Abstract
MicroRNAs (miRNAs) are a class of non-coding RNAs involved in a variety of pathophysiological processes. We have previously reported that the abnormally high expression of miR-99a is associated with drug resistance and poor prognosis in acute myeloid leukemia. However, the impact of miR-99a on normal hematopoiesis is not well understood. To investigate the effect of aberrant miR-99a overexpression on hematopoietic stem and progenitor cells (HSPCs), we overexpressed miR-99a in human umbilical cord blood CD34+ cells. We observed that miR-99a overexpression increased the proliferation, self-renewal capacity, and transplantation efficiency of HSPCs with or without a clonal hematopoiesis-associated mutation (JAK2V617F). Meanwhile, we found that overexpression of miR-99a blocked the maturation and differentiation of granulocytes/monocytes and erythrocytes. We then identified NIPBL as a direct target of miR-99a. NIPBL knockdown in HSPCs showed a phenotype similar to miR-99a overexpression. In this study, we elucidate that abnormally high expression of miR-99a can enhance the proliferative capacity of HSPCs but inhibit myeloid differentiation and maturation. Taken together, our work has uncovered important roles for miR-99a in regulating HSPCs by enhancing the proliferation and self-renewal capacity of HSPCs but inhibiting differentiation, which play important roles in leukemic transformation.
Similar content being viewed by others
Introduction
Hematopoietic stem cells (HSCs) are the fundamental source of sustained production of all blood cell lineages1. The capacities for self-renewal and differentiation are the biological properties of HSCs in maintaining homeostasis of the hematopoietic system2. In the context of malignant transformation, normal hematopoietic regulation is disturbed, enhanced expansion and differentiation disorders of hematopoietic stem and progenitor cells (HSPCs) eventually leading to the failure of terminal differentiation to functional cell types in peripheral blood.
In hematopoiesis, miRNAs were identified and found to control the fate of hematopoietic cells3,4. The expression of miR-125, let-7e, and miR-99b are significantly higher in HSCs compared with differentiated progenitor cells, which may maintain the HSC self-renewal5,6,7. On the other hand, miR-126, miR-212/132 complex, and miR-193b exhibit inhibitory effects on HSC function8,9. MiRNA expression profiles are closely correlated to the risk categories, prognosis, and the leukemia transformation3, such as the co-overexpression of miR-125 and miR-29a inducing the development of myeloid leukemia10,11. Single miRNAs can also enhance the self-renewal ability of leukemic stem cells (LSCs), such as miR-126, miR-196, miR-21, and multi-cistron gene cluster miR-17-9212. Antagonizing the expression of miR-196 and miR-21 may inhibit LSCs in a human MLL rearrangement leukemia model13. MiR-22, as a cancer-promoting miRNA, promotes proliferation, survival, self-renewal, and differentiation inhibition, induced transformation of HSCs, and the occurrence of myeloid tumors by targeting TET214. The above evidence indicates the important regulatory roles of miRNAs in normal hematopoietic stem cells and leukemic cells.
MiR-99a is a member of the miR-125b/miR-99a/let-7c gene cluster. We previously reported that the abnormally high expression of miR-99a in LSCs was associated with poor prognosis of acute myeloid leukemia (AML) and promotes cell expansion and resistance15. O’Connell et al. observed elevated levels of miR-99a expression in murine bone marrow hematopoietic stem cells relative to more differentiated cells11. The significantly higher expression of miR-99a in LSC compared to that in normal HSPCs, points to the importance of further investigating the role of miR-99a in governing HSC stemness and the malignant transformation. Our study showed that abnormally high expression of miR-99a promoted the expansion of HSPCs derived from cord blood and inhibited the terminal differentiation of granulocytes/monocytes and erythrocytes. Overexpression of miR-99a in mouse c-Kit+ cells with clonal hematopoiesis-related mutation provided a growth advantage for malignant clones. Therefore, overexpression of miR-99a dysregulated the biological function of HSPCs, which may be involved in the hematopoietic leukemia transformation.
Methods
Human samples and cell lines
The human leukemic cell lines K562, HL60, and NB4 were obtained from ATCC. All these cell lines were cultured in RPMI 1640 (Gibco, Carlsbad, USA) supplemented with 10% fetal bovine serum (FBS, Gibco) and 1% penicillin/streptomycin (Beyotime, Shanghai, China). HL60 and NB4 were cultured in the complete RPMI 1640 media containing 1 µM all-trans retinoic acid (ATRA) for induction of differentiation. K562 induced by 30 µM hemin and 1 µM Ara-C were cultured in IMDM supplemented with 20% FBS and 1% penicillin/streptomycin for 48 h.
HSPCs from human cord blood (CB) samples were acquired from healthy full-term newborns at Tianjin Obstetric Central Hospital (Tianjin, China) after obtaining informed consent. This study was approved by the Ethics Committee of the Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Sciences, according to the guidelines of the 1975 Declaration of Helsinki. All methods were performed in accordance with relevant local guidelines and regulations.
Vector construction
The lentiviral vectors carrying miR-99a or scramble sequence (Ctrl) were purchased from GeneCopoeia (Rockville, USA), and reconstructed with the SFFV promoter (Synbio Tech, Suzhou, China). HSPCs were transduced at a multiplicity of infection (MOI) of 30. EGFP+ CD34+ positive cells were sorted by flow cytometry.
The shRNA vectors used to target NIPBL were purchased from GeneCopoeia, Inc.
The shRNA sequences used to knock down NIPBL are as follows: shNIPBL#1, 5′-GGATGGAGAACCTATGTATATTCAAGAGATATACATAGGTTCTCCATC-3′;
shNIPBL#2, 5′- GGATGACAATTTGGTTTCACTCAAGAGGTGAAACCAAATTGTCATCC − 3′.
Colony-forming cell assay
CB HSPCs were enriched using CD34 magnetic beads (130–046–702; Miltenyi Biotec) and transduced with lentiviral vectors carrying hsa-miR-99a or scrambled control (Ctrl). Cells were maintained in StemSpan serum-free expansion media (SFEM, STEMCELL Technologies) supplemented with TPO (20ng/ml), Flt3L (100ng/ml), and SCF (100ng/ml) (Peprotech) for 48–72 h after transduction. GFP+ CD34+ cells were sorted and then plated into H4434 media (STEMCELL Technologies) containing SCF, IL-3, EPO, and GM-CSF (500 cells/well). The colonies were counted after 12-14d in culture. Cells were resuspended in PBS containing 2 mM EDTA and 2% FBS, and analyzed by flow cytometry.
