Abstract
Metabolic dysfunction-associated steatotic liver disease (MASLD) is an emerging global health concern with limited therapeutic options. Multivitamins, widely consumed dietary supplements, have been proposed to modulate oxidative stress and inflammation, potentially impacting MASLD progression. However, their efficacy in reducing mortality and other complications in MASLD remains unclear. Using data from the UK Biobank with 7 years of median follow-up period, this study assessed the association between multivitamin use and health outcomes, including all-cause mortality, liver-related mortality, cardio-cerebrovascular disease (CVD), and chronic kidney disease (CKD), in individuals with MASLD and those without steatotic liver disease. Inverse probability of treatment weighting (IPTW) was employed to adjust for confounders. Multivitamin users showed a significantly lower all-cause mortality risk in the MASLD cohort both before (HR: 0.88, 95% CI 0.81–0.95, P = 0.034) and after (HR: 0.94, 95% CI 0.88–1.00, P = 0.037) IPTW adjustment. Multivitamin use was also associated with the lower risk of CVD (HR: 0.72, 95% CI 0.68–0.76, P < 0.001) and CKD (HR: 0.73, 95% CI 0.67–0.81, P < 0.001) in the MASLD cohort. No significant reduction was found for liver-related mortality or liver cirrhosis incidence. These findings suggest that multivitamins might provide broader protective effects in populations with metabolic dysfunction. Further research is needed to clarify their role in liver-specific outcomes.
Similar content being viewed by others
Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD) is an emerging liver disorder that includes a spectrum of liver pathologies, ranging from hepatic steatosis to steatohepatitis, fibrosis, cirrhosis and hepatocellular carcinoma (HCC)1. As the global prevalence of obesity and type 2 diabetes are rising, the burden of MASLD would also be increased, which became the leading cause of liver-related morbidity worldwide2. The pathogenesis of MASLD is multifactorial, involving insulin resistance, lipid metabolism dysregulation, oxidative stress, and chronic inflammation3. Despite advances in the pathogenesis of the MASLD, effective therapeutic interventions are limited in the present era, emphasizing the requirement for novel approaches to both prevention and management.
Among the various lifestyle interventions considered for MASLD, dietary supplements have been focused recently. Among the supplements, multivitamins are widely used across the world, with studies indicating that nearly half of adults in developed countries consume them regularly4. Their use is often motivated by the belief that they could help prevent chronic diseases and promote longevity5. Despite their widespread utilization, evidence supporting their efficacy in preventing chronic diseases, including cardiovascular disease, cancer, and metabolic disorders, remains inconclusive. For instance, large-scale randomized controlled trials and observational studies have not consistently shown a clear benefit of multivitamin use in reducing overall mortality or the incidence of major chronic diseases6,7,8.
Despite widespread utilization of multivitamins, evidence supporting their efficacy in preventing chronic diseases, including cardiovascular disease, cancer, and metabolic disorders, remains inconclusive. Given these mixed results, it is important to investigate whether multivitamins might provide health benefits in specific contexts, such as liver health. Vitamins such as vitamin D, vitamin E, and other antioxidants found in multivitamin formulations have been shown to modulate oxidative stress and inflammation, both of which are critical mechanisms in the progression of MASLD9. However, it remains unclear whether multivitamins as a whole could help attenuate the progression of MASLD or offer protection against liver-related complications.
The present study utilized the data from the UK Biobank, a large cohort, to examine the association between multivitamin use and the progression of MASLD. Our study specifically investigated the effects of multivitamin use on key outcomes, including all-cause mortality, liver-related mortality, major vascular events, and chronic kidney disease (CKD) incidence, in individuals with MASLD. In addition, this study compared the effects of multivitamin use between individuals with MASLD and those without steatotic liver disease (No SLD), providing the broader insights of how multivitamin use might differentially impact these populations. By utilizing inverse probability of treatment weighting (IPTW) to account for potential confounding factors of the baseline health characteristics, we minimized bias and provided more estimates of the true effects of multivitamin use.
