Abstract
Obstructive sleep apnea (OSA) is a prevalent sleep disorder characterized by disrupted breathing patterns and dysfunctions in multiple organ systems. Although studies support a close correlation between OSA and immune function, the broader implications and specific manifestations remain unclear. Therefore, it is pressingly needed to identify potential immune-related markers and elucidate underlying immunological mechanisms of OSA. OSA-related datasets (GSE38792) and immune-related genes were downloaded from the GEO and ImmPort databases and intersected to obtain differentially expressed immune-related genes (DEIRGs). GO, KEGG, and GSEA were employed to explore the biological functions of DEIRGs. Immune cells and immune regulation were analyzed by CIBERSORT. The ROC curve was constructed to assess the accuracy of each DEIRG. The co-regulatory networks of transcription factors, microRNAs, and drugs were built using the NetworkAnalyst database and visualized by Cytoscape. The levels of DEIRGs in clinical samples were validated by RT-qPCR. GO, KEGG, and GSEA revealed that DEGs were mainly enriched in negative regulation of immune response and antigen processing and presentation in OSA. IL33, IL10RB, ANGPTL1, EIF2AK2, SEM1, IFNA16, SLC40A1, FCER1G, IL1R1, TNFRSF17, and ERAP2 were identified as DEIRGs among 175 differentially expressed genes in OSA. Memory B cells, mast cells resting, and dendritic cells resting were the predominant immune cells related to DEIRGs. The co-regulatory network contained 128 miRNAs, 40 transcription factors, and 172 drugs/compounds. Finally, IL33, EIF2AK2, IL10RB, and ANGPTL1 were also upregulated in clinical OSA samples. The present study identified potential immune-related biomarkers and systematically elucidated underlying immunological mechanisms of OSA. These findings provide novel insights into the diagnosis, mechanism research, and management strategies for future studies.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA), a prevalent yet frequently underestimated sleep-related breathing disorder, has a prevalence of up to 10% in the general population across all age groups1,2. OSA is characterized by recurrent upper airway obstruction, intermittent hypoxemia, and sleep fragmentation, leading to secondary sympathetic activation, oxidative stress, and systemic inflammation3. Its physiological functions mainly rely on the balance between pro- and anti-inflammatory factors. The progression of OSA often results in a shift towards pro-inflammatory cytokines4, contributing to immune disorder, cellular dysfunction, tissue failure, and developmental retardation, regardless of age5,6. These outcomes are strongly associated with the development of cardiovascular diseases, metabolic disorders, and cognitive dysfunction7,8,9,10.
Intermittent hypoxia (IH) during OSA and its complications can release the overexpression of hypoxia-inducible factor 1-α (HIF-1α), which exerts systemic effects on the immune surveillance system through the regulation of immune cells, immune checkpoint axis, and various immune components, ultimately disrupting the physiological microenvironment across multiple organ systems11,12,13. IH also releases TGFβto establish immunosuppression in the monocytes and natural killer cells of OSA patients14. An immune checkpoint PSGL-1 might cause T-cell dysfunction in OSA patients13. Additionally, in the tumor microenvironment, monocytes of OSA impair cytotoxicity by secreting more HIF-1α. Moreover, both IH and sleep fragmentation induce M2-polarized macrophage infiltration and drive tumor cell proliferation, migration, and invasion15,16. However, although studies support the close correlation between OSA and immune function, the macro cognition and micro manifestation remain unclear. Exploring OSA pathogenesis from an immunological perspective is essential to further understand OSA and provide references for early detection and non-invasive treatment.
Bioinformatics analysis has made great strides and has become an important tool for identifying pathogenic genes17. This study first combined differentially expressed genes (DEGs) of OSA from the gene expression omnibus (GEO) database with immune-related genes (IRGs), immunologic functions, and regulatory networks from public databases. Furthermore, in-depth bioinformatics analysis was employed to uncover OSA-related IRGs and molecular mechanisms, which were then validated in clinical samples. This comprehensive approach sought to preliminarily elucidate the immune immunological mechanisms and clinical implications of OSA, thereby offering valuable insights into OSA management.
Materials and methods
Data source
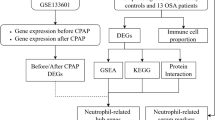
The GSE38792 dataset of gene expression in OSA was downloaded from the GEO database (https://www.ncbi.nlm.nih.gov/geo/) using the R package GEOquery. The GSE38792 dataset is a training dataset with 8 normal samples and 10 OSA visceral fat tissue samples. GPL6244 (Affymetrix Human Gene 1.0 ST Array) is the platform for the GSE38792 dataset. Gene probes were annotated as gene symbols. Probes that did not match gene symbols or matched many symbols were removed. Gene expression of duplicate symbols was calculated at the maximum. Through R packages clusterProfiler, org.Hs.eg.db, enrichplot, and ggplot2, the biological functions of DEGs were determined by Gene Oncology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG), and Gene Set Enrichment Analysis (GSEA)18,19.