For mouse colony-forming cell assay, c-Kit+ cells of JAK2V617F transgenic mice16 or WT mice were enriched using magnetic beads (130-091-224, Miltenyi Biotec) and then transduced with lentiviral vectors carrying mmu-miR-99a or Ctrl. After culturing in SFEM for 48–72h, GFP+ c-Kit+ cells were sorted and then plated into M3434 media (STEMCELL Technologies) containing SCF, IL-3, EPO and IL-6 (1000 cells/well). After incubation at 37 °C for 12–14 days, the number of colonies was counted. Cells were resuspended in PBE buffer (PBS with 0.5% BSA and 2 mM EDTA) and then we analyzed the expression of cell surface markers.
For colony replating assays, colonies were counted after 7 days of culture in the colony-forming assay, and collected GFP+ cells were used for replating assays (20,000/well). After scoring the colonies, all cells were resuspended in IMDM + 2% FBS and replated in M3434. Colonies were counted and replated 7 days afterward.
Long-term culture-initiating cells (LTC-IC) assay and limiting-dilution assay
For LTC-IC assays, CD34+ cells (EGFP+ CD34+ cells) transduced with Ctrl or mir-99a vector were incubated in SFEM for 2 days. Then, cells were resuspended in α-MEM medium (STEMCELL Technologies) supplemented with 12.5% FBS, 12.5% Horse serum, 2 mM L-glutamine, 57.2 µM β-mercaptoethanol and 10− 6 M hydrocortisone at a concentration of 10,000/ml, then overlaid on a preestablished, irradiated (MS-5) stromal cell layer17. For limiting-dilution assay, serially diluted EGFP+ CD34+ cells (3450 down to 35 cells/well by 1:2.5 dilutions) were plated into 96 well plates, respectively. Cultures were maintained for 5 weeks with weekly half-medium changes. The well was scored positive or negative for the presence of at least one cobblestone area. The estimated stem cell frequency was calculated by linear regression analysis and Poisson statistics using extreme limiting dilution analysis software18.
To measure the input of LTC-IC number, cells were then harvested and counted, and CFC assays were performed to obtain LTC-IC–derived CFC colonies as previously described19.
Mice and transplantations
Human CD34+ cells were sorted and transduced with miR-99a or Ctrl vector. The cells were kept in SFEM with 100 ng/ ml SCF, 100 ng/ ml Flt3, and 50 ng/ml TPO. Forty-eight hours after transduction, transplantations were performed by the injection of 10µL of the sorted GFP+CD34+ cells into the tibial medullary cavity of sub-lethally irradiated (200 cGy) NOD/SCID/gamma (NOG) mice (20,000 GFP+CD34+ cells per mouse). Mice were sacrificed for analysis 12 to 16 weeks after transplantation to evaluate hematopoietic reconstitution. Mice were euthanized at indicated time points by cervical dislocation. NOG mice used in this study were supplied by Vitalriver Experimental Animal Technical Co. (Beijing, China). JAK2V617F transgenic mice were generated as previously described 16. All animal experiments were approved by the Animal Research Committee of the Institute of Hematology and Blood Diseases Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College.
Bioinformatic analyses
Total RNA was extracted from transduced human CB CD34+ cells by TRIzol reagent and purified using RNeasy Mini Kit (Qiagen, Germany) including the DNase digestion step. RNA integrity was assessed with a Bioanalyzer, and library preparation was performed using the Illumina TruSeq Stranded mRNA Library Prep Kit. Paired-end reads (150 bp) were generated and sequenced on the Illumina NovaSeq 6000 platform, with a sequencing depth of at least 20 million reads per sample. The RNA-seq data were aligned to the GRCh38 human genome reference using the STAR aligner. Gene expression levels were quantified from the mapped reads using HTSeq. The edgeR package was used for batch correction, normalization, and differential gene expression analysis. To find genes that are differentially expressed in multiple conditions, we used a relaxed threshold to identify differentially expressed genes (P < 0.05).
Dual-luciferase reporter assay
The coding region of NIPBL containing the predicted binding sites with miR-99a was cloned into the pmir-GLO dual-luciferase vector (Promega, Madison, WI, USA). The binding sequence of NIPBL was then mutated to 5’-AGCCGT-3’. The vectors were transfected into leukemia cell lines (K562, THP1 and HL60) with miR-99a or Ctrl vector overexpression. The transfected cells were lysed 48 h after transfection, and luciferase activity was then evaluated with a Dual-Luciferase Reporter System by measuring firefly and Renilla luciferase activities according to the manufacturer’s instructions (Promega, Madison, WI, USA).
Reverse transcription quantitative PCR
Quantitative reverse transcription PCR (qRT-PCR) was performed using SYBR Green Master Mix (Roche) and Applied Biosystems 7900HT Real-Time PCR System. GAPDH and β-actin were amplified as housekeeping genes. Relative expression was calculated using the 2−ΔΔCT method. Primers used for qPCR are listed in Supplementary Table 1.
Cell proliferation and cell cycle analysis
Cell proliferation was evaluated by MTT assay and flow cytometry. Cell cycle analysis was performed with the Bromodeoxyuridine (BrdU) Cell Proliferation Assay Kit (BD Biosciences) according to the manufacturer’s protocol.
Statistical analyses
Statistical analyses were performed using GraphPad Prism 7.0. An unpaired t-test or Mann-Whitney U test was applied for two-group comparisons, and ANOVA analysis was applied to determine differences among three or more groups. P < 0.05 was considered statistically significant.
Ethics statement
Ethical approval for this project was obtained from the Ethics Committee of Blood Diseases Hospital, Chinese Academy of Medical Sciences (KT2020016-EC-2). All methods were carried out in accordance with relevant guidelines and regulations. This study is reported in accordance with ARRIVE guidelines (https://arriveguidelines.org).
