Abstract
Studies have highlighted complex bidirectional relationships between autoimmune diseases and depressive disorders. Given that early mental health interventions have substantial public health implications, this study investigated association between optic neuritis, an autoimmune inflammatory disorder of the optic nerve, and risk of developing depressive disorders. Utilizing extensive national health insurance data encompassing almost the entire Korean population, this cohort study included 11,745 patients with optic neuritis and 58,725 age- and sex- matched controls between 2010 and 2017. The diagnosis of optic neuritis was confirmed using ICD-10 code H46 and patient medical records. The association with depression risk identified by ICD-10 codes F32 and F33 was assessed using Cox proportional hazards regression models after adjusting for demographics, lifestyle variables, and other comorbidities. Newly diagnosed optic neuritis was associated with an increased risk of depression (hazard ratio = 1.349, 95% confidence interval: 1.277–1.426), independent of potential confounding factors. Subgroup analysis revealed a stronger association for individuals under 50 years, males, current smokers, and those without hypertension. This association suggests that autoimmune neuroinflammatory responses impact mental health differently across demographics. These findings underscore the importance of implementing routine depression screening and developing targeted early intervention strategies for patients with optic neuritis, particularly for those with a high-risk of depression.
Similar content being viewed by others
Introduction
Depressive disorder is characterized by persistent sadness, lack of interest in daily activities, and various emotional and physical problems. It significantly impacts an individual’s quality of life, posing a major public health challenge globally. As one of the leading causes of disability worldwide, depressive disorder affects more than 300 million people and contributes substantially to the global burden of disease1. Early diagnosis and identification of high-risk individuals for depressive disorder by recognizing potential risk factors and indicators of this condition early in its course are vital for implementing timely interventions and tailored treatments to significantly hamper disease progression and improve outcomes2. Among the myriad of risk factors associated with depressive disorder, autoimmune diseases have emerged as a significant area of interest. Previous studies have indicated complex and bidirectional relationships between autoimmune conditions, where the immune system mistakenly attacks the body’s own cells, and depressive disorders3,4.
Autoimmune diseases such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) have been associated with an increased risk of developing depressive disorders5,6. Conversely, the presence of depressive disorder can adversely affect the course of autoimmune diseases, potentially triggering flare-ups or exacerbating symptoms7,8. However, many aspects of such reciprocal causal relationships between autoimmune diseases and depressive disorders remain poorly understood, necessitating further investigation.
Recent studies including nationwide, population-based cohort research have revealed that optic neuritis (ON)—an autoimmune-mediated inflammatory condition of the optic nerve leading to vision loss—might significantly increase the risk of developing systemic autoimmune diseases in affected individuals9. Although ON has a substantial incidence rate of 3.29–3.9 per 100,000 person-years worldwide9,10,11, contribution of ON to the pathogenesis of depressive disorders remains uncertain. Given that early identification and intervention in depression can significantly improve outcomes, understanding the relationship between ON and depression risk could provide valuable opportunities for targeted mental health screening and timely intervention. Thus, this study aimed to assess the risk of developing depressive disorders in patients newly diagnosed with ON by leveraging comprehensive nationwide data and accounting for potential confounders. Our findings could inform clinical practice guidelines regarding implementation of routine depression screening for ON patients, potentially enabling earlier detection and more effective management of mental health concerns in this population.
Results
Baseline characteristics
A total of 70,470 participants were analyzed after applying exclusion criteria, including 11,745 individuals diagnosed with ON and a control group of 58,725 participants matched for age and sex who did not have ON. Key demographics and health characteristics of both groups are summarized in Table 1, distinguishing between those with ON and those without ON. Notably, the prevalence of current smoking or drinking habits, obesity, and the proportion of individuals in the lowest income quartile were significantly lower in the ON group than in the control group. In contrast, incidence rates of diabetes mellitus (DM), hypertension, dyslipidemia, and chronic kidney disease (CKD) were higher in the ON group than in the control group, with all comparisons reaching statistical significance (p < 0.0001 for all).
