Abstract
This research aimed to investigate the value of clinical data in preterm infants on admission for the early prediction of retinopathy of prematurity (ROP). 98 preterm infants (66 males and 32 females) with an average gestational age of 30.42 ± 1.20 weeks were included. Basic vital signs, clinical tests, and maternal information were collected at admission. Preterm infants were divided into a non-ROP group and a ROP group based on whether they eventually developed ROP. The receiver operating characteristic (ROC) curve was used to evaluate the predictive value of the above indexes and the combined indexes in the ROP of preterm infants. (1) The differences in systolic blood pressure (SBP), red blood cell count (RBC), hemoglobin (HGB), direct bilirubin (DBIL), and total bilirubin (TBIL) were statistically significant between the non-ROP group and ROP group (all P < 0.05). (2) RBC, HGB, DBIL, and TBIL, all of which have diagnostic value for ROP [area under curve (AUC) 0.643, 0644, 0.887, and 0.744, respectively, all P < 0.05]. (3) The combined indicator possessed a good diagnostic value for ROP (AUC of 0.962, P < 0.05), with a sensitivity and specificity of 88.64% and 91.49%, respectively. (4) Combined indicator (body temperature, body weight, heart rate, SBP, diastolic blood pressure, mean arterial pressure, RBC, HGB, red blood cell distribution width, DBIL, TBIL) has better diagnostic value for ROP than each of RBC, HGB, DBIL, and TBIL alone (Z-value 5.386, 5.475, 2.410 and 4.420, respectively, all P < 0.05). Combined indicator has good predictive value for ROP in preterm infants.
Similar content being viewed by others
Background
Retinopathy of prematurity (ROP) is a proliferative disease of the retina that occurs in premature infants and infants with low birth weight (LBW). 65.8% of infants had some degree of ROP; 81.6% for infants of less than 1000 g birth weight. Lower birth weight and gestational age had a higher incidence and severity of ROP1 which is the leading cause of poor vision and blindness in infants and young children. The mortality rate of LBW and premature infants has improved over the years due to improvement in medical technology, thus, the incidence of ROP has increased annually2. The diagnosis of ROP relies on digital fundus cameras or indirect ophthalmoscopes. However, by the time ROP is detected, the retina has already been damaged. ROP can be reduced or even prevented by early identification in infants at high risk of ROP3 and dynamic adjustment of their oxygen therapy or other disease management regimens. Some clinical biological markers, such as circRNAs expression profile changes in peripheral blood mononuclear cells (PBMCs)4, serum fructosamine5, complete blood count (CBC) in the first week after birth6, critical levels of interleukin-6 (IL-6), tumour necrosis factor-α (TNF-α) and vascular endothelial growth factor-A in cord blood7, serum IL-33 and endorphin levels8, etc., revealed some value in the early detection of ROP. The aim of this research was to investigate the relationship between vital signs, clinical examination, maternal information and ROP in preterm infants and to explore a simple and practical marker for early prediction of ROP in preterm infants.
Methods
Study population
49 preterm infants admitted to our Neonatal Intensive Care Unit (NICU) with a final diagnosis of ROP between Jun. 2022 and Dec. 2022 were retrospectively collected as the ROP group (34 males, 15 females, mean gestational age 30.58 ± 1.05 weeks). The non-ROP group was matched with 49 preterm infants with similar gestational age and birth weight admitted to NICU at the same time (32 males, 17 females, mean gestational age 30.25 ± 1.32 weeks). Cases in the ROP group/showed at least a demarcation line between the peripheral avascular zone and the retinal vascular endings in the posterior pole, i.e., ROP stage I. Informed consent was signed by the subjects’ legal guardians. This research was approved by the Medical Ethics Committee of The Second Xiangya Hospital, Central South University [Ethical Audi No. Study K034 (2021)] and conforms to the principles stated in the Declaration of Helsinki.
