Abstract
The progression of Alzheimer’s disease (AD) and its interaction with COVID-19-induced social isolation remains poorly understood. This study investigated the longitudinal trajectories of AD severity on cognitive function, functional ability, and neuropsychiatric symptoms, and examined the impact of COVID-19 lockdown on AD patients in South Korea. In this retrospective longitudinal study, data from 253 adults (aged ≥ 55) diagnosed with mild cognitive impairment (MCI) or AD were analyzed, collected between 2018 and 2022. Participants were classified into four groups based on clinical dementia rating (CDR) scores: MCI, AD-CDR0.5, AD-CDR1, and AD-CDR2. Cognitive function, functional abilities, neuropsychiatric symptoms, depressive symptoms, and overall dementia severity were assessed. Linear mixed-effects models, along with mediation and moderation analyses were employed to analyze the data. Significant trajectories of decline in cognitive function and functional abilities were observed over time, with more pronounced declines in higher AD severity groups. The COVID-19 lockdown exacerbated cognitive decline and impairment in activities of daily living (ADL) specifically in the most severe AD group (AD-CDR2). Instrumental activities of daily living (IADL) mediated the relationship between mini-mental state examination (MMSE) scores and CDR sum of boxes (CDR-SB) in the MCI, AD-CDR0.5, and AD-CDR1 groups. A significant interaction between MMSE scores and neuropsychiatric symptoms was observed in the moderate AD group (AD-CDR1), indicating that worsening neuropsychiatric symptoms intensified cognitive decline. Neuropsychiatric Inventory (NPI) scores increased over time, indicating worsening neuropsychiatric symptoms, whereas depressive symptoms, measured by the short geriatric depression scale (SGDS), remained stable over the study period. This study highlights the impact of AD severity on cognitive and functional decline, further exacerbated by the COVID-19 lockdown. The mediating role of IADL suggests that maintaining complex daily activities may be crucial in slowing disease progression in AD patients. Additionally, the worsening of neuropsychiatric symptoms underscores the need for targeted mental health support, especially during periods of social isolation, to mitigate adverse effects on patients and caregivers.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder characterized by a gradual decline in cognitive functions and daily living abilities, along with various neuropsychiatric symptoms. This decline typically follows a predictable pattern, beginning with subtle memory impairments and mild difficulties in complex activities, and progressing to more severe cognitive deficits and loss of independence in daily activities1,2. As the global population ages, the prevalence of AD is expected to rise, posing significant challenges for healthcare systems and caregivers alike2,3.
Recent research has highlighted the significant impact of social isolation and quarantine measures on individuals with dementia, including those with AD. Studies have reported substantial behavioral and psychological effects of quarantine on dementia patients, emphasizing their heightened vulnerability during such periods4,5. Social isolation has been shown to accelerate cognitive decline in older adults, including those with AD6,7,8. Mok and colleagues found that disrupted care routines were associated with exacerbated neuropsychiatric symptoms in AD patients, suggesting that the severity of AD might influence the degree of vulnerability to these effects8.
Given the variability in AD severity, the impact of lockdown may not be uniform across all individuals with AD. It is plausible that those with milder AD may experience less severe impacts, or even some protective effects, due to the reduced external stressors and simplified routines during lockdown periods9,10. However, individuals with more severe AD may face a greater risk of exacerbated cognitive and functional decline due to their heightened dependence on consistent care and social interaction.
In addition to the severity of AD, functional abilities are typically categorized into activities of daily living (ADL), which encompass basic self-care tasks, and instrumental activities of daily living (IADL), which involve more complex tasks requiring higher cognitive function. While ADL are often preserved until the later stages of AD, IADL tend to decline earlier, making them critical indicators of disease progression. Functional abilities, such as managing daily tasks, can influence the relationship between cognitive function and the overall severity of dementia11. During the COVID-19 pandemic, pandemic-induced social isolation may make these functional abilities even more critical in determining the course of the disease.
Neuropsychiatric symptoms, such as agitation, anxiety, irritability, and apathy, have been associated with faster cognitive decline and functional impairment in AD12. These symptoms might not only exacerbate cognitive and functional decline but also moderate the relationship between cognitive function and daily living abilities. The Neuropsychiatric Inventory (NPI) is a tool commonly used to assess these symptoms13. Siafarikas suggested that neuropsychiatric symptoms may reinforce cognitive decline in AD and could serve as clinical markers for incipient dementia13. Understanding how neuropsychiatric symptoms moderate the relationship between cognitive function and functional abilities is essential for developing targeted interventions that can alleviate the compounded effects of these symptoms on disease progression.
