Abstract
Aims Studies confirm that microalbuminuria (MAU) can not only predict diabetic kidney disease (DKD) but also indicate of systemic vascular endothelial injury. Thyroid hormones (TH) have been reported to be associated with various cardiovascular diseases and endothelial cell damage. Currently, few studies have reported the association between free thyroxine (FT4) to free triiodothyronine (FT3) ratio and MAU. The purpose of this study was to investigate the association between FT4/FT3 ratio and MAU in euthyroid patients with type 2 diabetes mellitus (T2DM). Methods This study enrolled a total of 1734 T2DM patients with euthyroid status. MAU was defined as 30 ≤ urinary albumin-to-creatinine ratio (UACR) < 300 mg/g. The participants were divided into MAU group and normal albuminuria group (NAU group). The relationship between FT4/FT3 ratio and MAU was analyzed. Results In this study, there were 367 patients with MAU. Compared with the NAU group, the MAU group had higher FT4/FT3 ratio (P < 0.001). In univariate analysis, the FT4/FT3 ratio was positively related to both UACR and MAU (both P < 0.001). In multivariate linear stepwise regression, the FT4/FT3 ratio is independently related to UACR (Standardized coefficients: 0.148, P < 0.001). In binary logistic regression analysis, the FT4/FT3 ratio emerges as an independent risk factor for MUA (odds ratio: 1.947, 95% confidence interval: 1.522–2.491). Conclusion The FT4/FT3 ratio was independently and positively correlated with MAU in euthyroid patients with T2DM.
Similar content being viewed by others
Introduction
Diabetes, particularly type 2 diabetes mellitus (T2DM), has emerged as a significant global health challenge. The International Diabetes Federation (IDF) reports that there are around 422 million individuals living with diabetes worldwide1. The challenge of long-term management of this chronic disease lies in its multitude of complications, which affect the vasculature, nerves, and multiple organs, particularly the kidney. Microalbuminuria (MAU), identified by urinary albumin to creatinine ratio (UACR) ranging from 30 to 300 mg/g, was initially recognized for its predictive value in diabetic kidney disease (DKD)2. Research indicates that MAU not only serves as an indicator for DKD but is also intricately linked to elevated risks of cardiovascular diseases and associated mortality rates3,4,5. An earlier finding suggests a significant correlation between elevated urinary albumin levels and heightened cardiovascular disease risk among individuals with T2DM6. Therefore, analyzing risk factors for MAU can offer new insights for the prevention and treatment of progressing to significant proteinuria or various cardiovascular diseases, ultimately enhancing the prognosis of patients with T2DM7.
The thyroid gland plays a vital role as an essential endocrine gland in the human body. Its function is primarily governed by levels of thyroid hormones (TH), which are crucial for cellular metabolism, blood sugar regulation, and other essential processes8. TH directly impact renal tubular function, glomerular filtration rate, and renal hemodynamics9. Previous research demonstrates that, even within populations with normal thyroid function, levels of TH are closely linked to the risk of developing conditions such as DKD and cardiovascular diseases10,11. Furthermore, studies suggest that TH levels also influence endothelial cell function. TH regulate vascular dilation, angiotensin II receptor activity, and its signaling pathway, thus modulating endothelial function and vascular homeostasis12. The primary TH include free triiodothyronine (FT3), free thyroxine (FT4), and thyroid-stimulating hormone (TSH). The FT3/FT4 ratio can be understood as the conversion rate of thyroxine (T4) to triiodothyronine (T3), indicating the responsiveness to TH in peripheral tissues13. Additionally, research indicates that the correlation between the FT3/FT4 ratio and cardiovascular diseases, as well as DKD, is stronger than the correlation between either FT3 or FT4 alone14,15.
In recent years, researches have highlighted the significant association between thyroid dysfunction and both MAU and DKD16,17,18. However, in euthyroid patients with T2DM, studies on TH, particularly the ratio of FT4 to FT3, in relation to MAU are still limited. Therefore, this study aims to explore the potential link between the FT4/FT3 ratio and MAU in euthyroid patients with T2DM.