Results
Overexpression of miR-99a accelerated human HSPC proliferation
We previously observed that the expression level of miR-99a is significantly upregulated in enriched leukemia stem cells from primary samples compared to normal HSPCs. Flow cytometry analysis showed the expression level of miR-99a in normal human HSPCs is higher than that in the differentiated lineages (Fig. 1A). To investigate whether the upregulation of miR-99a leads to impaired functional potential in HSPCs, human cord blood CD34+ cells were transduced with lentiviral vectors carrying the hsa-miR-99a and green fluorescent protein (GFP) or with a scrambled vector used as control (Fig. 1B and Fig. S1A). The growth of cells with miR-99a overexpression (miR-99a group) was significantly accelerated than that of the control cells (Fig. 1C). Cell cycle analysis showed that the proportion of miR-99a group cells in the S phase was between 15 and 20%, while less than 10% in control cells (Fig. 1D). Cell proliferation assay showed that the miR-99a group divided faster compared with the control group. The proliferation index of cells with miR-99a overexpression, estimated based on the average number of divisions, was significantly higher than that of control cells (Fig. 1E-F). In addition, fewer apoptotic cells were observed in CD34+ miR-99a group (Fig. 1G). These results indicate that overexpression of miR-99a leads to significantly increased proliferation of human HSPCs.
Overexpression of miR-99a accelerated the proliferation of human HSPCs. (A) The miR-99a expression levels in subpopulations of peripheral blood. Error bars represent the standard deviation resulting from quadruplicate measurements. (B) Flow chart of miR99a overexpression by lentivirus vector in cord blood (CB) CD34+ cells. (C,D) Growth curves (C) and Cell cycle analysis (D) of control and miR-99a overexpression CB CD34+ cells maintained in StemSpan SFEM with SCF (100ng/ml), Flt3L (100ng/ml), TPO (50ng/ml). Data represent mean ± SEM (student’s t-test; n = 3) and are representative of three independent experiments. (E,F) CB CD34+ cells were transduced with miR-99a or Ctrl vectors. The proliferation indexes (E) and the analysis of the proportions (F) of different generations of CB CD34+ cells were determined by CellTrace Violet staining. Cells were harvested at 12 h, 24 h, 48 h, 72 h, 96 h after dye labeling and analyzed by flow cytometry. G. The effect of miR-99a overexpression on cell apoptosis. Data represent three independent experiments and each carried out with three replicates. * P < 0.05, ** P < 0.01, *** P < 0.001.
Overexpression of miR-99a enhanced self-renewal of human HSPCs in vitro
In addition to proliferation, self-renewal is a fundamental characteristic of HSPCs. We further investigated the role of miR-99a overexpression in HSPC self-renewal in vitro. The frequency of long-term culture initiating cell (LTC-IC) was evaluated by limiting dilution cobblestone area-forming cells (CAFC) assays with sorted CD34+ GFP+ cells, found that the frequency of LTC-ICs in the miR-99a group and Ctrl group were 1:483 and 1:943, respectively (Fig. 2A). To quantify LTC-IC, the CAFC assay was performed by coculturing equal numbers of miR-99a group or control CD34+ cells with feeder layers for 5 weeks. The size and number of cobblestone areas were significantly increased in the miR-99a group compared to the Ctrl group (Fig. 2B, Fig. S2A). The GFP+ cells from the CAFC were then collected for another 14-day colony forming unit-cell (CFU-C) assay. In addition, these results confirmed that the number of LTC-IC with self-renewal potential was higher in the miR-99a group than in the Ctrl (Fig. 2C).
To characterize the in vitro self-renewal capacity of CD34+ cells after miR-99a overexpression, a colony-replating assay was performed. We observed that the total number of colonies in the first plating was similar between the two groups. However, miR-99a group exhibited increased colony-forming capacity compared to control CD34+ cells in the subsequent round of replating (Fig. 2D).
Overexpression of miR-99a enhanced the self-renewal ability of human HSPCs. (A) Limiting dilution CAFC assays was performed in CD34+ cells transduced with miR-99a overexpression and Ctrl vectors. The frequency of each group to form CAFC was determined by limiting dilution 5 weeks after seeding on MS5 stroma. The representative results of two independent experiments are shown. (B) CAFC numbers were counted according to the different sizes of clones. The black bar represents the number of small clones (5–50 cells per clone), the grey bar represents the number of medium-sized clones (50–100 cells per clone), and the white bar represents the number of large clones (> 100 cells). (C) Bar plot shows the total number of colonies formed in each group after 14 days of cultivation in a semi-solid medium, with the cells sorted CAFCs in the miR-99a overexpression group and the control group after the 5th week. (D) Number of colony forming units (CFU) counted at day 7 per 1,000 CD34+ cells plated in methocult medium after first plating, or after replating 20,000 cells washed out from first plating (2nd plating), or from second plating (3rd plating). Three biological replicates and technical replicates were used for each experiment. Student’s t test, * P < 0.05, ** P < 0.01, *** P < 0.001.
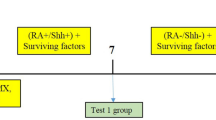
Overexpression of miR-99a promoted the growth advantage of malignant HSPCs in vitro
It is now known that normal hematopoietic stem cells acquire certain somatic mutations as a part of the aging process, a phenomenon referred to as clonal hematopoiesis of indeterminate potential (CHIP). To understand the impact of miR-99a overexpression on clones with CHIP mutations and the initiation of hematopoietic malignancies, bone marrow c-Kit+ cells were enriched from JAK2V617F (a common CHIP mutation) mice and their littermate control, and they were transduced with miR-99a or the control virus. GFP+ c-Kit+ cells were then sorted for replating assay (Fig. 3A). Notably, a comparison of the second and third rounds of replating revealed that miR-99a overexpress c-Kit+ cells produced a higher number of colonies than the control group (Fig. 3B). In addition, flow cytometry analysis showed that the proportion of c-Kit+ cells in the miR-99a overexpression colonies after the first plating was significantly increased, compared to that in the control group (Fig. 3C). These results indicate that overexpression of miR-99a can promote the clonality of c-Kit+ cells from JAK2V617F transgenic mice, demonstrating that miR-99a can provide a growth advantage in the process of clonal hematopoiesis.
Overexpression of miR-99a conferred a growth advantage of malignant mouse HSPCs. (A) Flow chart of overexpression of miR-99a in c-Kit+ cells of JAK2V617F transgenic mice. (B) The number of CFU counted on day 7 per 1,000 CD117+ cells from miR-99a overexpression or Ctrl group, plated in methocult medium after first plating, or after replating 5,000 cells washed out from the first plating or the second plating. GM: granulocyte-macrophage; E: erythroid; GEMM: granulocyte-erythrocyte-macrophage-monocyte. The results shown are representative of one of the two independent experiments. t-test, * P < 0.05, ** P < 0.01, *** P < 0.001. (C) The proportion of CD117+ cells from HSPCs overexpressing miR-99a or Ctrl vector. MiR-99a was overexpressed in c-Kit+ cells of JAK2V617F transgenic mice, followed by CFC assays. Cells were collected on the 7th day, and the proportion of CD117+ HSPCs was analyzed by flow cytometry. Each experiment has three biology replicates with similar result.
