Abstract
The current treatments for diabetic macular edema (DME) include laser, steroids or vascular endothelial growth factors inhibitors (antiVEGF). Some DME are resistant to these treatments, which can respond to somatostatin inhibitors such as lanreotide. These drugs appear to influence the development of diabetic retinopathy (DR) and DME either through a direct antiVEGF effect or through the inhibition of growth hormone (GH), endothelial cell apoptosis and anti-inflammatory effect. It was conducted a study of the effects of lanreotide in retinal pigment epithelial cell cultures and a clinical study in patients with DME resistant to conventional treatments in order to better understand the usefulness of this drug. Lanreotide showed antiapoptotic effects and significantly improved visual acuity. Lanreotide could be applied in non-respondent patients to other treatments as an alternative in refractory DME patients.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is one of the main complications of diabetes mellitus (DM) and the major cause of blindness in the developed countries1. Diabetic retinopathy leads to 12% of new cases of blindness each year1. The two clinical entities which are going to determine the visual prognosis of DR patients are the Proliferative Diabetic Retinopathy (PDR) and Diabetic Macular Edema (DME), which could lead to a significant vision loss2. Laser photocoagulation, intraocular steroids and anti-vascular endothelial grow factors (antiVEGF) are the common treatment of DME. Vitrectomy might be also recommended especially in treatment resistant DME or DME coexisting with Epiretinal Membrane (ERM). Nevertheless, there are some diabetic patients who do not respond to conventional therapy, so they end up developing a persistent DME3.
Somatostatin and its analogues have been suggested as candidates for developing novel therapies for DR. Thus, the relationship between growth hormone inhibition and improvement of diabetic retinopathy has been reported2,4. Somatostatin may perform its antiangiogenic effects, both through antagonism of the growth hormone (GH) and through direct anti-proliferative and antiapoptotic effects on endothelial cells. It also regulates the fluid and ions transport through the retinal pigment epithelium (RPE) receptors and has an antiinflammatory and neuroprotective action. Nevertheless, the effect on cellular apoptosis is not clear5.
Somatostatin analogues have shown promising results in the treatment of DME2. Thus, the aim of this work was to examine the effectiveness of a new prolonged lanreotide formulation, which has a more comfortable dosage for the patient compared to the predecessor octreotide (was administered as a continuous infusion pump or 3 times/day subcutaneously), in order to improve clinical prognosis of patients with persistent DME, as well as to modulate apoptosis and oxidative stress-induced apoptosis in diabetic cells6.
Materials and methods
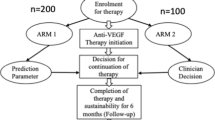
We have carried out two studies: (a) experimental study to determine the antiapoptotic effect of lanreotide on retinal pigment epithelium cells in culture, and (b) clinical study to determine the effectiveness of lanreotide in patients with refractory DME to standard treatments.
Ethical concerns
The study was conducted according to the guidelines of the Declaration of Helsinki7 and approved by the Ethics Committee of FISABIO Eye Clinic (Valencia, Spain) (procedure number: 151008). Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to participate in this study.
Cell culture
Retinal pigment epithelium (ARPE-19) human cells were used from the ARPE-19 cell line (ATCC, number CRL-2302), which were obtained from LGC Promochem Standards. Cells were cultured as previously described by Dunn and collaborators8 and were used after 20 passages and cultured to 85% confluence in p100 culture well plates at a seeding high density of 200,000-582,500 cells/cm2. The cultures were exposed to a selective medium with high (45mM) or low concentration (5mM) of glucose during 7 days in order to create diabetic and control groups. This laboratory model was used, based on published experience using ARPE-19 cells exposed to hyperglycemia, to evaluate metabolic and preventive effects on the alteration of oxidative stress in the RPE. Although cell culture does not reach the complexity of the disease in humans, it allows to obtain data that can guide us in the better understanding of the pathophysiological processes of the disease9.
The treatment with lanreotide (Somatuline Autogel®) was started at a concentration of 1/1000 in some cultures in order to establish the final 4 groups: group 1: not treated controls (C); group 2: controls treated with lanreotide (C + L); group 3: non treated diabetic cultures (D); group 4: diabetic cultures treated with lanreotide (D + L). A sample was taken at 24 h (when the effect was maximum for that concentration) in order to perform the histochemical analysis. Samples were prepared and embedded in paraffin and cut at 3–5 μm thickness.