Methods
Study design: This study employed a cross-sectional design aimed at evaluating the relationship between the FT4/FT3 ratio and MAU in patients with T2DM, who were receiving care at the Endocrinology Department of Linyi People’s Hospital, Shandong Province, China, from January 2020 to March 2023. These individuals were diagnosed according to the criteria established by the World Health Organization (WHO) in 1999. The selection process incorporated specific exclusion criteria, including: (1) patients manifesting any form of thyroid dysfunction; (2) patients with UACR ≥ 300 mg/g; (3) individuals < 18 years; (4) patients suffering from significant liver or kidney impairments; (5) patients with urinary tract infections; and (6) cases with incomplete medical records. After a rigorous screening process, a cohort of 1734 patients who satisfied all eligibility requirements was assembled. This cohort was further stratified into two distinct groups for analysis: participants were divided into MAU group (30 ≤ UACR < 300 mg/g) and NAU group (UACR < 30 mg/g).
Laboratory biochemical indices: Following a period of overnight fasting, venous blood is collected in the early morning for comprehensive analysis. The assay panel includes alanine aminotransferase (ALT), aspartate aminotransferase (AST), serum creatinine (Scr), uric acid (UA), total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), hemoglobin (Hb), fasting blood glucose (FBG), and glycated hemoglobin (HbA1c, assessed through high-performance liquid chromatography), utilizing an automated biochemical analyzer (Cobas c 702, Roche, Germany). The analysis of urinary creatinine, using the Jaffe method, and urinary microalbumin (UMA), determined by transmission turbidimetry, along with the calculation of the urinary albumin-to-creatinine ratio (UACR), is performed using an automated analyzer (Beckman Coulter AU5821). Visceral fat area (VFA) and subcutaneous fat area (SFA) measurements were conducted using the Omron DUALSCAN BIA machine (Omron HDS-2000, Kyoto, Japan). Thyroid function tests, covering FT3, FT4, thyroid-stimulating hormone (TSH), and anti-thyroid peroxidase antibody (TPOAb), are conducted via chemiluminescence immunoassay (Siemens, USA), with the normal ranges for thyroid function specified as follows: TSH from 0.55 to 4.78 uIU/mL, FT3 from 3.5 to 6.5 pmol/L, and FT4 from 11.5 to 22.7 pmol/L.
Medical data and anthropometric measurement: In this study, comprehensive medical data were extracted from patients’ records, including demographic information (age, gender), lifestyle factors (smoking and drinking status), and clinical parameters (diabetes duration). Laboratory results, such as blood glucose, lipid profiles, and thyroid function tests, were also collected to analyze their potential associations with the FT4/FT3 ratio and MAU. Anthropometric measurements, including height, weight and blood pressure, were obtained following standardized protocols, with BMI calculated as BMI (kg/m²) = weight (kg) / height² (m²)19. These data were analyzed to examine the relationship between the FT4/FT3 ratio and the occurrence of MAU in T2DM patients. The estimated glomerular filtration rate (eGFR) was calculated following the Modification of Diet in Renal Disease equation: 194 × serum Cr −1.094 × age −0.287(×0.739 if women)20.
Diagnosis of diabetic retinopathy (DR)
According to the corresponding criteria, diagnose DR21.
Statistical analysis: The Statistical Package for the Social Sciences (SPSS), version 20.0 (Chicago, IL, USA) was utilized for data analysis. The software can be accessed at https://www.ibm.com/products/spss-statistics. Normal distribution variables were presented as mean ± SD, while non-normal variables were described with medians and interquartile ranges. The comparisons of normally and non-normally distributed continuous variables were performed using the independent-samples T test and Mann-Whitney U test, respectively. Categorical variables were compared using the chi-square test. Pearson and Spearman coefficients assessed correlations between UACR, MAU, and other factors. Multiple linear regression and binary logistic stepwise regression analyses identified independent predictors for UACR and MAU. A two-tailed P value < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study subjects
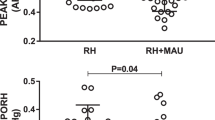
The baseline clinical characteristics of the study participants are shown in Table 1. The MAU group (n = 367) demonstrated marked increases in several parameters including age, diabetes duration, systolic blood pressure (SBP), TC, TG, FBG, HbA1c, FT4, FT4/FT3 ratio, UA, and Scr, compared to the NAU group (all P < 0.05). Conversely, significant reductions in FT3, eGFR, and Hb levels were observed (both P < 0.05). Notably, the incidence of diabetic retinopathy (DR) was significantly higher within the MAU group than in the NAU group (P < 0.05). Yet, no significant distinctions were found between two groups regarding the proportions of male participants, smokers, and drinkers, as well as BMI, VFA, SFA, diastolic blood pressure (DBP), LDL-c, HDL-c, AST, ALT, TSH, and TPOAb levels (all P > 0.05).