The role of depression in AD progression has also gained considerable attention. Previous studies have suggested that depressive symptoms can exacerbate cognitive decline in AD patients14,15,16. Wang and colleagues found that a formal diagnosis of depression was a stronger predictor of cognitive decline than the presence of depressive symptoms alone, based on data from a large electronic health record-based cohort15. This suggests that the severity of depressive symptoms may be an important factor in cognitive decline. Additionally, Zheng and colleagues reported that older adults with depressive symptoms suffered more severe cognitive deterioration and had a higher risk of incident dementia during the COVID-19 pandemic16. These findings underscore the importance of considering initial depressive symptoms as a potential predictor or accelerated decline, particularly under the stressful conditions of a lockdown.
Despite this growing body of research, several important gaps remain in our understanding of how social isolation and lockdown affect AD progression. First, most studies have focused on short-term effects, with limited investigation of longitudinal impacts. Second, the differential effects across various stages of AD severity have not been fully elucidated. Third, the potential mediating role of functional abilities in the relationship between cognitive decline and overall dementia severity during periods of social isolation has not been explored in depth. Additionally, the moderating role of neuropsychiatric symptoms on this relationship requires further investigation.
This study aims to address these gaps by investigating the longitudinal effects of AD severity on cognitive function, functional ability, and neuropsychiatric symptoms in South Korea, with a specific focus on the impact of COVID-19 social distance. We hypothesize that:
-
1.
AD severity will be associated with faster cognitive decline, greater functional impairment, and increased neuropsychiatric symptoms over time.
-
2.
The impact of COVID-19 lockdown will vary across AD severity groups, with more severe AD patients experiencing greater negative effects on cognitive function, functional ability, and neuropsychiatric symptoms.
-
3.
Functional abilities (ADL and IADL) will mediate the relationship between cognitive function (MMSE) and overall dementia severity (CDR-SB), with this mediation effect being more pronounced during the lockdown period.
-
4.
Initial depressive symptoms (SGDS scores) will be associated with accelerated cognitive decline, functional impairment, and increased neuropsychiatric symptoms, particularly during the lockdown period.
-
5.
Neuropsychiatric symptoms (NPI scores) will moderate the relationship between cognitive function (MMSE) and functional abilities (ADL and IADL), with higher NPI scores strengthening this relationship, especially during the lockdown period.
By examining these relationships through a comprehensive longitudinal analysis, this study seeks to provide deeper insights into the progression of AD under conditions of social isolation and the complex interplay between cognitive, functional, and neuropsychiatric factors.
Methods
Study design and participants
We conducted a retrospective longitudinal study using data collected from January 2018 to December 2022 at the Dementia Clinic of Seoul Metropolitan Government-Seoul National University Boramae Medical Center, South Korea. The study population included 253 adults aged 55 years or older who had been diagnosed with Alzheimer’s Disease according to the NINCDS-ADRDA criteria17, or with mild cognitive impairment (MCI) based on Petersen’s criteria18. Participants were classified into four groups based on their diagnosis and Clinical Dementia Rating Global Score (CDR-Global): MCI (CDR-Global = 0.5 and not meeting AD criteria), AD-CDR0.5 (CDR-Global = 0.5 and meeting AD criteria), AD-CDR1 (CDR-Global = 1), and AD-CDR2 (CDR-Global = 2).
Descriptive statistics, including means, standard deviations (SD), and ranges, were reported for all key variables (CDR-SB, MMSE, IADL, ADL, NPI, SGDS, Age, Education years) to summarize the baseline characteristics of the study population (Table 1). Participants underwent neuropsychiatric evaluations at least annually, conducted by trained neuropsychologists following standardized procedures. To ensure a consistent longitudinal dataset for analyzing changes across the pre-lockdown and lockdown periods, only participants who completed at least two neuropsychiatric evaluations before the COVID-19 lockdown (pre-lockdown period) and at least two evaluations after the lockdown began (lockdown period) were included in the analysis. Each evaluation was conducted independently, with each participant serving as their own control over time to account for within-individual variations. Neuropsychologists conducting the annual evaluations were blinded to the study hypotheses to minimize assessment bias.
The COVID-19 lockdown in South Korea began on March 22, 2020, when the government elevated the alert level to ‘serious’, leading to school closures, work-from-home policies, and restrictions on public gatherings. The lockdown and various levels of social distancing measures continued throughout the study period, with some measures extending beyond December 2022.
Ethical considerations
This study was approved by the Institutional Review Board (IRB) of Seoul National University Boramae Medical Center (Approval Number: 10-2020-295). The requirement for informed consent was waived due to the retrospective nature of the study, as all data were anonymized and de-identified prior to analysis. The study adhered to the principles of the Helsinki Declaration.
