Abstract
The isolation of pathogenic Leptospira is fundamental for a comprehensive characterization of circulating strains in endemic regions. Unfortunately, culture methods of Leptospira spp. are laborious and challenging. Here, we present a method for the isolation of these pathogenic bacteria from non-fresh serum samples, previously stored at 4–8 °C for several days. Briefly, 730 serum samples collected from leptospirosis-suspected patients (presenting acute signs) were screened for Leptospira DNA by real-time PCR. Thirty-one PCR-positive sera were then assessed for Leptospira isolation on specialized media for up to 6 months. Using this methodology, 11 Leptospira isolates were obtained, resulting in an isolation rate of 35.4% (11/31). Through whole-genome analysis, ten strains were identified as Leptospira santarosai and one strain as Leptospira borgpertersenii. The isolates were classified into six different serogroups, namely Hebdomadis, Shermani, Tarassovi, Pyrogenes, Ballum, and Grippotyphosa, demonstrating a wide diversity of Leptospira strains circulating in Costa Rica. This study reveals that serum is a suitable sample for Leptospira isolation in patients with positive PCR results, even after maintenance at cold conditions, promoting the use of serum for Leptospira isolation in reference laboratories around the world.
Similar content being viewed by others
Introduction
Leptospirosis is a widespread zoonosis caused by pathogenic bacteria of the genus Leptospira1,2. The highest incidences of Leptospira infection occur in tropical and subtropical countries, where abundant rainfall and frequent flooding favors its transmission3. Over one million cases of leptospirosis are estimated annually, responsible of approximately 60,000 deaths worldwide4. In humans, the disease manifests as an acute febrile illness with non-specific symptoms such as fever, malaise, joint pain, headache. Remarkably, this disease can evolve into severe multiorgan failure, involving renal failure and jaundice, a condition known as “Weil Syndrome”, associated with a mortality rate that ranges from 5 to 50%5,6. In the tropics, the disease is frequently underdiagnosed, since the symptoms overlap with other circulating febrile diseases, such as dengue fever, rickettsioses, ehrlichiosis, brucellosis, malaria, chikungunya, and zika3,7.
The main reservoirs of Leptospira are wild and domestic mammals, with rodents being the most common hosts8. In humans, infection occurs through direct contact with the urine or body fluids of infected animals, or indirectly through the exposure of environments, such as soil or water, contaminated with the urine of reservoir infected animals9,10.
Costa Rica is an endemic country for leptospirosis11,12. This country has a great variety of microclimates and experiences a prolonged rainy season from May to the end of November. These conditions often result in flooding in both urban and rural areas, creating a favorable environment for the permanence of Leptospira. Notably, in 1997, an outbreak of leptospirosis in Costa Rica was linked to water rafting in flooded rivers13. Between 2001 and 2005, the Costa Rican National Reference for Leptospirosis group isolated Leptospira santarosai, Leptospira interrogans, and Leptospira noguchii from febrile patients (laboratory records, unpublished data). Among these isolates, three strains of L. santarosai corresponded to serovars not previously described. These were named serovar Arenal (belonging to serogroup Javanica14), serovar Corredores (from the serogroup Tarassovi) and serovar Costa Rica (belonging to serogroup Pyrogenes12). These findings confirm the endemic nature of leptospirosis in Costa Rica and suggest a widespread diversity of Leptospira in the region.
The isolation and proper identification of Leptospira spp. is crucial for comprehending the local epidemiology and transmission cycles of circulating strains in an endemic region. Such insights can subsequently improve serological panels used for diagnosing leptospirosis in humans and animals15. However, the culture of Leptospira spp. is a laborious technique that has historically presented many challenges for reference laboratories. The slow growth rate of Leptospira makes then highly susceptible to contamination, and their isolation requires specialized media16.
In human diagnosis, whole blood has traditionally been the specimen of choice for Leptospira isolation, whereas other samples, such as urine and cerebrospinal fluid, are also used1. Although serum samples are commonly submitted to clinical laboratories for serological diagnosis of febrile illnesses, they are not typically used for molecular diagnosis or isolation of Leptospira spp. Here, we present an in-house culture protocol for the isolation of Leptospira from serum samples previously maintained in refrigeration (i.e., 4–8 °C) for up to ten days. The implementation of this protocol allowed the culture of 11 Leptospira isolates from serum samples collected from 2020 to 202117. Through molecular analyses, ten isolates were confirmed as Leptospira santarosai and one as L. borgepetersenii, classified into six distinct serogroups. The results present here demonstrated the wide biodiversity of Leptospira strains circulating in Costa Rica. We are certain that this method will promote the isolation of Leptospira in other laboratories worldwide.