Inclusion and exclusion criteria
Inclusion criteria: Meet the diagnostic criteria for preterm infants and ROP. Exclusion criteria: Preterm infants with complex congenital heart disease, inherited metabolic diseases, and congenital multiple malformations, such as congenital abdominal cleft, intestinal atresia, esophageal atresia, esophageal-tracheal fistula, and congenital biliary atresia; for whom it is not possible to dilate pupils to perform funduscopic examination9,10.
Variables
Categorical variables: sex, body weight, body temperature, heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), red blood cell count (RBC), hemoglobin (HGB), red blood cell distribution width (RDW), direct bilirubin (DBIL), total bilirubin (TBIL).
Continuous variables: polyembryony, weight and gestational age classification, gestational hypertension, delivery mode, gestational diabetes mellitus (GDM), and intrauterine distress.
Fundus examination
(1) Prior to the examination, informed consent was signed by the legal guardians of the infants. Mydrin-P eye drops (compound tropicamide eye drops containing 50 mg tropicamide and 50 mg phenylephrine hydrochloride; Santen Pharmaceutical Co., Ltd, Osaka, Japan) were then applied 2–3 times in both eyes at 15-minute intervals. After the pupil dilated, a digital fundus camera (SW-8000P, Tianjin Suowei Electronic Technology, China) was used to perform fundus examination, taking retinal imaging in 5 directions including midline, up, down, left, and right. The fundus photos were sent to experienced ophthalmologists.
(2) Results record: Ophthalmologists described the development of retinal blood vessels based on fundus photos and recorded the zoning, staging, and presence of bleeding, neovascularization, retinal detachment, or not. ROP diagnosis and classification was conducted according to the ROP screening guideline published by the Chinese Ophthalmological Society and the International Classification of Retinopathy of Prematurity, Third Edition9,10,11.
Statistical analysis
If the continuous variable is normally distributed, it is expressed as mean ± SD; otherwise, it is expressed as the quartile M (P25, P75). Categorical variables were expressed in frequency or as a percentage. Chi-square test (categorical variables), Student’s t-test (normal distribution), or Mann-Whitney U-test (skewed distribution) were used to analyze differences between non-ROP group and ROP group. A receiver operating characteristic (ROC) curve was used to evaluate the diagnostic efficacy of different indicators for ROP. Logistic regression was used to combine the diagnostic efficacy of multiple indicators. The area under the curve (AUC) was compared using the Z-test. AUC = 1 denotes perfect prediction. 0.85 < AUC ≤ 0.95 represents excellent prediction. 0.7 < AUC ≤ 0.85 indicates moderate prediction. 0.5 < AUC ≤ 0.7 represents low prediction. P-values < 0.05 (two-sided) were considered statistically significant.
Results
Study population comparison between the non-ROP group and ROP group
There were 98 preterm infants included in this study, 66 males and 32 females, with a mean gestational age of 30.42 ± 1.20 weeks. SBP, RBC, HGB, DBIL, and TBIL in the ROP group were higher than those in the non-ROP group (P < 0.05) (Table 1).
ROC for single indicator on ROP
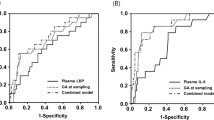
RBC and HGB had a low predictive efficacy for ROP (AUC of 0.643 and 0.644, respectively, all P < 0.05); DBIL had an excellent predictive efficacy for ROP (AUC of 0.887, with sensitivity and specificity of 88.64% and 85.11%, respectively, P < 0.001). TBIL had a moderate predictive efficacy for ROP (AUC 0.744, with sensitivity and specificity of 90.91% and 46.81%, respectively, P < 0.001) (Table 2; Fig. 1).
ROC for combined indicator on whether or not ROP
To explore whether the predictive value of ROP can be further improved, we combined the 11 indicators listed in Table 2 (specific indicators are listed, such as body temperature, body weight, HR, SBP, DBP, MAP, RBC, HGB, RDW, DBIL, TBIL). The combined indicator has an excellent predictive value for ROP (AUC = 0.962, 95%CI = 0.930–0.995, P-value = 0.017, cut-off value = 0.57, sensitivity = 88.64%, specificity = 91.49, positive likelihood ratio = 91.49, negative likelihood ratio = 0.12, jordon index = 0.80) (Fig. 2).
