Abstract
The Sydney lymphadenopathy cytology system was proposed in 2020, but its validation for neck ultrasound-guided fine-needle aspiration cytology remains to be explored. Patients with lymphadenopathy who underwent ultrasound and cytology were included. The final diagnosis relies on histology and consensus of the multidisciplinary team. Cytology results follow the Sydney system (L1-L5); L3-L5 categories indicate malignancy, and we further calculate sensitivity, specificity, and overall accuracy. From July 2020 to April 2023, a total of 208 patients were included, of which 68 had malignant tumors and 140 were benign cases. According to the Sydney system, the malignancy rates for L2 to L5 are 2%, 89%, 100%, and 98%, respectively. The Sydney system demonstrated 97% sensitivity, 99% specificity, and 99% accuracy in the diagnosis of neck lymphadenopathy. The study shows that the Sydney system is highly effective in reporting neck lymphadenopathy.
Similar content being viewed by others
Introduction
Head and neck cancers (HNC) are one of the most common cancers in the world1. A retrospective study of over 70,000 patients with HNC revealed that 52% have neck lymph node metastases at presentation2. Therefore, it is important to differentiate benignity and malignancy for neck lymphadenopathy. Ultrasound (US) examination is a useful tool to examine neck masses3. Abnormal lymphadenopathy is usually larger in size, irregular/burred in border, more heterogeneous in echotexture, rounder in size, harder in elastography, and absent of hilum in Doppler and contrast ultrasound4.
Since no single US characteristic is specific for malignancy, we combined age and three ultrasound characteristics to develop a comprehensive an ultrasound scoring system for assessing neck lymph nodes5. The validity of this scoring method has been previously confirmed6. Additionally, recent US elastography and contrast-enhanced US have also been applied to check in the evaluation of lymph nodes(LNs)7.
Excision biopsy is a method for harvesting tissue to determine its etiology. However, it’s important to note that most neck lymphadenopathies are benign and do not typically require excisional biopsy, which can result in skin wounds8. Fine needle aspiration serves as a viable alternative method for obtaining tissue samples without the need for excision. When performed under the guidance of real-time ultrasound (US-FNA), this procedure can yield more precise cytology specimens, especially in the case of non-palpable small lymph nodes9. This approach helps minimize invasiveness and provides valuable diagnostic information in a less invasive manner.
Cytology reporting relies on established systems, the Bethesda system and Milan system, are used for thyroid and salivary glandular tumor/nodule cytology10,11. Recently, the Sydney system was proposed for reporting lymphadenopathy4. Similar to the Bethesda system, the Sydney system categorizes lymphadenopathy five groups: inadequate/insufficient, benign, atypical undetermined significance/atypical lymphoid of uncertain significance (AUS/ALUS), suspicious, and malignant. This classification system was reported to be effective in lymphadenopathy12,13,14,15. Kanhe et al. reported that the accuracy of Sydney system for reporting lymphadenopathy was higher than 99%15. The study combined US guided and non-US-guided; rapid on-site evaluation and non-rapid on-site evaluation; neck lymphadenopathy and other sides.
Based on previous reports and meta-analyses12,16,17, use of the Sydney reporting system exhibits significant heterogeneity and is subject to inherent partial validation bias. This heterogeneity results from different operators, nodal sites, and clinical settings.
Therefore, the performance of Sydney system is still not well understood in cervical lymphadenopathies. In our setting, all procedures were performed in the cervical region by experienced head and neck surgeons under ultrasound guidance. This result can verify the effectiveness of the Sydney system in diagnosing cervical lymphadenopathy after US-FNA. We intend to check the performance of the ultrasound scoring system, elastography and Sydney system in reporting neck lymphadenopathy.
Methods
This is a cross-sectional study and the institutional ethics committee review board approved this study plan. (FEMH-IRB-109074-E). All patients signed written informed consent forms. Research was performed in accordance with the Declaration of Helsinki.