Association between ON and risk of developing depressive disorders
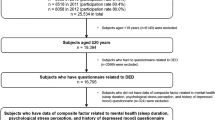
Over a mean (SD) follow-up period of 3.80 (2.23) years for patients with ON and 3.93 (2.24) years for their matched counterparts, 7,751 (11.00%) instances of depressive disorders were identified, with 1,616 (13.76%) occurring in the ON group and 6,135 (10.45%) in the matched control group as illustrated in Fig. 1. The Kaplan–Meier analysis revealed that patients with ON experienced lower rates of survival free from depressive disorders than those without ON (Fig. 2). Table 2 outlines outcomes from multivariable-adjusted Cox regression analyses (Models 2–4), examining the effect of ON on incidence of depressive disorders in the Korean cohort. For individuals with ON, hazard ratios (HRs) for developing depressive disorders were found to be 1.362 (95% confidence interval [CI]: 1.289–1.438) in the unadjusted Model 1, 1.365 (95% CI: 1.293–1.442) in Model 2 (adjusted for age and sex), 1.369 (95% CI: 1.296–1.446) in Model 3 (adjusted for age, sex, smoking habits, alcohol use, regular physical activity, and income level), and 1.349 (95% CI: 1.277–1.426) in Model 4 (Further adjusted for obesity, DM, hypertension, dyslipidemia, and CKD in addition to variables specified in Model 3) relative to those in the non-ON group.
Subgroup analysis to investigate associations of depressive disorder risk with diverse characteristics and comorbidities
Table 3 and Supplementary Table 1 show incidence rates and HRs adjusted for multiple variables for the development of depressive disorder. These variables included age, sex, smoking status, alcohol consumption, regularity of physical activity, income level, and the presence of comorbidities such as obesity, DM, hypertension, dyslipidemia, and CKD. Notably, Model 4 revealed that individuals aged under 50 years (HR: 1.574, 95% CI: 1.393–1.780; p for interaction = 0.006), males (HR:1.450, 95% CI: 1.338–1.571; p for interaction = 0.018), current smokers (HR: 1.588, 95% CI: 1.392–1.812; p for interaction = 0.008), and those not suffering from hypertension (HR: 1.447, 95% CI: 1.341–1.561; p for interaction = 0.010) exhibited a stronger association between ON and the onset of depressive disorders compared to their counterparts who aged over 50 years, females, non-smokers, and those with hypertension, respectively.
Discussion
This study extensively explored the association between ON and the development of depressive disorders in a nationwide cohort from Korea. Our findings revealed that individuals diagnosed with ON had a significantly higher risk of developing depressive disorders than those without ON, with adjusted HRs demonstrating a robust association across various models. Specifically, younger individuals, males, current smokers, and those without hypertension exhibited stronger associations of ON with depressive disorders. These results underscore the potential role of ON as a risk factor or early indicator for depressive disorders, emphasizing the need for close monitoring and early intervention strategies of affected patients. To the best of our knowledge, this study presents an inaugural comprehensive analysis of the relationship between ON and depression in a nationwide, population-based cohort.
The impact of depression on global health cannot be overstated, with early diagnosis and intervention, including psychotherapy, medication, and lifestyle modifications, playing crucial roles in management and prognosis of this disease. These preemptive measures can substantially improve long-term outcomes and enhance patients’ quality of life and functionality. Early intervention for patients with depression can lead to better long-term outcomes by preventing progressive neurobiological changes12 and minimizing subsequent progression to more severe forms of the disease13, leading to better response to treatment and higher chance of achieving remission14. In addition, given that depression co-occurs with other medical conditions such as cardiovascular diseases and chronic pain, early diagnosis and treatment of depression can help manage these comorbidities more effectively15. Economically, early detection and treatment of depression can lead to considerable savings by reducing lost productivity, healthcare costs, and the burden on families and caregivers16.