Biochemical analysis
By immunohistochemical analysis, an angiogenesis marker (VEGF), apoptosis marker (Caspase-3) and oxidative stress-induced apoptosis marker (JNK) were analyzed in all samples. These samples were dewaxed in xylene and then dehydrated in graded alcohols and finally washed in 0.01 M phosphate-buffered saline (PBS) in a pH between 7.2 and 7.4. Endogenous peroxidase was blocked with hydrogen peroxide 0.3% in absolute methanol for 30 min. The immunohistochemical analysis (streptavidin biotin-peroxidase method) for the detection of caspase-3, VEGF and JNK was used. Primary antibodies were diluted in PBS (VEGF 1:100; JNK 1:100; caspase-3 1:50) and applied overnight at 4 °C. After 4 washes in PBS, Ultravision ONE HRP Polymer (Thermo Scientific, Cheshire, England) was applied for 30 min at room temperature. After 4 more washes, 40 µl of DAB Plus Chromogen and 2 mL of DAB Plus Substrate (Thermo Scientific, Cheshire, England) were applied for 10 min at room temperature. After 4 washes with distilled water the samples were dehydrated and washed with xylene. The samples were photographed with a digital Olympus OM101 camera applied to a Leica DM5000B microscope.
Clinical study
A one-year non-controlled prospective follow-up study was performed. Patients over 18 year of age and type II DM that were treated at FISABIO Eye Clinic (Valencia, Spain) for persistent DME were recruited. Persistent DME was defined as having at least one eye with clinically significant DME (thickening of the retina at or within 500 μm of the center of the macula there was no minimum macular thickness for inclusion) that did not respond to regular treatment (treatment with more than 12 months intravitreal injections of antiVEGF -at least 6- and/or intraocular steroids. All eyes had been previously treated with the treatments considered first choice: laser photocoagulation, intravitreal injections of anti-VEGF and corticosteroids in antiVEGF resistant cases at least during one year. As antiVEGF we used bevacizumab as a first choice (at that time it was the available one for DME in our center) we used intravitreal triamcinolone as CTT. Three eyes had also undergone vitrectomy and removal of tractional membranes on the macular surface, being the macular edema refractory to all the treatments mentioned above.
Excluded patients were those treated with another somatostatin analogue, gall bladder disease, high cardiovascular risk, renal insufficiency and/or severe liver disease. Pregnant women and patients with cataract surgery 3 months before the present study, posterior subcapsular cataract (LOCS > II-III) or macular ischemia (foveal avascular zone-FAZ > 50% measured in fluorescein angiography) were also excluded. A sample of 32 eyes of 18 patients was studied. Enrolled patients were treated with a subcutaneous injection of 90 mg of a new prolonged lanreotide formulation (SomatulineAutogel®, Ipsen Pharma S.A., Barcelona, Spain), every 4 weeks during 12 consecutive months.
At baseline, each patient had a medical exam that gathered information on medical history, DM and glycemic control, blood pressure, renal function and lipid profile. Ocular examination included slit-lamp biomicroscopy, lens status, best-corrected visual acuity (VA) and central macular thickness and volume (Cirrus OCT® macular cube 512 × 128 and Five Line Raster, from here we obtain the central macular thickness and macular volume, and Stratus OCT® Fast Macular Thickness Map: foveolar volume and macular volume and 6 mm Cross Hair San for average foveolar thickness). VA was measured by means of the Early Treatment Diabetic Retinopathy Study (ETDRS) scale10. Pattern and multifocal electroretinogram (Roland Consult® software RETIscan 3.20/RETIport 32, Ganzfeld Q450HF, 20 inches monitor CRC de SONY® CPDE530) was performed to asses electrophysiological changes. These measurements were repeated at 3, 6 and 12 months after treatment. Information on adverse effects was collected throughout all examinations at 1, 2, 3, 6 and 12 months.
The assessment of the impact of VA on quality of life was done using the Visual Function-VF 14 Questionnaire at baseline and at the end of the study11. Central macular thickness and macular volume were documented using Optical Coherence Tomography (OCT) using Cirrus-OCT (Carl Zeiss Meditec S.A., Spain).