Patients
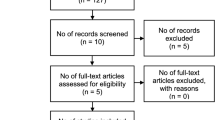
The inclusion criteria included patients more than 20 years old who had enlarged neck lymphadenopathy and at least one US characteristic abnormality5,18,19,20,21 (i.e., size, shape, hilar echogenicity, margin, or vascular pattern) that permitted US-FNA. Patients with lymph node enlargement identified by the Otolaryngology or Oncology departments at Far-Eastern Memorial Hospital were referred for ultrasound examination. The ultrasound scans were primarily conducted by Dr. Liao (the first author), with a smaller portion performed by Dr. Lo (the fourth author). Informed consent was obtained either by Dr. Liao or a research nurse who explained the study and invited patients to participate. Pathological examinations were mainly conducted by Dr. Wu (the second author) in the Pathology department. In the determination of the final diagnosis, pathology results are employed whenever accessible. In cases where pathology findings are unavailable, a collaborative approach is undertaken through a multidisciplinary team meeting, involving experts from the Pathology, Radiology, and Oncology departments. Patients who had negative cytopathology results were followed for a minimum of 6 months to verify that no malignancy had developed in these LNs afterward.
US examination
Sonograms were performed with one high-resolution 7- to 18-MHz real-time linear-array transducer (Aplio MX, Toshiba, Tokyo, Japan). The detailed method was described in our previous study5. In brief, all patients in our study underwent thorough neck US examination using grayscale, power Doppler US and US elastography. We measured the lengths of the short and long axes and the diameter ratio of the short to long axis (S/L ratio) of enlarged LNs. The nodal margin was classified as regular or irregular. Echogenicity compared to the adjacent muscles was speculated and classified as hypoechoic, isoechoic, or hyperechoic. The echogenic hilum was differentiated and classified as its presence or absence. The internal echotexture was examined and classified as a homogenous or heterogeneous pattern. The vascular pattern was evaluated with power Doppler US and grouped into avascular or hilar type versus mixed, spotted, or peripheral type. All the morphological US data were entered into our Marosis PACS system (Marotech Inc., Seoul, South Korea). A predictive scoring scale was proposed as: 0.06 x (age) + 4.76 x (S/L ratio) + 2.15 x (internal echo) + 1.80 x (vascular pattern). Cervical lymphadenopathy was regarded as malignant with a score > or = 75.
Elastography
For our elastographic technique, real-time elastographic images were demonstrated together with grayscale sonograms in a two-panel format. We further compressed with light pressure followed by decompression, which repeated the cycle until the size and color distribution of the region of interest (ROI) in numerous sequential images appeared nearly identical. Compression was directed along the radiation axis, with a focus on preventing any motions that deviate from the plane. Real-time elastographic visual employed a color-coded graphic format, with emphasis on the selected target area. Stiffness was denoted by blue, intermediate firmness by green and yellow, and softness by red within this representation. We used the 4-point scoring system22 to evaluate lymphadenopathy as follows: Elastographic score (ES) 1 represents soft (less than 10% of red areas), ES 2 represents moderately soft (10–50% of red areas), ES 3 represents moderately stiff (10–50% of blue, green, and yellow areas), and ES 4 represents stiff (less than 10% of blue, green, and yellow areas). An LN with RTE of ES 3 or 4 was classified as malignant.
Another elastographic technique employed in this study was shear wave elastography (SWE). Shear wave elastographic images were also displayed along with the grayscale sonograms in two-panel images for comprehensive evaluation. A high-intensity pulse is generated by the ultrasound probe toward the target, where perpendicular shear wave propagation is detected. The shear wave propagation is then converted and recorded as shear velocity (m/s) and Young’s modulus (kPa). The mean SWE value of the included lymphadenopathy was used as a cutoff value for evaluation. An LN with SWE higher than the cutoff value of SWE is classified as malignant.
US-FNA procedure
In US-guided FNA procedure, each patient underwent the process by placing the array probe parallel to the needle for guidance and with a 22-G needle within the node that was the most suspicious to be malignant. All procedures were performed after injection of local anesthesia and visualization of the needle as it advanced toward the desired target. During the US-FNA procedure, only one specimen was obtained through a single needle aspiration. The syringe needle unit was quickly withdrawn when the appropriate amount of material filled the plastic portion of the needle. Following the aspiration, two slides were prepared for cytological analysis: One of the two slides was air-dried for Liu’s stain, and the other was rapidly fixed in alcohol for the Papanicolaou stain. This meticulous approach ensured the acquisition of high-quality cytological specimens for accurate diagnostic evaluation. On-site examination was not available in this study.