The pathogenesis of depressive disorders involves a complex interplay of genetic predisposition, biological and medical factors, environmental conditions, and lifestyle factors, ultimately leading to depression17. It has been hypothesized that dysregulation of synaptic activity governed by intricate coordination of molecular pathways and physiological processes plays a substantial role in the development of depression, although the precise underlying molecular mechanisms involved remain to be elucidated18. Preventive strategies for depression include targeted interventions for those with risk factors contributing to the pathogenesis of depressive disorder. Among various risk factors, the relationship between autoimmune conditions and depression has been well-established, with inflammation serving as a central element in this association19,20. Autoimmune conditions characterized by an abnormal immune response against the body’s own cells can lead to chronic inflammation, which has been implicated in the pathogenesis of depression21,22,23,24. Chronic inflammation can affect brain function by altering neurotransmitter systems, particularly those involving serotonin, dopamine, and norepinephrine known to be crucial for mood regulation24. Pro-inflammatory cytokines such as interleukin (IL)-1β, interferon (IFN)-γ, tumor necrosis factor (TNF)-α, and excitatory amino acid glutamate are known to decrease the bioavailability of these neurotransmitters22,24. In addition, neuroinflammation might lead to disruption of the hypothalamic-pituitary-adrenal axis, pathological activation of microglial cells, compromised neuroplasticity, and alterations in the structure and function of the brain21,23,24.
Beyond these inflammatory mechanisms, recent evidence has suggested additional pathways linking autoimmune conditions to depression. Of particular interest is the role of microbiome in this association. Studies have demonstrated that gut dysbiosis, an imbalance in gut bacteria, is linked to both major depressive disorder and autoimmune conditions25. This indicates that gut dysbiosis might potentially represent a common underlying mechanism of depression and autoimmune conditions. In this context, the gut-brain axis appears to provide another shared pathophysiological pathway in this complex relationship. Indeed, previous studies have demonstrated that autoimmune diseases such as RA and SLE are associated with a significantly increased risk of depressive disorder5,6. Intriguingly, the presence of depression is known to be associated with a significantly increased risk of developing subsequent autoimmune diseases (such as RA, SLE, and Crohn’s disease) with exacerbation of symptoms7,8. Taken together, these findings highlight a robust bidirectional link between systemic autoimmunity and depressive disorder, providing a foundation for exploring their link to ON.
The development of ON is intricate, characterized by an aberrant immune response in which the immune system mistakenly attacks the optic nerve. This misdirected attack results in inflammation and demyelination, subsequently leading to a deterioration of visual function26. ON is commonly indicative of various autoimmune neurological disorders such as multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD), and myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD). These conditions involve various antigenic targets, leading to distinct pathogenic mechanisms. For instance, in NMOSD, autoantibodies specifically target the Aquaporin-4 water channel, which is expressed on astrocyte endfeet27. In contrast, in MS, cloned patient’s autoantibodies targeting myelin have been shown to induce complement-mediated demyelination28, although the precise target antigen in MS remains unidentified. Of note, ON may reflect a wider systemic autoimmune dysfunction as evidenced by an increased cumulative incidence of autoimmune diseases such as giant cell arteritis, polymyalgia rheumatica, Sjögren’s syndrome, Behcet’s disease, SLE, ankylosing spondylitis, and myasthenia gravis in ON patients9,29.
Our study highlights a notable association between ON and a heightened risk of depression, implying that ON could be a marker of extensive autoimmune neuroinflammatory activity within the central nervous system, which plays a vital role in the onset of depressive disorder. Another factor to consider is that patients with autoimmune conditions often experience high levels of stress, negative mood, poor self-efficacy, and maladaptive coping mechanisms30. This psychosocial burden together with visual impairment and eye discomfort resulting from ON might significantly affect their quality of life and mental health, potentially contributing to the initiation or exacerbation of depressive disorders31,32.