Measures
Dementia severity
Dementia severity was assessed using the Korean version of the Clinical Dementia Rating scale (CDR), with the CDR-Sum of Boxes (CDR-SB) scores employed to evaluate the severity of dementia symptoms. The CDR-SB score ranges from 0 to 18, with higher scores indicating more severe dementia19.
Cognitive function
Cognitive function was measured using the Mini-Mental State Examination in the Korean version of the CERAD Assessment Packet (MMSE-KC). This scale evaluates multiple cognitive domains, including orientation, registration, attention, calculation, recall, and language abilities. Scores range from 0 to 30, with higher scores reflecting better cognitive performance20.
Functional ability
Functional ability was assessed using two scales:
Instrumental activities of daily living (IADL)
The Korean version of the Lawton instrumental activities of daily living (IADL) scale evaluates complex daily activities such as telephone use, shopping, transportation, medication management, and financial management. Lower scores indicated better functional ability21.
Activities of daily living (ADL)
The Barthel ADL Index measures performance in 10 basic activities of daily living, including feeding, bathing, grooming, dressing, bowel control, bladder control, toilet use, transfers, mobility, and stair climbing. Scores range from 0 to 20, with higher scores indicating greater independence in daily activities22,23.
Neuropsychiatric symptoms
Neuropsychiatric symptoms were evaluated using the Korean version of the Neuropsychiatric Inventory (K-NPI). The K-NPI assesses 12 neuropsychiatric disturbances common in dementia, including their frequency and severity as reported by caregivers. Scores range from 0 to 144, with higher scores indicating more severe behavioral symptoms19.
Depressive symptoms
Depressive symptoms were evaluated using the Korean version of the Short Geriatric Depression Scale (SGDS-K). This 15-item scale is specifically designed to assess depression in older adults. Scores range from 0 to 15, with higher scores indicating more severe depressive symptoms24.
Data preprocessing and analysis
Missing data were handled using available case analysis, which utilizes all available data for each analysis to minimize information loss. This approach minimizes bias and increases the robustness of the analysis. Key variables (CDR-SB, MMSE, IADL, ADL, NPI, SGDS, Age, Education years) were standardized using z-score transformation to enhance comparability across variables. For longitudinal analysis, a time variable in years was generated, setting each participant’s first visit as the baseline (0). This variable quantified the time elapsed since the initial evaluation for each participant.
Statistical analysis
Longitudinal analysis
Linear mixed-effects models were used to analyze longitudinal changes in cognitive function (MMSE), daily living abilities (IADL, ADL), and neuropsychiatric symptoms (NPI) and depressive symptoms (SGDS). These models account for both within-individual (time-based) and between-individual (group-based) variations25. The model structure include fixed effects for time, AD Severity group, their interaction, and covariates such as initial depressive symptoms (SGDS), age, sex, and education level. Random effects included random intercepts and slopes for each individual to capture individual-specific trajectories over time.
Where \(\:{Y}_{ij}\) represents the normalized outcome variable for individual \(\:i\) at time \(\:j\), \(\:{u}_{0i}\) is the random intercept, \(\:{u}_{1i}\)is the random slope for time, and \(\:{\epsilon}_{ij}\) is the residual error.
COVID-19 lockdown impact analysis
To assess the impact of the COVID-19 lockdown on longitudinal changes, we incorporated lockdown status and its interactions with time and AD severity into the mixed effects models.
This model evaluates whether the lockdown period differentially affected the trajectories of the outcome variables across AD Severity groups.
Initial depression effect analysis
To investigate the influence of initial depressive symptoms on the progression of dementia-related outcomes, we modeled the interaction between time and initial SGDS scores.
This model assesses how initial depressive symptoms modify the trajectory of cognitive and functional outcomes over time.
Mediation analysis
We conducted causal mediation analyses with bootstrapping (1,000 repetitions) to explore whether functional abilities (ADL and IADL) and neuropsychiatric symptoms (NPI) mediate the relationship between cognitive function (MMSE) and dementia severity (CDR-SB). These analyses were performed separately for each AD Severity group to account for potential group-specific mediation pathways. Linear mixed-effects models were employed for both the mediator and outcome models to accommodate the longitudinal data structure.
Moderation analysis
Moderation analyses examined whether the relationship between cognitive function (MMSE) and dementia severity (CDR-SB), as well as the relationship between functional abilities (ADL and IADL) and dementia severity, were influenced by neuropsychiatric symptoms (NPI), lockdown status, and sex. Interaction terms between predictors (e.g., MMSE, NPI) and moderators (e.g., lockdown, sex) were included in the mixed-effects models to assess these potential moderating effects.
Multiple comparisons correction
To mitigate the risk of Type I errors due to multiple hypothesis testing, we applied both Bonferroni correction and False Discovery Rate (FDR) correction across all analyses. Bonferroni correction was utilized to adjust for family-wise error rates in the primary longitudinal analyses, while FDR correction was employed to control the expected proportion of false discoveries across multiple tests in secondary analyses, including mediation and moderation assessments.