Methods
Study design and data source
This study utilized data from the UK Biobank, a large-scale biomedical database containing health information on approximately 500,000 participants across the UK. Specifically, this study focused on participants categorized into three groups: the entire cohort, the No SLD cohort, and the MASLD cohort. The UK Biobank Application ID for this research is 117,214. Ethical approval was obtained from the North West Multi-Centre Research Ethics Committee, and all participants provided written informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Study population
Participants included in the study were diagnosed with MASLD based on the presence of hepatic steatosis, as determined by imaging or histology, and at least one cardiometabolic risk factor (CMRF). CMRFs included obesity (BMI ≥ 30 kg/m2 or ≥ 25 kg/m2 in Asians), type 2 diabetes, hypertension (blood pressure ≥ 130/85 mmHg or use of antihypertensive medication), dyslipidemia characterized by hypertriglyceridemia (triglycerides ≥ 150 mg/dL or lipid-lowering treatment), or low HDL cholesterol (men < 40 mg/dL, women < 50 mg/dL). Participants who exceeded the alcohol consumption thresholds were excluded to ensure compliance with the MASLD diagnostic criteria10. Individuals without clinical information were excluded, as well as those with significant alcohol consumption, or other chronic liver diseases to ensure specificity to MASLD. Specifically, individuals consuming more than 210 g of alcohol per week for men and 140 g per week for women were excluded, in accordance with the Delphi consensus statement on the definition of metabolic dysfunction and alcohol-associated liver disease10. This included participants with autoimmune hepatitis, chronic hepatitis B, chronic hepatitis C, primary biliary cirrhosis, cryptogenic steatotic liver disease, and alcohol-related liver diseases, including those with metabolic dysfunction and alcohol-associated liver disease and those with solely alcohol-associated liver disease. After these exclusions, the final study cohort consisted of 402,476 participants (Supplementary Fig. 1). Participants were categorized based on multivitamin use, identified through self-reported data from the “Vitamin and/or mineral supplement use” (Data-Field: 20084) and prescription records from the “Treatment/medication code” (Data-Field: 20003) during the observation period, ensuring the enrollment of participants with consistent multivitamin use throughout the study.
Primary and secondary outcomes
The primary outcomes were all-cause mortality and liver-related mortality. All-cause mortality was defined as the time from MASLD diagnosis to death from any cause, while liver-related mortality was defined as death from liver-specific causes, including cirrhosis or HCC. Secondary outcomes included the incidence of liver cirrhosis, cardio-cerebrovascular disease (CVD), and CKD. These events were tracked throughout the follow-up period and compared between multivitamin users and non-users across the study’s cohorts (No SLD and MASLD). Diagnoses were based on the date of the first recorded ICD-10 code during the observation period.
Statistical analysis
Baseline characteristics of the study population were summarized using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Covariate balance between multivitamin users and non-users, as well as between smoking status groups, was assessed using standardized mean differences (SMDs). Kaplan-Meier survival curves were generated to visualize overall survival and liver-related survival between multivitamin users and non-users. Differences in the survival curves were tested using the log-rank test. Cox proportional hazards models were applied to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations between multivitamin use and both primary and secondary outcomes, adjusting for relevant covariates.
The incidence rates of liver cirrhosis, CVD, and CKD were calculated and compared between groups. Cox proportional hazards models were also applied to assess the risks of these outcomes, adjusting for baseline covariates. A P value less than 0.05 was considered statistically significant for all tests. To account for potential confounders and balance baseline characteristics between multivitamin users and non-users, IPTW was utilized. Propensity scores were calculated using logistic regression models that included variables such as age, sex, body mass index, diabetes status, hypertension, dyslipidemia, and physical activity levels. Participants were then weighted by the inverse of their propensity score to create a weighted cohort with balanced covariates, minimizing selection bias and simulating a randomized controlled trial. To minimize the influence of extreme weights, we applied truncation at the 1st and 99th percentiles of the stabilized weight distribution and ensured a more stable estimation while maintaining covariate balance. The SMD was used to ensure that baseline characteristics were balanced after IPTW, and the effect of IPTW was visually evaluated using love plots. Most of the statistical analyses were conducted using R (version 4.2.3; R Foundation for Statistical Computing, Vienna, Austria) as the primary software tool.