In the present study, the relationship between ON and an increased risk of depression was notably more pronounced in patients younger than 50 years, males, smokers, and those without hypertension than in those older than 50 years, females, smokers, and those with hypertension, respectively. The elevated risk of depression observed in ON patients under 50 years of age indicates that autoimmune neuroinflammatory responses might play a more substantial role in younger populations than in older populations, although the potential impact of aging on autoimmune neuroinflammatory responses remains uncertain33. Moreover, the augmented risk of depression in male patients with ON suggests that regulation of autoimmune neuroinflammatory responses might differ between genders through distinct, gender-specific mechanisms34. In the case of smokers with ON, temporary mood-enhancing effects of nicotine might lead to long-term disruptions in neurotransmission35, exacerbating the risk of depression possibly due to pre-existing neurochemical imbalances. Interestingly, ON patients who also suffered from hypertension appeared to exhibit a reduced risk for depression, suggesting that hypertension-related biological mechanisms might exert a protective effect on the interplay between ON and depression36,37. This observation warrants further exploration to elucidate underlying pathophysiological mechanisms linking ON to an increased risk of depression (especially among younger individuals, males, and smokers) and to understand the potential mitigating role of hypertension. Understanding these intricate relationships is crucial for developing targeted interventions aimed at mitigating depression risk among individuals with ON, especially among those identified as being at a greater risk.
When evaluating outcomes of this study, it is worthy to acknowledge several limitations. First, data on depression levels of participants at baseline were not accessible, raising the concern that those with ON might experience undiagnosed or subclinical depression potentially due to a decline in quality of life from visual impairments. Moreover, although our study identified depressive disorders through ICD-10 codes F32 and F33, we were unable to analyze outcomes based on the severity spectrum of depression due to inherent limitations of insurance claim data. Although this broad classification approach is a standard in nationwide cohort studies, it might not capture nuanced variations in depression severity among patients. The absence of comprehensive clinical information such as the severity of ON symptoms and specifics of treatment approaches might have also impacted conclusions of this study. Furthermore, due to inherent structural limitations of a retrospective nationwide population-based cohort study, we were unable to completely distinguish between different types of ON and their underlying conditions such as MS, NMOSD, and MOGAD, which could have varying impacts on visual prognosis and subsequent depression risk. However, our study design enabled analysis of an exceptionally large cohort that would be difficult to achieve in a prospective setting, providing valuable population-level insights. Future prospective studies could build upon these findings by examining how different underlying etiologies of ON and their associated visual outcomes contribute to depression risk, potentially elucidating differential impacts of MS-related, NMOSD-related, and other types of ON on patients’ psychological well-being. In addition, although we applied strict diagnostic criteria requiring either two outpatient visits or one inpatient admission with ICD-10 code H46, some potential for diagnostic misclassification between ON and other acute optic neuropathies remains. However, this risk is likely to be minimal in the Korean healthcare system where cases of uncertain diagnosis are typically coded as H47.0 rather than being classified as ON. Moreover, although this study accounted for a variety of confounders, unaccounted factors such as family history of depression, other past medical history, history of medication usage, and dietary habits might have influenced our results. Another critical point is the representativeness of our study cohort. Participants were primarily individuals enrolled in the mandatory NHSP health screening, which covers about 80% of all eligible persons38. Nonetheless, this group might not fully represent the broader population, as those enrolled in NHSP might inherently be more health-conscious or in better health than those who did not participate in the program39.
In conclusion, our research demonstrates that ON is significantly associated with a higher risk of depressive disorders, suggesting its potential role as an early indicator and an independent risk factor for depression across a broad segment of the population. It sheds light on the broader impact of autoimmune neuroinflammatory diseases in the pathogenesis of depression. Consequently, it is imperative to perform mental health assessments for individuals diagnosed with ON, with consideration for further neuropsychological evaluations to detect any underlying, unrecognized depressive conditions. Monitoring mood changes over time in ON patients is also crucial as such variations could signal the emergence or worsening of depression. The implementation of routine depression screening in ON patients, especially among younger individuals, males, and current smokers, along with lifestyle changes such as cessation of smoking, might play a significant role in mitigating the risk of developing depression and improving outcomes of patients at risk.