ImmPort is a vast open database of subject-level human immunological data that is created to facilitate efficient data sharing among the basic, clinical, and translational research communities. In this paper, information on IRGs was obtained from the ImmPort database (https://www.immport.org/shared/). The workflow is displayed in Fig. 1.
Alteration analysis of IRGs between OSA and control samples
The limma R package was utilized to discern DEGs between OSA and control samples in the GSE38792 dataset, with p value < 0.05 and log2 |fold change (FC)| > 0.5 as the threshold. A Venn diagram was adopted to filter differentially expressed IRGs (DEIRGs) via the intersection of DEGs and IRGs. Through clusterProfiler, org.Hs.eg.db, enrichplot, and ggplot2 packages, the biological functions of DEIRGs were determined through GO and Friends analysis.
Analysis of immune cells and immunity regulation
The CIBERSORT algorithm was utilized for immune infiltration analysis. The corrplot in R was employed for Pearson correlation analysis of infiltrating immune cells and diagnostic genes, and the correlations were visualized with lollipop.
Construction of potential gene regulatory networks
NetworkAnalyst (https://www.networkanalyst.ca/) is a comprehensive website for gene expression analysis for diverse species and meta-analysis. This tool was applied for data collection from the RegNetwork repository to build the networks of transcription factor (TF), microRNA (miRNA), and drug to unveil the regulatory mechanism of DEIRGs at the transcriptional and post-transcriptional level. Moreover, the interaction network was visualized with Cytoscape.
The ROC curve analysis and expression analysis
In the GSE38792 dataset, receiver operating characteristic (ROC) curve analysis was done on each screened hub gene to verify its accuracy using the pROC package. Hub genes with AUC > 0.7 were regarded as having high diagnostic accuracy. The levels of hub genes in OSA and control samples were presented in the boxplots with the ggplot2 package. The functional similarity of genes was analyzed using the GOSemSim package and their correlations were assessed using the corrplot package.
Sample sources for validation
Eight subjects (four OSA patients and four controls) were enrolled at the otolaryngology head and neck surgery department of the Shanghai Sixth People’s Hospital between December 2023 and January 2024. Subjects underwent standard overnight polysomnography before treatment. Four OSA patients were aged over 18 years old, with total sleep duration of > 240 min and an apnea-hypopnea index (AHI) of ≥ 5 events per hour. The other four patients with benign neck mass were selected as controls with AHI < 5 events/h. Both OSA and control groups were matched by sex, age, body mass index, absence of other comorbid sleep disorders (such as insomnia, upper airway resistance syndrome, narcolepsy, or restless legs syndrome), and psychotropic medication. Adipose tissue is a key player in OSA20. Tissue samples in the GSE38792 dataset were obtained from visceral adipose tissue21. To ensure tissue homogeneity and the representativeness of OSA, specimens for validation in this study were specifically collected from soft palate adipose tissue during uvulopalatopharyngoplasty procedures in OSA patients. Additionally, control specimens were obtained from paratracheal adipose tissue during surgical procedures in patients with benign cervical masses. Details of patient data are displayed in Table 1.
RNA isolation and cDNA synthesis
Total RNA was isolated with a Tissue RNA Purification Kit (for adipose tissue) (EZBioscience, Cat.No.: EZB-RN001A) based on the manufacturer’s instructions. Optical densities were tested using a NanoDrop™ One spectrophotometer (Thermo Scientific) to determine the concentration of obtained RNAs. The obtained RNA samples were synthesized into cDNA using a Color Reverse Transcription Kit (EZBioscience, Cat.No.: A0010CGQ) under the following thermal conditions for enzyme inactivation: 42 °C for 15 min and 95 °C for 5 min. The cDNAs obtained were stored at − 20 °C and the remaining RNAs were stored at – 80 °C.
Reverse transcriptionquantitative PCR (RTqPCR)
According to the significant expression of DEIRGs in the GSE38792 dataset, RT-qPCR was performed to verify their expression in OSA and control adipose tissues using LightCycler™ 480 (Roche Applied Science) with the SYBR Green qPCR Mater Mix (ROX2 plus) (EZBioscience, Cat.No.: A0012-R2). RT-qPCR was carried out at 95 °C for 5 min, followed by 40 cycles of 95 °C for 10s and 60 °C for 30s. Primers from the primer bank are listed in Table 2. Expression levels were normalized to PPIA22,23 and computed using the comparative threshold cycle method (2−ΔΔCT).