Materials and methods
Clinical samples
In Costa Rica, all the clinical samples from patients suspected of leptospirosis are referred to the Laboratory of Zoonotic Febrile Diseases of the National Reference Center of Bacteriology (previously known as Costa Rican National Reference for Leptospirosis), at the Costa Rican Institute of Research and Education in Nutrition and Health (INCIENSA), for diagnosis and confirmation. Accordingly, from November 2020 to December 2021, 730 serum samples from patients in the acute phase of the disease (1–6 days since onset of symptoms) were received. All the samples were analyzed by real-time PCR and serology, without excluding samples in which the patient had previously received treatment with antibiotics. The clinical samples were stored at 4 °C from one to ten days before further analyses (Fig. 1).
Stepwise protocol for the isolation of Leptospira from serum human samples. (1) Patient with febrile symptoms compatible with leptospirosis and with 1–6 days from the onset of symptoms. (2). Draw blood into collection tubes without additives. (3) Centrifugation of blood sample in a bench centrifuge at 3500 rpm for 10 min to obtain serum. (4) Storage of serum samples at 4–8 °C until further analysis. (5) Extraction of genomic DNA from 200 µl of serum samples. (6) Real time PCR targeting the Leptospira-secY gene (a Ct of 40 was considered positive when the Tm value of the amplicon from 2 or more replicates did not vary by more than 0.5 °C). (7) Five drops of each of the qPCR-positive serum samples were inoculated in 6 ml of Ellinghausen-McCullough-Johnson-Harris (EMJH) medium supplemented with albumin-fatty-acid-supplement (AFAS) and in EMJH medium supplemented with sulfamethoxazole-trimethoprim-amphotericin-fosfomycin-5-fluorouracil (STAFF) and AFAS. (8) The culture tubes were incubated at 30 °C for 6 months until turbidity was observed. (9) Once a tube becomes turbid, the culture was examined by dark field microscopy to determine the presence of leptospires. (10) Cultures confirmed positive by dark-field microscopy were further characterized using microagglutination test (MAT) and whole-genome sequencing (WGS).
Clinical and epidemiological information of the patients
The clinical and epidemiological information of the patients was obtained from the specimen submission forms that are referred together with the clinical samples to the INCIENSA for diagnosis of leptospirosis. The information included geographic distribution, sex, age, symptoms, of each patient, as well as risk factors of exposure.
Serological diagnosis of Leptospira
The 730 serum samples were analyzed by the Serion ELISA Classic Leptospira IgM (Virion/Serion, Germany) kit, according to manufacturer´s instructions. In addition, the samples were evaluated using the microagglutination test (MAT)18 with a panel of 35 reference Leptospira serovars (Supplementary Table 1).
DNA extraction and real-time PCR amplification
Genomic DNA was extracted from 200 µl of serum using the StarMag 96 extraction kit and the automatized platform SEEPREP 32 (Seegene, Korea) according to manufacturer’s instructions. Pathogenic Leptospira DNA was amplified using the real-time PCR assay targeting the secY gene19 in a 7500 Fast Real-Time PCR system (Applied Biosystems). The following conditions were applied: reactions were performed in a total volume of 25 µl, consisting of 1x Platinum SYBR Green qPCR SuperMix-UDG (Fischer Scientific, USA), forward (SecYIVF, 5´-GCGATTCAGTTTAATCCTGC-3´) and reverse primers (SecYIV, 5´-GAGTTAGAGCTCAAATCTA-AG-3´) were added at a final concentration of 400 nM each, 0.5 µl of a solution of ROX 1X, freshly prepared for in each run, and 10 µl of extracted DNA. The amplification protocol consisted of 4 min at 95 °C, followed by 45 cycles of amplification (95 °C for 10 s, 54 °C for 5 s, 72 °C for 15 s). Subsequently, the reaction was stopped at 95 °C for 2 min, cooled (20 °C for 1 min), followed by a melting analysis from 70 to 95 °C, with plate readings set at 0.5 °C. The samples were analyzed by triplicates. A sample was considered positive with a Ct value < 42, and only if the melting temperature (Tm) of two or more replicates meet the Leptospira-secY profile (single peak of 78.5–84.5ºC), not varying by more than 0.5 ºC.