Overexpression of miR-99a impairs myeloid maturation and erythroid lineage development
Our analysis of normal human peripheral blood subpopulations revealed that the highest expression level of miR-99a was found in CD34+ HSPCs. (Fig. 1A). Therefore, to evaluate the impact of miR-99a on the differentiation of HSPCs, we performed the CFC assay and flow cytometry analysis. The results showed that the numbers of CFU-GEMM and CFU-GM colonies significantly increased, while the CFU-E count decreased in the miR-99a group compared with control cells. (Fig. 4A). Interestingly, subsequent flow cytometry analysis of the collected CFU colonies revealed that the proportion of myeloid cells with the maturation markers (CD13+ CD11b+) in the miR-99a group was significantly reduced, indicating a blocked cellular differentiation in granulocytic/monocytic lineages (Fig. 4B).
We cultured umbilical cord blood CD34+ cells that overexpress miR-99a in erythroid differentiation liquid medium and detected the dynamic changes in the surface marker CD235a and CD71 of erythroid cells to assess the impact of miR-99a overexpression on the erythroid differentiation of HSPCs. The results showed that on the 8th day of differentiation, the proportion of CD235ahigh CD71+ cells in the miR-99a group was 21%, compared to 31.9% in the Ctrl group. Moreover, the percentage of cells in the early stage of erythroid differentiation (CD235a- CD71+) in the miR-99a group was higher than in the Ctrl group. Similar results were observed on day 15, indicating that overexpression of miR-99a slowed down the process of erythroid differentiation (Fig. 4C). On day 21, Hoechst 33342 was applied to observe the enucleation of red blood cells. Consistent with the delayed erythroid differentiation, the proportion of enucleated erythrocytes (Hoechst 33342- CD235a+) was markedly decreased in the miR-99a group (Fig. 4D), suggesting that both early-stage erythropoiesis and terminal differentiation were affected by the overexpression of miR-99a. Furthermore, we conducted Wright Giemsa–stained cytospins on the liquid-cultured cells to assess cell morphology and determine the stage of differentiation. The results showed that most of the cells in the miR-99a group were in a more primitive state than those in the Ctrl group (Fig. 4E).
We evaluated the effect of miR-99a overexpression on retinoic acid (ATRA) induced differentiation in the acute promyelocytic leukemia cell lines NB4 and HL6020,21,22. The results showed that after 48 h of ATRA treatment, the percentages of CD11b positive cells were 9.58% in NB4-miR-99a and 23.4% in HL-60-miR99a, and compared to 28.8% and 32.5% in their parental cells, respectively (Fig. S3A). Similarly, hemin, an inducer of heme oxygenase (HO)-1, was used to induce the erythroid differentiation of K56223. The proportion of CD235a+ CD71+ cells in the miR-99a group was 67.4% after hemin treatment, while that in the Ctrl group was 86.5% (Fig. S3B). Hemoglobin staining with benzidine further confirmed that cells in the miR-99a group showed a significant reduction in benzidine-positive cells compared to the control group (Fig. S3C). These results indicate that overexpression of miR-99a also inhibits the induced differentiation of myeloid leukemia cells.
MiR-99 functionally suppresses both myeloid and erythroid differentiation of HSPCs. (A) Bar plot of colony numbers from 500 CD34+ cells per well in colony forming assay. Human CB CD34+ cells were transduced with miR-99a or control vector and sorted by flow cytometry 48 h after infection; then, cultured with semisolid matrix H4434 for two weeks. BFU-E: burst-forming unit-erythroid; GM: granulocyte-macrophage; GEMM: granulocyte-erythrocyte-macrophage-monocyte. The data are shown as the mean ± SEM of five biologically independent experiments. (B,C) Representative results of flow cytometric analysis of CD13/CD11b and CD235a after colony forming units (CFU) culture and the percentages of each group. (D) Cord blood CD34+ cells overexpressed with miR-99a were cultured in erythroid differentiation liquid medium. On the 21st day of culture, cells were collected and labeled with CD235a and Hoechst 33342. Flow cytometry was used to analyze the enucleation status during the final stage of erythroid differentiation. (E) Cytospins were stained with Wright-Giemsa of cells after CFU culture. (red arrow, indicate immature erythrocytes; blue arrow, indicate immature granulocytes; scale bars: 10 μm) *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001; ns, P > 0.05, unpaired t-test. Three biological replicates and technical replicates were used for each experiment.
Effect of miR-99a overexpression on the transplantation of cord blood CD34+ cells in vivo
To verify the effect of abnormally high expression of miR-99a on the maintenance and differentiation of HSPCs in vivo, CD34+ cells were transduced with lentivirus carrying miR-99a or Ctrl vector and transplanted into NOG mice (Fig. 5A). Peripheral blood and bone marrow cells were collected at 16 weeks post-transplantation to assess the reconstitution of human CD34+ HSPCs by flow cytometry analysis. The results revealed that the proportion of human CD34+ cells in the peripheral blood of the miR-99a group was about 2.6%, whereas it was only 1% in the Ctrl group (Fig. 5B). In the bone marrow, the proportion of human CD34+ cells in the miR-99a group reached as high as 17%, while that in the Ctrl group was 9% (Fig. 5C). These results demonstrated that overexpression of miR-99a significantly improved the engraftment ability of CD34+ cells in vivo.
Effect of overexpression of miR-99a on the transplantation of cord blood CD34+cells in vivo. (A) Flow chart of HSPCs xenotransplanted experiments in NOG mice. (B,C) Flow cytometry analysis of human HSPCs (hCD45+ CD34+) implantation in peripheral blood (PB) and bone marrow (BM) of NOG mice at 11 weeks after transplantation. *P < 0.05, ** P < 0.01, ***P < 0.001. The experiments were performed at least three times (experimental replicates) and each experimental replicate contained four to five biological replicates.