Sydney system
The cases were classified according to the Sydney system4 into five groups, denoted as L1 to L5: L1: Inadequate/Insufficient; L2: Benign; L3: Atypical (cells) Undetermined Significance/Atypical Lymphoid (Cells) of Uncertain Significance (AUS/ALUS); L4: Suspicious and L5: Malignant. The categories L3 to L5 were classified as malignant, and calculate the sensitivity, specificity, and overall accuracy for the malignancy classification. This comprehensive approach allowed for a thorough assessment of diagnostic performance.
Statistical analysis
Mann‒Whitney U tests and chi-squared tests were used to determine the differences in clinical parameters (i.e., age, sex, side and site of occurrence, diameter of short and long axes, S/L ratio, echogenicity, internal echo, margin, echogenic hilus, vascular pattern, real-time elasticity score and our combined US L/N score5) between benign and malignant LNs as appropriate. The optimal cutoff point of ES in share wave elastography was determined at the point of highest accuracy for malignancy. The diagnostic accuracy was expressed as the sensitivity, specificity and area under the ROC curve (AUC). A p value < 0.05 was interpreted as statistically significant. All statistical analyses were accomplished using Stata software, version 12.0 (StataCorp. LP, College Station, TX).
Results
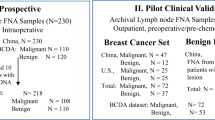
From July 2020 to April 2023, this study enrolled 208 patients presenting with neck lymphadenopathy, comprising 68 cases with malignancy and 140 with benign condition. Of these patients with malignant LNs, 61 underwent pathological examination (21 underwent lymphadenectomy and 5 underwent core needle biopsy of cervical LNS; 36 of these underwent biopsy at the primary site). After collaborative discussion by a multidisciplinary team, 7 patients were also diagnosed as malignant. Another 140 patients with negative cytopathology results were followed for at least 6 months to verify the subsequent presence of malignancy in these LNs. Nine of the patients underwent resection surgery.
The prevalence of malignant LNs was 33% (68/208). Of the enrolled patients, 117 were males, accounting for 56% of the patients, while 91 were females, constituting the remaining 44%. The mean age of the participants was 46 years old, with ages spanning a range from 20 to 82 years. Among the malignant LNs, 14 had nasopharyngeal carcinoma, 10 had hypopharyngeal cancer, 8 had oral cancer, 8 had papillary thyroid carcinoma, and 6 had esophageal carcinoma. Among individuals diagnosed with benign nodal disease, the majority (N = 122) were found to have reactive lymphoid hyperplasia. The patients’ final diagnoses are summarized in Table 1.
Table 2 presents the rate of malignancy based on the Sydney system classification. We found that the specimen inadequate rate of US-FNA was 2% (4/208). The malignancy rates varied across different Sydney system categories with rates of 2%, 89%, 100% and 98% for the L2 to L5 groups, respectively. Moving from L1 to L5, the probability of malignancy increases.
Table 3 demonstrates the patient and US characteristics for benign and malignant lymphadenopathies. In patients with malignant lymphadenopathies, there is a higher proportion of males, and the average age is comparatively older (55.9 yeas vs. 41.4 years) when compared to the benign group. However, there is no significant difference observed between the left and right sides of the lymph nodes. Malignant lymph nodes frequently tend to be larger in size, rounder in size (S/L ratio), and greater stiffness in both RTE and SWE. We also found that the LN score was notably higher in malignant lesions as compared to benign lesions, with respective mean scores (± SD) of 9.2 ± 2.6 versus 5.9 ± 1.8 (p value < 0.01).
A comparison of the diagnostic performance of elastography, share wave elastography, the US scoring system and the Sydney system in reporting neck lymphadenopathy is demonstrated in Table 4. The real-time elastography (ES 3&4) demonstrated a sensitivity of 62.7%, specificity of 58.2% and an overall accuracy of 59.8%. For shar wave elastography (> 44 kPa), the sensitivity was 63.9%, specificity was 62.0%, and the accuracy reached 62.6%. When utilizing the US scoring system, we observed a sensitivity of 81%, specificity of 77%, and an accuracy of 78%. Conversely, the Sydney system exhibited remarkable performance, with a sensitivity of 97%, specificity of 99% and a high accuracy of 99%.