It was recorded also arterial blood pressure and blood and urine test analysis for determination of glycaemia, glycosylated hemoglobin, cholesterol, triglycerides, insulinemia, urine albumin and creatinine.
Statistical analysis
All data were given as mean ± SE. One-way analysis of variance, ANOVA, was performed for inter group comparisons and false discovery rate-adjusted P-value < 0.05. Brown-Forsythe test produced the ANOVA data which was run by the Tukey test whenever data were homogeneous (p < 0.05) as a post hoc procedure or whenever variances differed by Dunnett T3 test. Statistical significance was set at P < 0.05. GraphPad Prism version 7.04 for Windows (GraphPad Software, La Jolla, CA, USA) was used to carry out the statistical analysis along with SPSS v24 statistical package (IBM SPSS Statistics for Windows, Armonk, NY, USA). We did not address the intereye correlations if both eyes were used in a patient. This is because in the design of the study, each eye was considered independent since each eye started from a different condition and therefore the behavior would also be different.
Results
Experimental studies
Regulation of VEGF
The treatment of the diabetic cells of ARPE-19 line with lanreotide reduced in a significant manner the expression of VEGF from 94.14 ± 6.10 to 80.59 ± 2.98 (Fig. 1). The samples of diabetic cultures had a significant higher proportion of positive cells to VEGF (p = 0.009) than the control ones, suggesting the implication of VEGF in the pathogenesis of DR. IN the samples treated with lanreotide the expression of VEGF decreased (p = 0.007) and that expression was similar in diabetic cells treated with lanreotide and the control ones. There were no differences in the expression of VEGF in diabetic cells treated with lanreotide and the controls (Fig. 1).
Immunohistochemical staining (A) Analysis with VEGF marker to validate the angiogenic response. The cells which are stained in brown indicate positivity for VEGF. (B) Expression of the angiogenesis marker VEGF. (C) Analysis with Caspase-3 marker to validate the antiapoptotic response. The cells which are stained in brown indicate positivity for Caspase-3. (D) Expression of the apoptotic marker Caspase-3 in each one of the four groups. (E) Analysis with JNK marker to validate the oxidative stress response. The cells which are stained in brown indicate positivity for JNK. (F) Expression of the oxidative stress marker JNK in each one of the four groups. *p < 0.05 C: control; D: diabetic; C + L: Control + lanreotide; D + L: Diabetic + lanreotide.
Regulation of apoptosis
The treatment of the diabetic cells of ARPE-19 line with lanreotide reduced in a significant manner the expression of Caspase-3 from 77.15 ± 12.48 to 47.39 ± 11.91 (Fig. 2). The results for Caspase-3 were similar to the ones for VEGF. The samples of diabetic cells had a significant higher proportion of positive cells to Caspase-3 (p = 0.032) than the control ones. In the samples treated with lanreotide the expression of Caspase-3 decreased (p = 0.013) and that expression was similar in diabetic cells treated with lanreotide and the control ones, showing a protective role of lanreotide against apoptosis of diabetic ARPE-19 cells mediated through the Caspase-3 pathway (Fig. 1).
Regulation of oxidative stress-induced apoptosis
The treatment of the diabetic cells of ARPE-19 line with lanreotide reduced in a significant manner the expression of JNK from 55.49 ± 4.81 to 35.76 ± 6.17 (Fig. 1). The results for JNK were similar to the ones for VEGF and Caspase-3. The samples of diabetic cells had a significant higher proportion of positive cells to JNK (p = 0.0006) than the control ones. In the samples treated with lanreotide the expression of JNK decreased (p = 0.002) and that expression was similar in diabetic cells treated with lanreotide and the control ones and thus it could be proposed that cellular apoptosis caused by oxidative stress measured through the JNK pathway decreases significantly with the administration of lanreotide (Fig. 1).
Correlations
When the levels of the different studied markers were correlated in the diabetic and control cultures there is a significant direct relation between the reduction of the levels of JNK and the reduction of the levels of VEGF (r = 0.590; p = 0.016) (Fig. 3), and so the decrease of VEGF due to the action on lanreotide could be explained with the decrease of JNK. Positive significant relations between the levels of VEGF and Caspase-3 (r = 0.558; p = 0.025) and between Caspase-3 and JNK (r = 0.544; p = 0.029) were also found (Fig. 2).