Methods
Research cohort and information repositories
The Republic of Korea maintains a comprehensive National Health Insurance Service (NHIS), mandating enrollment for nearly 97% of its population, with the balance receiving coverage through alternate schemes such as the Medical Aid program and benefits for Patriots and Veterans. This comprehensive coverage framework enables aggregation of extensive healthcare data into publicly accessible databases managed by the NHIS. These databases compile a vast array of healthcare information, including inpatient and outpatient services, emergency care, and prescription details. All of these are systematically organized based on Korean Standard Classification of Diseases (KCD)-7 codes. These codes align with the International Classification of Diseases, Tenth Revision (ICD-10) system. The NHIS also conducts a biennial National Health Screening Program (NHSP) for individuals aged 20 years or more.
For this nationwide retrospective study, we initially identified 40,608 individuals diagnosed with ON between 2010 and 2017 based on specific diagnostic criteria, including two outpatient visits or one inpatient admission with ICD-10 code H46. Following exclusions for various reasons such as lack of recent NHSP health screenings within two years, incomplete records, and prior depressive disorders, our analysis ultimately focused on 11,745 ON patients. Using identical exclusion criteria applied to the ON group, we identified 58,725 age- and sex-matched controls without ON (Fig. 1).
This study adhered to ethical standards as confirmed by the Samsung Medical Center’s Institutional Review Board (IRB) (IRB approval no. SMC 2023-05-098), adhering to the Declaration of Helsinki and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Due to its retrospective design and anonymized data use, the requirement of patient consent was exempted by the IRB of Samsung Medical Center.
Measurements, definitions, and outcomes
We gathered demographic information including age, sex, and monthly insurance contributions from the NHSP. Data on medical histories, health-related lifestyle habits, physical measurements (body mass index [BMI], waist circumference, blood pressure [BP]), and laboratory results (fasting blood glucose, cholesterol levels) were also obtained. Individuals who reported smoking or consuming alcohol daily were categorized accordingly. Physical activity was assessed based on either engaging in high-intensity activities such as running or heavy lifting that caused extreme breathlessness for at least 20 min three times weekly, or participating in moderate-intensity activities such as brisk walking or light lifting that caused considerable breathlessness for at least 30 min five days a week. We defined the lowest 25% income group as the low-income bracket. The formula for BMI calculation was an individual’s weight in kilograms divided by the square of height in meters. Obesity was classified when BMI was 25 kg/m2 or higher40. DM was identified with a fasting glucose level of 126 mg/dL or higher, or through ICD-10 codes E11–E14 in combination with treatment using insulin or oral hypoglycemic agents. Hypertension diagnosis involved BP measurements above 140 mmHg for systolic BP or above 90 mmHg for diastolic BP, or the presence of ICD-10 codes I10–I13 and I15 with antihypertensive medication usage. Dyslipidemia was indicated by total cholesterol level over 240 mg/dL or the use of cholesterol-lowering medications along with ICD-10 code E78. CKD was defined by a glomerular filtration rate below 60 mL/min/1.73 m2.
Our study aimed to detect new cases of depressive disorder denoted by ICD-10 codes F32 and F33 following our previous research41,42. The observation span for participants was until the diagnosis of depressive disorder, death, or the end of the study period on December 31, 2019, whichever came first.
Statistical analysis
For analyses of baseline characteristics, categorical data are presented as percentages (%), while continuous data are summarized using means and standard deviations (SDs). The investigation into survival rates free from depressive disorder utilized crude Kaplan–Meier survival curves. To assess the association between ON and the risk of depressive disorder, Cox proportional hazards regression models were applied after adjusting for a wide array of variables to calculate HRs and 95% CIs. The analysis progressed through four models. Model 1 was unadjusted. Model 2 was adjusted for age and sex. Model 3 was adjusted for age, sex, and lifestyle factors (such as smoking, alcohol consumption, regular exercise, income, and BMI). Model 4 was adjusted for age, sex, lifestyle factors (such as smoking, alcohol consumption, regular exercise, income, and BMI), and medical conditions (such as obesity, DM, hypertension, dyslipidemia, and CKD). Moreover, the analysis differentiated participants with ON from those without ON, offering stratifications by age (< 50 years or ≥ 50 years), sex, smoking status, alcohol consumption, regularity of physical activity, income level (comparing quartiles Q2–Q4 with Q1), and the presence of medical conditions such as obesity, DM, hypertension, dyslipidemia, and CKD. All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA), with a significance threshold set at p < 0.05.