Results
Baseline characteristics of the population
Baseline characteristics of multivitamin users and non-users were compared across the entire cohort, No SLD, and MASLD groups. In the entire cohort, 3.3% of participants were multivitamin users, while 96.7% were non-users. This distribution was similar across subgroups, with 3.7% of participants in the No SLD group and 3.1% in the MASLD group reporting multivitamin use (Supplementary Table 1, Supplementary Fig. 2). Notable differences were observed in key variables such as body mass index, with a mean of 27.3 kg/m2 in multivitamin users and 26.8 kg/m2 in non-users. Additionally, the prevalence of type 2 diabetes was higher in non-users (10.5%) compared to multivitamin users (8.0%). After applying IPTW adjustment, these differences were effectively minimized, with SMDs for all covariates significantly reduced, indicating a good balance between the groups (Supplementary Table 2, Supplementary Fig. 3).
In the MASLD cohort, significant differences between multivitamin users and non-users were observed in variables such as age (mean age 57.0 vs. 56.9 years, respectively), waist circumference (mean 97.4 cm vs. 95.9 cm), and physical activity levels before the IPTW adjustment. After IPTW, the SMDs for these variables were reduced, with age having an SMD of 0.005 and waist circumference showing an SMD of 0.04, indicating that the IPTW method effectively balanced these covariates between the groups (Table 1, Supplementary Fig. 3). In summary, IPTW adjustment successfully balanced the baseline characteristics between multivitamin users and non-users, as evidenced by the significant reduction in SMDs across all cohorts.
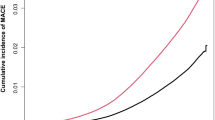
Survival and incidence of liver cirrhosis in various cohort with or without liver disease
The comparison of all-cause mortality between multivitamin users and non-users was evaluated in the entire cohort, No SLD, and MASLD groups, both before and after IPTW adjustment. In the entire cohort, multivitamin users had a significantly lower all-cause mortality compared to non-users before IPTW (HR: 0.94, 95% CI 0.89–1.00, P = 0.040) (Table 2, Supplementary Fig. 4A). However, after IPTW adjustment, the difference in all-cause mortality between the two groups was no longer statistically significant in the multivariate analysis (HR: 0.96, 95% CI 0.90–1.02, P = 0.203) (Table 2, Supplementary Fig. 4B). In the No SLD cohort, there was no significant difference of all-cause mortality between multivitamin users and non-users before IPTW adjustment (HR: 0.91, 95% CI 0.82–1.02, P = 0.103) and this trend remained after IPTW adjustment (HR: 0.93, 95% CI 0.84–1.04, P = 0.158), in univariate analysis (Table 2; Fig. 1A and B).
Kaplan-Meier curves comparing all-cause mortality between multivitamin users and non-users in No SLD and MASLD cohorts. (A) No SLD cohort before IPTW. (B) No SLD cohort after IPTW. (C) MASLD cohort before IPTW. (D) MASLD cohort after IPTW. OS, overall survival, IPTW, inverse probability of treatment weighting; SLD, steatotic liver disease; MASLD, metabolic dysfunction-associated steatotic liver disease.
In contrast, the MASLD cohort showed a different pattern. Before IPTW adjustment, multivitamin users had significantly lower all-cause mortality compared to non-users in multivariate analysis (HR: 0.88, 95% CI 0.81–0.95, P = 0.034) (Table 2; Fig. 1C). After IPTW adjustment, multivitamin users also showed a significantly lower mortality risk (HR: 0.94, 95% CI 0.88–1.00, P = 0.037) in the multivariate analysis (Table 2; Fig. 1D). In addition, multivitamin users had no significance in lowering risk of liver-related mortality and liver cirrhosis incidence compared to non-users in the entire, No SLD, and MASLD cohort, both before and after IPTW adjustment (Supplementary Tables 3 and Supplementary Fig. 4C and 4D). Overall, multivitamin use was associated with a significantly lower all-cause mortality in both the entire cohort and the MASLD group before IPTW adjustment. However, after IPTW adjustment, the association remained significant only in the MASLD group, with no significant effect on liver-related mortality or liver cirrhosis incidence.