Statistical software
All statistical analyses were performed using R software (version 4.4.1). The lme4 and lmerTest packages were used for linear mixed-effects modeling, mediation for mediation analyses, and emmeans for estimated marginal means and trend analysis. Graphical representations were created using ggplot2 and patchwork. Statistical significance was set at p < 0.05 for all tests26.
Results
Longitudinal changes in cognitive function, functional ability, and neuropsychiatric symptoms
Cognitive function (MMSE and CDR-SB)
Both MMSE and CDR-SB scores significantly changed over time, indicating a decline in cognitive function over time (see Fig. 1 for longitudinal trends and Table 2 for detailed statistical results). Specifically, MMSE scores decreased by an average of 0.137 points per unit time (β = −0.137, SE = 0.025, p < 0.001), while CDR-SB scores increased significantly (β = 0.106, SE = 0.019, p < 0.001). Participants with more severe AD had lower MMSE scores and higher CDR-SB scores compared to those with MCI (p < 0.001 for all comparisons). Additionally, the rate of cognitive decline was faster in participants with higher AD severity, as evidenced by the significant interaction between time and AD severity for both MMSE (F = 55.11, p < 0.001) and CDR-SB (F = 2.97, p = 0.032). Age was also associated with higher CDR-SB scores (β = 0.082, SE = 0.040, p = 0.002).
Longitudinal changes in cognitive function, functional ability, and neuropsychiatric symptoms by AD severity. Longitudinal changes in CDR-SB, MMSE, IADL, ADL, NPI, SGDS scores across different AD severity groups. The red dashed line indicates the onset of the COVID-19 lockdown. AD Alzheimer’s disease, CDR-SB clinical dementia rating sum of boxes, MMSE mini-mental state examination, IADL instrumental activities of daily living, ADL activities of daily living, NPI neuropsychiatric inventory, SGDS short geriatric depression scale.
Functional ability (ADL and IADL)
There was a significant decline in both ADL and IADL over time (ADL: β = 0.138, SE = 0.019, p < 0.001; IADL: β = 0.124, SE = 0.014, p < 0.001) (see Fig. 1; Table 2). Participants with higher AD severity showed more significant impairments in both ADL and IADL compared to the MCI group (p < 0.001 for all comparisons). Specifically, the AD-CDR2 group exhibited the most rapid decline in ADL (p = 0.005) and IADL (p < 0.001) compared to the MCI group. Additionally, higher age was associated with higher IADL scores (β = 0.157, SE = 0.041, p < 0.001), indicating greater functional impairment.
Neuropsychiatric symptoms (NPI) and depression (SGDS)
NPI scores increased significantly over time (β = −0.091, SE = 0.035, p = 0.011), indicating worsening neuropsychiatric symptoms. *(Note: The negative β value reflects the standardized scaling of the NPI variable, where higher values correspond to more severe symptoms.) Participants with more severe AD had higher NPI scores compared to those with MCI (p < 0.001). However, the interaction between time and AD severity was not significant (p = 0.051), suggesting that the rate of change in NPI scores over time did not differ substantially across AD severity groups. Depression scores (SGDS) did not show significant changes over time (p = 0.645) and were not significantly affected by AD severity (p = 0.951).
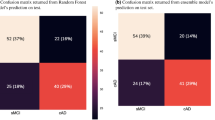
Impact of COVID-19 lockdown
The COVID-19 lockdown period had varying effects on different outcomes across AD severity groups (see Fig. 2). MMSE scores showed a significant decline in the AD-CDR2 group during the lockdown period (p = 0.019). The AD-CDR2 group also experienced a significant decline in ADL performance during lockdown (p = 0.002). IADL scores did not show a significant effect of lockdown across any of the AD severity groups (p = 0.356). There was a marginally significant overall effect of lockdown on NPI scores (p = 0.0367, adjusted p = 0.064). Specifically, the AD-CDR2 group showed a significant increase in NPI scores during the lockdown period (p < 0.005). SGDS scores were not significantly affected by the lockdown across AD severity groups (p = 0.855).
Impact of COVID-19 lockdown on longitudinal changes. The effect of COVID-19 lockdown on CDR-SB, MMSE, IADL, ADL, NPI, SGDS scores across different AD severity groups. The red dashed line indicates the onset of the lockdown. AD Alzheimer’s disease, CDR-SB clinical dementia rating sum of boxes, MMSE mini-mental state examination, IADL instrumental activities of daily living, ADL activities of daily living, NPI neuropsychiatric inventory, SGDS short geriatric depression scale.