Univariate analysis
As shown in Table 2, Pearson’s correlation analysis indicated that UACR positively correlated with age, duration of diabetes, SBP, TC, TG, FBG, HbA1c, FT4, the FT4/FT3 ratio, and Scr, while it negatively correlated with FT3, eGFR and Hb (all P < 0.05). There was no significant relationship between UACR and BMI, VFA, SFA, DBP, LDL-c, HDL-c, AST, ALT, TSH, TPOAb, UA (all P > 0.05). Similarly, Spearman correlation analysis showed that MAU was positively related to age, duration of diabetes, SBP, TG, FBG, HbA1c, FT4, the FT4/FT3 ratio, UA, and Scr, and negatively related to FT3, eGFR and Hb (all P < 0.05). No significant correlations were found between MAU and BMI, VFA, SFA, DBP, TC, LDL-c, HDL-c, AST, ALT, TSH, TPOAb (all P > 0.05).
Multivariate analysis
In our analytical framework, UACR was designated as the dependent variable, while various aforementioned metrics served as independent variables. Consequently, a multivariate linear stepwise regression analysis was undertaken. Following the adjustment for additional variables, the derived model from the multivariate linear regression equation is presented in Table 3. Our findings indicate that the FT4/FT3 ratio, SBP, Scr, Hb, HbA1c, duration of diabetes, and TG were significant contributors to the model (with standardized coefficients of 0.148, 0.164, 0.150, −0.209, 0.184, 0.119, and 0.088 respectively, all P < 0.001).
In this investigation, MAU was classified as having a UACR between 30 and 300 mg/g. The binary logistic regression analysis, adjusted for confounding factors and illustrated in Table 4, revealed odds ratios (OR) and 95% confidence intervals (CI) for the FT4/FT3 ratio, SBP, Scr, Hb, HbA1c, duration of diabetes, UA, and DR as follows: 1.947 (1.522–2.491), 1.021 (1.014–1.029), 1.018 (1.009–1.027), 0.980 (0.972–0.989), 1.196 (1.117–1.280), 1.045 (1.025–1.066), 1.003 (1.002–1.005), and 1.385 (1.037–1.851), respectively.
Discussion
In our research, we have introduced FT4/FT3 ratio to more effectively delineate the independent risk factors for the onset of MAU. This study found that in patients with T2DM and normal TH levels, the level of FT4/FT3 is positively correlated with the risk of developing MAU. After adjusting for confounding factors, high FT4/FT3 levels remain an independent risk factor for MAU.
The progression of DKD encompasses several stages, beginning with MAU and culminating in end-stage renal disease (ESRD). In patients with diabetes, MAU has a heightened propensity to evolve into overt proteinuria, ultimately culminating in renal failure22,23. This is a critical factor leading to mortality and the incidence of cardiovascular events in patients with T2DM. A global study indicates that the overall prevalence of MAU among patients with T2DM is approximately 39%24. In this study, the prevalence of MAU in patients with T2DM is approximately 21.2%. This variance may be attributed to factors such as ethnicity, sample size, among others. Another meta-analysis concerning the prevalence of MAU in diabetic patients in Africa revealed that the overall prevalence of MAU among African diabetic patients is approximately 37%25. Generally, the prevalence of MAU among diabetic patients is high25,26.