Major vascular events with or without MASLD between multivitamin users and non-users
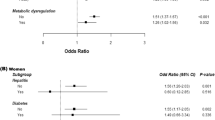
Next, we aimed to explore the effect of multivitamin on CVD, with the evidence of favorable effect of low dose multivitamin on nonfatal myocardial infarction11. The incidence and risk of CVD, including both cardiovascular and cerebrovascular events, were evaluated across the entire cohort, as well as in the No SLD and MASLD groups, based on multivitamin use. In the entire cohort, multivitamin users had a significantly lower risk of CVD compared to non-users (HR: 0.74, 95% CI 0.71–0.78, P < 0.001) (Table 3; Fig. 2A, Supplementary Fig. 5A). For cardiovascular events, multivitamin users also had a lower risk of events compared to non-users (HR: 0.75, 95% CI 0.71–0.79, P < 0.001) (Supplementary Table 4, Supplementary Fig. 5B and 6). In addition, multivitamin users showed a significantly lower risk for cerebrovascular disease (HR: 0.81, 95% CI 0.75–0.88, P < 0.001) (Supplementary Table 5, Supplementary Fig. 5C and 7).
Forest plot of the HRs and CIs for cardio-cerebrovascular disease and chronic kidney disease in each cohort. (A) Risk of cardio-cerebrovascular disease (B) Risk of chronic kidney disease. SLD, steatotic liver disease; MASLD, metabolic dysfunction-associated steatotic liver disease; HR, hazard ratio.
In the No SLD cohort, multivitamin users had a significantly lower risk of CVD (HR: 0.89, 95% CI 0.82–0.97, P = 0.008) (Table 3; Fig. 2A, Supplementary Fig. 6A and 7). While there was a significantly lower risk of cardiovascular disease with multivitamin use (HR: 0.90, 95% CI 0.81–0.99, P = 0.035), the significance diminished for the cerebrovascular disease (HR: 1.04, 95% CI 0.92–1.19, P = 0.523) (Supplementary Tables 4 and 5, Fig. 3A and B, Supplementary Fig. 7). In the MASLD cohort, multivitamin users exhibited a significantly lower risk of CVD (HR: 0.72, 95% CI 0.68–0.76, P < 0.001) (Table 3; Fig. 2A, Supplementary Fig. 6B). There were also significant lower risks for both cardiovascular disease (HR: 0.74, 95% CI 0.70–0.79, P < 0.001) and cerebrovascular disease (HR: 0.74, 95% CI 0.66–0.82, P < 0.001) (Supplementary Tables 4 and 5, Fig. 3C and D, Supplementary Fig. 7). These data suggest that multivitamin use was linked to a significantly lower risk of CVD, including both cardiovascular and cerebrovascular events, in the entire cohort, No SLD, and MASLD groups, with the most substantial reductions observed in the MASLD cohort.
Kaplan-Meier curves assessing cardiovascular and cerebrovascular events in No SLD and MASLD cohorts. (A) Cardiovascular events in the No SLD cohort. (B) Cerebrovascular events in the No SLD cohort. (C) Cardiovascular events in the MASLD cohort. (D) Cerebrovascular events in the MASLD cohort. SLD, steatotic liver disease; MASLD, metabolic dysfunction-associated steatotic liver disease.
Effect of multivitamin on CKD incidence with or without MASLD
Research indicates that patients with CKD are highly likely to experience vitamin deficiencies, making supplementation an important consideration in their treatment plan12. The incidence and risk of CKD were assessed in the entire cohort, No SLD, and MASLD groups, comparing the multivitamin users and non-users. In the entire cohort, multivitamin users had a significantly lower incidence of CKD compared to non-users (HR: 0.73, 95% CI 0.68–0.79, P < 0.001) (Table 4; Fig. 2B, Supplementary Fig. 5D). In the No SLD cohort, multivitamin users also exhibited a lower incidence of CKD compared to non-users (HR: 0.83, 95% CI 0.72–0.97, P = 0.020) (Table 4; Fig. 2B, Supplementary Fig. 6C). In the MASLD cohort, there was a similar potential benefit, with multivitamin users having a significantly lower risk of CKD (HR: 0.73, 95% CI 0.67–0.81, P < 0.001) (Table 4; Fig. 2B, Supplementary Fig. 6D). These results consistently show that multivitamin use is associated with a lower risk of CKD across all cohorts, with the strongest association observed in the MASLD group.