Effect of miR-99a overexpression on the transcriptional profile of cord blood CD34+ cells
To gain further insight into the underlying mechanisms of miR-99a-mediated effects on HSPC functions, we conducted transcriptome sequencing on human CD34+ HSPCs transduced with either miR-99a or control vectors. We identified 547 differentially expressed genes (DEGs) between the Ctrl and miR-99a groups, with 238 genes upregulated and 309 genes downregulated (|log2FC| ≥ 1, p < 0.05). Heat map of these results were shown (Fig. 6A). Gene set enrichment analysis (GSEA) of RNA-Seq data revealed that genesets related to HSCs and hematopoietic differentiation, as well as genes associated with E2F targets and WNT signaling, were upregulated in miR-99a group (Fig. 6B). Additionally, gene sets associated with both long-term and short-term HSCs, DNA replication, AML, MYC targets, and KRAS were significantly enriched in the miR-99a overexpression group (Fig. S4A). Using the R software package DOSE, we queried the Disease Ontology database for human information related to these DEGs. Remarkably, 7 out of the top 10 diseases associated with miR-99a were malignancies, including bone marrow cancer and myeloma (Fig. 6C). Further enrichment analyses were performed to elucidate the potential biological functions of miR-99a. The top 10 gene ontology (GO) enrichment items are shown (Fig. 6D). The most significantly enriched GO terms among the DEGs included negative regulation of immune system process, cell cycle arrest, protein-DNA complex organization, chromatin assembly or disassembly, negative regulation of hemopoiesis, cellular response to unfolded protein, mitotic cell cycle checkpoint, cell proliferation, chemokine receptor binding, chemokine activity.
Overexpression of miR-99a leads to changes in the expression profile of CB CD34+ genes. Human CB CD34+ cells were transduced with miR-99a or control vector and sorted by flow cytometry 48 h after infection to conduct bioinformatics analysis. (A) Heatmap of miR-99a related differentially expressed genes (DEGs). (B) Gene set enrichment analysis (GSEA) of miR-99a related DEGs. (C) DEGs enrichment analysis in Disease Ontology Database. (D) Differential gene GO analysis reveals GO functional gene set.
MiR-99a enhanced self-renewal ability and inhibited differentiation of HSPCs by targeting NIPBL
To better determine the key targets of miR-99a that regulate hematopoiesis, we performed an integrated analysis of three gene sets: (1) downregulated DEGs from RNA sequencing, (2) genes associated with stem cell maintenance and hematopoietic differentiation in HSPCs, and (3) predicted miR-99a target genes from miRTarBase, TargetScan, and miRanda database24,25 (Fig. S5A). Heat map of potential target genes among the 63 overlapping genes was shown. Expression of transcription factors critical for HSCs and myeloid differentiation were downregulated, such as NIPBL, HOXA1, SPI1, GATA1, RUNX1A, MPO, and GFI. In addition, expression of MYB was upregulated, which promotes the proliferation of hematopoietic stem cells (Fig. 7A). These results were confirmed by qPCR analysis (Fig. 7B).
Through analysis of potential target genes and further literature review, we preliminarily identified NIPBL as a potential target gene for miR-99a overexpression in hematopoietic cells. Therefore, we performed the luciferase reporter assay to investigate whether NIPBL is a direct target of miR99a. Reporter vectors carrying either the wild-type fragment with the putative NIPBL-miR99a binding sites or a fragment with mutated sequences were transiently transfected into K562 and THP1 cells overexpressing either the miR99a or the control vector. The results showed that cells overexpressing miR-99a exhibited significantly decreased luciferase activity when transfected with vectors carrying the wild-type NIPBL mRNA sequence, which confirmed NIPBL is a direct target of miR99a (Fig. 7C).
We then utilized shRNA to interfere with the expression of NIPBL in HSPCs to determine whether the knockdown of NIPBL would exhibit a phenotype similar to that observed with miR-99a overexpression. The knockdown efficiency detected by qPCR was approximately 40% for shNIPBL#2 and up to 70% for shNIPBL#1 in both cell lines (Fig. 7D). CB CD34+ cells were transduced with lentivirus carrying the empty vector (EV) or shNIPBL (#1 and #2), and cells were sorted 48 h after the secondary infection. After a liquid culture to induce cell differentiation for 7 days, we observed that the proportion of CD34+ cells was significantly higher in the shNIPBL group compared with the control (Fig. 7E). Furthermore, the proportion of CD11b+ cells and CD235a+ cells in the shNIPBL group was significantly lower than that in the Ctrl group (Fig. 7F-G). These results suggest that abnormally high expression of miR-99a inhibited the maturation and differentiation of hematopoietic cells by targeting NIPBL.
NIPBL mediates miR-99a function in hematopoietic stem/progenitor cells. (A) Heatmap depicting the expression levels of hematopoietic stem cell-related genes in control (Ctrl) and miR-99a overexpression groups. The color gradient indicates differential gene expression, highlighting the impact of miR-99a overexpression on hematopoietic gene regulation. (B) Quantitative PCR (qPCR) analysis of potential targeted hematopoietic regulatory transcription factor expression in umbilical cord blood-derived CD34+ cells overexpressing miR-99a. Statistical significance was assessed using the t-test, with * indicating P < 0.05, ** indicating P < 0.01, and *** indicating P < 0.001. (C) Dual-luciferase Reporter Assay for luciferase assays in THP1 and K562 cell lines. The luciferase activity was measured 3 days after transfection. (D) Knockdown efficiency of NIPBL was measured by qPCR analysis on HSPCs lentivirally transduced with control vectors or NIPBL targeting shRNA. (E) Growth curve for HSPCs as a function of time after transduction. Data represent mean count ± SEM (Student’s t test; n = 3) and are representative of three independent experiments. (F,G) Human CB CD34+ cells were transduced with empty vector or shNIPBL vector and sorted by flow cytometry 48 h after infection; then, cells were placed in liquid culture for two weeks. Representative results of flow cytometric analysis of CD13/CD11b and CD235a after liquid culture and the percentages of each group are shown (right, **P < 0.01, ***P < 0.001, unpaired t-test). Data represent three independent experiments and each carried out with three replicates.