Prior studies have assessed the relationship between TH levels and DKD progression, demonstrating a negative correlation between FT3 and the advancement of DKD10,27,28. Further research has discovered that, within the middle-aged and elderly demographic in China, low FT3 levels within the normal range are linked to the development of MAU29. In our study, the results differ from those of the aforementioned study. Although in univariate analysis, FT3 levels were negatively associated with UACR and MAU respectively (p< 0.05), FT3 did not ultimately enter into the multiple linear regression and logistic regression equations. Moreover, reports on the correlation between FT4, TSH, and UACR have been inconsistent10,30. In our study, FT4 exhibited a positive correlation with both UACR and MAU in both Pearson and Spearman correlation analyses (p < 0.05), while TSH demonstrated no correlation in either analysis (p> 0.05). The variation could be attributed to the differences in the populations screened, confounding factors adjusted, ethnicities, and study designs. It is noteworthy that the FT4/FT3 ratio is the only TH-related parameter that entered the final regression equation, suggesting a closer association with MAU in euthyroid patients with T2DM. Currently, there is no reported analysis of the relationship between these two factors, which is consistent with prior research findings, with the distinction that they did not differentiate between significant albuminuria and MAU15. The underlying mechanism for the positive correlation between the FT4/ FT3 ratio and MAU remains incompletely understood. In addition, it is crucial to consider the broader implications of TH imbalances on kidney function. Endothelial dysfunction, a key factor in the progression of DKD, contributes to kidney damage through mechanisms such as inflammation, fibrosis, and microvascular injury31. Research suggests that TH play a significant role in regulating various biological processes, including cardiovascular and renal function, and influence endothelial function9. When TH levels are dysregulated, particularly when elevated or reduced, endothelial dysfunction may be exacerbated, accelerating the progression of DKD32. This dysregulation adds complexity to the relationship between TH levels and the progression of MAU in T2DM.
From a biological perspective, TH play a crucial role in the human body, impacting the cardiovascular system, metabolism, and growth and development, among other aspects. They can influence kidney function through multiple mechanisms, including the activation of the renin-angiotensin-aldosterone system (RAAS), and affect the function of the renal tubules and glomeruli9. TH receptors are expressed in both cardiac myocytes and vascular tissues. Therefore, in addition to their direct effects on the kidneys, TH can also impact renal function through the cardiovascular system, potentially leading to renal damage and MAU33.
In addition, we also found that SBP, HbA1c, duration of diabetes, DR, and MAU were independently associated. This is consistent with previous research findings29,34,35.
Limitations
This study has certain limitations. Firstly, due to its cross-sectional design, we cannot establish a causal relationship between the FT4/FT3 ratio and MAU. Future prospective or interventional studies would be beneficial in further exploring this relationship. Secondly, the study results may be influenced by the limited sample size. In the future, we need to expand the sample size, conduct multicenter studies, and refine the findings of this study.
Conclusion
In conclusion, this study demonstrates that the FT4/FT3 ratio is positively correlated with MAU in patients with normal thyroid function and T2DM, suggesting that this ratio may be an independent risk factor for the development of MAU in these patients. Future studies should further explore the potential application value of this ratio in the monitoring and management of MAU in patients with normal thyroid function and T2DM.
Data availability
The datasets utilized in this study are accessible upon reasonable request from the corresponding author.
References
Thomas, M. C. et al. Diabetic kidney disease. Nat. Rev. Dis. Primers. 1, 15018. https://doi.org/10.1038/nrdp.2015.18 (2015).
Gerstein, H. C. et al. Prevalence and determinants of microalbuminuria in high-risk diabetic and nondiabetic patients in the heart outcomes prevention evaluation study. The HOPE study.Investigators. Diabetes Care. 23 (Suppl 2), B35–39 (2000).
Ahmad, T., Ulhaq, I., Mawani, M. & Islam, N. Microalbuminuria in Type-2 diabetes mellitus; the tip of iceberg of diabetic complications. Pak J. Med. Sci. 33, 519–523. https://doi.org/10.12669/pjms.333.12537 (2017).
Kim, J. J. et al. A prospective two-center study on the associations between microalbuminuria, coronary atherosclerosis and long-term clinical outcome in asymptomatic patients with type 2 diabetes mellitus: evaluation by coronary CT angiography. Int. J. Cardiovasc. Imaging. 31, 193–203. https://doi.org/10.1007/s10554-014-0541-6 (2015).
Watanabe, H., Iino, K. & Ito, H. Subclinical microalbuminuria as a predictor of heart failure prognosis. Circ. J. 78, 2838–2839. https://doi.org/10.1253/circj.cj-14-1120 (2014).
Stehouwer, C. D. et al. Increased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of death. Diabetes 51, 1157–1165. https://doi.org/10.2337/diabetes.51.4.1157 (2002).
Strain, W. D. & Paldánius, P. M. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc. Diabetol. 17 https://doi.org/10.1186/s12933-018-0703-2 (2018).