Discussion
The aim of this study was to investigate the performance of the US scoring system, elastography, and the Sydney system in their ability to distinguish between benign and malignant LNs. Most patients with enlarged LNs first visited an otolaryngologist and arranged an ultrasound. Therefore, most LNs was metastatic cancer from the head and neck region. Under the guidance of US, FNA had a low rate of inadequate specimens, with only 2% (4/208) falling into this category. The variation in nondiagnostic rate, which ranged from 3.58 to 10.57% in other studies13,14,23,24,25, contrasts with the low nondiagnostic rate observed in our study. The low nondiagnostic rate in our study might be due to real-time US guidance with experience and superficial location of the neck LNs. In our opinion, the Sydney System is a very effective classification system for reporting the cytology of neck lymphadenopathy. It demonstrates a remarkable level of sensitivity (97%), specificity (99%), and overall accuracy (99%). These findings underscore the system’s reliability and utility in clinical practice.
FNA cytology remained one of the most accurate method for evaluating lymphadenopathy. The accuracy of FNA cytology in diagnosing malignant neck lymphadenopathy was approximately 82–97%26. However, there is no standard criterion for reporting the results of FNA cytology. The Sydney system plays a good role in reporting lymphadenopathy and showed good results in our study. A recent international, multi-institutional study reported the Sydney system had adequate interobserver concordance with digitally whole-slide images27. Another previous study in southern India app lied the Sydney system to evaluate neck lymphadenopathy, used L3-L5 as malignancy and reported a sensitivity and specificity of 93% and 95%, respectively25. The study had a nondiagnostic rate of 11%, while in our series, the nondiagnostic rate (L1) was only 2%. This highlighted the importance of real-time US guidance. The sensitivity, specificity and overall accuracy of FNAB when considering category L3 ~ L5 to represent malignant cytopathology in this study were 92.6%, 95.1% and 92.8%, respectively. The results were comparable to our study and support the useful of the Sydney system. It has been documented that cancer cells may be arranged as scattered infiltrative nests, often intermixed with fibrous stroma, which might hamper the chance of correct sampling and increase the possibility of false negative results28. In our series, we had two cases with false-negative cytology results. One patient with NPC underwent concurrent chemoradiotherapy, and another patient had thyroid papillary cancer. The cytology for thyroid cancer revealed no malignancy; however, there was a high thyroglobulin level in the washing examination. The final surgical pathology shown metastatic papillary cancer. Therefore, a washing thyroglobulin exam for residual material in the FNA needle is useful in diagnosing metastatic lymphadenopathy from thyroid cancer.
US characteristics play a pivotal role in distinguishing between benign and malignant neck lymphadenopathy. Because the malignant lymphadenopathy keep growth, therefore the size is bigger for malignancy. Additionally, the malignant lymph nodes invade in multiple directions, leading to rounder in shape and irregular in border, which are indicative features. Furthermore, due to the angiogenesis process, the malignant nodes often display atypical vascular features. The elastography can reveal increased tissue hardness in malignant nodes, primarily attributable to tissue fibrosis. All these characteristics can provide the information for malignant lymphadenopathy. However, most of these features are subjective and operator dependent and no single one characteristic has high sensitivity, specificity and accuracy.
Table 3 provides an overview of the US characteristics of benign and malignant lymphadenopathies in our cases series. Malignant lymph nodes were more common in male and older patients, tended to be larger in size and rounder in shape (as indicated by the S/L ratio) and were more likely to have vague boundaries, heterogeneous internal echotexture, calcifications, absent hilar echotexture, and other vascular patterns. We previously reviewed these characteristics and developed an US scoring system that also showed significant differences between benign and malignant lymphadenopathies in our study. Malignant lymph nodes also exhibited increased stiffness on both real-time elastography (RTE) and shear wave elastography (SWE). These findings suggest that clinical data, US features, and elasticity characteristics can serve as indicators for distinguishing between benign and malignant lymphadenopathies. The US scoring system demonstrated acceptable diagnostic performance. These findings highlight the importance of combining multiple diagnostic approaches to improve the accuracy of diagnosing neck lymphadenopathy. The US scoring system can be used as a screening tool, while the Sydney system can serve as the gold standard before the final histopathology.