Discussion
This study evaluated the effect of multivitamin use on various health outcomes, including all-cause mortality, liver-related mortality, major vascular events, and CKD in individuals with MASLD and those without steatotic liver disease (No SLD). Using data from the UK Biobank, we found that multivitamin users experienced significantly lower risks of CVD and CKD, with the most prominent protective link observed in individuals with MASLD. These findings contributed to providing evidences suggesting that certain dietary supplements, particularly multivitamins, might have beneficial effects on health, especially in populations with underlying metabolic disorders such as MASLD.
One of the key findings from the present study is the significant reduction in all-cause mortality observed in multivitamin users within the MASLD cohort. Although the overall cohort showed a trend toward reduced mortality among multivitamin users, the effect was more prominent in individuals with MASLD. These data suggest that multivitamins might exert more substantial protective effects in populations with metabolic dysfunction. MASLD is characterized by an increased burden of oxidative stress, inflammation, and insulin resistance, all of which contribute to disease progression13,14,15. Multivitamins, particularly those containing antioxidants such as vitamins D and E, may interrupt these pathogenic mechanisms, thereby reducing mortality risk16,17,18.
Previous studies have reported controversial results on the association between multivitamin use and mortality in the general population. For instance, large cohort studies such as the Physicians’ Health Study II and the Women’s Health Initiative found no clear benefit of multivitamin use on cardiovascular events and malignancies19,20. Nevertheless, our study suggests that individuals with MASLD might represent a distinct population in which multivitamins could be linked to lower risks. This result is consistent with previous research highlighting the role of antioxidants in reducing oxidative stress and inflammation, both of which are central to the pathogenesis of MASLD. In particular, Vitamin E has been shown to improve liver histology in patients with steatohepatitis, a more advanced form of MASLD, by reducing liver inflammation and oxidative damage21,22.
Vitamin deficiencies, particularly of vitamins C, D, and E, are commonly observed in patients with type 2 diabetes and cardiometabolic diseases, and are associated with increased oxidative stress, endothelial dysfunction, and chronic inflammation. These micronutrients play critical roles in modulating gene expression and signal transduction pathways that contribute to anti-inflammatory, antioxidant, and hypolipidemic effects23. In the context of MASLD, where metabolic dysfunction and systemic inflammation are prominent, multivitamin supplementation might provide targeted benefits by attenuating these pathogenic processes. Our study demonstrated that multivitamin use was associated with reduced risks of CVD and CKD, particularly in individuals with MASLD, suggesting that improvements in micronutrient status could translate into significant clinical outcomes.
Furthermore, vitamin D, another key component of multivitamin formulations, is known to play a crucial role in regulating immune function and modulating inflammation24,25. Vitamin D deficiency has been linked to worse outcomes in individuals with metabolic diseases, including MASLD, due to its role in reducing pro-inflammatory cytokine production and enhancing insulin sensitivity26,27,28. Vitamin D deficiency has been strongly associated with the progression of CKD, and supplementation may help slow kidney function decline, particularly in individuals with MASLD who are at increased risk of renal complications due to metabolic dysfunction29. Additionally, the antioxidant properties of vitamins C and E may help reduce renal oxidative stress and inflammation, thereby preserving kidney function and reducing the incidence of CKD in high-risk populations30. Therefore, the observed reduction in all-cause mortality in MASLD patients who use multivitamins may reflect the combined impact of these vitamins on reducing the systemic inflammatory and metabolic burden associated with MASLD. Collectively, vitamin D has established immunomodulatory and anti-inflammatory effects, which are particularly relevant in metabolic diseases such as MASLD and CKD.
Our findings also demonstrated a significant reduction in the risk of CVD in multivitamin users across all cohorts, with the greatest effect shown in the MASLD group. CVD, including both cardiovascular and cerebrovascular events, is a major complication in individuals with metabolic disorders like MASLD, where insulin resistance, dyslipidemia, and chronic inflammation contribute to increased vascular risk31,32. The protective effect of multivitamins including vitamin A, B, C, D, and E, on CVD may be attributed to several factors, including the antioxidant properties of vitamins, their ability to improve endothelial function, and their role in modulating blood pressure and lipid levels33,34,35,36.