Comparison of different ROCs
To compare whether the 11 combined indicators (body temperature, body weight, HR, SBP, DBP, MAP, RBC, HGB, RDW, DBIL, TBIL) were superior to the predictive value of RBC, HGB, TBIL, and DBIL for ROP, a comparison of multiple ROCs was performed. The AUC of the combined index was significantly greater than that of RBC, HGB, TBIL, and DBIL, thereby providing better predictive value. (Z = 5.386, 5.475, 2.410, 4.420, all P<0.05). Thus, the predictive value of the combined indicator for ROP is better than the remaining four indicators (Table 3; Fig. 3).
Discussion
Early detection and diagnosis of ROP can prevent retinal detachment and blindness. Clinical screening of newborn infants for ocular disease has been undertaken with a focus on ROP. Some biomarkers have been reported in the literature which revealed some value in predicting retinopathy of prematurity, while they may be difficult to obtain or have limited predictive value. A few researchers have used possible risk factors such as gestational age, birth weight, sepsis, respiratory distress syndrome, abdominal bleeding, continuous positive pressure ventilation, oxygen saturation, apnoea, number and duration of blood transfusions, oxygen therapy and phototherapy to predict the occurrence of ROP12, but the cut-off time of the indicators were long or the predictive accuracy was low, so they were still not good early predictions of ROP. Therefore, there is still a demand to explore the clinical utility of biomarkers as more effective predictive tools. The indicators used in our study were common indicators (including body temperature, weight, HR, SBP, DBP, MAP, RBC, HGB, RDW, DBIL, and TBIL), all of which were available at the time of admission, which allowed us to anticipate the occurrence of ROP in neonates in the first place, and thus pay attention to early intervention.
The results of this research showed that RBC, HGB, DBIL and TBIL had predictive value for ROP. RBC and HGB are normally involved in oxygen transport in the body. Anaemia caused by reduced RBC and HGB leads to reduced oxygen levels in the blood, and retinal blood vessels are very sensitive to oxygen supply. They require sufficient oxygen to maintain normal vascular development and function. If the oxygen supply is inadequate, the vascular endothelial cells can be damaged, affecting the normal growth and branching of blood vessels13. Anaemia can also cause an imbalance of angiogenic factors, abnormal blood flow and hypoperfusion, oxidative stress and inflammatory responses14. Anaemia indicates that oxygen delivery to the retina may be compromised, thereby increasing the risk of ROP. However, those two indicators are only indicative of possible anaemia, which may explain the low predictive value.
The predictive value of DBIL and TBIL for ROP may be due to the fact that they are measures of bilirubin levels, which are mainly produced by the liver and excreted via the biliary tract. Therefore, they partially reflect the function of the hepatobiliary system15,16,17. The immature development of the hepatobiliary system in premature infants may lead to bilirubin metabolism disorders, and high levels of DBIL and TBIL may indicate abnormal function of the hepatobiliary system. Bilirubin is an endogenous antioxidant that reacts with oxygen free radicals, thereby interfering with their activity18,19. However, the antioxidant effects of bilirubin are not absolute and its effectiveness depends on many factors. Elevated bilirubin can sometimes be associated with increased production of oxygen free radicals. For example, the body may produce more free radicals in certain disease states or under stressful conditions, and elevated bilirubin may not compensate for the increase in free radicals. In this case, high bilirubin levels also indicate a state of high oxygen free radicals. Excessive oxygen free radicals may cause early damage to retinal vascular endothelial cells, affect vascular development and function, and increase the risk of ROP20. Hoppe et al.21 reported that reducing hypoxia-inducing factor (HIF) may mitigate the damaging effects on the retina.