Table 4 presents a comparison of the diagnostic performance of real-time elastography, shear wave elastography, the US scoring system, and the Sydney system. The US scoring system achieved a sensitivity of 81%, specificity of 77%, and overall accuracy of 78% in distinguishing between benign and malignant lymphadenopathy. On the other hand, the Sydney system exhibited higher sensitivity (97%), specificity (99%), and accuracy (99%). The post-hoc power analysis demonstrated a power of 86% for sensitivity and 99% for both specificity and accuracy. These findings suggest that the US scoring system can be used as a screening tool for diagnosing malignant LNs, while the Sydney system demonstrates superior performance and can serve as the gold standard before the final histopathology.
US elastography, on the other hand, showed poor diagnostic performance in this study. The sensitivity, specificity, and accuracy were 63%, 58%, and 60% for RTE with the 4-point scoring system, 64%, 62%, and 63% for SWE higher than 44 kPa, and 54%, 68%, and 64% for SWE higher than 3.8 m/s, respectively.
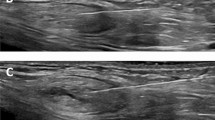
It is difficult to diagnose LNs after radiation therapy. Figure 1 demonstrates another case of a false-positive result; this is a hypopharyngeal cancer patient. He received an US exam 3 months after concurrent chemoradiotherapy. On US, multiple heterogeneous LNs above the carotid artery were found. US-FNA with the Sydney system was positive for malignancy. Preoperative US found lymph nodes with heterogeneous echo texture overriding the common carotid artery (Fig. 1A). On cytology, the smear showed a tumor necrotic debris background with some keratinocyte-like cells (in orange color) and some cell shadows with enlarged nuclei (in green color). This finding was comparable to malignancy in cytology according to the Sydney system (Fig. 1B). In the final pathology with H&E staining, calcifications, histiocytes, and necrotic debris with necrotic keratinocyte-like cells were observed (C: low power & D: high power). Because there were no viable carcinoma cells, the final diagnosis was no metastatic carcinoma.
There was one false-positive case in our study. Preoperative ultrasound found lymph nodes with heterogeneous echo texture overriding the common carotid artery (A). On cytology, the smear showed a tumor necrotic debris background with some keratinocyte-like cells (in orange color) and some cell shadows with enlarged nuclei (in green color). This finding was comparable to malignancy in cytology according to the Sydney system (B). In the final pathology with H&E staining, calcifications, histiocytes, and necrotic debris with necrotic keratinocyte-like cells were observed (C: low power & D: high power). Because there were no viable carcinoma cells, the final diagnosis was no metastatic carcinoma.
Diagnosing neck lymphadenopathy becomes challenging after radiation therapy due to the alterations in ultrasound and cytology findings. Documentation indicates that radiation therapy can lead to the disappearance of certain lymphoid tissues and the replacement of parts of lymph nodes with fibrous tissue. These changes can complicate the diagnostic process and necessitate careful evaluation to distinguish between benign and malignant conditions in the post-radiation context28. In our previous study, radiation therapy had influence on sonographic characteristics, ultimately impacting diagnostic accuracy in this patient population29. On computed tomography (CT) scans, the criteria used for detecting pathological lymph nodes, such as nodal necrosis or a short-axis diameter, can at times be deemed unreliable in the evaluation of irradiated neck regions30. According to previous systematic review and meta-analysis, the pooled sensitivity and specificity for identifying malignant lymph nodes in patients with a history of prior irradiation were found to be relatively modest, with values of 69.1% and 84.2%, respectively31. Therefore, it should be very careful in interpretation of the cytology results of LNs after radiation.
There are some limitations need to be mention. First, our study is constrained by a relatively small cases number and a single institution setting. Second, there is a degree of selection bias as most patients with a US scoring less than 7 did not received US-FNA examination. Third, we encountered a rarity of lymphoma cases in our study, and in such instances, we opted for ultrasound-guided core needle biopsy (US-CNB) when lymphoma was suspected. Therefore, the cases in our series is selected. In our opinion, ancillary techniques usually are still necessary to classified different types of lymphoma32. Further study focus on Sydney system in lymphoma diagnosis is still mandatory. Fourth, our dataset lacks contrast-enhanced ultrasound (CEUS) data, which could have provided additional valuable insights. Fifth, this study is still not well external validated, which should include more cases numbers and demographic information such as ethnicity, and make the results more robust.