Serum in-house isolation protocol for Leptospira spp.
Serum samples secY-PCR-positive were processed for Leptospira isolation by an in-house culture protocol (Fig. 1). Briefly, the refrigerated serum samples and culture reagents were tempered at room temperature before inoculation. After brief mixing by vortex, five drops of each serum were inoculated in 6 ml of liquid Ellinghausen-McCullough-Johnson-Harris (EMJH) medium (Difco) supplemented with albumin-fatty-acid-supplement (AFAS, University Medical Centers AMC, Netherlands), hereinafter referred as “EMJH”, and in 6 ml of EMJH supplemented with “sulfamethoxazole-trimethoprim-amphotericin-fosfomycin-5-fluorouracil” media (STAFF)20, hereinafter referred as “EMJH-STAFF”. Then, culture tubes were incubated at 30ºC for up to 6 months or until turbidity was observed (weekly checked). Once turbid, a 5 µl culture aliquot was examined by dark field microscopy to determine the presence of leptospires. To avoid contamination, culture tubes were only opened in a biosafety cabinet and only once turbidity was visually detected.
Serotyping of isolates
The serotyping of the isolated strains to serogroup level was performed by the microagglutination test (MAT) using a panel of 45 polyclonal rabbit antisera against reference serovars of Leptospira comprising 23 pathogenic and one saprophytic serogroup (OIE Reference Laboratory for Leptospirosis, AMC, Netherlands) (Supplementary Table 2). High rates of agglutination (cut-off titer ≥ 1:320) of the isolate with the antisera of a specific serogroup were indicative of the presumptive serogroup. Isolates were further analyzed by MAT using sets of specific monoclonal antibodies (Supplementary Table 3; OIE Reference Laboratory for Leptospirosis, AMC, Netherlands) to determine isolate affiliation between serogroups, for those cases where high titers were found to different serogroups.
Whole-genome characterization
The libraries and whole-genome characterization of the isolates was performed at the Biology of Spirochetes Unit, Institut Pasteur, Paris, France, as previously described17. Genomic analyses to determine the species of the strains and the core-genome multilocus sequence typing (cgMLST) profiles were performed using the Bacterial Isolate Genome Sequence Database (BIGSdb) hosted at the Institut Pasteur (https://bigsdb.pasteur.fr/leptospira/). Moreover, genomic assemblies were compared to the deposited Leptospira genomes in the BIGSdb. For this, 61 additional genomes of L. santarosai and 287 genomes of L. borgpetersenii were downloaded. Prokka21 was used for genome annotation and core genome was obtained using Panaroo protocol22. A maximum likelihood phylogenetic tree was constructed using the core gene alignment output from Panaroo on IQ-TREE23. The resulting ML tree was uploaded in GrapeTree24. The presence and absence output table obtained from Panaroo was converted into a binary table and imported to R25 to calculate Jaccard distances using vegan package26 and ggpubr package27 to calculate Spearman’s rank correlation tests. The average nucleotide identities (ANI) were calculated with FastANI28.
Data accessibility
Genome assemblies were deposited in the BIGSdb (https://bigsdb.pasteur.fr/leptospira/) under the identification (id) numbers 1251–1261.
Ethical considerations
According to decree number 40556-s of the General Health Law of Costa Rica, epidemiological studies that incorporate the review of clinical records do not require the approval of an ethics-scientific committee. Human samples were anonymized, and collection of the samples was conducted according to the Declaration of Helsinki.
Consent statement
The need to obtain informed consent was waived by the Costa Rican Institute for Research and Education in Nutrition and Health (INCIENSA) Scientific Committee.
Results
Serological diagnosis of Leptospira in study samples
Out of 730 sera evaluated, 41 (5.6%, 41/730) tested reactive for Leptospira IgM ELISA. However, all 730 samples were negative when tested by the microscopic agglutination test (MAT).
Molecular detection of Leptospira in serum samples
From the 730 sera analyzed by real-time PCR targeting the secY gene, amplification of pathogenic Leptospira DNA was detected in 42 (5.7%) samples (Supplementary Table 4). Seven (16%) of these PCR-positive patients were also ELISA Leptospira IgM reactive (Supplementary Table 4).