Discussion
Under physiological conditions, the self-renewal and differentiation capabilities of hematopoietic cells are tightly regulated by a complex signaling network to maintain homeostasis. As integral post-transcriptional regulators in this network, dysregulated miRNAs can lead to abnormal proliferation and differentiation of hematopoietic cells, potentially resulting in malignant transformation and leukemia. It is generally believed that leukemias are cancers of the blood that originate from the hematopoietic stem/ progenitor cells as a result of the accumulation of genetic mutations that lead to cell transformation26,27,28,29,30. Currently, a large amount of research evidence suggests that in addition to genetic mutations, epigenetic changes, including DNA methylation, histone modification, and the expression imbalance of non-coding RNA, are closely associated with LSCs and contribute significantly to the initiation and progression of leukemia. MiRNAs play an important role in the regulation of hematopoietic development and differentiation, as well as the occurrence and progression of leukemia31,32,33. Our previous work demonstrated that miR-99a overexpression in AML patients leads to an increase in CD34+ cells, which correlates with leukemia-initiating clone formation in vitro and is clinically associated with chemotherapy resistance15. This suggests indicated that the increase of miR-99a in AML CD34+ cells may play a clinically significant role, particularly in leukemia progression and therapeutic resistance. Furthermore, our studies have shown that miR-99a expression is elevated in LSCs compared to normal HSCs, with miR-99a levels being high in HSCs and gradually decreasing during differentiation15. A key study has also provided important insights into miR-99a’s role in HSC expansion and megakaryopoiesis, further highlighting its potential implications in hematopoietic malignancies34. However, despite these findings, it remains unclear whether aberrantly increased miR-99a expression in HSPCs disrupts normal hematopoietic function and contributes to leukemic transformation.
In this study, we utilized lentiviral vectors to overexpress miR-99a in human and murine HSPCs, and demonstrated that miR-99a overexpression enhanced HSPC proliferation and clonogenicity while inhibiting differentiation. Additionally, we showed that miR-99a overexpression promotes the self-renewal capacity of CD34+ cord blood cells. Both continuous colony formation assay and long-term culture initiating cell assay revealed that miR-99a overexpression preserves the clonogenic potential of normal HSPCs. Furthermore, we demonstrated that upregulated of miR-99a robustly inhibited the terminal differentiation of granulocyte/monocyte and erythroid lineages in both normal HSPCs and leukemia cell lines. In the acute promyelocytic leukemia (APL) cell lines NB4 and HL60, despite the varying degrees of suppression, presumably due to their distinct genetic background, the overall tendency consistently manifested as myeloid differentiation inhibition. These alterations, in conjunction with the observed accelerated cellular proliferation, represent pivotal biological modifications intricately linked to the progression of neoplasms.
Due to the ability of individual miRNAs to target multiple downstream genes and pathways, the mechanisms underlying miRNA-mediated regulation of cell biology are highly complex. To identify the target genes and mechanisms through which miR-99a regulates hematopoiesis, we performed RNA sequencing on CD34+ cord blood cells overexpressing miR-99a. The transcriptional changes observed in HSPCs included the downregulation of lineage-specific factors (e.g., GATA1, MPO) and stem cell-associated factors (e.g., HOXA1, RUNX1A), alongside the upregulation of MYB. These findings suggest that miR-99a may modulate a core transcription factor network that simultaneously regulates both stem cell maintenance and differentiation. The upregulation of MYB could represent a compensatory mechanism to sustain proliferative potential or an alternative pathway to preserve an undifferentiated state.
To identify miR-99a target genes and mechanisms involved in hematopoietic regulation, we combined miRNA target prediction algorithms and literature mining to preliminarily identify NIPBL as a potential miR-99a target mediating effects in hematopoietic cells. NIPBL knockdown in CD34+ cord blood cells inhibited granulocytic differentiation, phenocopying miR-99a overexpression, indicating aberrantly high expression of miR-99a potentially inhibiting NIPBL expression and partially impairing differentiation.
NIPBL is a cohesin loading factor that plays an important role in hematopoietic differentiation and cell cycle regulation. Haploinsufficiency of NIPBL is known to be associated with Cornelia de Lange syndrome35,36. NIPBL has been found to be recurrently mutated in hematologic and solid malignancies25,37. Previous studies have shown that NIPBL plays a critical role in NIPBL-HOXB9-driven leukemogenesis, mediated in part by its interaction with Mau2, the component of the cohesin complex that recruits NIPBL to the genome38. Recent results have shown that loss-of-function mutations in NIPBL lead to dysregulation of myeloid cell differentiation, characterized by an increase in the number of myeloid progenitors and a decrease in mature myeloid cells39. NIPBL positively regulates RUNX1 transcription. The link between NIPBL dysregulation and RUNX1-driven hematopoietic defects may explain hematopoietic defects resulting in increased myeloid precursors and reduced circulating mature erythroid and myeloid cells, which might contribute to the occurrence of hematological malignancies40. Notably, NIPBL regulates the expression of the c-Myc gene, a key regulator of cell proliferation, in humans, mice, Drosophila, and zebrafish41,42. In addition to NIPBL, another target of miR-99a, HOXA1, has been shown to influence the maintenance and differentiation of HSPCs in mice, further highlighting the broad impact of miR-99a on hematopoietic regulation43.
In our study, overexpression of miR-99a alone was insufficient to induce leukemic transformation in normal HSPCs, prompting us to investigate its role in the pre-leukemic state. The currently accepted model for the origin of LSCs suggests that HSCs harboring pre-leukemic (first-hit) mutations, referred to as pre-LSCs, acquire the potential for malignant clonal expansion upon subsequent mutations (multiple “hits”) and the loss of multilineage differentiation ability (differentiation block), ultimately giving rise to LSCs or leukemic cells44,45. Clinically, JAK2V617F mutations are frequently observed in patients with myeloproliferative neoplasms (MPNs), which can mimic a pre-leukemic state with the potential to progress to acute leukemia. To explore the role of miR-99a in this context, we utilized JAK2V617F transgenic mice as a model of the first-hit mutation and overexpressed miR-99a in this background. Our study demonstrates that miR-99a overexpression promotes the clonal growth advantage of malignant MPN clones. Further studies are needed to explore the relationship between miR-99a and other first-hit mutations.
Furthermore, our study underscores the critical role of the miR-99a/NIPBL axis in promoting HSPC proliferation and expansion under various hematologic conditions, including JAK2V617F clonal hematopoiesis and ATRA-treated acute promyelocytic leukemia. Targeting miR-99a or NIPBL may offer a novel therapeutic approach for hematologic malignancies, potentially overcoming treatment resistance and improving clinical outcomes. These findings suggest that combining miR-99a/NIPBL modulation with existing therapies, such as ATRA and JAK2 inhibitors, could enhance differentiation efficiency, reduce leukemia clones, and provide personalized intervention strategies. However, further research is necessary to evaluate the safety and specificity of these interventions, particularly with regard to preserving normal hematopoiesis.
