corrected; (H) postoperative axial CT images show the bionic cage in good position; (I, J) postoperative sagittal CT scans after 3 months and at final follow-up show adequate bone grafting within the bionic cage and good correction of the kyphosis; (K, L) postoperative coronal CT scans after 3 months and at final follow-up show adequate bone grafting within the bionic cage and good correction of the kyphosis.
According to the ASIA neurological classification system, 8 patients were classified preoperatively as grade D and 14 as grade E. None of them developed new permanent neurological deficits postoperatively. All patients with a preoperative grade of D were improving to E at the final follow-up visit (Table 4).
One patient (4.5%) experienced delayed wound healing after surgery due to superficial infections, which was successfully treated with antibiotic therapy and frequent dressing changes until discharge from hospital. One patient (4.5%) had a rupture of the dural sac, which was discovered intraoperatively and repaired immediately. There were no other obvious surgical complications. During the follow-up period, there were no cases of posterior instrumentation failure, including pedicle screw loosening or breakage.
Discussion
The surgical procedure for the treatment of Kümmell disease complicated by kyphosis remains controversial. Although various surgical methods for spinal reconstruction have been reported in the literature and have shown a trend toward improvement in symptoms and nerve recovery, most of these procedures have been associated with nonunion of the bones, limited correction of the posterior convex deformity, and large surgical trauma12,13,14.
Recently, several researchers have attempted one stage posterior stabilization and decompression in combination with VP for the treatment of Kümmell disease. These researchers believe that the major advantage of this technique is that it allows reconstruction of the anterior and middle column to support the vertebral body with less surgical trauma8,15. However, there are also some limitations to this technique. First, the incidence of postoperative vertebral recollapse and injured vertebral nonunion was high16. Second, bone cement has no osteoconductive or inductive properties and cannot replace autogenous or allogeneic bone graft in achieving the best bone healing. Thirdly, there is a risk of nerve damage due to cement leakage8. Therefore, it is difficult to achieve a permanent reconstruction of the anterior column16.
In the present study, we found that kyphosis improved significantly from 33.56 ± 8.18 preoperatively to 5.51 ± 3.64 postoperatively. We believe that osteotomy with the BDBO technique is an important reason for achieving a satisfactory correction. The advantages of BDBO compared to other osteotomy techniques include: Correction of the deformity at its apex, especially when the apex is in the disc space; comparable correction rates; potential reduction in pseudoarthrosis rate due to removal of the disc; better stability and less trauma17. All patients in this study had osteoporosis, but all received good correction in the immediate postoperative period and all were maintained until last follow-up. We believe that the reasons for this favorable outcome are as follows: After BDBO osteotomy, we altered the sagittal sequence of the spine by adjusting the surgical bed and then placing the pre-bent titanium rod according to the degree of correction observed by intraoperative fluoroscopy, so that no stress was exerted between the titanium rod and the pedicle screw. This may explain why we did not observe any cases of instrument failure. At the final follow-up, no recurrence of pain and only a slight increase in the kyphosis angle was observed.
In this study, we used biomimetic bone materials to reconstruct the stability of the anterior column and promote bone healing, whose main principles include 3 aspects: Osteogenesis, osteoconduction and osteoinduction. The osteoinductive capacity and mechanical properties of nanolight-based apatite can be improved by incorporating polymeric materials into the composition of nanolight-based apatite. Wei et al.18 developed an artificial bioactive material [nano light-based apatite/polycoolamine 66 (n-HA/PA66)] with compressive and flexural strength and elastic modulus similar to human cortical bone, which is biocompatible and thermally stable and has a high safety factor. Nanobiomimetic bone made of n-HA/PA66 composite biomaterials is a kind of high-performance material for tissue repair and reconstruction, as demonstrated by biomechanical studies: The biomechanical properties of n-HA/PA66-biomimetic bone is better than those of autologous bone graft. The porous structure of nanomimetic bone can provide an ideal place for the growth of bone tissue into bone tissue, which promotes the growth of bone tissue, microvessels and fibrous connective tissue, as well as the transport of nutrients and metabolic products. The products of the material itself also favor the degradation and absorption of the material, so that the pore size is further increased, which favors the migration and growth of osteoblasts and promotes the formation of new bone. The use of nano-sized apatite bionic bone in the reconstruction of the anterior column after thoracolumbar osteotomy has the following advantages: first, it has similar compressive and flexural strength and modulus of elasticity to human cortical bone; second, it has good biocompatibility and osteoconductivity; third, it participates in matrix calcification and promotes new bone formation; fourth, it is non-allergenic, no heat source and no soft tissue irritation; fifth, it achieves good support and increases the contact area between the upper and lower supporting surfaces, with a low subsidence rate of the supporting body; sixth, it achieves good support and increases the contact area between the upper and lower supporting surfaces. Seven, good support and effectively increase the contact area with the upper and lower supporting bone surfaces, low subsidence rate of the supporting body; eight, no masking effect on X-rays; nine, unlimited dosage.