Conclusion
In conclusion, this study provides valuable insights into the characteristics of neck lymphadenopathy and the diagnostic capabilities of various US methods. Specifically, the Sydney System demonstrated superior performance with higher sensitivity, specificity, and overall accuracy compared to the conventional US scoring system and elastography. Our findings observed that the Sydney System is very effective for reporting neck lymphadenopathy.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Sung, H. A. O. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Kuperman, D. I. et al. Squamous cell cancer of the head and neck with distant metastasis at presentation. Head Neck 33(5), 714–718 (2011).
Feier, J., Self, Q., Karabachev, A., Brundage, W. & Sajisevi M. Assessing the role of ultrasound for the evaluation of adult neck masses. Laryngoscope Investig. Otolaryngol. 8 (1), 135–139 (2023).
Al-Abbadi, M. A. et al. A proposal for the performance, classification, and reporting of lymph node Fine-Needle aspiration cytopathology: The Sydney system. Acta Cytol. 64(4), 306–322 (2020).
Liao, L. J., Wang, C. T., Young, Y. H. & Cheng, P. W. Real-time and computerized sonographic scoring system for predicting malignant cervical lymphadenopathy. Head Neck 32(5), 594–598 (2010).
Wu, M., Chen, H., Zheng, X. & Burstein, D. E. Evaluation of a scoring system for predicting lymph node malignancy in ultrasound guided fine needle aspiration practice. Diagn. Cytopathol. 41(12), 1100–1106 (2013).
Spiesecke, P., Neumann, K., Wakonig, K. & Lerchbaumer, M. H. Contrast-enhanced ultrasound (CEUS) in characterization of inconclusive cervical lymph nodes: A meta-analysis and systematic review. Sci. Rep. 12(1), 7804 (2022).
Cavallo, M. et al. An economic evaluation of fine-needle cytology as the primary diagnostic tool in the diagnosis of lymphadenopathy. Open Med. 18(1), 20230719 (2023).
Ahn, D., Kim, H., Sohn, J. H., Choi, J. H. & Na, K. J. Surgeon-performed ultrasound-guided fine-needle aspiration cytology of head and neck mass lesions: Sampling adequacy and diagnostic accuracy. Ann. Surg. Oncol. 22(4), 1360–1365 (2015).
Cibas, E. S. & Ali, S. Z. The Bethesda system for reporting thyroid cytopathology. Am. J. Clin. Pathol. 132(5), 658–665 (2009).
Rossi, E. D. et al. The Milan system for reporting salivary gland cytopathology: Analysis and suggestions of initial survey. Cancer Cytopathol. 125(10), 757–766 (2017).
Gupta, P. et al. Assessment of risk of malignancy by application of the proposed Sydney system for classification and reporting lymph node cytopathology. Cancer Cytopathol. 129(9), 701–718 (2021).
Caputo, A. et al. Real-world experience with the Sydney system on 1458 cases of lymph node fine needle aspiration cytology. Cytopathology 33(2), 166–175 (2022).
Ahuja, S. Categorisation of lymph node aspirates using the proposed Sydney system with assessment of risk of malignancy and diagnostic accuracy. Cytopathology 33(4), 430–438 (2022).
Kanhe, R., Tummidi, S., Kothari, K. & Agnihotri, M. Utility of the proposed Sydney system for classification of Fine-Needle aspiration cytopathology of lymph node: A retrospective study at a tertiary care center. Acta Cytol. 67455–67467 (2023).
Alqaidy, D. & Althomali, H. &Almaghrabi A. Sydney reporting system for lymph node Fine-Needle aspiration and malignancy risk stratification: Is it of clinical value?? Diagnostics 14(16) (2024).
Liang, S., Cozzolino, I., Zeppa, P. & Field, A. S. The Sydney system for lymph node FNA biopsy cytopathology: A detailed analysis of recent publications and meta-analysis and a proposal for the components of an ideal prospective study of a cytopathology reporting system. Cancer Cytopathol. 132(12), 745–756 (2024).
Rubaltelli, L. et al. Sonography of abnormal lymph nodes in vitro: Correlation of sonographic and histologic findings. AJR Am. J. Roentgenol. 155(6), 1241–1244 (1990).
Steinkamp, H. J. et al. Cervical lymphadenopathy: Ratio of long-to short-axis diameter as a predictor of malignancy. Br. J. Radiol. 68(807), 266–270 (1995).