Data availability
The data presented in this study can be accessed through the Korean National Health Insurance Service (KNHIS) database. Due to legal restrictions, the data cannot be publicly shared. However, the data are available for research purposes to any researcher who obtains approval from their institutional review board and submits a data request to the KNHIS. Qualified researchers can request access to the data by contacting the corresponding author or the KNHIS directly.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CKD:
-
Chronic kidney disease
- HRs:
-
Hazard ratios
- ICD-10:
-
International Classification of Diseases, Tenth Revision
- IRB:
-
Institutional review board
- KCD:
-
Korean standard classification of diseases
- MS:
-
Multiple sclerosis
- NHIS:
-
National health insurance service
- NHSP:
-
National health screening program
- NMOSD:
-
Neuromyelitis optica spectrum disorder
- ON:
-
Optic neuritis
- RA:
-
Rheumatoid arthritis
- SDs:
-
Standard deviations
- SLE:
-
Systemic lupus erythematosus
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
References
Moreno-Agostino, D. et al. Global trends in the prevalence and incidence of depression: A systematic review and meta-analysis. J. Affect. Disord. 281, 235–243. https://doi.org/10.1016/j.jad.2020.12.035 (2021).
Zhang, X. et al. Early-diagnosis of major depressive disorder: From biomarkers to point-of-care testing. TrAC Trends Anal. Chem. 159, 116904. https://doi.org/10.1016/j.trac.2022.116904 (2023).
Brann, E. et al. Bidirectional association between autoimmune disease and perinatal depression: A nationwide study with sibling comparison. Mol. Psychiatry 29, 602–610. https://doi.org/10.1038/s41380-023-02351-1 (2024).
Euesden, J., Danese, A., Lewis, C. M. & Maughan, B. A bidirectional relationship between depression and the autoimmune disorders - New perspectives from the National Child Development Study. PLoS One 12, e0173015. https://doi.org/10.1371/journal.pone.0173015 (2017).
Hesselvig, J. H., Egeberg, A., Kofoed, K., Gislason, G. & Dreyer, L. Increased risk of depression in patients with cutaneous lupus erythematosus and systemic lupus erythematosus: A Danish nationwide cohort study. Br. J. Dermatol. 179, 1095–1101. https://doi.org/10.1111/bjd.16831 (2018).
Wang, S. L. et al. Risk of developing depressive disorders following rheumatoid arthritis: A nationwide population-based study. PLoS One 9, e107791. https://doi.org/10.1371/journal.pone.0107791 (2014).
Andersson, N. W. et al. Depression and the risk of autoimmune disease: A nationally representative, prospective longitudinal study. Psychol. Med. 45, 3559–3569. https://doi.org/10.1017/S0033291715001488 (2015).
Roberts, A. L., Kubzansky, L. D., Malspeis, S., Feldman, C. H. & Costenbader, K. H. Association of depression with risk of incident systemic lupus erythematosus in women assessed across 2 decades. JAMA Psychiatry 75, 1225–1233. https://doi.org/10.1001/jamapsychiatry.2018.2462 (2018).
Braithwaite, T. et al. Trends in optic neuritis incidence and prevalence in the UK and association with systemic and neurologic disease. JAMA Neurol. 77, 1514–1523. https://doi.org/10.1001/jamaneurol.2020.3502 (2020).
Hassan, M. B. et al. Population-based incidence of optic neuritis in the era of aquaporin-4 and myelin oligodendrocyte glycoprotein antibodies. Am. J. Ophthalmol. 220, 110–114. https://doi.org/10.1016/j.ajo.2020.07.014 (2020).