Clinical studies
18 patients who met the inclusion criteria were included. Five of them dropped out of the study before the year and were totally excluded due to undesirable digestive effects of the drug. A total of 13 completed the study, 9 men and 4 women with a mean age of 63.2 years (range 48–81).
All patients had type II diabetes except for one who had type I diabetes. The time of evolution of diabetes was 17.8 years on average (standard deviation 10.2, median 17).
Non proliferative diabetic retinopathy (NPDR) was present in 85% eyes (15% severe and 70% moderate). The other 15% had proliferative diabetic retinopathy (PDR). Initial average macular thickness (Cirrus) was 478.12 μm ± 158.41 μm. The previous treatments that the patients received were laser, anti-VEGF and intravitreal corticosteroids. Three eyes had vitrectomy and membrane peeling prior lanreotide treatment.
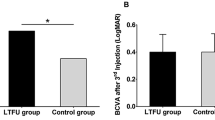
Visual improvement
VA significantly improved (p = 0.002). The improvement was on average of 8.62 letters (± 13.07), with a range of -21 to + 43 letters (Fig. 4). If the results are divided into intervals, 50% (13 eyes) improved more than 10 letters and 26.92% (7 eyes) more than 15 letters. On the other hand, 3.85% (1 eye) lostmore than 15 letters because of persistent macular edema, 15.38% (4 eyes) lose 10 letters or less and 3.85% (1 eye) remained the same. Most eyes improved their VA with treatment.
Visual and anatomical improvements. (A) Average VA in the number of letters read at a distance of 4 m (ETDRS scale) from baseline to end of study at 12 months. (B) Evolution of the average central macular thickness from baseline to end of study at 12 months (*p < 0.05). (C) Variation in the central macular thickness from baseline to end of study at 12 months.
Anatomical improvement
There is a statistical significant decrease in central macular thickness (p = 0.001) (Fig. 4). There is a progressive improvement till the sixth month and then a stabilization and no high differences between months 6 and 12 could be observed (Fig. 4).
The average decrease is of -106 μm (± 158.2) (Fig. 4).
The macular edema decreased in the majority of the eyes.
There was progressive improvement in both macular edema and Best Corrected Visual Acuity at 12 months. The average letter improvement was 8.62 letters and the average macular thickness decrease was about 93 microns. It must be considered that these were patients with DME refractory to all the usual treatments, so although the results are relatively modest, the importance of these results lies in the fact that they had not responded before.
In the macular volume, the results are similar. There is an average decrease of -1.25mm3 (± 2.10) which was statistical significant (p = 0.001).
Electrophysiological changes
There are no significant changes in the latency (p = 0.489) and amplitude (p = 0.317) of the response, even though there is a weak decrease in latency and a weak increase in the amplitude of the response between the basal visit and after 12 months of lanreotide treatment in patients with DME (Table 1).
There were no significant changes in latency and amplitude of response measured by ERG-Pattern after 12 months of lanreotide treatment. In the multifocal ERG, no statistically significant differences were found before and after lanreotide treatment for any of the measurements. Only the increases in rings 2 and 3 with p-values around 0.1 suggest a weak tendency to increase with treatment.
Biochemical changes
There is a statistically significant decrease in total cholesterol (p = 0.019), triglycerides (p = 0.010) and albuminuria (p = 0.021) between the first and the last visit in patients with DME under lanreotide treatment (Fig. 3).
Specific questionnaire of visual function VF-14
There are no significant differences in the global grading of the questionnaire before and after the treatment (baseline 40.41 ± 20.39 and 12 months 44.5 ± 19 mean ± standard deviation). Seven patients improved it, one remained the same and five had lower grading. There was a significant improvement in items 5 (see a stair step and sidewalk step) with p = 0.045 and item 8 (do crosswords, fill in a form or do a soccer pool) with p = 0.041. There was a tendency to improve in item 7 (fine crafts) with p = 0.053. Inability to perform certain tasks decreases with treatment.
The global perception of the patient with respect to the visual function has not changed in a significant manner after the treatment with lanreotide, but it has changed for certain tasks.