Isolation of Leptospira strains from serum samples
Thirty-one of the PCR positive serum samples stored at 4 °C were cultured in EMJH and EMJH-STAFF. Due to insufficient volume, culture could not be performed on 11 PCR-positive sera. A total of 11 Leptospira strains were isolated, both in the EMJH and the EMJH-STAFF media, yielding a 35.4% (11/31) isolation rate. Previously to the isolation protocol, the storage time at 4 °C of the positive samples ranged 3 to 9 days (Supplementary Table 4). The average time for culture positivity was 7.45 weeks (5 to 10 weeks). Notably, the average (± standard deviation) Ct value of the serum samples that were positive by culture was 37.49 ± 2.62. These amplicons presented an average Tm value of 81.36 ± 0.45 °C (Supplementary Table 4). Average Ct and Tm values of the samples in which Leptospira was not isolated were 37.41 ± 2.80 and 81.16 ± 0.69, respectively, suggesting that the number of bacteria in the original sample was not crucial for a successful isolation.
Clinical and epidemiological information of the patients
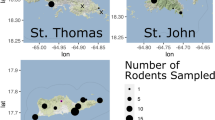
We collected the clinical and epidemiological information of the 11 patients from which Leptospira was isolated (Table 1). The samples were referred from the north, central and south regions of the country (Fig. 2). Ten out of the 11 patients were male. The age of the patients ranged from 17 to 68 years old, being seven of the patients under 28 years old.
Most of the patients presented mild symptoms at the time of sample collection, including fever, arthralgia, myalgia, headache, abdominal pain, vomit, diarrhea, and chills, except for patient #8 (Table 1), who presented a severe disease with jaundice, liver failure, seizures, and had to be admitted to the intensive care unit. None of the patients died from the infection.
Seven patients reported a risk factor for infection with Leptospira, including agricultural work, livestock occupation and exposure to water bodies. In four patients, risk factor data was not included in their report.
Serotyping of the Leptospira isolates
Serotyping of the 11 Leptospira isolates identified six distinct serogroups, namely: Hebdomadis, Shermani, Tarassovi, Pyrogenes, Grippotyphosa and Ballum (Table 2). Notably, the polyclonal antisera exhibited strong cross-reactivity between the serogroups Manhao-Pyrogenes, Hebdomadis-Mini-Sejroe, Shermani-Tarassovi, Autumnalis-Ballum, Grippotyphosa-Autumnalis, respectively. In ten isolates, the monoclonal antibodies determined the final affiliation to the specific serogroup. Isolate CR0421 (Table 2), resulted in strong reactions with the polyclonal antisera against serogroups Grippotyphosa (> 1:20480), Djasiman (1:2560), Louisiana (1:1280) and Cynopteri (1:640). The monoclonal antibodies F71C9 (Grippotyphosa), F69C11, F69C15 (Cynopteri) yielded negative results against this isolate.
Whole-genome characterization of the isolates
Whole genome sequencing analyses identified 10 isolates as L. santarosai and one isolate as L. borgpetersenii (Table 2). Genomic analyses and comparison with the BIGSdb database showed that all isolates correspond to novel and different cgMLST sequence types (cgST), except for the L. borgpetersenii that matched its cgST with isolates from Uruguay (n = 1, from human source), Cuba (n = 1, from human source), and Saint Kitts and Nevis (n = 3, from rodent sources) (Supplementary Figs. 1 and 2).
The phylogenetic analyses between L. santarosai strains from Costa Rica showed no identical pair of genomes (Fig. 3). Accordingly, whole-genome ANI values ranged from 98.57 to 99.88%, being the farthest related pair of genomes BIGSdb-id 1255 (Shermani strain from this study) and BIGSdb-id 1215 (Inciensa-04 strain, Pyrogenes serogroup collected in 2004), whereas the closest pair was BIGSdb-id 1254 and BIGSdb-id 1257 (a Tarassovi and a Grippotyphossa strains, respectively). Despite the nucleotide similarities revealed, marked differences were evident among their genetic content (i.e., shared genes), with diversities ranging from 64.5 to 94.1% of shared genes (i.e., Jaccard distance ranging from 0.059 to 0.355; (Fig. 3).