Lee, J. Y., Han, J., Yang, M. & Oh, S. Y. Population-based incidence of pediatric and adult optic neuritis and the risk of multiple sclerosis. Ophthalmology 127, 417–425. https://doi.org/10.1016/j.ophtha.2019.09.032 (2020).
Sheline, Y. I., Sanghavi, M., Mintun, M. A. & Gado, M. H. Depression duration but not age predicts hippocampal volume loss in medically healthy women with recurrent major depression. J. Neurosci. 19, 5034–5043. https://doi.org/10.1523/JNEUROSCI.19-12-05034.1999 (1999).
Colizzi, M., Lasalvia, A. & Ruggeri, M. Prevention and early intervention in youth mental health: Is it time for a multidisciplinary and trans-diagnostic model for care?. Int. J. Ment. Health Syst. 14, 23. https://doi.org/10.1186/s13033-020-00356-9 (2020).
Rush, A. J. et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am. J. Psychiatry 163, 1905–1917. https://doi.org/10.1176/ajp.2006.163.11.1905 (2006).
Moussavi, S. et al. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet 370, 851–858. https://doi.org/10.1016/S0140-6736(07)61415-9 (2007).
Kessler, R. C. The costs of depression. Psychiatr. Clin. North Am. 35, 1–14. https://doi.org/10.1016/j.psc.2011.11.005 (2012).
Cui, L. et al. Major depressive disorder: Hypothesis, mechanism, prevention and treatment. Signal Transduct. Target. Ther. 9, 30. https://doi.org/10.1038/s41392-024-01738-y (2024).
Fries, G. R., Saldana, V. A., Finnstein, J. & Rein, T. Molecular pathways of major depressive disorder converge on the synapse. Mol. Psychiatry 28, 284–297. https://doi.org/10.1038/s41380-022-01806-1 (2023).
Raison, C. L., Capuron, L. & Miller, A. H. Cytokines sing the blues: Inflammation and the pathogenesis of depression. Trends Immunol. 27, 24–31. https://doi.org/10.1016/j.it.2005.11.006 (2006).
Troubat, R. et al. Neuroinflammation and depression: A review. Eur. J. Neurosci. 53, 151–171. https://doi.org/10.1111/ejn.14720 (2021).
Becher, B., Spath, S. & Goverman, J. Cytokine networks in neuroinflammation. Nat. Rev. Immunol. 17, 49–59. https://doi.org/10.1038/nri.2016.123 (2017).
Miller, A. H. Mechanisms of cytokine-induced behavioral changes: Psychoneuroimmunology at the translational interface. Brain Behav. Immun. 23(2), 149–158. https://doi.org/10.1016/j.bbi.2008.08.006 (2009).
Miller, A. H. & Raison, C. L. The role of inflammation in depression: From evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 16, 22–34. https://doi.org/10.1038/nri.2015.5 (2016).
Rhie, S. J., Jung, E. Y. & Shim, I. The role of neuroinflammation on pathogenesis of affective disorders. J. Exerc. Rehabil. 16, 2–9. https://doi.org/10.12965/jer.2040016.008 (2020).
Marano, G. et al. The microbiota-gut-brain axis: Psychoneuroimmunological insights. Nutrients 15, 1496. https://doi.org/10.3390/nu15061496 (2023).
Bennett, J. L. et al. Optic neuritis and autoimmune optic neuropathies: Advances in diagnosis and treatment. Lancet Neurol. 22, 89–100. https://doi.org/10.1016/S1474-4422(22)00187-9 (2023).
Lennon, V. A., Kryzer, T. J., Pittock, S. J., Verkman, A. S. & Hinson, S. R. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J. Exp. Med. 202, 473–477. https://doi.org/10.1084/jem.20050304 (2005).
Liu, Y. et al. Myelin-specific multiple sclerosis antibodies cause complement-dependent oligodendrocyte loss and demyelination. Acta Neuropathol. Commun. 5, 25. https://doi.org/10.1186/s40478-017-0428-6 (2017).
Ma, K. S. et al. Risk of autoimmune diseases following optic neuritis: A nationwide population-based cohort study. Front. Med. (Lausanne) 9, 903608. https://doi.org/10.3389/fmed.2022.903608 (2022).