Conclusions
Our results demonstrate that miR-99a overexpression dysregulates normal hematopoiesis by stimulating HSPC proliferation and inhibiting differentiation, which are critical biological alterations closely linked to the development of leukemogenesis. However, further mechanistic studies are needed to gain deeper insight into the role of miR-99a in normal and or malignant hematopoiesis, which may provide novel therapeutic opportunities.
Data availability
All data supporting the findings of this study are available within the article and its supplementary information file or are available from the corresponding author upon request. RNA-seq data generated for this study are available at the National Omics Data Encyclopedia (NODE) with the accession number OEP00005662 and the link https://www.biosino.org/node/project/detail/OEP00005662.
References
Doulatov, S. et al. Revised map of the human progenitor hierarchy shows the origin of macrophages and dendritic cells in early lymphoid development. Nat. Immunol. 11, 585–593. https://doi.org/10.1038/ni.1889 (2010).
Dick, J. E. Stem cells: Self-renewal writ in blood. Nature 423, 231–233. https://doi.org/10.1038/423231a (2003).
Wallace, J. A. & O’Connell, R. M. MicroRNAs and acute myeloid leukemia: therapeutic implications and emerging concepts. Blood 130, 1290–1301. https://doi.org/10.1182/blood-2016-10-697698 (2017).
Liu, Y. et al. Role of MicroRNAs, circrnas and long noncoding RNAs in acute myeloid leukemia. J. Hematol. Oncol. 12 https://doi.org/10.1186/s13045-019-0734-5 (2019).
Guo, S. et al. MicroRNA miR-125a controls hematopoietic stem cell number. Proc. Natl. Acad. Sci. U S A. 107, 14229–14234. https://doi.org/10.1073/pnas.0913574107 (2010).
Ooi, A. G. et al. MicroRNA-125b expands hematopoietic stem cells and enriches for the lymphoid-balanced and lymphoid-biased subsets. Proc. Natl. Acad. Sci. U S A. 107, 21505–21510. https://doi.org/10.1073/pnas.1016218107 (2010).
Gerrits, A. et al. Genetic screen identifies MicroRNA cluster 99b/let-7e/125a as a regulator of primitive hematopoietic cells. Blood 119, 377–387. https://doi.org/10.1182/blood-2011-01-331686 (2012).
Lechman, E. R. et al. Attenuation of miR-126 activity expands HSC in vivo without exhaustion. Cell. Stem Cell. 11, 799–811. https://doi.org/10.1016/j.stem.2012.09.001 (2012).
Haetscher, N. et al. STAT5-regulated microRNA-193b controls Haematopoietic stem and progenitor cell expansion by modulating cytokine receptor signalling. Nat. Commun. 6, 8928. https://doi.org/10.1038/ncomms9928 (2015).
Bousquet, M., Nguyen, D., Chen, C., Shields, L. & Lodish, H. F. MicroRNA-125b transforms myeloid cell lines by repressing multiple mRNA. Haematologica 97, 1713–1721. https://doi.org/10.3324/haematol.2011.061515 (2012).
O’Connell, R. M. et al. MicroRNAs enriched in hematopoietic stem cells differentially regulate long-term hematopoietic output. Proc. Natl. Acad. Sci. U S A. 107, 14235–14240. https://doi.org/10.1073/pnas.1009798107 (2010).
Wong, P. et al. The miR-17-92 MicroRNA Polycistron regulates MLL leukemia stem cell potential by modulating p21 expression. Cancer Res. 70, 3833–3842. https://doi.org/10.1158/0008-5472.CAN-09-3268 (2010).
Velu, C. S., Baktula, A. M. & Grimes, H. L. Gfi1 regulates miR-21 and miR-196b to control myelopoiesis. Blood 113, 4720–4728. https://doi.org/10.1182/blood-2008-11-190215 (2009).
Song, S. J. et al. The oncogenic MicroRNA miR-22 targets the TET2 tumor suppressor to promote hematopoietic stem cell self-renewal and transformation. Cell. Stem Cell. 13, 87–101. https://doi.org/10.1016/j.stem.2013.06.003 (2013).
Si, X. et al. Upregulation of miR-99a is associated with poor prognosis of acute myeloid leukemia and promotes myeloid leukemia cell expansion. Oncotarget 7, 78095–78109. https://doi.org/10.18632/oncotarget.12947 (2016).
Xing, S. et al. Transgenic expression of JAK2V617F causes myeloproliferative disorders in mice. Blood 111, 5109–5117. https://doi.org/10.1182/blood-2007-05-091579 (2008).
Petzer, A. L. et al. Characterization of primitive subpopulations of normal and leukemic cells present in the blood of patients with newly diagnosed as well as established chronic myeloid leukemia. Blood 88, 2162–2171 (1996).
Hu, Y. & Smyth, G. K. ELDA: extreme limiting Dilution analysis for comparing depleted and enriched populations in stem cell and other assays. J. Immunol. Methods. 347, 70–78. https://doi.org/10.1016/j.jim.2009.06.008 (2009).
Chen, M. et al. Targeting primitive chronic myeloid leukemia cells by effective Inhibition of a new AHI-1-BCR-ABL-JAK2 complex. J. Natl. Cancer Inst. 105, 405–423. https://doi.org/10.1093/jnci/djt006 (2013).
Breitman, T. R., Selonick, S. E. & Collins, S. J. Induction of differentiation of the human promyelocytic leukemia cell line (HL-60) by retinoic acid. Proc. Natl. Acad. Sci. U S A. 77, 2936–2940. https://doi.org/10.1073/pnas.77.5.2936 (1980).
Wang, R., Xia, L., Gabrilove, J., Waxman, S. & Jing, Y. Sorafenib Inhibition of Mcl-1 accelerates ATRA-Induced apoptosis in Differentiation-Responsive AML cells. Clin. Cancer Res. 22, 1211–1221. https://doi.org/10.1158/1078-0432.Ccr-15-0663 (2016).
Nowak, D., Stewart, D. & Koeffler, H. P. Differentiation therapy of leukemia: 3 decades of development. Blood 113, 3655–3665. https://doi.org/10.1182/blood-2009-01-198911 (2009).
Andersson, L. C., Jokinen, M. & Gahmberg, C. G. Induction of erythroid differentiation in the human leukaemia cell line K562. Nature 278, 364–365. https://doi.org/10.1038/278364a0 (1979).
Han, T. et al. Identification of novel genes and networks governing hematopoietic stem cell development. EMBO Rep. 17, 1814–1828. https://doi.org/10.15252/embr.201642395 (2016).