Mediation analysis
IADL significantly mediated the relationship between MMSE and CDR-SB in the MCI (indirect effect: −0.130, 95% CI [−0.210, -0.050], p = 0.001), AD-CDR0.5 (indirect effect: 0.046, 95% CI: [0.012, 0.081], p = 0.008), and AD-CDR1 groups (indirect effect: −0.041, 95% CI [−0.070, −0.012], p = 0.005) (see Table 3; Fig. 3). ADL did not show significant mediation effects in any of the groups.
Mediation effects of functional abilities on the relationship between cognitive function and dementia severity in Alzheimer’s disease. This diagram illustrates the mediation model, where functional abilities (mediator: IADL) mediate the relationship between cognitive function (MMSE) and dementia severity (CDR). The total effect (C) is composed of the indirect effect (A x B) through functional abilities and the direct effect (C’) between cognitive function and dementia severity. MMSE mini-mental state examination, CDR clinical dementia rating, IADL instrumental activities of daily living.
Moderation analysis
The interaction between MMSE scores and NPI was significant for the AD-CDR1 group (p = 0.036), indicating that cognitive decline was associated with worsening neuropsychiatric symptoms in participants with moderate AD. Other interactions between cognitive function, functional ability, and neuropsychiatric symptoms did not reach statistical significance across the different AD severity groups.
Depression effect analysis
Initial SGDS scores had significant effects on several outcomes. For ADL, higher initial SGDS scores were associated with lower ADL performance (β = -0.087, SE = 0.041, p = 0.036). For NPI, higher initial SGDS scores were associated with higher NPI scores (β = 0.304, SE = 0.054, p < 0.001) and also influenced the change in NPI scores over time (β = -0.052, SE = 0.017, p = 0.003). Additionally, higher initial SGDS scores were significantly associated with higher CDR-SB scores (p < 0.001). However, initial SGDS scores did not significantly affect MMSE (p = 0.681) or IADL (p = 0.217) outcomes.
Discussion
This longitudinal study demonstrated that AD severity significantly influenced the trajectories of cognitive function, functional ability, and neuropsychiatric symptoms in South Korean older adults. The COVID-19 lockdown had differential effects across AD severity groups, with the most severe group (AD-CDR2) experiencing the greatest declines in cognitive function and ADL performance. IADL mediated the relationship between cognitive function and overall dementia severity in the MCI, AD-CDR0.5, and AD-CDR1 groups. Furthermore, Neuropsychiatric symptoms moderated the relationship between cognitive function and functional ability in the AD-CDR1 group. Initial depressive symptoms were associated with lower ADL performance, higher NPI scores, and influenced the trajectory of NPI scores over time.
The observed decline in cognitive function and functional abilities aligns with established knowledge about AD progression, corroborating the systematic review by Cummings and colleagues (2023)27. This review highlighted predictable declines in both cognitive and functional domains as AD progresses, correlating strongly with CDR scale progression. These findings emphasize the importance of early detection and intervention in cognitive and functional impairments, which may help mitigate the adverse effects of AD progression on patients’ quality of life and caregivers’ burden18,28.
The differential impact of COVID-19 lockdown across AD severity groups highlights the elevated risk to cognitive and functional decline of severe AD patients when exposed to environmental stressors. This finding is consistent with previous research on the effects of social isolation, which has shown that such isolation accelerates cognitive decline in older adults with AD4,5,8. The exacerbation of cognitive and functional declines in severe AD patients during lockdown underscores the need for targeted interventions and support strategies that consider the specific challenges faced by this population during global health crises.
A worsening of neuropsychiatric symptoms among participants over time aligns with previous studies that have documented the progression of behavioral and psychological symptoms in AD patients over time. Participants with more severe AD exhibited higher NPI scores compared to those with MCI underscores the association between disease severity and the prevalence of neuropsychiatric disturbances. Although the interaction between time and AD severity was not statistically significant, the trend suggests that while neuropsychiatric symptoms worsen over time, the rate of this deterioration does not significantly differ across varying levels of AD severity. The increase in NPI scores over time may be attributable to several mechanisms. Prolonged social isolation and reduced caregiver interactions during the COVID-19 lockdown could exacerbate behavioral disturbances due to increased frustration and decreased social stimulation.
The stable depressive symptoms (SGDS) among the study periods suggests that depressive symptoms may remain relatively constant throughout the progression of AD. This finding contrasts with some studies that have reported fluctuating depression levels in AD patients, potentially influenced by various factors such as caregiver support, environmental changes, or intervention strategies. The lack of significant change in SGDS scores may also indicate effective management of depressive symptoms through ongoing care or therapeutic interventions. However, it is essential to consider that the retrospective design of this study might have limitations in capturing subtle changes in depression over time. Future research should employ longitudinal designs with more frequent assessments to better understand the trajectory of depressive symptoms in AD populations.