Statistical analysis
All data were calculated and analyzed using R programming (https://www.r-project.org/, version 4.3.1). Wilcoxon test and Kruskal–Wallis test were adopted to compare subgroup differences. Pearson correlation coefficient was utilized for correlation analysis. GraphPad Prism 9 (La Jolla, CA, USA) and SPSS 26.0 were utilized for statistical analyses. The Shapiro-Wilk normality test and the variance homogeneity test were first performed. Normally distributed continuous variables were compared using an unpaired t-test and non-normally distributed continuous variables were compared using the Mann-Whitney U test. The level of confidence was set at 95%, and P < 0.05 implied statistical significance (ns: no significance, *: p < 0.05, **: p < 0.01, ***: p < 0.001).
Results
Differential gene expression analysis
175 DEGs were obtained from the GSE38792 dataset (Fig. 2A; Supplementary Table 1). To identify DEIRGs, all 1793 IRGs were downloaded from the ImmPort database. Then, IRGs and DEGs were matched and 11 DEIRGs were obtained (Fig. 2B; Supplementary Table 2). In the OSA group, 7 DEIRGs were significantly upregulated and 2 DEIRGs were significantly downregulated compared to the normal group (Fig. 2C, D). In 11 DEIRGs, Pearson correlation analysis showed strong positive correlations between IL33, IL10RB, ANGPTL1, and EIF2AK2 expression (Fig. 2E). Friends analysis revealed that ANGPTL1 had the strongest correlation with other DEIRGs, followed by TNFRSF17, IL10RB, IL1R1, and other hub genes (Fig. 2F). GSEA results revealed that Alzheimer’s disease, antigen processing and presentation, autophagy —animal, cell cycle, and mitophagy–animal and protein processing in endoplasmic reticulum were enriched in the OSA group, while drug metabolism —cytochrome P450 and metabolism of xenobiotics by cytochrome P450 were enriched in the control group (Fig. 2G). GO analysis revealed that DEGs were mainly enriched in endoplasmic reticulum lumen, secretory granule membrane, extracellular matrix, negative regulation of immune response, and immune response—regulating signaling pathway (Fig. 2H). Furthermore, DEIRGs were related to cytokine-mediated signaling pathways, defense response to virus, positive regulation of cytokine production, inflammatory response, adaptive immune response, immune receptor activity, and Epstein-Barr virus infection (Fig. 2I).
Screening DEGs and DEIRGs in OSA. (A) Volcano plot showing DEGs in GSE38792. (B) Venn diagram showed DEIRGs. (C) and (D) Heatmap and differentially expression analysis of 11 DEIRGs in GSE38792. (E) Correlation analysis of DEIRGs. (F) GSEA result of DEIRGs. The enrichment score of curve above 0 points indicates that the gene sets up-regulated, and the curve below 0 points indicates that the gene sets down-regulated. (G) and (H) GO analysis of DEIRGs. (I) Friends analysis of DEIRGs. DEGs, differentially expressed genes; DEIRGs, differentially expressed immune-related genes; OSA, obstructive sleep apnea; GSEA, Gene Set Enrichment Analysis; GO, Gene Oncology; p.adjust, adjusted p-value.
DEIRGs are associated with immune characteristics of OSA
To uncover the biological behaviors of DEIRGs in the immune microenvironment, the correlation of DEIRGs with infiltrating immune cells, immune checkpoints, and human leukocyte antigen (HLA) was analyzed. DEIRGs were closely linked to many immune cells. FCER1G had the most positive correlation with macrophages M2 (p < 0.001), and IL10RB had the most positive correlation with dendritic cells (DCs) resting (p = 0.007); IL33 had the most passive correlation with memory B cell (p = 0.005), and IFNA16 had the most passive correlation with macrophages M2 (p = 0.022) (Fig. 3A). The cell composition of monocytes was greatly lower in the OSA group, profoundly affected by FCER1G and IL10RB expression, and strongly correlated with the function of T cell follicular helper; DCs resting abundance was notably higher in the OSA group, positively correlated with FCER1G, IL33, IL10RB, and strongly associated with the function of memory B cells; mast cells (MCs) resting abundance was markedly higher in the OSA group, positively correlated with ERAP2, EIF2AK2, ANGPTL1, and strongly correlated with the function of eosinophils; macrophages M1 abundance was negatively correlated with IL10RB, IL1R1, EIF2AK2 and SEM1; macrophages M2 abundance was positively linked to FCER1G and negatively linked to IFNA16; both macrophages M1 and M2 were closely related to DCs resting (Fig. 3B, C). Analysis of immune checkpoints showed that LAG3 and PDCD1 were negatively correlated with most DEIRGs, while CD274 was positively correlated with most DEIRGs (Fig. 3D). IFNA16 and TNFRSF17 were negatively correlated with most HLA-related genes. Except for HLA-DOA, EIF2AK2, SLC40A1, IL33, and IL10RB had strongly positive correlations with other HLA-related genes (Fig. 3E). In addition, ERAP2, EIF2AK2, IL33, ANGPTL1, SEM1, IL10RB, FCER1G, and SLC40A1 expression was positively correlated with HLA, para-inflammation, type I interferon (IFN) response, and negatively correlated with the inflammation-promoting, checkpoint, T cell co-stimulation, APC co-stimulation, and CCR (Fig. 3F).