In particular, vitamins such as C and E are potent antioxidants that can reduce oxidative stress, a major contributor to vascular dysfunction in metabolic diseases37. Oxidative stress damages endothelial cells, promotes atherosclerosis, and impairs vascular reactivity, all of which increase the risk of cardiovascular events38. By reducing oxidative damage, multivitamins might help preserve vascular integrity and reduce the incidence of both cardiovascular and cerebrovascular events. Although previous studies suggest that vitamins C and E may contribute to improved endothelial function and vascular health, the direct impact of multivitamin supplementation on CVD risk in MASLD remains speculative and requires further investigation37,38.
In addition to the observed reduction in CVD, our study found that multivitamin use was associated with a significantly lower incidence of CKD across all cohorts, particularly in the MASLD group. CKD is a common comorbidity in individuals with metabolic disorders, and the progression of both CKD and MASLD is driven by similar etiologies, including hypertension, type 2 diabetes, chronic inflammatory state and dyslipidemia39. The reduction in CKD risk among multivitamin users would reflect the role of specific vitamins, such as D and E, in modulating these pathogenic processes. Vitamin D deficiency has been strongly associated with the progression of CKD, and supplementation may help slow kidney function decline, particularly in individuals with MASLD who are at increased risk of renal complications due to metabolic dysfunction29. Additionally, the antioxidant properties of vitamins C and E may help reduce renal oxidative stress and inflammation, thereby preserving kidney function and reducing the incidence of CKD in high-risk populations30.
Although the observed effect sizes of multivitamin use on MASLD-related outcomes were modest (HRs ranging from 0.7 to 0.9), even small risk reductions could have significant clinical and public health implications. Given the increasing global burden of MASLD and its associated complications, interventions with even modest protective effects might be valuable. Multivitamins are widely used, and their potential health benefits extend beyond liver-related outcomes. Our findings contribute to the broader discussion on preventive strategies for metabolic and liver diseases. Future studies, particularly randomized controlled trials, are required to elucidate the role of multivitamin supplementation in individuals with MASLD.
The strengths of this study include the use of a large, well-characterized cohort from the UK Biobank, which provided robust data on participants’ health, lifestyle, and clinical outcomes. The application of IPTW to control for confounding factors also strengthens the validity of our findings, allowing for more accurate estimates of the effects of multivitamin use. However, there are several limitations. First, multivitamin use was self-reported, which could introduce recall bias or inaccuracies regarding the frequency and duration of supplementation. Additionally, we could not specify formulations of multivitamins used by participants, which would differ in their composition and effects. Furthermore, the observational nature of the study means that we cannot infer causality, and residual confounding by unmeasured factors may still be present. In addition, despite the application of IPTW to balance measured confounders, residual confounding due to unmeasured health-related behaviors, such as diet quality, physical activity, and healthcare utilization, might still influence the observed associations, representing a potential healthy user bias. Moreover, the reliance on self-reported multivitamin use at baseline does not capture long-term adherence, as the UK Biobank lacks longitudinal data on supplement consumption. Notably, although the UK Biobank recruited participants from the general population, the voluntary nature of enrollment may have led to a cohort that is healthier and more health-conscious than the broader population, potentially introducing selection bias. Lastly, the UK Biobank cohort is predominantly of European ancestry, limiting the generalizability of our findings to more diverse ethnicity.
Conclusions
In conclusion, this study provides evidence that multivitamin use is associated with reduced all-cause mortality, CVD, and CKD, particularly in individuals with MASLD. While multivitamins do not appear to be significantly associated with liver-related mortality or cirrhosis incidence, they offer broader potential benefit, especially in populations with metabolic dysfunction. These findings suggest that multivitamin supplementation would be an alternative option in the prevention and management of chronic diseases in high-risk individuals.
Data availability
The data used in this study were obtained from the UK Biobank under application number 117214. Due to data sharing restrictions, the raw data cannot be made publicly available. However, researchers could apply for access to the UK Biobank dataset by following the procedures outlined on the UK Biobank website. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CMRF:
-
Cardiometabolic risk factor
- CVD:
-
Cardio-cerebrovascular disease
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- IPTW:
-
Inverse probability of treatment weighting
- MASLD:
-
Metabolic dysfunction-associated steatotic liver disease
- SLD:
-
Steatotic liver disease
- SMD:
-
Standardized mean difference
References
Lekakis, V. & Papatheodoridis, G. V. Natural history of metabolic dysfunction-associated steatotic liver disease. Eur. J. Intern. Med. 122, 3–10 (2023).