The mediation analysis revealed that functional abilities partially mediate the relationship between cognitive function (MMSE scores) and overall dementia severity (CDR-SB). This finding emphasizes the critical role of functional decline in determining disease severity and progression, adding to the growing body of evidence that functional impairment is not merely a consequence of cognitive deterioration but also a crucial factor in shaping the overall disease course11,29,30. The stronger mediating effect of IADL compared to ADL suggests that complex instrumental activities may be more sensitive indicators of disease progression than basic daily activities. This underscores the importance of assessing and targeting IADL in the management of AD, particularly in the earlier stages of the disease.
In contrast, activities of daily living (ADL) did not exhibit significant mediation effects in any of the groups. This lack of mediation indicates that basic daily activities may not directly influence the pathway between cognitive decline and dementia severity, possibly because ADL tasks are less sensitive to subtle cognitive changes compared to IADL tasks. ADL measures may capture more fundamental aspects of daily functioning that remain relatively stable until later stages of AD, whereas IADL tasks, being more complex, are more responsive to cognitive fluctuations. Additionally, since the MCI group maintained normal IADL and ADL functions, it suggests that while IADL can mediate the relationship in groups with some functional impairment, ADL remains unaffected in the earliest stages of cognitive decline. Another possible explanation is the influence of other unmeasured variables, such as social support, caregiver burden, or physical health status, which might impact ADL independently of cognitive function and dementia severity. This distinction underscores the importance of focusing on IADL assessments in early to moderate stages of AD to better understand and monitor disease progression.
The moderation analysis revealed that neuropsychiatric symptoms (NPI) moderate the relationship between cognitive function (MMSE) and functional ability in the mild to moderate AD group (AD-CDR1). This finding suggests that behavioral symptoms may exacerbate cognitive decline and serve as early indicators of worsening dementia12,13. The interplay between cognitive function, neuropsychiatric symptoms, and functional ability in this stage of AD highlights the importance of a comprehensive approach to assessment and management that considers the complex interactions between these domains. Interventions targeting neuropsychiatric symptoms in moderate AD may have the potential to mitigate cognitive decline and functional impairment, thereby improving overall disease outcomes.
Initial SGDS scores had significant effects on several outcomes. For ADL, higher initial SGDS scores were associated with lower ADL performance. For NPI, higher initial SGDS scores were associated with higher NPI scores and also influenced the change in NPI scores over time. Additionally, higher initial SGDS scores were significantly associated with higher CDR-SB scores. These results align with previous studies that have demonstrated an association between depressive symptoms and accelerated cognitive decline, functional impairment, and increased neuropsychiatric symptoms in AD patients14,15,16. The impact of initial depression levels on the progression of behavioral disturbances in AD emphasizes the necessity of early screening and management of depressive symptoms in this population. Incorporating depression assessment and treatment into the comprehensive care of AD patients may help mitigate the adverse effects of depression on functional abilities and neuropsychiatric symptoms, potentially improving overall disease outcomes.
Our findings have important clinical implications, underscoring the need for a holistic approach to AD management that addresses cognitive, functional, neuropsychiatric, and affective domains. The significant impact of initial depression levels on ADL and NPI outcomes emphasizes the importance of early depression screening and treatment in AD care. Integrating mental health support with cognitive and functional interventions can mitigate the adverse effects on functional abilities and neuropsychiatric symptoms, potentially improving overall disease prognosis.
Additionally, the varying impacts of lockdown across AD severity groups suggest that care strategies during global crises should be tailored to the stage of cognitive impairment. For instance, severe AD patients (AD-CDR2) may benefit from enhanced remote monitoring, increased caregiver support, and structured daily routines to counteract the negative effects of social isolation and disrupted routines. Healthcare providers and caregivers should be aware of the heightened vulnerability of this group and implement targeted interventions to support their cognitive, functional, and emotional well-being during challenging times.
Furthermore, the mediating role of IADL in the relationship between cognitive function and overall dementia severity highlights the potential benefits of interventions aimed at maintaining functional independence in AD patients. Occupational therapy, cognitive rehabilitation, and caregiver training programs that focus on enhancing IADL skills may help slow the progression of dementia and improve patients’ quality of life. Future research should explore the efficacy of such interventions in different stages of AD and investigate additional mediators that could influence disease progression. Additionally, developing targeted interventions that address both cognitive and functional domains concurrently could provide more effective strategies for managing AD progression.