Immune microenvironment of DEIRGs in OSA. (A) Immunocytes related to DEIRGs. (B) Differentially expression of immunocytes in GSE38792 dataset. (C) Correlation analysis between the various immunocyte types in DEIRGs. (D) Correlation between immune checkpoint data and DEIRGs. (E) Correlation between HLA-related genes and DEIRGs. (F) Correlation between immune reaction gene-sets and DEIRGs. DEIRGs, differentially expressed immune-related genes; OSA, obstructive sleep apnea; HLA, human leukocyte antigen.
ROC analysis of DEIRGs
The diagnostic value of 11 DEIRGs was validated via the ROC curve (Fig. 4). The AUC of IL10RB in the GSE38792 was 0.9 (95% CI, 0.7255–1.000), SLC40A1 was 0.9 (95% CI, 0.7584–1.000), IL33 was 0.8375 (95% CI, 0.6224–1.000), EIF2AK2 was 0.825 (95% CI, 0.6306–1.000), TNFRSF17 was 0.825 (95% CI, 0.613–1.000), FCER1G was 0.825 (95% CI, 0.6066–1.000), ANGPTL1 was 0.8125 (95% CI, 0.5794–1.000), SEM1 was 0.7875 (95% CI, 0.5381–1.000), IFNA16 was 0.7875 (95% CI, 0.5713–1.000), IL1R1 was 0.775 (95% CI, 0.5526–1.000), and ERAP2 was 0.775 (95% CI, 0.5255–1.000).
Construction of the related regulatory network
The miRNA, TFs, and drug co-regulatory networks on 11 DEIRGs were identified using the NetworkAnalyst database. Cross-linked miRNAs were selected to ensure the accuracy and stability of the results. The regulatory network contained 128 miRNAs and 10 DEIRGs (Fig. 5A). The drug–gene interaction network contained 172 potential target drugs/compounds and 11 DEIRGs (Fig. 5B). For the TF-DEIRG regulatory network, 40 TFs and 11 DEIRGs were obtained (Fig. 5C).
The regulatory networks of DEIRGs in OSA. (A) The regulatory network of 128 miRNAs and 10 DEIRGs. (B) The regulatory network of 40 TFs and 11 DEIRGs. (C) The drug–gene interaction network of 172 potential target drugs/compounds (represented by ID cord in Comparative Toxicogenomics Database) and 11 DEIRGs. DEIRGs, differentially expressed immune-related genes; OSA, obstructive sleep apnea; miRNA, micro-RNA; TF, transcription factor.
Validation of significant DEIRG expression in clinical samples
No significant differences in sex (2 females and 2 males in each group), age (33.00 ± 8.10 vs. 41.75 ± 12.81, P = 0.437), and body mass index (25.74 ± 4.18 vs. 23.87 ± 1.65, P = 0.292) were found between OSA and control clinical samples. To verify the results of bioinformatics analysis, we performed RT-qPCR in clinical adipose tissue samples. Consistently, IL33, EIF2AK2, IL10RB, and ANGPTL1 were significantly upregulated in the OSA group, while no differences were found in the expression of SEM1, FCER1G, IFNA16, SLC40A1, and TNFRSF17 between the OSA and NOSA groups (Fig. 6).
Discussion
OSA is an intricate systemic disorder characterized by recurrent episodes of total or partial upper airway obstruction during sleep, leading to hypoxemia, hypercapnia, or sleep fragmentation1. It demonstrates strong associations with excessive daytime sleepiness, cardiovascular disease, metabolic disorder, and cognitive dysfunction7,8,9. Due to its increasing incidence and significant limitations in early detection and clinical treatment, OSA has recently garnered considerable attention9. Nevertheless, its pathogenesis has not been fully elucidated.
In the present study, we uncovered 11 DEIRGs using differential expression analysis by intersecting transcriptome data from GEO (GSE38792 dataset) and IRGs from ImmPort. Furthermore, 4 common DEIRGs (IL33, EIF2AK2, IL10RB, and ANGPTL1) were verified in clinical samples.
Interleukin 33 (IL33) is an alarmin cytokine of the interleukin family and is mainly expressed in myofibroblasts, fibroblasts-like cells, epithelial cells, and endothelial cells, with close relations to respiratory diseases24,25. IL33 is produced by adipocytes26 and is substantially higher in adipose tissue of OSA patients, possibly due to IH, leading to systemic inflammation, vascular remodeling, and cognitive dysfunction through the IL-33/ST2, HIF-1α/VEGFA, and NF-κB pathways24,25,27,28. Interleukin 10 (IL10), a potent regulatory cytokine, is essential for maintaining self-tolerance and limiting tissue damage during inflammation29. Deficiencies in IL10 or its receptor correlate with poor immune surveillance30. The single nucleotide polymorphisms of IL10 receptor beta (IL10RB), which is strongly correlated with IL33 in the present study, are associated with ischemic stroke and hypertension31. Additional investigation is necessary for the interaction between IL10RB and IL33.