Discussion
In this study we demonstrated that serum is a suitable sample for isolation of Leptospira in patients confirmed of leptospirosis by real-time PCR. Using this method, we could isolate 11 Leptospira non-clonally related strains, belonging to six serogroups. The ability to isolate different serogroups and species, suggested that this method presents no bias to certain group of leptospires.
Although whole blood has traditionally been the sample of choice for the molecular detection and isolation of Leptospira, it presents several challenges due to the low bacterial loads commonly found in such samples29,30. Firstly, blood contains PCR-inhibitory substances, such as hemoglobin, IgG immunoglobulins and lactoferrin, as well as anticoagulants commonly used in blood collection tubes, including sodium heparin and EDTA31. Secondly, additional factors such as antibiotics administered in cases where therapy has begun can further reduce the success of Leptospira isolation. Consequently, using blood for Leptospira diagnosis often lead to reduced sensitivity in both real-time PCR systems and isolation protocols16,32. While serum samples may also contain inhibitory substances, their concentrations are much lower than those found in whole blood31. For instance, in healthy individuals, normal hemoglobin levels range from 12 to 18 g per deciliter (g/dl) in whole blood, while in plasma or serum ranges below 5 mg/dL33. Therefore, serum samples are proposed as a more suitable matrix for Leptospira molecular diagnosis and isolation34.
It has been acknowledged that the successful isolation of Leptospira depends significantly on processing freshly obtained clinical samples15. This means that the time elapsed between sample collection and inoculation into leptospiral culture medium is crucial for achieving successful isolation15. However, in our study, four out of the 11 isolates were obtained from specimens with six or more days of storage at 4 °C, demonstrating that Leptospira remains viable in non-fresh clinical serum samples, even in samples with low Leptospira loads, as evidenced by their high real-time PCR Ct values. Similarly, the isolation of Leptospira weilii from a separator tube was previously reported after stored at 4 °C for a week35. These findings will facilitate and promote the isolation of Leptospira in samples commonly received in reference laboratories for other diagnostic methodologies such as serology.
In this study, 16% of the patients with a positive PCR result were also positive for anti-Leptospira IgM antibodies, demonstrating that detectable leptospires can be found in patients concomitantly with an early IgM antibody response. Remarkably, none of the patients were positive by MAT, evidencing the lower sensitivity of this technique for the initial stages of the disease15.
Six different serogroups were identified among the patients, namely Hebdomadis, Shermani, Grippotyphosa, Tarassovi, Pyrogenes and Ballum. Since different animal hosts are preferentially infected with different Leptospira serovars36, the serological identification of the isolates allows the identification of the potential sources of the infection in humans15. Accordingly, raccoons, marsupials, and armadillos have been described as reservoirs for Hebdomadis serogroup37,38; Shermani has been associated with livestock39; Grippotyphosa serogroup has been associated with a wide range of mammals such as opossums40, rodents, bats37, horses41, dogs42, among others; while swine is the main reservoir for Tarassovi serogroup36,43,44; Pyrogenes serogroup has been associated mainly to dairy cattle45; and, the reservoirs for Ballum serogroup are mainly rodents, such as mice and rats46,47,48. Remarkably, Costa Rica is one of the most biodiverse places on the planet, hosting the 4.5% of the world’s ecological diversity49 and has a wide variety of microenvironments in which Leptospira could thrive and maintain in nature. Thus, the diversity of Leptospira serogroups detected in this study correlates with this potential reservoir diversity. Serovars Arenal, Corredores and Costa Rica, belonging to serogroups Javanica, Tarassovi and Pyrogenes respectively, were described for the first time in Costa Rica from human blood samples12,14, suggesting that more serovars not yet described may be actively circulating in this territory. Therefore, exploring environmental and animal samples in Costa Rica is essential to gaining a comprehensive understanding of the presence and distribution of both saprophytic and pathogenic Leptospira in the region.
Genomic analyses of the isolates in this study classified ten strains as L. santarosai and one isolate (CR2021 Ballum) corresponds to L. borgpertersenii. The genomic characterization of the sequences from L. santarosai strains demonstrated a close phylogenetic but not clonal relationships between the isolates. In fact, none of the strains were identical in their nucleotide identities (i.e., ANI comparison). Moreover, their gene content was diverse within this species, reflecting its open pangenome17. Interestingly, we found only a moderate correlation between the gene content and the nucleotide similarities among all sequenced L. santarosai genomes. Altogether, these results demonstrated the broad diversity of Leptospira spp. not only at the nucleotide level but also in the genes carried within their genomes.