Adverse effects
There were local adverse effects in 4 patients, but had a tendency to decrease over time, and disappeared at 6 months after starting the treatment (Table 2). There were 13 patients with systemic adverse effects, but tolerance improved with time and the adverse effects decreased. After one year of treatment 77% of patients reported no systemic adverse effects. Five patients abandoned the treatment, two of them due to adverse gastrointestinal effects and three patients due to concomitant pathologies like pericarditis, a bone fracture and coronary artery bypass surgery (Table 2).
Discussion
During almost thirty years, the treatment with focal laser was considered the treatment of choice for the clinically significant macular edema. Nevertheless, its effect is limited because it only stabilizes visual acuity in 50% of the patients and improve it in only 10% of them12. During the last decades, other treatments have been introduced as the intra-vitreous corticosteroids or anti-VEGF in order to stabilize and recover the lost visual acuity in patients with DME. The applications of these treatments have greatly improved the prognosis of DME. However, certain percentage of patients continue to develop an extensive loss of visual acuity2,3.
The association between GH and DR has led to the study of somatostatin analogues4. Several studies have shown the efficacy of these drugs in the treatment of PDR and DME, being the octreotide the most common one2,13,14. The mechanisms through which somatostatin could work in DR, besides inhibiting GH, is consequently inhibiting proangiogenic factors like insulin-like growth factor (IGF), VEGF, basic fibroblastic growth factor (bFGF), endothelial growth factor (EGF) and platelet-derived growth factor (PDGF).
In the last twenty years, the study of oxidative stress-induced apoptosis has gained more popularity because it was described as the initial stimulus which brings about the rest of the pathways implicated in the ethiopathogenesis of DR15,16. Thus, working through treatments which modulate oxidative stress-induced apoptosis, we could potentially act on the rest of the pathways involved in the DR pathogeny. Besides in some animal models, the good glycemic control does not change the pathological effects after hyperglycemia, demonstrating the concept of “metabolic memory”6. This shows that the cellular damage persists after hyperglycemic crisis due to the fact that all the damaged molecules have not disappeared. The implication of oxidative stress-induced apoptosis in the development of DR could be the basis for the phenomenon of “metabolic memory”17. And so, one of the most promising lines of research on protection against vascular damage in the diabetic person is the control of free radical generation.
Our study is the first one with lanreotide in human ARPE-19 cells. There are few studies on the regulation of apoptosis of RPE in DR. The majority of the studies are performed in neural and vascular cells. RPE is vital in the survival of the neuroretina and so in the VA. Carrasco and coworkers already suggested that the apoptosis in RPE could be higher than in the neuroretina18. There is a real need to explore the apoptosis of RPE in DR19. In the retina, somatostatin is produced by the healthy RPE and somatostatin receptors are expressed at the apical site of the RPE and the neuroretina. Damage of the RPE cells is involved in other types of macular edema, such as that associated with retinitis pigmentosa20. Given the important role played by the RPE in the maintenance of neuroretina, we believed that it was important to determine not only the beneficial role of lanreotide in improving DME, but also to assess the possible addition of the anti-apoptotic effect that seems to benefit the maintenance of RPE cells.
Cellular apoptosis of RPE in diabetic patients produce an increase in Caspase-3 so there is higher apoptosis of RPE in diabetic patients. These are similar to the studies performed before in which apoptosis in different layers of the retina and in endothelial cells. The increase of apoptosis in these cells could damage the rest of the retina and hence the progression of DR given the importance of RPE for the survival of the neuroretina. Lanreotide decreases the expression of Caspase-3 and the levels of Caspase-3 in diabetics treated with it are similar to the non-diabetic controls, and this is shown in rats21. In some studies, it is not clear whether lanreotide has proapoptotic or antiapoptotic functions. The fact that protects against apoptosis could be a possible mechanism of action explaining its efficacy in treating DR. Simó and coworkers19 described that low levels of somatostatin increases the apoptotic process. At the same time, administration of somatostatin decreases apoptosis in all the layers of the retina.
Regarding oxidative stress-induced apoptosis, there is an increase of JNK in diabetic patients. There is obviously more cellular damage in these patients. Lanreotide decreases de expression of JNK so there is less apoptosis caused by oxidative stress.