Eukaryotic translation initiation factor 2 alpha kinase 2 (EIF2AK2) is highly expressed in brain tissue and is a critical protein in fatty acid-induced endoplasmic reticulum stress, which bridges the signals between lipid metabolism and inflammation and modulates multiple signal transduction pathways32,33,34. Angiopoietin-like protein 1 (ANGPTL1) is a member of the ANGPTL family that encompasses a coiled-coil domain and a fibrinogen-like domain and can regulate angiogenesis35. Recent research has highlighted that ANGPTLs are therapeutic targets for cardiovascular, metabolic, and obesity-related diseases36,37. A strong correlation between EIF2AK2 and ANGPTL1 was found in our present study, indicating their potential interactions in OSA. The above 4 DEIRGs simultaneously regulate metabolic homeostasis, vascular stability, and tumorigenesis, which are obvious physiological changes under hypoxia. The pathophysiological mechanisms are worth further investigation.
Our immune filtration analysis investigated OSA-related immune cells and their interactions and unraveled higher DCs/MCs resting abundance and lower monocyte abundance in OSA patients. Systemic hypoxia could maintain inflammation by reducing IFN signaling, thereby suppressing monocyte egress, while overcoming the direct effects of hypoxia on monocyte dynamics could improve outcomes in patients with hypoxic respiratory and cardiovascular injuries38,39. DCs are distributed in lymphoid and extra-lymphoid tissues and sense their surroundings via the membrane and cytoplasmic receptors. Hypoxia inhibits monocyte-derived DC maturation and upregulates chemokine receptor expression40,41. Recent research has elucidated that MCs adapt to long-term hypoxia by stabilizing HIF-1α, increasing MC extracellular traps, and decreasing phagocytic active cells42. However, higher CD8 + T cells and macrophages M2, and lower memory B cells and plasma cells were observed in OSA patients. Consistently, previous findings stated that a hypoxic burden on such IRGs might lead to alterations in metabolic substrates, local inflammatory molecules, hormones, mechanical stretch, and hypoxia-induced pathways, potentially contributing to metabolic and vascular damage on the target organ43,44,45. Although the therapeutic medicines for OSA remain unclear, drug targets based on DEIRGs may theoretically prevent OSA complications. HLA, positively related to most DEIRGs, is the expression product of the human major histocompatibility complex (MHC). MHC genes exhibit complex polygenic structures, high polymorphisms, and sensitivity to oxygen content46. Adequate evidence reveals the correlation between hypoxia and MHC, especially in tumor progression47,48. Additionally, IH in OSA upregulates the programed cell death 1 (PDCD1) ligand/receptor crosstalk and reduces CD8 + T-cell activation and cytotoxicity, thus increasing tumor incidence and aggressiveness and the risk of infections in these patients49.
Apart from IRGs, we also explored miRNAs and TFs on DEIRGs. miRNAs are short non-coding RNAs that control gene expression post-transcriptionally, while TFs represent the central hub of multiple pathways in eukaryotic cells, both of which are key elements in response to hypoxia50,51. Numerous studies have noted that miRNAs and TFs are implicated in pathophysiological processes, like mitochondrial function, endoplasmic reticulum stress, cellular proliferation, and DNA repair, which may ultimately lead to tumor progression, cardiovascular sequelae, and abnormal lipid metabolism51,52,53,54. Our study constructed a network of miRNAs and TFs based on target genes, which contained 128 miRNAs and 40 TFs, providing a basis for further research on the immunological mechanisms of OSA.
Continuous positive airway pressure is the main highly effective treatment regimen for OSA, but its clinical effectiveness is restricted by poor tolerance and poor adherence in many patients. The effectiveness of alternative therapies like upper airway surgeries, oral appliances, and hypoglossal nerve stimulation depends on patients’ specific conditions and is difficult to predict55,56. Although pharmacologic therapies for OSA cover drugs that enhance airway muscle tone, ventilatory drive, and arousal threshold, these therapies are still under investigation56,57. The present study predicted 172 potential target drugs/compounds associated with IRGs in OSA and its complications. Better matching of drugs to OSA patients according to dominant mechanisms may yield better results.