Takashima, S. et al. Nonpalpable lymph nodes of the neck: Assessment with US and US-Guided fine-needle aspiration biopsy. J. Clin. Ultrasound 25(6), 283–292 (1997).
Wu, C. H., Hsu, M. M., Chang, Y. & L.&Hsieh, F. J. Vascular pathology of malignant cervical lymphadenopathy—Qualitative and quantitative assessment with power doppler ultrasound. Cancer 83(6), 1189–1196 (1998).
Bhatia, K. S. et al. Real-time qualitative ultrasound elastography of cervical lymph nodes in routine clinical practice: Interobserver agreement and correlation with malignancy. Ultrasound Med. Biol. 36(12), 1990–1997 (2010).
Robert, A. S. & Saldanha, C. An approach to classification and reporting lymph node cytopathology using Sydney system and evaluating the likelihood of malignancy. Biomedicines 43(2), 701–705 (2023).
Torres Rivas, H. E. et al. Ultrasound-Guided Fine-Needle aspiration of superficial lymphadenopathy performed by interventional pathologists: The applicability of the Sydney system from 2 years of experience and 363 cases. Acta Cytol. 65(6), 453–462 (2021).
Balasubramanian, N. B., Shanmugasundaram, S. & Sundari Amirthakatesan, A. The application of the proposed Sydney system for reporting lymph node cytopathology: A five year experience of an academic institution in South India. Acta Cytol. (2023).
Ton Eryilmaz, O., Ucak, R. & Ozagari, A. A. & Kabukcuoglu F. Diagnostic value of lymph node fine-needle aspiration cytology. CytoJournal 188 (2021).
Caputo, A. et al. Digital examination of lymph node cytopathology using the Sydney system (DELYCYUS). An international, multi-institutional study. Cancer Cytopathol. (2023).
Chan, J. Y., Chan, R. C., Chow, V. L., To, V. S. & Wei W. I. Efficacy of fine-needle aspiration in diagnosing cervical nodal metastasis from nasopharyngeal carcinoma after radiotherapy. Laryngoscope 123(1), 134–139 (2013).
Lo, W. C. et al. The effect of radiotherapy on ultrasound-Guided fine needle aspiration biopsy and the ultrasound characteristics of neck lymph nodes in oral cancer patients after primary treatment. PLoS One 11(3), e0149346 (2016).
Brown Jr, J. J. Management of the neck in nasopharyngeal carcinoma (NPC). Otolaryngol. Clin. North. Am. 31(5), 785–802 (1998).
Costantino, A. et al. Accuracy of fine-needle aspiration cytology in detecting cervical node metastasis after radiotherapy: Systematic review and meta-analysis. Head Neck 43(3), 987–996 (2021).
Ronchi, A. et al. Diagnosis of anaplastic large cell lymphoma on late peri-implant breast Seroma: Management of cytological sample by an integrated approach. Cytopathology 29(3), 294–299 (2018).
Acknowledgements
This work was supported by the Far Eastern Memorial Hospital and Fu Jen Catholic University Joint Research Program (111-FEMH-FJU-05) and grants from the Far Eastern Memorial Hospital and Yuan Ze University Joint Research Program (FEMH-YZU-2020-018).
Funding
This work was supported by the grants from National Science and Technology Council (NSTC 112-2314-B-418-004), Far Eastern Memorial Hospital (FEMH 112-2314-B-418-004) and Far Eastern Memorial Hospital and Yuan Ze University Joint Research Program (FEMH-YZU-2023-021).
Author information
Authors and Affiliations
Contributions
Conception and design: L.L.J. and H.W.L. Analysis: L.L.J., H.W.L. Interpretation of data: L.L.J., W.C.H., C.P.C., L.W.C., C.C.M., W.M.H., and H.W.L. Drafting of the manuscript: L.L.J. Revising: L.L.J., W.C.H., C.P.C., L.W.C., C.C.M., W.M.H., and H.W.L. Final approval of the version to be published. L.L.J., W.C.H., C.P.C., L.W.C., C.C.M., W.M.H., and H.W.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
All patients signed written informed consent forms.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liao, LJ., Wu, CH., Cheng, PC. et al. Utility of Sydney system for reporting the neck lymphadenopathy underwent real-time ultrasound guided fine-needle aspiration. Sci Rep 15, 9724 (2025). https://doi.org/10.1038/s41598-025-93330-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93330-9