There are positive correlations between these markers: VEGF, oxidative stress and apoptosis. There are some studies which show some of these features, like the causal relationship between oxidative stress-induced apoptosis and the expression of VEGF22, relationship between JNK, VEGF and angiogenesis23, relationship between JNK and cellular apoptosis24.
In DR, there is a clear clinical efficacy of long-acting somatostatin analogues because it was shown that it reduces the progression of the disease as it was used in severe non-proliferative and early proliferative DR5, and in the regression of ocular neovasculatization and preventing the worsening of preexisting retinal neurodysfunction25.
In some studies of refractory DME, there has been described anatomical improvement in the macular thickness without improvement in visual acuity in only three patients14 In our clinical study the treatment of lanreotide in patients with persistent DME has been effective regarding the visual and anatomical results, being significant the improvement of visual acuity in a progressive manner, and the reduction of central macular thickness and macular volume after twelve months of administering the drug. Besides, the study of the subjective visual function with VF14 improves in certain tasks. Our study included patients with chronic refractory DME who have lower initial levels of visual acuity. There are studies with more than three years of duration and a progressive increase has been shown year after year26,27.
Lanreotide significantly reduces the DME. If there is a stabilization of the DME at the 6th month of treatment but a continuous increase in visual acuity this has to be due to improvements at the cellular level of the antiapoptotic effect of the drug. The values are lower than in other studies because ours were cases of persistent ME, and there are variations in the OCTs used, duration of ME and previous treatments27.
The clinical efficacy of lanreotide can be shown in the ERG as well. There are several studies in the literature that describe increases in the Pattern ERG P50 amplitude and central responses in ERG Multifocal after Ranibizumab, Bevacizumab or laser treatment28,29,30. There is a lack of prospective studies with a higher number of patients. There is a weak tendency to increased amplitude in rings 2 and 3, the central ones, in Multifocal ERG which would improve the central visual function, but a higher sample is required to see whether statistical significance is obtained.
There is a significant decrease in total cholesterol, triglycerides and proteinuria and a tendency to a decrease in diastolic arterial pressure. This is connected with the relationship between serum lipids like cholesterol and triglycerides with the severity of DME, especially in the area of hard exudates31,32. There is a relationship of proteinuria and diastolic arterial pressure with the severity of exudates33. There is a tendency to increase in glycosylated hemoglobin (see supplementary material) and lanreotide inhibits the secretion of insulin and glucagon which are involved in the possible changes of glycemic control. There is a need to monitor glycaemia more strictly at the beginning of the treatment.
There is a good tolerance to lanreotide in acromegaly studies34. The adverse effects are frequently gastrointestinal ones, erythema or induration at injection site but these effects are weak, moderate and transitory35,36. The common adverse effects of diarrhea and meteorism have led to two patients to leave our study. But there is a progressive decrease of adverse effects during the time of the study.
The shortcomings of the present study are that, in the experimental work, the number of oxidative stress-induced apoptosis markers is limited, and the clinical work has a small sample and lacks control group. Thus, the future lines of research would be to study the effect of lanreotide on other oxidative stress-induced apoptosis markers, pursue other dosage intervals and routes of administration like through the skin or intravitreal injections.
Conclusions
Lanreotide, despite having a certain percentage of adverse effects that would limit its widespread use as a first line treatment, seems to be useful as a treatment of refractory DME patients (those with absence of retinal thickness reduction (> 50) and changes in corrected visual acuity of less than 5 letters). Also, it can be used as an alternative to the first order treatments. It has affordable adverse effects as the administration is more comfortable for the patients than other somatostatin analogues.
Data availability
All data generated or analyzed during this study are included in this article.
References
Yin Wong, T. & Tan, T-E. The diabetic retinopathy pandemic and evolving global strategies: The 2023 Friedenwald lecture. Invest. Ophthalmol. Vis. Sci. 64, 47. https://doi.org/10.1167/iovs.64.15.47 (2023).
Gomes-Porras, M., Cárdenas-Salas, J. & Alvarez-Escolá, C. Somatostatin analogs in clinical practice: A review. Int. J. Mol. Sci. 21, 1682. https://doi.org/10.3390/ijms21051682 (2020).
Giuliari, G. P. Diabetic retinopathy: Current and new treatment options. Curr. Diabetes Rev. 8, 32–41 (2012).