The present investigation identified the most promising DEIRGs and elucidated underlying immune-related pathophysiological performance in OSA. Two major limitations in this study warrant attention in future research. Firstly, the sample size for clinical validation was relatively small, which may have constrained the generalizability of the findings. Secondly, variations in different tissues could influence gene expression profiles. However, the results, in conjunction with bioinformatic analysis and validation after controlling for confounding factors, might be critical for screening DIERGs in OSA. Future large-scale longitudinal cohort studies should include diverse tissue samples and conduct in vitro validation to investigate the triggering signals and underlying pathophysiological mechanisms and provide direct evidence of complications.
Conclusions
This study systematically evaluated the immune-related patterns in OSA, investigated the immunologic functions of immunocytes, and constructed a drug network using bioinformatics approaches. Additionally, we identified potential immune-related biomarkers and offered novel insight into diagnosis, mechanism research, and management strategies for future studies on OSA.
Data availability
The original contributions presented in the study are included in the article/Supplementary Materials. Further inquiries can be directed to the corresponding author.
Abbreviations
- AHI:
-
Apnea-hypopnea index
- CI:
-
Confidence interval
- DC:
-
Dendritic cells
- DEG:
-
Differentially expressed genes
- DEIRG:
-
Differentially expressed-related and immune-related gene
- GEO:
-
Gene expression omnibus
- GSEA:
-
Gene Set Enrichment Analysis
- GO:
-
Gene oncology
- HLA:
-
Human leukocyte antigen
- IFN:
-
Type I interferon
- IRG:
-
Immune-related gene
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- MC:
-
Mast cells
- miRNA:
-
Micro-RNA
- NOSA:
-
Non-obstructive sleep apnea
- OSA:
-
Obstructive sleep apnea
- ROC:
-
Receiver operating characteristic
- RT-qPCR:
-
Reverse transcriptionquantitative PCR
- TF:
-
Transcription factor
References
Jordan, A. S., McSharry, D. G. & Malhotra, A. Adult obstructive sleep Apnoea. Lancet 383(9918), 736–747 (2014).
Benjafield, A. V. et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir. Med. 7(8), 687–698 (2019).
Lévy, P. et al. Obstructive sleep Apnoea syndrome. Nat. Rev. Dis. Primers 1, 15015 (2015).
Fang, Y. et al. Autoantibodies of inflammatory cytokines as serum biomarkers in OSA patients. Clin. Chim. Acta 547, 89 (2023).
Liu, X. et al. The relationship between inflammation and neurocognitive dysfunction in obstructive sleep apnea syndrome. J. Neuroinflammation. 17(1), 229 (2020).
Kuhle, S. & Urschitz, M. S. Anti-inflammatory medications for the treatment of pediatric obstructive sleep apnea. Paediatr. Respir Rev. 34, 35–36 (2020).
Marchi, N. et al. Obstructive sleep Apnoea and 5-year cognitive decline in the elderly. Eur. Respir. J. 61, 4 (2023).
Gleeson, M. & McNicholas, W. Bidirectional relationships of comorbidity with obstructive sleep Apnoea. Eur. Respir Rev. 31, 164 (2022).
Redline, S., Azarbarzin, A. & Peker, Y. Obstructive sleep Apnoea heterogeneity and cardiovascular disease. Nat. Rev. Cardiol. 20(8), 560–573 (2023).
Cortese, R. et al. Single-cell RNA-seq uncovers cellular heterogeneity and provides a signature for paediatric sleep Apnoea. Eur. Respir. J. 61, 2 (2023).
Song, R., Baker, T. L., Watters, J. J. & Kumar, S. Obstructive sleep Apnea-Associated intermittent Hypoxia-Induced immune responses in males, pregnancies, and offspring. Int. J. Mol. Sci. 25, 3 (2024).
Alzoubi, M. R. & Aldomi Al-Domi, H. Could omega-3 fatty acids a therapeutic treatment of the immune-metabolic consequence of intermittent hypoxia in obstructive sleep apnea? Diabetes Metab. Syndr. 11(4), 297–304 (2017).
Díaz-García, E. et al. Cubillos-Zapata, PSGL-1: a novel immune checkpoint driving T-cell dysfunction in obstructive sleep apnea. Front. Immunol. 14, 1277551 (2023).
Hernández-Jiménez, E. et al. E. López-Collazo, monocytes inhibit NK activity via TGF-β in patients with obstructive sleep Apnoea. Eur. Respir. J. 49, 6 (2017).
Cubillos-Zapata, C. et al. Obstructive sleep apnea monocytes exhibit high levels of vascular endothelial growth factor secretion, augmenting tumor progression. Mediators Inflamm. 2018, 7373921 (2018).
Almendros, I., Martinez-Garcia, M. A., Farré, R. & Gozal, D. Obesity, sleep apnea, and cancer. Int. J. Obes. (Lond). 44(8), 1653–1667 (2020).
Akalin, P. K. Introduction to bioinformatics. Mol. Nutr. Food Res. 50(7), 610–619 (2006).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28(1), 27–30 (2000).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51(D1), D587–D592 (2023).