In view of the low quality of iliac bone in osteoporotic patients and the possible donor-site complications(primarily chronic pain at the harvest site), we did not perform an iliac graft and used only the small bone fragments of autogenous bone from spinous processes and lamina, which promotes osteogenesis and microangiogenesis19.
Our result showed that no failure of internal fixation was detected in all patients at final follow-up, although all of these patients had osteoporosis or low bone mass preoperatively. We believe that the use of long segmental posterior instrumentation to stabilize the spine is another important reason for the satisfactory results of our surgeries. Furthermore, during the intraoperative placement of the pedicle screw, we assessed the holding force of the screw based on the resistance we felt when the screw was tapped into the screw channel, so no cement reinforcement was performed in our patients. Postoperatively, we asked patients to wear a thoracolumbar brace to prevent loosening of the pedicle screws. Although short-segment posterior instrumentation has been widely used and allows more motion segments to be preserved, implant failure and progression of kyphosis have been reported in long-term follow-up studies20,21. Lee et al.20 described the use of a transpedicular intracorporeal bone graft with short-segment posterior instrumentation in 36 patients with Kümmell disease. Although symptoms improved in a short time, screw loosening occurred in 14% of patients during the follow-up period, and more than 70% of patients developed progressive kyphosis and back pain 1 year after surgery. Even when the axial load-bearing capacity of the anterior column was partially restored by transpedicular bone grafting to the fractured body, the bone graft failed to provide adequate structural support immediately before fracture healing20. In our opinion, the low bone mass of the spine of patients with Kümmell disease also requires higher strength requirements for the fixation strength of the instruments, and this view has been supported by researchers14. Previous studies have shown that long-segment posterior instrumentation can largely reinforce fixation and is superior to short-segment fixation in preventing the progression of postoperative kyphosis and vertebral recollapse21. Taking these factors into account, we have used long-segment posterior instrumentation to stabilize the spine in patients with Kümmell disease with kyphosis.
Our study has some limitations. First, it was a retrospective study with a limited sample size, which could limit the generalizability of our results. Second, selection bias may have occurred because we did not include a control group in this study. Although direct comparisons with other surgical techniques were not possible, our results demonstrate the efficacy and safety of our technique. A larger population and a longer follow-up period are needed to verify the efficacy of our surgical approach for the treatment of Kümmell disease complicated by kyphosis.
In conclusion, BDBO in combination with biomimetic bone grafting and pedicle screw implantation is a novel, safe, effective and elective treatment strategy for patients who experienced Kümmell disease complicated by kyphosis.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Kümmell, H. Ueber die traumatischen erkrankungen der Wirbelsäule. Dtsch. Med. Wochenschr. 21, 180–181. https://doi.org/10.1055/s-0029-1199707 (1895).
Bae, J. et al. Minimally invasive surgery transpedicular intrabody cage technique for the management of Kummell disease. Int. J. Spine Surg. 18, 73–80. https://doi.org/10.14444/8570 (2024).
Ning, Y. et al. Comparison of the clinical efficacy and bone cement distribution difference between Kummell’s disease and osteoporotic vertebral compression fracture after percutaneous kyphoplasty. Pain Physician. 27, E327–E336 (2024).
Liu, T., Gu, G., Zhan, C., Zhang, S. & Tang, Y. Comparison of percutaneous vertebroplasty and percutaneous vertebroplasty combined with pediculoplasty for Kummell’s disease: a retrospective observational study. J. Orthop. Surg. Res. 18, 471. https://doi.org/10.1186/s13018-023-03957-5 (2023).
Yang, D. L., Yang, S. D., Chen, Q., Shen, Y. & Ding, W. Y. The treatment evaluation for osteoporotic Kummell disease by modified posterior vertebral column resection: minimum of One-Year Follow-Up. Med. Sci. Monit. 23, 606–612. https://doi.org/10.12659/msm.902669 (2017).
Ma, R., Chow, R. & Shen, F. H. Kummell’s disease: delayed post-traumatic osteonecrosis of the vertebral body. Eur. Spine J. 19, 1065–1070. https://doi.org/10.1007/s00586-009-1205-4 (2010).
Liu, F. et al. Anterior reconstruction versus posterior osteotomy in treating Kummell’s disease with neurological deficits: A systematic review. Acta Orthop. Traumatol. Turc. 52, 283–288. https://doi.org/10.1016/j.aott.2018.05.002 (2018).