Teng, M. L. et al. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin. Mol. Hepatol. 29, 32 (2023).
Guariglia, M., Saba, F., Rosso, C. & Bugianesi, E. Molecular mechanisms of Curcumin in the pathogenesis of metabolic dysfunction associated steatotic liver disease. Nutrients 15, 5053 (2023).
Loftfield, E. et al. Multivitamin use and mortality risk in 3 prospective US cohorts. JAMA Netw. Open. 7, e2418729. https://doi.org/10.1001/jamanetworkopen.2024.18729 (2024).
Cowan, A. E. et al. Dietary supplement use differs by socioeconomic and health-related characteristics among US adults, NHANES 2011–2014. Nutrients 10, 1114 (2018).
Behrendt, I., Eichner, G. & Fasshauer, M. Association of antioxidants use with all-cause and cause-specific mortality: A prospective study of the UK biobank. Antioxidants 9, 1287 (2020).
Li, K., Kaaks, R., Linseisen, J. & Rohrmann, S. Vitamin/mineral supplementation and cancer, cardiovascular, and all-cause mortality in a German prospective cohort (EPIC-Heidelberg). Eur. J. Nutr. 51, 407–413 (2012).
Loftfield, E. et al. Multivitamin use and mortality risk in 3 prospective US cohorts. JAMA Netw. Open. 7, e2418729–e2418729 (2024).
Raza, S., Tewari, A., Rajak, S. & Sinha, R. A. Vitamins and non-alcoholic fatty liver disease: A molecular insight. Liver Res. 5, 62–71 (2021).
Rinella, M. E. et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology 78, 1966–1986. https://doi.org/10.1097/hep.0000000000000520 (2023).
Holmquist, C., Larsson, S., Wolk, A. & De Faire, U. Multivitamin supplements are inversely associated with risk of myocardial infarction in men and women—Stockholm heart epidemiology program (SHEEP). J. Nutr. 133, 2650–2654 (2003).
Juszczak, A. B., Kupczak, M. & Konecki, T. Does vitamin supplementation play a role in chronic kidney disease?? Nutrients 15, 2847 (2023).
Nakagawa, H. et al. ER stress cooperates with hypernutrition to trigger TNF-dependent spontaneous HCC development. Cancer Cell. 26, 331–343 (2014).
Meakin, P. J. et al. Susceptibility of Nrf2-null mice to steatohepatitis and cirrhosis upon consumption of a high-fat diet is associated with oxidative stress, perturbation of the unfolded protein response, and disturbance in the expression of metabolic enzymes but not with insulin resistance. Mol. Cell. Biol. 34, 3305–3320 (2014).
Huby, T. & Gautier, E. L. Immune cell-mediated features of non-alcoholic steatohepatitis. Nat. Rev. Immunol. 22, 429–443 (2022).
Rains, J. L. & Jain, S. K. Oxidative stress, insulin signaling, and diabetes. Free Radic. Biol. Med. 50, 567–575 (2011).
Argano, C. et al. The role of vitamin D and its molecular bases in insulin resistance, diabetes, metabolic syndrome, and cardiovascular disease: State of the Art. Int. J. Mol. Sci. 24, 15485 (2023).
Sepidarkish, M. et al. The effect of vitamin D supplementation on oxidative stress parameters: A systematic review and meta-analysis of clinical trials. Pharmacol. Res. 139, 141–152 (2019).
Sesso, H. D. et al. Multivitamins in the prevention of cardiovascular disease in men: The physicians’ health study II randomized controlled trial. Jama 308, 1751–1760 (2012).
Neuhouser, M. L. et al. Multivitamin use and risk of cancer and cardiovascular disease in the women’s health initiative cohorts. Arch. Intern. Med. 169, 294–304 (2009).
Podszun, M. C. et al. Vitamin E treatment in NAFLD patients demonstrates that oxidative stress drives steatosis through upregulation of de-novo lipogenesis. Redox Biol. 37, 101710 (2020).
Bril, F. et al. Role of vitamin E for nonalcoholic steatohepatitis in patients with type 2 diabetes: A randomized controlled trial. Diabetes Care. 42, 1481–1488 (2019).