This study has several limitations. As a single-center study in South Korea, its generalizability may be limited to similar populations and healthcare settings. The retrospective design prevents control of all potential confounding factors, such as changes in medication usage, caregiver support, or environmental influences over time. Specifically, the study did not account for the usage rates of medications such as antidepressants, cholinesterase inhibitors, or antipsychotics, which could influence cognitive function and neuropsychiatric symptoms in dementia patients. Future studies should incorporate detailed meditation profiles to better elucidate their potential moderating or mediating effects on Alzheimer’s disease progression, particularly under conditions of social isolation. While we used widely accepted measurement tools (MMSE, NPI, CDR), these instruments have inherent limitations, including potential ceiling or floor effects that may affect sensitivity to changes. Although the depression effect analysis yielded significant results, the causal relationship between initial depression and AD progression cannot be definitively established due to the study’s retrospective nature. Future prospective studies with more comprehensive assessments of depression, medication use, and other potential confounders are needed to validate these findings. Additionally, research should explore the long-term effects of external stressors like lockdowns on AD progression and investigate interventions targeting functional abilities to develop strategies for mitigating cognitive decline in AD patients.
Conclusions
This study contributes to the understanding of AD progression by confirming and extending previous findings on the complex interplay between cognitive decline, functional impairment, neuropsychiatric symptoms, and depressive symptoms. Our findings emphasize the importance of a comprehensive approach to AD management, considering the differential impact of COVID-19 lockdown across AD severity groups and the mediating and moderating factors identified. As the global population ages and the prevalence of AD continues to rise, it is crucial to integrate these insights into clinical practice and future research. This integration will facilitate the development of personalized, evidence-based interventions and support systems. These approaches can adapt to the changing needs of patients and their caregivers, ultimately improving the care and quality of life for individuals affected by AD. Such adaptability is particularly important in the face of unprecedented challenges like the COVID-19 pandemic.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy concerns and institutional data sharing policies but are available from the corresponding author upon reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- ADL:
-
Activities of daily living
- CDR:
-
Clinical dementia rating
- CDR-SB:
-
Clinical dementia rating sum of boxes
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- FDR:
-
False discovery rate
- IADL:
-
Instrumental activities of daily living
- IRB:
-
Institutional review board
- K-NPI:
-
Korean version of the neuropsychiatric inventory
- MCI:
-
Mild cognitive impairment
- MMSE:
-
Mini-mental state examination
- MMSE-KC:
-
Mini-mental state examination in the Korean version of the CERAD assessment packet
- NINCDS-ADRDA:
-
National institute of neurological and communicative disorders and stroke and the Alzheimer’s disease and related disorders association
- NPI:
-
Neuropsychiatric inventory
- SD:
-
Standard deviation
- SGDS:
-
Short geriatric depression scale
- SGDS-K:
-
Korean version of the short geriatric depression scale
References
Jack, C. R. Jr et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14 (4), 535–562 (2018).
Scheltens, P. et al. Alzheimer’s disease. Lancet 397 (10284), 1577–1590 (2021).
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 396 (10248), 413–446 (2020).
Boutoleau-Bretonnière, C. et al. The effects of confinement on neuropsychiatric symptoms in Alzheimer’s disease during the COVID-19 crisis. J. Alzheimers Dis. 76 (1), 41–47 (2020).
Cagnin, A. et al. Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front. Psychiatr. 11, 578015 (2020).
Evans, I. E. M. et al. Social isolation, cognitive reserve, and cognition in healthy older people. PLoS One 13 (8), e0201008 (2018).
Kuiper, J. S. et al. Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 22, 39–57 (2015).
Mok, V. C. T. et al. Tackling challenges in care of Alzheimer’s disease and other dementias amid the COVID-19 pandemic, now and in the future. Alzheimers Dement. 16 (11), 1571–1581 (2020).
Chandler, J. M., Ye, W., Mi, X., Doty, E. G. & Johnston, J. A. Potential impact of slowing disease progression in early symptomatic Alzheimer’s disease on patient quality of life, caregiver time, and total societal costs: estimates based on findings from GERAS-US study. J. Alzheimers Dis. 100 (2), 563–578 (2024).
Dubbelman, M. A. et al. Decline in everyday functioning in relation to cerebral tau burden across the clinical spectrum of Alzheimer’s disease. Alzheimers Dement. 19 (S18). https://doi.org/10.1002/alz.075056 (2023).
Fujii, K. et al. Mediating role of instrumental activities of daily living ability on cognitive function of older adults living alone: A 4-year longitudinal study from the Kasama study. Medicine 100 (40), e27416 (2021).
Chen, Y. J., Chang, M. C., Jhang, K. M., Wang, W. F. & Liao, Y. C. Neuropsychiatric symptoms predict faster cognitive decline in dementia collaborative care than antipsychotic use. Neuropsychiatr. Dis. Treat. 20, 689–696 (2024).