Lu, W. et al. Analysis of percutaneous kyphoplasty or short-segmental fixation combined with vertebroplasty in the treatment of Kummell disease. J. Orthop. Surg, Res. 14 https://doi.org/10.1186/s13018-019-1358-8 (2019).
Kose, K. C., Bozduman, O., Yenigul, A. E. & Igrek, S. Spinal osteotomies: indications, limits and pitfalls. EFORT Open. Rev. 2, 73–82. https://doi.org/10.1302/2058-5241.2.160069 (2017).
Bridwell, K. H. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 31, S171-178, (1976). https://doi.org/10.1097/01.brs.0000231963.72810.38 (2006).
Bradford, D. S. & Tribus, C. B. Vertebral column resection for the treatment of rigid coronal decompensation. Spine (Phila Pa 22, 1590–1599, (1976). https://doi.org/10.1097/00007632-199707150-00013 (1997).
Lee, J. & Song, K. S. Transpedicular intravertebral cage augmentation in a patient with neurologic deficits after severely collapsed Kummel disease: minimum 2-Year Follow-Up. World Neurosurg. 135, 146–155. https://doi.org/10.1016/j.wneu.2019.11.131 (2020).
Zhang, X., Hu, W., Yu, J., Wang, Z. & Wang, Y. An effective treatment option for Kümmell disease with neurological deficits. Spine 41, E923–E930. https://doi.org/10.1097/BRS.0000000000001467 (2016).
Sudo, H. et al. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J. 13, 1726–1732. https://doi.org/10.1016/j.spinee.2013.05.041 (2013).
Zhang, G. Q. et al. Posterior decompression and short segmental pedicle screw fixation combined with vertebroplasty for Kümmell’s disease with neurological deficits. Experimental Therapeutic Med. 5, 517–522. https://doi.org/10.3892/etm.2012.833 (2013).
Deng, H. et al. Therapeutic efficacy of transpedicular intracorporeal cement augmentation with short segmental posterior instrumentation in treating osteonecrosis of the vertebral body: A retrospective case series with a minimum 5-year follow-up. BMC Musculoskelet. Disord. 20 https://doi.org/10.1186/s12891-019-2671-4 (2019).
Enercan, M. et al. Osteotomies/spinal column resections in adult deformity. Eur. Spine J. 22 (Suppl 2), 254–264. https://doi.org/10.1007/s00586-012-2313-0 (2013).
Jie, W., Yubao, L. & Yi, H. Processing properties of nano apatite-polyamide biocomposites. J. Mater. Sci. 40, 793–796. https://doi.org/10.1007/s10853-005-6326-5 (2005).
Gangji, V., De Maertelaer, V. & Hauzeur, J. P. Autologous bone marrow cell implantation in the treatment of non-traumatic osteonecrosis of the femoral head: five year follow-up of a prospective controlled study. Bone 49, 1005–1009. https://doi.org/10.1016/j.bone.2011.07.032 (2011).
Lee, G. W., Yeom, J. S., Kim, H. J. & Suh, B. G. A therapeutic efficacy of the transpedicular intracorporeal bone graft with short-segmental posterior instrumentation in osteonecrosis of vertebral body: A minimum 5-year follow-up study. Spine 38, E244–E250. https://doi.org/10.1097/BRS.0b013e31827efef2 (2013).
Sheng, X. & Ren, S. Surgical techniques for osteoporotic vertebral collapse with delayed neurological deficits: A systematic review. Int. J. Surg. 33, 42–48. https://doi.org/10.1016/j.ijsu.2016.07.050 (2016).
Acknowledgements
The authors declare that there is no conflict of interests. This study was supported by the Jilin Provincial Science and Technology Department Project (YDZJ202301ZYTS032), Jilin Province Health Science and Technology Capability Enhancement Project (2023JC012) and Jilin University Bethune Plan Project (2024B09).
Author information
Authors and Affiliations
Contributions
TY, DXG and WBJ participated in the manuscript writing and editing; XWG, GHY and JLW participated in the literature search; YBS performed data analysis under the supervision of YS; TY revised the manuscript. All authors contributed to the reviewal and interpretation of data. The manuscript was drafted by DXG, reviewed by all authors, and revised with contributions from all authors under the supervision and final revision of WBJ. WBJ was responsible for the integrity of the work from inception to the finished article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, DX., Guo, XW., Yang, GH. et al. A technical note on the posterior approach BDBO for treating Kümmell disease. Sci Rep 15, 9892 (2025). https://doi.org/10.1038/s41598-025-91923-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91923-y