Ryan, S. et al. Adipose tissue as a key player in obstructive sleep Apnoea. Eur. Respir Rev. 28, 152 (2019).
Gharib, S. A., Hayes, A. L., Rosen, M. J. & Patel, S. R. A pathway-based analysis on the effects of obstructive sleep apnea in modulating visceral fat transcriptome. Sleep 36(1), 23–30 (2013).
Chechi, K., Gelinas, Y., Mathieu, P., Deshaies, Y. & Richard, D. Validation of reference genes for the relative quantification of gene expression in human epicardial adipose tissue. PLoS One 7(4), e32265 (2012).
Liu, X. et al. Identification and validation of reference genes for quantitative RT-PCR analysis of retinal pigment epithelium cells under hypoxia and/or hyperglycemia. Gene 580(1), 41–46 (2016).
Agata, G., Piotr, K., Adam, A., Piotr, B. & Michał, P. IL-33 mediated inflammation in chronic respiratory Diseases-Understanding the role of the member of IL-1 superfamily. Front. Immunol. 10, 10 (2019).
Dandan, Z. et al. IL-33/ST2 mediating systemic inflammation and neuroinflammation through NF-kB participated in the neurocognitive impairment in obstructive sleep apnea. Int. Immunopharmacol. 115, 109604 (2023).
Dmitriy, K. et al. Antigen- and cytokine-driven accumulation of regulatory T cells in visceral adipose tissue of lean mice. Cell. Metab. 21, 4 (2015).
Dileep, U., Jonathan, J. & Vsevolod, P. Inflammation in sleep apnea: an update. Rev. Endocr. Metab. Disord 16, 1 (2014).
Liu, J. et al. IL-33 Initiates vascular remodelling in hypoxic pulmonary hypertension by up-regulating HIF-1α and VEGF expression in vascular endothelial cells. EBioMedicine 33, 196–210 (2018).
O’Garra, A. & Vieira, P. T(H)1 cells control themselves by producing interleukin-10. Nat. Rev. Immunol. 7(6), 425–428 (2007).
Hanna, B. S. et al. Interleukin-10 receptor signaling promotes the maintenance of a PD-1int TCF-1 + CD8 + T cell population that sustains anti-tumor immunity. Immunity 54, 12 (2021).
Park, H. K., Kim, D. H., Yun, D. H. & Ban, J. Y. Association between IL10, IL10RA, and IL10RB SNPs and ischemic stroke with hypertension in Korean population. Mol. Biol. Rep. 40(2), 1785–1790 (2013).
Wei, W. et al. Discovery and identification of EIF2AK2 as a direct key target of Berberine for anti-inflammatory effects. Acta Pharm. Sin. B 13(5), 2138–2151 (2023).
Li, Y. et al. Novel role of PKR in palmitate-induced Sirt1 inactivation and endothelial cell senescence. Am. J. Physiol. Heart Circ. Physiol. 315(3), H571–H580 (2018).
Hugon, J. & Paquet, C. The PKR/P38/RIPK1 signaling pathway as a therapeutic target in alzheimer’s disease. Int. J. Mol. Sci. 22, 6 (2021).
Chen, H. et al. ANGPTL1 attenuates colorectal cancer metastasis by up-regulating microRNA-138. J. Exp. Clin. Cancer Res. 36(1), 78 (2017).
Thorin, E. et al. Angiopoietin-Like proteins: cardiovascular biology and therapeutic targeting for the prevention of cardiovascular diseases. Can. J. Cardiol. 39(12), 1736–1756 (2023).
Kadomatsu, T., Tabata, M. & Oike, Y. Angiopoietin-like proteins: emerging targets for treatment of obesity and related metabolic diseases. FEBS J. 278(4), 559–564 (2011).
Systemic hypoxia drives. Inflammation persistence via suppression of monocytes. Nat. Immunol. 23(6), 830–831 (2022).
Jaipersad, A. S., Lip, G. Y. H., Silverman, S. & Shantsila, E. The role of monocytes in angiogenesis and atherosclerosis. J. Am. Coll. Cardiol. 63, 1 (2014).
Mancino, A. et al. Divergent effects of hypoxia on dendritic cell functions. Blood 112(9), 3723–3734 (2008).
Barroeta Seijas, A. et al. Mouse dendritic cells in the steady State: hypoxia, autophagy, and stem cell factor. Cell Biochem. Funct. 40(7), 718–728 (2022).
Möllerherm, H. et al. Köckritz-Blickwede, hypoxia modulates the response of mast cells to Staphylococcus aureus infection. Front. Immunol. 8, 541 (2017).
Viola, A., Munari, F., Sánchez-Rodríguez, R., Scolaro, T. & Castegna, A. The metabolic signature of macrophage responses. Front. Immunol. 10, 1462 (2019).