Anjos-Afonso, F. et al. Single cell analyses identify a highly regenerative and homogenous human CD34 + hematopoietic stem cell population. Nat. Commun. 13, 2048. https://doi.org/10.1038/s41467-022-29675-w (2022).
Passegue, E., Jamieson, C. H., Ailles, L. E. & Weissman, I. L. Normal and leukemic hematopoiesis: are leukemias a stem cell disorder or a reacquisition of stem cell characteristics? Proc. Natl. Acad. Sci. U S A. 100 (Suppl 1), 11842–11849. https://doi.org/10.1073/pnas.2034201100 (2003).
Gentles, A. J., Plevritis, S. K., Majeti, R. & Alizadeh, A. A. Association of a leukemic stem cell gene expression signature with clinical outcomes in acute myeloid leukemia. JAMA 304, 2706–2715. https://doi.org/10.1001/jama.2010.1862 (2010).
Eppert, K. et al. Stem cell gene expression programs influence clinical outcome in human leukemia. Nat. Med. 17, 1086–1093. https://doi.org/10.1038/nm.2415 (2011).
Metzeler, K. H. et al. A stem cell-like gene expression signature associates with inferior outcomes and a distinct MicroRNA expression profile in adults with primary cytogenetically normal acute myeloid leukemia. Leukemia 27, 2023–2031. https://doi.org/10.1038/leu.2013.181 (2013).
Kreso, A. & Dick, J. E. Evolution of the cancer stem cell model. Cell. Stem Cell. 14, 275–291. https://doi.org/10.1016/j.stem.2014.02.006 (2014).
Roden, C. & Lu, J. MicroRNAs in control of stem cells in normal and malignant hematopoiesis. Curr. Stem Cell. Rep. 2, 183–196. https://doi.org/10.1007/s40778-016-0057-1 (2016).
Ciccone, M. & Calin, G. A. MicroRNAs in myeloid hematological malignancies. Curr. Genomics. 16, 336–348. https://doi.org/10.2174/138920291605150710122815 (2015).
Lechman, E. R. et al. miR-126 regulates distinct Self-Renewal outcomes in normal and malignant hematopoietic stem cells. Cancer Cell. 29, 602–606. https://doi.org/10.1016/j.ccell.2016.03.015 (2016).
Emmrich, S. et al. miR-99a/100 ~ 125b tricistrons regulate hematopoietic stem and progenitor cell homeostasis by shifting the balance between TGFβ and Wnt signaling. Genes Dev. 28, 858–874. https://doi.org/10.1101/gad.233791.113 (2014).
Krantz, I. D. et al. Cornelia de Lange syndrome is caused by mutations in NIPBL, the human homolog of Drosophila melanogaster Nipped-B. Nat. Genet. 36, 631–635. https://doi.org/10.1038/ng1364 (2004).
Tonkin, E. T., Wang, T. J., Lisgo, S., Bamshad, M. J. & Strachan, T. NIPBL, encoding a homolog of fungal Scc2-type sister chromatid cohesion proteins and fly Nipped-B, is mutated in Cornelia de Lange syndrome. Nat. Genet. 36, 636–641. https://doi.org/10.1038/ng1363 (2004).
Jann, J. C. & Tothova, Z. Cohesin mutations in myeloid malignancies. Blood 138, 649–661. https://doi.org/10.1182/blood.2019004259 (2021).
Dang, J. et al. AMKL chimeric transcription factors are potent inducers of leukemia. Leukemia 31, 2228–2234. https://doi.org/10.1038/leu.2017.51 (2017).
Mazzola, M. et al. NIPBL: a new player in myeloid cell differentiation. Haematologica 104, 1332–1341. https://doi.org/10.3324/haematol.2018.200899 (2019).
Mazzola, M. et al. Dysregulation of NIPBL leads to impaired RUNX1 expression and Haematopoietic defects. J. Cell. Mol. Med. 24, 6272–6282. https://doi.org/10.1111/jcmm.15269 (2020).
Mannini, L., Cucco, F., Quarantotti, V., Krantz, I. D. & Musio, A. Mutation spectrum and genotype-phenotype correlation in Cornelia de Lange syndrome. Hum. Mutat. 34, 1589–1596. https://doi.org/10.1002/humu.22430 (2013).
Liu, T. et al. MYC predetermines the sensitivity of Gastrointestinal cancer to antifolate drugs through regulating TYMS transcription. EBioMedicine 48, 289–300. https://doi.org/10.1016/j.ebiom.2019.10.003 (2019).
Khalaj, M. et al. miR-99 regulates normal and malignant hematopoietic stem cell self-renewal. J. Exp. Med. 214, 2453–2470. https://doi.org/10.1084/jem.20161595 (2017).
Chan, S. M. & Majeti, R. Role of DNMT3A, TET2, and IDH1/2 mutations in pre-leukemic stem cells in acute myeloid leukemia. Int. J. Hematol. 98, 648–657. https://doi.org/10.1007/s12185-013-1407-8 (2013).
Pandolfi, A., Barreyro, L. & Steidl, U. Concise review: preleukemic stem cells: molecular biology and clinical implications of the precursors to leukemia stem cells. Stem Cells Transl Med. 2, 143–150. https://doi.org/10.5966/sctm.2012-0109 (2013).
Funding
This work was supported by grants National Natural Science Foundation of China (82270148), Special Research Funds for Central Universities (Peking Union Medical College, 3332023059 and 3332023060), CAMS Innovation Fund for Medical Sciences (2023-I2M-2–007), and Haihe Laboratory of Cell Ecosystem Innovation Fund (24HHXBSS00008).
Author information
Authors and Affiliations
Contributions
W.W. and X.H. contributed to the experimental design of the study. W.W. contributed to the performance of experiments, analysis and interpretation of data and writing of the manuscript. X.H. performed the experiments and contributed to analysis and interpretation of data. X.L. contributed to the performance of experiments and data analysis. Y.L. contributed to array data analysis. W.X. contributed to experimental performance. T.C. contributed to the experimental design and data analysis. X.S., contributed to study design analysis and writing of the manuscipt. Y.Z. and J.S. contributed to the concept and design of the study, critical revising of the draft and supervision. All authors gave final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, W., Hao, X., Lv, X. et al. Overexpression of miR-99a promoted expansion and suppressed differentiation of hematopoietic stem/progenitor cells. Sci Rep 15, 8890 (2025). https://doi.org/10.1038/s41598-025-92827-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92827-7