Nagy, Z., Szigedi, E., Takacs, S. & Csaszar-Nagy, N. The effectiveness of psychological interventions for rheumatoid arthritis (RA): A systematic review and meta-analysis. Life Basel 13, 849. https://doi.org/10.3390/life13030849 (2023).
Parravano, M. et al. Association between visual impairment and depression in patients attending eye clinics: A meta-analysis. JAMA Ophthalmol. 139, 753–761. https://doi.org/10.1001/jamaophthalmol.2021.1557 (2021).
Pryce, C. R. & Fontana, A. Depression in autoimmune diseases. Curr. Top. Behav. Neurosci. 31, 139–154. https://doi.org/10.1007/7854_2016_7 (2017).
Musella, A. et al. Interplay between age and neuroinflammation in multiple sclerosis: Effects on motor and cognitive functions. Front. Aging Neurosci. 10, 238. https://doi.org/10.3389/fnagi.2018.00238 (2018).
Fonken, L. K. et al. Neuroinflammatory priming to stress is differentially regulated in male and female rats. Brain. Behav. Immun. 70, 257–267. https://doi.org/10.1016/j.bbi.2018.03.005 (2018).
Benowitz, N. L. Pharmacology of nicotine: Addiction, smoking-induced disease, and therapeutics. Annu. Rev. Pharmacol. Toxicol. 49, 57–71. https://doi.org/10.1146/annurev.pharmtox.48.113006.094742 (2009).
Penninx, B. W. Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neurosci. Biobehav. Rev. 74, 277–286. https://doi.org/10.1016/j.neubiorev.2016.07.003 (2017).
Schaare, H. L. et al. Associations between mental health, blood pressure and the development of hypertension. Nat. Commun. 14, 1953. https://doi.org/10.1038/s41467-023-37579-6 (2023).
Shin, D. W., Cho, J., Park, J. H. & Cho, B. National General Health Screening Program in Korea: History, current status, and future direction. Precis Future Med. 6, 9–31. https://doi.org/10.23838/pfm.2021.00135 (2022).
Dryden, R., Williams, B., McCowan, C. & Themessl-Huber, M. What do we know about who does and does not attend general health checks? Findings from a narrative scoping review. BMC Public Health 12, 723. https://doi.org/10.1186/1471-2458-12-723 (2012).
Kim, K. K. et al. Evaluation and treatment of obesity and its comorbidities: 2022 update of clinical practice guidelines for obesity by the Korean society for the study of obesity. J. Obes. Metab. Syndr. 32, 1–24. https://doi.org/10.7570/jomes23016 (2023).
Hwang, S. et al. Impact of age-related macular degeneration and related visual disability on the risk of depression: A nationwide cohort study. Ophthalmology 130, 615–623. https://doi.org/10.1016/j.ophtha.2023.01.014 (2023).
Jeon, K. H. et al. Rheumatoid arthritis and risk of depression in south Korea. JAMA Netw. Open 7, e241139. https://doi.org/10.1001/jamanetworkopen.2024.1139 (2024).
Funding
This research was supported by a grant (grant number: RS-2024-00341030, awarded to Kyung-Ah Park) from the National Research Foundation (NRF) funded by the Ministry of Science and ICT, Republic of Korea and a grant (grant number: RS-2024-00439930, awarded to Jaeryung Kim) from the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health and Welfare, Republic of Korea, with neither funding body participating in the study’s design or execution.
Author information
Authors and Affiliations
Contributions
JK, SJ, SYO, KAP, and JHM contributed to the conception and design of this study. JK, KH, JJ, KAP, and JHM contributed to the acquisition and analysis of data. JK, JC, KAP, and JHM drafted the text and prepared figures.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, J., Jang, S., Choi, J. et al. Association of optic neuritis with incident depressive disorder risk in a Korean nationwide cohort. Sci Rep 15, 7764 (2025). https://doi.org/10.1038/s41598-025-92370-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92370-5