Yuno, A. et al. Advanced proliferative diabetic retinopathy and macular edema in acromegaly: A case report and literature review. Diabetol. Int. 13, 575–579. https://doi.org/10.1007/s13340-022-00571-4 (2022).
Amato, R. et al. Association of the somatostatin analog octreotide with magnetic nanoparticles for intraocular delivery: A possible approach for the treatment of diabetic retinopathy. Front. Bioeng. Biotechnol. 8, 144. https://doi.org/10.3389/fbioe.2020.00144 (2020).
Yang, T. et al. An update on chronic complications of diabetes mellitus: From molecular mechanisms to therapeutic strategies with a focus on metabolic memory. Mol. Med. 30, 71. https://doi.org/10.1186/s10020-024-00824-9 (2024).
World Medical, A. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310, 2191–2194 (2013).
Dunn, K. C., Aotaki-Keen, A. E., Putkey, F. R. & Hjelmeland, L. M. ARPE-19, a human retinal pigment epithelial cell line with differentiated properties. Exp. Eye Res. 62, 155–169 (1996).
Bardak, H. et al. Selenium protects ARPE-19 and ACBRI 181 cells against high glucose-induced oxidative stress. Molecules 28, 5961. https://doi.org/10.3390/molecules28165961 (2023).
Ferris, F., Kassoff, A., Bresnick, G. & Bailey, I. New visual acuity charts for clinical research. Am. J. Ophthalmol. 94, 91–96 (1982).
Steinberg, E. P. et al. The VF-14: An index of functional impairment in patients with cataract. Arch. Ophthalmol. 112, 630–638 (1994).
Bakri, S. J., Wolfe, J. D., Regillo, C. D., Flynn, H. W. Jr & Wykoff, C. C. Evidence-based guidelines for management of diabetic macular edema. J Vitreoretin Dis. 3, 3 (2019). https://doi.org/10.1177/24741264198347111796-1806
Choi, M. Y., Jee, D. & Kwon, J. W. Characteristics of diabetic macular edema patients refractory to anti-VEGF treatments and a dexamethasone implant. PLoS ONE. 14, e0222364. https://doi.org/10.1371/journal.pone.0222364 (2019).
Hernaez-Ortega, M. C., Soto-Pedre, E. & Piniés, J. A. Lanreotide autogel for persistent diabetic macular edema. Diabetes Res. Clin. Pract. 80 (e8-10). https://doi.org/10.1016/j.diabres.2008.02.007 (2008).
Lacobini, C., Vitale, M., Pesce, C., Pugliese, G. & Menini, S. Diabetic complications and oxidative stress: A 20-Year voyage back in time and back to the future. Antioxidants 10 (727). https://doi.org/10.3390/antiox10050727 (2021).
Evans, J. L., Goldfine, I. D., Maddux, B. A. & Grodsky, G. M. Oxidative stress and stress-Activated signaling pathways: A unifying hypothesis of type 2 diabetes. Endocr. Rev. 23, 599–622. https://doi.org/10.1210/er.2001-0039 (2002).
Williams, M., Hogg, R. E. & Chakravarthy, U. Antioxidants and diabetic retinopathy. Curr. Diab Rep. 13, 481–487 (2013).
Carrasco, E. et al. Lower somatostatin expression is an early event in diabetic retinopathy and is associated with retinal neurodegeneration. Diabetes Care. 30, 2902–2908 (2007).
Simó, R., Villarroel, M., Corraliza, L., Hernández, C. & Garcia-Ramírez, M. The retinal pigment epithelium: Something more than a constituent of the blood-retinal barrier–implications for the pathogenesis of diabetic retinopathy. J Biomed. Biotechnol. 190724; (2010). https://doi.org/10.1155/2010/190724 (2010).
Heutinck, P. A. T. et al. Somatostatin analogues as a treatment option for cystoid maculopathy in retinitis pigmentosa. BMJ Open. Ophthalmol. 9, e001722. https://doi.org/10.1136/bmjophth-2024-001722 (2024).
Hernández, C. et al. Topical administration of somatostatin prevents retinal neurodegeneration in experimental diabetes. Diabetes 62, 2569–2578 (2013).
Hsueh, Y-J. et al. The pathomechanism, antioxidant biomarkers, and treatment of oxidative stress-related eye diseases. Int. J. Mol. Sci. 23, 1255. https://doi.org/10.3390/ijms23031255 (2022).