Hoermann, R., Midgley, J. E. M., Larisch, R. & Dietrich, J. W. Recent advances in thyroid hormone regulation: toward a new paradigm for optimal diagnosis and treatment. Front. Endocrinol. (Lausanne). 8, 364. https://doi.org/10.3389/fendo.2017.00364 (2017).
Iglesias, P., Bajo, M. A., Selgas, R. & Díez, J. J. Thyroid dysfunction and kidney disease: an update. Reviews Endocr. Metabolic Disorders. 18, 131–144. https://doi.org/10.1007/s11154-016-9395-7 (2017).
Liu, M. C. et al. Association between thyroid hormones and diabetic kidney disease in Chinese adults. BMC Endocr. Disord. 23 https://doi.org/10.1186/s12902-023-01299-1 (2023).
Neves, J. S. et al. Association of thyroid function, within the euthyroid range, with cardiovascular risk: the EPIPorto study. Front. Endocrinol. (Lausanne). 13, 1067801. https://doi.org/10.3389/fendo.2022.1067801 (2022).
Cai, Y. et al. Thyroid hormone affects both endothelial and vascular smooth muscle cells in rat arteries. Eur. J. Pharmacol. 747, 18–28. https://doi.org/10.1016/j.ejphar.2014.11.036 (2015).
Nie, X. et al. Increased serum adipocyte fatty Acid-Binding protein levels are associated with decreased sensitivity to thyroid hormones in the euthyroid population. Thyroid 30, 1718–1723. https://doi.org/10.1089/thy.2020.0011 (2020).
Lang, X. et al. FT3/FT4 ratio is correlated with all-cause mortality, cardiovascular mortality, and cardiovascular disease risk: NHANES 2007–2012. Front. Endocrinol. 13, 964822. https://doi.org/10.3389/fendo.2022.964822 (2022).
Zhao, X., Sun, J., Xin, S. & Zhang, X. Predictive Effects of FT3/FT4 on Diabetic Kidney Disease: An Exploratory Study on Hospitalized Euthyroid Patients with T2DM in China. Biomedicines 11, (2023). https://doi.org/10.3390/biomedicines11082211
El-Eshmawy, M. M., El-Hafez, A. & Shabrawy, H. A. E. Abdel Aal, I. A. Subclinical hypothyroidism is independently associated with microalbuminuria in a cohort of prediabetic Egyptian adults. Diabetes Metab. J. 37, 450–457. https://doi.org/10.4093/dmj.2013.37.6.450 (2013).
Xie, J. et al. The longitudinal effect of subclinical hypothyroidism on urine microalbumin-to-urine creatinine ratio in patients with type 2 diabetes mellitus. BMC Endocr. Disord. 19, 84. https://doi.org/10.1186/s12902-019-0405-0 (2019).
Furukawa, S. et al. Association between subclinical hypothyroidism and diabetic nephropathy in patients with type 2 diabetes mellitus. Endocr. J. 61, 1011–1018. https://doi.org/10.1507/endocrj.ej14-0206 (2014).
Eknoyan, G. Adolphe Quetelet (1796–1874)--the average man and indices of obesity. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association -. Eur. Ren. Association. 23, 47–51. https://doi.org/10.1093/ndt/gfm517 (2008).
Zhang, L. et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet (London England). 379, 815–822. https://doi.org/10.1016/s0140-6736(12)60033-6 (2012).
Hao, Z. et al. Application of non-mydriatic fundus examination and artificial intelligence to promote the screening of diabetic retinopathy in the endocrine clinic: an observational study of T2DM patients in Tianjin, China. Ther. Adv. Chronic Dis. 11, 2040622320942415. https://doi.org/10.1177/2040622320942415 (2020).
Chen, C. et al. Normoalbuminuric diabetic kidney disease. Front. Med. 11, 310–318. https://doi.org/10.1007/s11684-017-0542-7 (2017).
Roscioni, S. S. & Heerspink, L. Zeeuw, D. Microalbuminuria: target for renoprotective therapy PRO. Kidney Int. 86, 40–49. https://doi.org/10.1038/ki.2013.490 (2014). de.
Parving, H. H., Lewis, J. B., Ravid, M., Remuzzi, G. & Hunsicker, L. G. Prevalence and risk factors for microalbuminuria in a referred cohort of type II diabetic patients: a global perspective. Kidney Int. 69, 2057–2063. https://doi.org/10.1038/sj.ki.5000377 (2006).