From the confirmed leptospirosis cases in which Leptospira was isolated, 10 common non-specific signs were recorded: fever, arthralgia, myalgia, headache, abdominal pain, vomit, chills, diarrhea, dizziness, and jaundice. Only one patient showed severe symptomatology, presenting convulsions and liver failure. Interestingly, this patient carried the only L. borgpertersenii isolated. Notably, L.santarosai and L. borgpetersenii belong to the subclade P1 of pathogenic Leptospira and are grouped together in subgroup 250,51. At the time of the drawn of the samples, ten of the patients infected with L. santarosai showed mild to moderate symptomatology and none of the patients had a fatal outcome. It will be interesting to further explore potential pathogenicity levels between the species of the subclade P1 and to analyze the gene content of clinical isolates in patients showing a wide variety of symptoms and outcomes, from mild to severe.
A limitation of this study arises from the use of secY as the target for detection of acute leptospirosis. PCR assays directed to secY and other genes, such as lipL32 52,53, present low sensitivity for Leptospira spp. with intermediate pathogenicity, hence limiting their diagnosis scope. Thus, it is important the exploration of new targets that may allow the detection of both highly and intermediate pathogenic leptospires to better understand the etiology of leptospirosis in the country.
In conclusion, this study presents a method that facilitates the isolation of Leptospira from the serum of ill-patients. We demonstrated that a great diversity of Leptospira serogroups belonging to two pathogenic species were successfully isolated from the serum of patients in a year period, even after the maintenance of the serum samples at 4 °C, evidencing that the methodology is not biased towards a certain group of strains. We believe that our results will serve other reference laboratories in their diagnosis of Leptospirosis.
Data availability
Genome assemblies were deposited in the BIGSdb (https://bigsdb.pasteur.fr/leptospira/) under the identification (id) numbers 1251-1261.
References
Levett, P. N. Leptospirosis Clin. Microbiol. Rev. 14, 296–326 (2001).
Farr, R. W. Leptospirosis Clin. Infect. Dis. 21, 1–8 (1995).
Valente, M. et al. Diagnosis of human leptospirosis: systematic review and meta-analysis of the diagnostic accuracy of the Leptospira microscopic agglutination test, PCR targeting Lfb1, and IgM ELISA to Leptospira fainei serovar Hurstbridge. BMC Infect. Dis. 24, 1–22 (2024).
Costa, F. et al. Global morbidity and mortality of leptospirosis: A systematic review. PLoS Negl. Trop. Dis. 9, e0003898 (2015).
WHO. Human Leptospirosis: Guidance for Diagnosis, Surveillance and Control (World Health Organization and International Leptospirosis Society, 2003).
McBride, A. J. A., Athanazio, D. A., Reis, M. G. & Ko, A. I. Leptospirosis. Curr. Opin. Infect. Dis. 18, 376–386 (2005).
Halliday, J. E. B. et al. Zoonotic causes of febrile illness in malaria endemic countries: a systematic review. Lancet Infect. Dis. 20, e27–e37 (2020).
Gomard, Y., Dellagi, K., Goodman, S. M., Mavingui, P. & Tortosa, P. Tracking animal reservoirs of pathogenic leptospira: The right test for the right claim. Trop. Med. Infect. Dis. 6 (2021).
Monteiro, M. B., de Sousa, I. E., Piteira, M., Coelho, S. & Freitas, P. Leptospirosis, a re-emerging threat. Cureus 13 (2021).
Faine, S., Adler, B., Bolin, C. & Perolat, P. Leptospira’ and Leptospirosis. Leptospira and Leptospirosis (MediSci, 1999).
Costa, F. et al. Surveillance for leptospirosis in the Americas, 1996-2005: a review of data from ministries of health. Rev. Panam. Salud Publica. 32 (3), sept2012–sept2032 (2012). (2012).
de los Valverde, M. New serovars of Leptospira isolated from patients in Costa Rica: implications for public health. J. Med. Microbiol. 62, 1263–1271 (2013).