The main finding of this research is that combining indicators that do not appear to have predictive value improves the predictive value of ROP. Abnormal body temperature usually indicates infection or other health problems. Infection and inflammation can damage the vascular endothelial cells of the retina and affect the normal development of blood vessels, which is associated with the development of ROP. Lyu et al.22 reported that neonatal hypothermia was associated with severe retinopathy in preterm infants. In addition, there was a U-shaped relationship between admission temperature and adverse neonatal outcomes. The lowest incidence of adverse outcomes occurred when the admission temperature was between 36.5 °C and 37.2 °C. In addition, LBW is one of the characteristics of preterm infants, which can lead to immature retinal development and fragile blood vessels, making preterm infants more prone to retinal vascular abnormalities, which is a major risk factor for ROP. Ozdemir et al.23 reported that birth weight and gestational age were positively correlated with lens thickness, vitreous length and axial length (r > 0.5).
Changes in HR and BP reflect the functional status of the cardiovascular system. A dysfunctional cardiovascular system may affect blood flow to the retina, with hypotension causing retinal ischaemia and increasing the risk of vascular injury, and hypertension inhibiting retinal vessel growth. Kistner et al.24 reported that preterm infants with severe abnormalities in retinal vascular development during the neonatal period may have an increased risk of elevated blood pressure in adulthood. RDW reflects the degree of variation in RBC size. A large RDW may indicate abnormal RBC morphology and function, which may affect oxygen delivery and blood supply to the retina.
To improve the ability to predict ROP, the combined indicator takes into account several potential risk factors for ROP and integrates them using a regression equation. This allows analysis of general data at the time of admission. Park et al.25 reported that elevated levels of IL-6 and C5a in cord plasma can be used as independent indicators to predict severe ROP and laser therapy, respectively. The combined model can predict the progression of ROP with good accuracy. The combined indicator in this research is convenient and practical for clinical collection. They can also be used as predictive biological markers for routine application in ROP.
Strengths and limitations
This study yielded good ROP prediction ability by fitting general data on preterm hospital admission. The indexes involved are straightforward, practical, and cost-effective. Moreover, the relatively small sample size and single-center data sources are the limitations of our study, which need to be validated in a larger cohort and in multi-center facilities. Moreover, the generality of our findings may be influenced by changes in ethnic and demographic distributions. Prospective studies should address these limitations to establish the availability of broader joint indicators in different clinical settings.
Conclusions
The combined indicator has an excellent predictive value for ROP, and the universality and cost-effectiveness of the indicators involved allow pediatricians at the primary level to better diagnose and manage ROP at an early stage.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Palmer, E. A. et al. Incidence and early course of retinopathy of prematurity. The cryotherapy for retinopathy of prematurity cooperative group. Ophthalmology 98 (11), 1628–1640 (1991).
Sabri, K., Ells, A. L., Lee, E. Y., Dutta, S. & Vinekar, A. Retinopathy of prematurity: A global perspective and recent developments. Pediatrics 150 (3), e2021053924 (2022).
Sun, H. et al. The use of the WINROP screening algorithm for the prediction of retinopathy of prematurity in a Chinese population. Neonatology 104 (2), 127–132 (2013).
Li, Y. et al. Potential biomarkers for retinopathy of prematurity identified by circular RNA profiling in peripheral blood mononuclear cells. Front. Immunol. 13, 953812 (2022).
Bozdag, S. et al. Serum Fructosamine and retinopathy of prematurity. Indian J. Pediatr. 78 (12), 1503–1509 (2011).
Fevereiro-Martins, M. et al. Complete blood count parameters as biomarkers of retinopathy of prematurity: a Portuguese multicenter study. Graefes Arch. Clin. Exp. Ophthalmol. 261 (10), 2997–3006 (2023).
Bartkevičienė, D. et al. Umbilical blood levels of IL-6 and TNF-α as predictors of the central nervous system damage and retinopathy in preterm infants. Am. J. Perinatol. 38 (10), 1036–1041 (2021).
Cakir, U., Tayman, C., Yucel, C. & Ozdemir, O. Can IL-33 and endocan be new markers for retinopathy of prematurity? Comb. Chem. High. Throughput Screen. 22 (1), 41–48 (2019).
Stahl, A. et al. Effect of intravitreal aflibercept vs laser photocoagulation on treatment success of retinopathy of prematurity: the FIREFLEYE randomized clinical trial. JAMA 328 (4), 348–359 (2022).