Mohammed, O. et al. Prevalence of microalbuminuria among diabetes patients in Africa: A systematic review and Meta-Analysis. Diabetes Metab. Syndr. Obes. 16, 2089–2103. https://doi.org/10.2147/dmso.S409483 (2023).
Ali, A. A. & Al Lami, F. H. Prevalence and determinants of microalbuminurea among type 2 diabetes mellitus patients, Baghdad, Iraq, 2013. Saudi J. Kidney Dis. Transplantation: Official Publication Saudi Cent. Organ. Transplantation Saudi Arabia. 27, 348–355. https://doi.org/10.4103/1319-2442.178561 (2016).
Siddiqui, K., Nawaz, S. S., Alfadda, A. A. & Mujammami, M. Low Circulating free Triiodothyronine levels are associated with the progression of diabetic nephropathy in patients with type 2 diabetes. Int. J. Gen. Med. 15, 8659–8668. https://doi.org/10.2147/ijgm.S389071 (2022).
Yang, Z. et al. The correlation between thyroid hormone levels and the kidney disease progression risk in patients with type 2 diabetes. Diabetes Metab. Syndr. Obes. 15, 59–67. https://doi.org/10.2147/dmso.S347862 (2022).
Zhou, Y. et al. Free Triiodothyronine concentrations are inversely associated with microalbuminuria. Int. J. Endocrinol. 2014, 959781. https://doi.org/10.1155/2014/959781 (2014).
Chen, Y. et al. Thyroid parameters and kidney disorder in type 2 diabetes: results from the METAL study. J. Diabetes Res. 2020 (4798947). https://doi.org/10.1155/2020/4798947 (2020).
Lassén, E. & Daehn, I. S. Molecular mechanisms in early diabetic kidney disease: glomerular endothelial cell dysfunction. Int. J. Mol. Sci. 21 https://doi.org/10.3390/ijms21249456 (2020).
Feng, X., Huang, J., Peng, Y. & Xu, Y. Association between decreased thyroid stimulating hormone and hyperuricemia in type 2 diabetic patients with early-stage diabetic kidney disease. BMC Endocr. Disorders. 21, 1. https://doi.org/10.1186/s12902-020-00672-8 (2021).
Mariani, L. H. & Berns, J. S. The renal manifestations of thyroid disease. J. Am. Soc. Nephrol. 23, 22–26. https://doi.org/10.1681/asn.2010070766 (2012).
Khan, T. M. et al. Incidence of microalbuminuria and factors affecting it in patients with type 2 diabetes mellitus. Cureus https://doi.org/10.7759/cureus.27294 (2022).
Chawla, S. et al. Relationship between diabetic retinopathy microalbuminuria and other modifiable risk factors. Prim. Care Diabetes. 15, 567–570. https://doi.org/10.1016/j.pcd.2021.01.012 (2021).
Acknowledgements
We express our heartfelt gratitude to all the research team members who participated in this study. This study was funded by grants from the Postdoctoral Program of Affiliated Hospital of Jining Medical University (JYFY322152).
Author information
Authors and Affiliations
Contributions
H.Z and X.M jointly designed the study, were responsible for the writing and revision of the manuscript, and oversaw the implementation of the research. S.S, X.W, and J.S were responsible for some of the data analysis and interpretation of results. B.B, G.G and B.J provided significant academic guidance and research direction. All authors contributed to the writing and revision of the manuscript and reached consensus on the final draft.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All patients included in this study provided written informed consent upon admission, explicitly stating that their medical records may be used for scientific research purposes. No objections were raised by any patients during the study period. Furthermore, this study adhered to the ethical guidelines set forth by the Helsinki Declaration and received ethical approval from the Human Ethics Committee of Linyi People’s Hospital.
Competing interests
The authors declare no competing interests.
Conflict of interest
Hongyan Zhao, Xuan Ma, Shuwei Shi, Xin Wang, Jie Sheng, Baolan Ji, Guanqi Gao and Bo Ban declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, H., Ma, X., Shi, S. et al. Association between FT4/FT3 ratio and microalbuminuria in euthyroid patients with type 2 diabetes mellitus. Sci Rep 15, 7324 (2025). https://doi.org/10.1038/s41598-025-92046-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92046-0