Centers for Disease Control and Prevention (CDC). Outbreak of leptospirosis among White-Water rafters -- Costa Rica, 1996. MMWR Morb Mortal. Wkly. Rep. 46, 577–579 (1997).
de los Valverde, M. Arenal, a new Leptospira serovar of serogroup Javanica, isolated from a patient in Costa Rica. Infect. Genet. Evol. 8, 529–533 (2008).
Sykes, J. E., Reagan, K. L., Nally, J. E., Galloway, R. L. & Haake, D. A. Role of diagnostics in epidemiology, management, surveillance, and control of leptospirosis. Pathogens 11, 395 (2022).
Wuthiekanun, V. et al. Optimization of culture of Leptospira from humans with leptospirosis. J. Clin. Microbiol. 45, 1363–1365 (2007).
Chinchilla, D. et al. Phylogenomics of Leptospira Santarosai, a prevalent pathogenic species in the Americas. PLoS Negl. Trop. Dis. 17, e0011733 (2023).
Goris, M. G. A. & Hartskeerl, R. A. Leptospirosis serodiagnosis by the microscopic agglutination test. Curr Protoc Microbiol 32, 1–18 (2014).
Ahmed, A., Engelberts, M. F. M., Boer, K. R., Ahmed, N. & Hartskeerl, R. A. Development and validation of a real-time PCR for detection of pathogenic leptospira species in clinical materials. PLoS ONE 4 (2009).
Chakraborty, A. et al. A novel combination of selective agents for isolation of Leptospira species. Microbiol. Immunol. 55, 494–501 (2011).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Tonkin-Hill, G. et al. Producing polished prokaryotic pangenomes with the Panaroo pipeline. Genome Biol. 21, 1–21 (2020).
Nguyen, L. T., Schmidt, H. A., Von Haeseler, A. & Minh, B. Q. IQ-TREE: A fast and effective stochastic algorithm for estimating Maximum-Likelihood phylogenies. Mol. Biol. Evol. 32, 268–274 (2015).
Zhou, Z. et al. GrapeTree: visualization of core genomic relationships among 100,000 bacterial pathogens. Genome Res. 28, 1395–1404 (2018).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2021).
Oksanen, J. et al. Vegan: Community Ecology Package. R Package Version 2.5-7. (2020).
Kassambara, A. ggpubr ‘ggplot2’ Based Publication Ready Plots. R package version 0.6.0. (2023). https://rpkgs.datanovia.com/ggpubr/
Jain, C., Rodriguez-R, L. M., Phillippy, A. M., Konstantinidis, K. T. & Aluru, S. High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat. Commun. 9, 1–8 (2018).
Levett, P. Leptospira culture. in Clinical Microbiology Procedures Handbook (ASM, 2016).
Adler, B. De La Peña Moctezuma, A. Leptospira and leptospirosis. Vet. Microbiol. 140, 287–296 (2010).
Schrader, C., Schielke, A., Ellerbroek, L. & Johne, R. PCR inhibitors – occurrence, properties and removal. J. Appl. Microbiol. 113, 1014–1026 (2012).
Mgode, G. F. et al. Leptospira serovars for diagnosis of leptospirosis in humans and animals in Africa: common Leptospira isolates and reservoir hosts. PLoS Negl. Trop. Dis. 9, e0004251 (2015).
Hoffman, R. et al. Hematology: basic principles and practice. Hematology: Basic. Principles Pract. 1–2374. https://doi.org/10.1016/C2013-0-23355-9 (2017).
Allan, K. J. et al. Molecular detection and typing of pathogenic Leptospira in febrile patients and phylogenetic comparison with Leptospira detected among animals in Tanzania. Am. J. Trop. Med. Hyg. 103, 1427–1434 (2020).
Haake, D. A. et al. Leptospirosis, water sports, and chemoprophylaxis. Clin. Infect. Dis. 34, e40–43 (2002).
Bonhomme, D. & Werts, C. Host and species-specificities of pattern recognition receptors upon infection with Leptospira interrogans. Front. Cell. Infect. Microbiol. 12 (2022).
Cilia, G., Bertelloni, F., Albini, S. & Fratini, F. Insight into the epidemiology of leptospirosis: A review of Leptospira isolations from unconventional hosts. Anim. 2021. 11, Page 191 (11), 191 (2021).
Koizumi, N. et al. Isolation and characterization of Leptospira spp. From raccoons in Japan. J. Vet. Med. Sci. 71, 425–429 (2009).