Chiang, M. F. et al. International classification of retinopathy of prematurity, third edition. Ophthalmology 128 (10), e51–e68 (2021).
Ophthalmology Group, Ophthalmology Society of Chinese Medical Association. Chinese Screening Guidelines for retinopathy of prematurity. Chin J Ophthalmol. 2014,50(12):933–935. (2014).
Azami, M., Jaafari, Z., Rahmati, S., Farahani, A. D. & Badfar, G. Prevalence and risk factors of retinopathy of prematurity in Iran: a systematic review and meta-analysis. BMC Ophthalmol. 18 (1), 83 (2018).
Di Fiore, J. M. et al. The relationship between patterns of intermittent hypoxia and retinopathy of prematurity in preterm infants. Pediatr. Res. 72 (6), 606–612 (2012).
Sola, A., Altimier, L., Bueno, M. T. M. & Muñoz, C. E. Monitoring SpO2: the basics of retinopathy of prematurity (back to basics) and targeting oxygen saturation. Crit. Care Nurs. Clin. North. Am. 36 (1), 69–98 (2024).
Hammermann, C. et al. Bilirubin in the premature: toxic waste or natural defense? Clin. Chem. 44 (12), 2551–2553 (1998).
Bélanger, S., Lavoie, J. C. & Chessex, P. Influence of bilirubin on the antioxidant capacity of plasma in newborn infants. Biol. Neonate. 71 (4), 233–238 (1997).
Gopinathan, V., Miller, N. J., Milner, A. D. & Rice-Evans, C. A. Bilirubin and ascorbate antioxidant activity in neonatal plasma. FEBS Lett. 349 (2), 197–200 (1994).
Hegyi, T., Goldie, E. & Hiatt, M. The protective role of bilirubin in oxygen-radical diseases of the preterm infant. J. Perinatol. 14 (4), 296–300 (1994).
Yeo, K. L., Perlman, M., Hao, Y. & Mullaney, P. Outcomes of extremely premature infants related to their peak serum bilirubin concentrations and exposure to phototherapy. Pediatrics 102 (6), 1426–1431 (1998).
Graziosi, A. et al. Oxidative stress markers and the retinopathy of prematurity. J. Clin. Med. 9 (9), 2711 (2020).
Hoppe, G. et al. Comparative systems pharmacology of HIF stabilization in the prevention of retinopathy of prematurity. Proc. Natl. Acad. Sci. U S A. 113 (18), E2516–2525 (2016).
Lyu, Y. et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr. 169 (4), e150277 (2015).
Ozdemir, O. et al. The relationship of birth weight, gestational age, and postmenstrual age with ocular biometry parameters in premature infants. Arq. Bras. Oftalmol. 78 (3), 146–149 (2015).
Kistner, A., Jacobson, L., Östergren, J. & Hellström, A. Retinopathy of prematurity is associated with increased systolic blood pressure in adults who were born preterm. Neonatology 112 (1), 87–91 (2017).
Park, Y. J. et al. Immune and inflammatory proteins in cord blood as predictive biomarkers of retinopathy of prematurity in preterm infants. Invest. Ophthalmol. Vis. Sci. 60 (12), 3813–3820 (2019).
Acknowledgements
The authors thank the research personnel and the research volunteers involved with the project.
Funding
Department of Science and Technology of Hunan Province (2023SK4018). Natural Science Foundation of Hunan Province of China (2021JJ70093).
Author information
Authors and Affiliations
Contributions
WS, SW and CW conceived the research. WS, LPZ and XRH collected and reviewed the subjects’ data. WS and SW performed statistical analysis and drafted the manuscript. All authors contributed to its revision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was signed by the subjects’ legal guardians. This research was approved by the Medical Ethics Committee of The Second Xiangya Hospital, Central South University [Ethical Audi No. Study K034 (2021)], and conforms to the principles stated in the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, W., Zhu, L., He, X. et al. Combined indicator assists in early recognition of retinopathy of prematurity. Sci Rep 15, 8048 (2025). https://doi.org/10.1038/s41598-025-92205-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92205-3