Siafarikas, N. Neuropsychiatric and cognitive symptoms: two sides of the same coin? J. Alzheimers Dis. 98 (1), 75–78 (2024).
Desai, P. et al. Associations between depressive symptoms, glial fibrillary acid protein, and cognitive decline in a population-based study. Alzheimers Dement. 19 (S15). https://doi.org/10.1002/alz.075850 (2023).
Wang, F. et al. A systematic review and meta-analysis of 90 cohort studies of social isolation, loneliness and mortality. Nat. Hum. Behav. 7 (8), 1307–1319 (2023).
Zheng, F., Liang, J., Li, C., Gao, D. & Xie, W. Cognitive decline among older adults with depressive symptoms before and during the COVID-19 pandemic. J. Affect. Disord. 344, 407–413 (2024).
McKhann, G. et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 34 (7), 939–944 (1984).
Petersen, R. C. et al. Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology. Neurology 90 (3), 126–135 (2018).
Choi, S. H. et al. The Korean version of the neuropsychiatric inventory: a scoring tool for neuropsychiatric disturbance in dementia patients. J. Korean Med. Sci. 15 (6), 609–615 (2000).
Lee, J. H. et al. Development of the Korean version of the consortium to Establish a registry for Alzheimer’s disease assessment packet (CERAD-K): clinical and neuropsychological assessment batteries. J. Gerontol. B Psychol. Sci. Soc. Sci. 57 (1), P47–53 (2002).
Kim, S., Won, J. W. & Cho, K. The validity and reliability of Korean version of Lawton IADL index. J. Korean Geriatr. Soc. 9, 23–29 (2005).
Mahoney, F. I. & Barthel, D. W. Functional evaluation: the Barthel index. Md. State Med. J. 14, 61–65 (1965).
Kim, S. Y., Won, C. W. & Rho, Y. G. The validity and reliability of Korean version of bathel ADL index. J. Korean Acad. Family Med. 25 (7), 534–541 (2004).
Bae, J. N. & Cho, M. J. Development of the Korean version of the geriatric depression scale and its short form among elderly psychiatric patients. J. Psychosom. Res. 57 (3), 297–305 (2004).
Murphy, J. I., Weaver, N. E. & Hendricks, A. E. Accessible analysis of longitudinal data with linear mixed effects models. Dis. Model Mech. 15 (5). https://journals.biologists.com/dmm/article-abstract/15/5/dmm048025/275308 (2022).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R Stat. Soc. Ser. B Stat. Methodol. 57 (1), 289–300 (1995).
Cummings, J. et al. Exploring the relationship between patient-relevant outcomes and Alzheimer’s disease progression assessed using the clinical dementia rating scale: a systematic literature review. Front. Neurol. 14, 1208802 (2023).
Razani, J. et al. Relationship between executive functioning and activities of daily living in patients with relatively mild dementia. Appl. Neuropsychol. 14 (3), 208–214 (2007).
Jekel, K. et al. Mild cognitive impairment and deficits in instrumental activities of daily living: a systematic review. Alzheimers Res. Ther. 7 (1), 17 (2015).
Marshall, G. A., Amariglio, R. E., Sperling, R. A. & Rentz, D. M. Activities of daily living: where do they fit in the diagnosis of Alzheimer’s disease? Neurodegener. Dis. Manag. 2 (5), 483–491 (2012).
Acknowledgements
We would like to express our gratitude to all the patients and their families who participated in this study for their invaluable contributions. We also acknowledge the dedicated medical professionals and staff at the Department of Psychiatry, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, for their assistance with data collection. Special thanks to the research assistants who supported the study logistics and to the neuropsychologists who performed the evaluations.
Author information
Authors and Affiliations
Contributions
H.L., J.L., S.S., G.N., and S.K. conceptualized and designed the study. H.L., S.S., G.N., Y.J., and E.H. conducted the investigation. H.L., S.O., and J.L. developed the methodology. H.L. and Y.J. performed the data analysis. H.L. wrote the original draft. S.Y. and J.L. reviewed and edited the manuscript. J.L. supervised the project. H.L. had full access to all the data in the study and verified the underlying data. All authors reviewed and approved the final manuscript, had full access to the study data, and take full responsibility for the integrity of the data and the decision to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) of Seoul National University Boramae Medical Center (Approval Number: 10-2020-295). The requirement for informed consent was waived due to the retrospective nature of the study, as all data were anonymized and de-identified prior to analysis. The study adhered to the principles of the Helsinki Declaration.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, H., Shin, S., Nam, G. et al. Longitudinal trajectories of cognitive, functional, and neuropsychiatric decline in Alzheimer’s disease during COVID-19 lockdown in South Korea. Sci Rep 15, 8081 (2025). https://doi.org/10.1038/s41598-025-92497-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92497-5