Guma, M. et al. Genetic and Pharmacological Inhibition of JNK ameliorates hypoxia-induced retinopathy through interference with VEGF expression. Proc. Natl. Acad. Sci. U. S. A. 106, 8760–8765 (2009).
Du, H. et al. JNK Inhibition reduces apoptosis and neovascularization in a murine model of age-related macular degeneration. Proc. Natl. Acad. Sci. U. S. A. 110, 2377–2382 (2013).
Simó, R. et al. Effects of topically administered neuroprotective drugs in early stages of diabetic retinopathy: Results of the EUROCONDOR clinical trial. Diabetes 68, 457–463. https://doi.org/10.2337/db18-0682 (2019).
Pearson, P. A. et al. Fluocinolone acetonide intravitreal implant for diabetic macular edema: A 3-year multicenter, randomized, controlled clinical trial. Ophthalmology 118, 1580–1587 (2011).
Cunha-Vaz, J. et al. Sustained delivery Fluocinolone acetonide vitreous implants: Long-term benefit in patients with chronic diabetic macular edema. Ophthalmology 121, 1892–1903 (2014).
Comyn, O. et al. A randomized trial to assess functional and structural effects of Ranibizumab versus laser in diabetic macular edema (the LUCIDATE study). Am. J. Ophthalmol. 157, 960–970 (2014).
Ozkiriş, A. Pattern electroretinogram changes after intravitreal bevacizumab injection for diabetic macular edema. Doc. Ophthalmol. 120, 243–250 (2010).
Lövestam-Adrian, M. & Holm, K. Multifocal electroretinography amplitudes increase after photocoagulation in areas with increased retinal thickness and hard exudates. Acta Ophthalmol. 88, 188–192 (2010).
Sasaki, M. et al. Quantitative measurement of hard exudates in patients with diabetes and their associations with serum lipid levels. Invest. Ophthalmol. Vis. Sci. 54, 5544–5550 (2013).
Rao, H., Jalali, J. A., Johnston, T. P. & Koulen, P. Emerging roles of dyslipidemia and hyperglycemia in diabetic retinopathy: Molecular mechanisms and clinical perspectives. Front. Endocrinol. (Lausanne). 12, 620045. https://doi.org/10.3389/fendo.2021.620045 (2021).
Shen, Y., Wang, H., Fang, J., Liu, K. & Xu, X. Novel insights into the mechanisms of hard exudate in diabetic retinopathy: Findings of serum lipidomic and metabolomics profiling. Heliyon 9, e15123. https://doi.org/10.1016/j.heliyon.2023.e15123 (2023).
Yazgan, S., Arpaci, D., Celik, H. U. & Isik, I. Evaluation of macular and peripapillary choroidal thickness, macular volume and retinal nerve fiber layer in acromegaly patients. Int. Ophthalmol. 38, 617–625 (2018).
Burness, C. B., Dhillon, S. & Keam, S. J. Lanreotide autogel(®): A review of its use in the treatment of patients with acromegaly. Drugs 74, 1673–1691 (2014).
Fleseriu, M. Clinical efficacy and safety results for dose escalation of somatostatin receptor ligands in patients with acromegaly: A literature review. Pituitary 14, 184–193 (2011).
Acknowledgements
The authors would like to thank Dr. Enrique Soto for the design of the clinical part of the study and revision of the manuscript. Also, we thank all of our patients for their participation in the study.
Funding
This work was supported by funds from Fundación CEU-Santander INDI20/06.
Author information
Authors and Affiliations
Contributions
Conceptualization, A.N, M.C.H-O. and F.B-M.; methodology, M.C.H-O., A.N., F.B-M.; validation E.P., M.C.H-O. and F.B-M.; investigation E.F-L.; data curation, M.L.M.; writing-original draft preparation, V.M.V and M.L.M; writing-review and editing, F.B-M and M.L.M.; supervision, A.N, M.C.H-O., E.P.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fernandez-Lopez, E., Moreno, M.L., Villar, V.M. et al. Study of the efficacy and the mechanism of action of lanreotide for the treatment of persistent diabetic macular edema. Sci Rep 15, 9157 (2025). https://doi.org/10.1038/s41598-025-93844-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93844-2