Mouton, A., Li, X., Hall, M. & Hall, J. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation. Circul. Res. 126(6), 789–806 (2020).
Cho, S. H. et al. Germinal centre hypoxia and regulation of antibody qualities by a hypoxia response system. Nature 537(7619), 234–238 (2016).
Liu, D. H., Mou, F. F., An, M. & Xia, P. Human leukocyte antigen and tumor immunotherapy (Review). Int. J. Oncol. 62, 6 (2023).
Siemens, D. R. et al. Hypoxia increases tumor cell shedding of MHC class I chain-related molecule: role of nitric oxide. Cancer Res. 68(12), 4746–4753 (2008).
Dong, S., Guo, X., Han, F., He, Z. & Wang, Y. Emerging role of natural products in cancer immunotherapy. Acta Pharm. Sin B. 12(3), 1163–1185 (2022).
Cubillos-Zapata, C. et al. Hypoxia-induced PD-L1/PD-1 crosstalk impairs T-cell function in sleep Apnoea. Eur. Respir. J. 50, 4 (2017).
Bartel, D. P. Metazoan MicroRNAs. Cell 173(1) 20–51 (2018).
Majmundar, A. J., Wong, W. J. & Simon, M. C. Hypoxia-inducible factors and the response to hypoxic stress. Mol. Cell. 40(2), 294–309 (2010).
Shang, F. et al. Obstructive sleep Apnea-induced endothelial dysfunction is mediated by miR-210. Am. J. Respir. Crit. Care Med. 207(3), 323–335 (2023).
Nallamshetty, S., Chan, S. Y. & Loscalzo, J. Hypoxia: a master regulator of MicroRNA biogenesis and activity. Free Radic Biol. Med. 64, 20–30 (2013).
Moriondo, G. et al. Lacedonia, intermittent hypoxia mediates cancer development and progression through HIF-1 and MiRNA regulation. Arch. Bronconeumol. 59(10), 629–637 (2023).
Schweitzer, P. K. et al. The combination of Aroxybutynin and Atomoxetine in the treatment of obstructive sleep apnea (MARIPOSA): a randomized controlled trial. Am. J. Respir Crit. Care Med. 208(12), 1316–1327 (2023).
Mason, M., Welsh, E. J. & Smith, I. Drug therapy for obstructive sleep Apnoea in adults. Cochrane Database Syst. Rev. 5, CD003002 (2013).
Gottlieb, D. J. & Punjabi, N. M. Diagnosis and management of obstructive sleep apnea: a review. JAMA 323(14), 1389–1400 (2020).
Acknowledgements
We thank GEO database, CIBERSORT database, NetworkAnalyz database, ImmPort database, KEGG database, GO database, GSEA database, and their contributors for the valuable public datasets used in this study. All of the authors are grateful to the staff in our sleep center and all of the subjects.
Funding
This study was supported by grants from the National STI2030-Major Projects of China (Grant No. 2021ZD0201900), National Natural Science Foundation of China (Grant Nos. 81970869, 82171125, and 82371131), Hospital Level Scientific Research Fund Program of Shanghai Sixth People’s Hospital (Grant No. ynts202404), Shanghai Municipal Commission of Science and Technology (Grant No. 18DZ2260200), Shanghai Science and Technology Innovation Program of Science and Technology Commission (Grant No. 20Y11902100), and Shanghai Shen-Kang Hospital Management Center Project (Grant Nos. SHDC2020CR2044B and SHDC2020CR3056B).
Author information
Authors and Affiliations
Contributions
The corresponding authors are responsible for the authenticity of the data. Conception and study design: J.Y.Z., H.L.Y. and W.J.H. Manuscript drafting and critical revision: E.H.Z., T.J.Z., S.K.Y., H.L.Y. Data collection and analysis: E.H.Z., X.T.W., T.J.Z. and J.G. Obtained funding: H.L.Y, S.K.Y., and W.J.H. All authors approved the final version of the manuscript to be published; they agreed on submission to this journal. All authors have agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (Approval No: 2019-KY-050[K]) and registered at the Chinese Clinical Trial Registry (No. ChiCTR1900025714; URL: http://www.chictr.org.cn/showproj.aspx?proj=43057). The research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
All patients provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, Eh., Zhou, Tj., Wang, Xt. et al. Identifying and validating immunological biomarkers in obstructive sleep apnea through bioinformatics analysis. Sci Rep 15, 9746 (2025). https://doi.org/10.1038/s41598-025-93915-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-93915-4
Keywords
This article is cited by
-
Polygenic insight identifies precision biomarkers decoding protein catabolism and autophagy pathways in obstructive sleep apnea
Scientific Reports (2025)
-
Integrating bulk and single-cell RNA sequencing data to dissect genetic links between periodontitis and obstructive sleep apnea
Sleep and Breathing (2025)