Chadsuthi, S. et al. Investigation on predominant Leptospira serovars and its distribution in humans and livestock in Thailand, 2010–2015. PLoS Negl. Trop. Dis. 11, e0005228 (2017).
Cordeiro, F., Sulzer, C. & Ramos, A. Leptospira interrogans in several Widlife species in Southeast Brazil. Pesquisa Veterinária Brasileira. 1, 19–29 (1981).
Ellis, W. A., O’Brien, J. J., Cassells, J. A. & Montgomery, J. Leptospiral infection in horses in Northern Ireland: serological and Microbiological findings. Equine Vet. J. 15, 317–320 (1983).
Brown, C. A. et al. Leptospira interrogans serovar Grippotyphosa infection in dogs. J. Am. Vet. Med. Assoc. 209, 1265–1267 (1996).
Ellis, W. A., McParland, P. J., Bryson, D. G. & Cassells, J. A. Prevalence of Leptospira infection in aborted pigs in Northern Ireland. Vet. Rec. 118, 63–65 (1986).
Bertelloni, F. et al. Serological survey on bacterial and viral pathogens in wild boars hunted in Tuscany. Ecohealth 17, 85–93 (2020).
Hamond, C. et al. Leptospira borgpetersenii serovar Hardjo and Leptospira santarosai serogroup pyrogenes isolated from bovine dairy herds in Puerto Rico. Front. Vet. Sci. 9, 1025282 (2022).
Moinet, M. et al. Of mice, cattle, and men: A review of the eco-epidemiology of Leptospira borgpetersenii serovar ballum. Trop. Med. Infect. Dis. 6, 189 (2021).
Costa, F. et al. Household rat infestation in urban slum populations: development and validation of a predictive score for leptospirosis. PLoS Negl. Trop. Dis. 15, e0009154 (2021).
Hathaway, S. C. & Blackmore, D. K. Ecological aspects of the epidemiology of infection with leptospires of the ballum serogroup in the black rat (Rattus rattus) and the brown rat (Rattus norvegicus) in new Zealand. J. Hyg. (Lond). 87, 427–436 (1981).
Kohlmann, B. Biodiversity conservation in Costa Rica - An animal and plant biodiversity atlas. Res. Biodivers. - Models Appl. https://doi.org/10.5772/24546 (2011).
Xu, Y. et al. Whole genome sequencing revealed host adaptation-focused genomic plasticity of pathogenic Leptospira. Sci. Rep. 6, 1–11 (2016).
Vincent, A. T. et al. Revisiting the taxonomy and evolution of pathogenicity of the genus Leptospira through the Prism of genomics. PLoS Negl. Trop. Dis. 13, e0007270 (2019).
Galloway, R. L. & Hoffmaster, A. R. Optimization of LipL32 PCR assay for increased sensitivity in diagnosing leptospirosis. https://doi.org/10.1016/j.diagmicrobio.2015.03.024 (2015).
Id, A. A. A., Goris, M. G. A. & Meijer, M. C. Development of lipL32 real-time PCR combined with an internal and extraction control for pathogenic Leptospira detection. https://doi.org/10.1371/journal.pone.0241584 (2020).
Acknowledgements
The authors thank Israel Chaverri Salazar for sharing his vast experience in Leptospira diagnosis and Bernal Quirós Mendoza for his assistance in the preparation of the leptospiral culture media. The authors thank the Social Security System of Costa Rica for the referral of the clinical samples for diagnosis of leptospirosis and other zoonotic diseases. Also, we thank the personnel of the Zoonotic Febrile Diseases Laboratory of Costa Rica and the National Reference Center of Institut Pasteur for their daily work in the diagnosis of this disease.
Author information
Authors and Affiliations
Contributions
Conceptualization: DC, IS, DM. Data curation: DC, MP, RG. Formal analysis: DC, MP, RG. Methodology: DC, IS, DM. Resources: DC, MP. Supervision: DC, MP, RG. Writing - original draft: DC, RG.Writing - review & editing: DC, MP, RG.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chinchilla, D., Sánchez, I., Montero, D. et al. In-house isolation protocol from human serum samples demonstrates the circulating of a broad diversity of Leptospira serogroups in Costa Rica. Sci Rep 15, 9614 (2025). https://doi.org/10.1038/s41598-025-93301-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93301-0