Aguilera-Mendez, A. et al. Role of vitamins in the metabolic syndrome and cardiovascular disease. Pflugers Arch. 474, 117–140. https://doi.org/10.1007/s00424-021-02619-x (2022).
Vanherwegen, A. S., Gysemans, C. & Mathieu, C. Regulation of immune function by vitamin D and its use in diseases of immunity. Endocrinol. Metabol. Clin. 46, 1061–1094 (2017).
Mousa, A., Misso, M., Teede, H., Scragg, R. & De Courten, B. Effect of vitamin D supplementation on inflammation: Protocol for a systematic review. BMJ Open. 6, e010804 (2016).
Sung, C. C., Liao, M. T., Lu, K. C. & Wu, C. C. Role of vitamin D in insulin resistance. BioMed Res. Int. 634195 (2012).
Vanherwegen, A. S., Gysemans, C. & Mathieu, C. Vitamin D endocrinology on the cross-road between immunity and metabolism. Mol. Cell. Endocrinol. 453, 52–67 (2017).
Calton, E. K., Keane, K. N., Newsholme, P. & Soares, M. J. The impact of vitamin D levels on inflammatory status: A systematic review of immune cell studies. PLoS ONE. 10, e0141770 (2015).
Williams, S., Malatesta, K. & Norris, K. Vitamin D and chronic kidney disease. Ethn. Dis. 19, S5 (2009).
Rapa, S. F., Di Iorio, B. R., Campiglia, P., Heidland, A. & Marzocco, S. Inflammation and oxidative stress in chronic kidney disease—potential therapeutic role of minerals, vitamins and plant-derived metabolites. Int. J. Mol. Sci. 21, 263 (2019).
Zhao, X. et al. The crucial role and mechanism of insulin resistance in metabolic disease. Front. Endocrinol. 14, 1149239 (2023).
Powell-Wiley, T. M. et al. Obesity and cardiovascular disease: A scientific statement from the American heart association. Circulation 143, e984–e1010 (2021).
Mitu, O. et al. The effect of vitamin supplementation on subclinical atherosclerosis in patients without manifest cardiovascular diseases: Never-ending hope or underestimated effect? Molecules 25, 1717 (2020).
Ülker, S., McKeown, P. P. & Bayraktutan, U. Vitamins reverse endothelial dysfunction through regulation of eNOS and NAD (P) H oxidase activities. Hypertension 41, 534–539 (2003).
Behers, B. J. et al. Vitamins and minerals for blood pressure reduction in the general, normotensive population: A systematic review and meta-analysis of six supplements. Nutrients 15, 4223 (2023).
Gholamzad, A., Khakpour, N., Kabipour, T. & Gholamzad, M. Association between serum vitamin D levels and lipid profiles: A cross-sectional analysis. Sci. Rep. 13, 21058 (2023).
Traber, M. G., Stevens, J. F. Vitamins C and E: Beneficial effects from a mechanistic perspective. Free Radic. Biol. Med. 51, 1000–1013 (2011).
Förstermann, U., Xia, N. & Li, H. Roles of vascular oxidative stress and nitric oxide in the pathogenesis of atherosclerosis. Circul. Res. 120, 713–735 (2017).
Byrne, C. D. & Targher, G. NAFLD as a driver of chronic kidney disease. J. Hepatol. 72, 785–801 (2020).
Funding
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (RS-2023-00238039). This work was also supported by the Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Contributions
Study concept and design: Tom Ryu, Hyun Yang, Keungmo Yang; Data curation and resources: Seung Yun Chae, Beom Sun Chung; Formal analysis: Tom Ryu, Jaejun Lee; Methodology: Hyun Yang, Jaejun Lee; Software development and data visualization: Ji Won Han; Drafting of the manuscript: Tom Ryu; Critical revision of the manuscript: Keungmo Yang; Funding acquisition: Tom Ryu. All authors reviewed and approved the final manuscript, had full access to the data, and ensured its accuracy and integrity. All authors are accountable for the work and approved the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The UK Biobank obtained ethical approval from the North West Multicenter Research Ethics Committee.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ryu, T., Chae, S.Y., Lee, J. et al. Multivitamin supplementation and its impact in metabolic dysfunction-associated steatotic liver disease. Sci Rep 15, 8675 (2025). https://doi.org/10.1038/s41598-025-92858-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92858-0