Abstract
Vancomycin-Resistant Enterococcus (VRE) is one of the key antibiotic-resistant pathogens that challenges the health system with its threat to human health. Most VRE infections occur in hospital settings as these pathogens are known to colonize hospital environments and maintain their viability for long periods. Without good infection control measures, these pathogens can spread in the hospital setting and cause hospital-acquired infections including bacteremia. In this study, we report the isolation of VRE from patient samples hospitalized in four Palestinian hospitals. The American Society for Microbiology proceedings were utilized to culture and identify VRE. During the 5-year study period between December 2020 and March 2024, 736 VRE isolates were detected, and 30 (4.76%) patients with bacteremia were reported. Excellent infection control measures including active surveillance swabs, contact precaution and following strict isolation protocols were important to limit the spread of these pathogens, as well as limiting the consumption of antibiotics, especially Vancomycin. In this research article, we discuss the detection of VRE in the different hospitals located in West Bank and East Jerusalem. We also analyze the prevalence of VRE in other body sites including anal surveillance swab, urine, wound and stool cultures that may be associated with developing VRE bacteremia. The cumulative average of VRE causing bacteremia was of urinary origin, followed by wound and stool positive cultures, respectively. Hospital number 2 had the highest risk of developing bacteremia in patients with other VRE positive culture or swab with a percentage of 11.3%.
Similar content being viewed by others
Introduction
Enterococci are gram positive facultative anaerobic bacteria, the two most common species are Enterococcus faecalis and Enterococcus faecium. These microorganisms are present as normal flora mostly in the gastrointestinal tract, it can cause severe infections including bacteremia, surgical site infection, urinary tract infection and endocarditis1. Some studies show that infections caused by Vancomycin-Resistant Enterococci (VRE) has increased in hospital settings, causing healthcare-associated (HAI) infections. It has been listed by World Health Organization (WHO) as a high-priority pathogen because it is estimated to be causing 30% of Enterococcus infection in hospital settings2.
VRE outbreaks can occur in hospital settings due to multiple factors including poor hand hygiene, exposure to broad-spectrum antibiotics, lack of environmental hygiene and poor compliance with infection control protocols3,4,5,6,7. A prospective study by Stefanie et al., mentions that Surgical ICU is not considered a special risk factor for acquiring VRE. However, VRE acquisition was significantly associated with length of ICU stay, long-term dialysis and antibiotic treatment with flucloxacillin and piperacillin/tazobactam7. Patients who undergo immune suppression such as hematopoietic stem cell transplant patients, as well as hematology patients can be at increased risk for acquiring VRE8.
Available studies have shown that there’s an increased concern regarding the resistance of VRE to Linezolid and Daptomycin, as well as the increased hospitalization days and mortality in infected VRE bacteremia cases. A multi-centered research over a 6 year period by Meschiari et al. has shown that screening of VRE and isolation can reduce the instances of VRE in a hospital9.
In our study, data had been collected from four hospitals in Palestine on a five-year duration, to find out the prevalence of VRE bacteremia in patients who are colonized or infected. Also, a comparison was done between the sites of colonization or infection that were mostly accompanied by bacteremia. In our study, most of the cases in hospital 1 were cancer patients, risk factors for developing VRE bacteremia in cancer patients colonized with VRE studied by Aimee et al., concluded the following factors: vancomycin use, diabetes mellitus, gastrointestinal procedures, and acute renal failure. Suggested strategies for prevention of VRE bloodstream infection in VRE-colonized cancer patients with cancer, should include limiting vancomycin use10. Another study on cancer patients, mentioned that VRE colonized patients with solid tumor had a significantly lower risk of developing VRE bacteremia compared to liquid tumor cases, it’s also suggested that neutropenic fever cases might benefit from coverage of VRE in case of colonization11.
Count of VRE infectious cases in each hospital was analyzed, including urinary tract infection, wound infection, positive stool culture and anal surveillance swab, sputum, CSF, catheter tip and skin swab culture. Four of these sites were related to VRE bacteremia, urinary tract infection, wound infection, stool culture and anal surveillance swab.
Methodology
Setting
The study included all patients who had a positive VRE culture in urine, sputum, aspirated fluid, and rectal surveillance culture and had a blood culture collected whether it was positive or negative. Patients with any positive VRE culture and no blood culture were excluded. The study included cases within five years from December 2020 until March 2024, in four hospitals in Palestine. :
These hospitals included a main hemato-oncology referral center with a long-term nursing facility, termed hospital 1 here, a specialized surgical hospital with a COVID-19 unit, termed hospital 2, a specialized pediatric hospital, termed hospital 3, and a main district hospital, termed hospital 4.
Study design and statistical analysis
Our study is a retrospective cohort study, data were collected from each hospital’s information system, data was filtered to avoid duplication and analyzed to calculate the percentage of patients having a positive VRE result in any culture or swab in addition to a positive blood culture within a fourteen-day duration using Microsoft Excel. The cumulative average of positive VRE culture in other sites causing VRE bacteremia was calculated.
Ethical considerations
All methods were carried out in accordance with relevant guidelines and regulations, and all experimental protocols were approved by Augusta Victoria Hospital Ethical committee under IRB number 40/GLD/2024. Written consent was waived by ethical committee, as no intervention was made in the treatment plan or tests done for patients, only readily available data on the hospital system was extracted and analyzed in this research. Due to the retrospective nature of the study, Medical Ethics Committee at Augusta Victoria Hospital IRB 40/GLD/2024 waived the need of obtaining informed consent.
Results
The total percentage of VRE bacteremia in all hospitals was 4.76%, 30 bacteremia cases were diagnosed out of 736 VRE isolations in all other sites.
The percentage of bacteremia cases due to VRE from highest to lowest was in hospital 2, followed by 4, 1 and 3, respectively.
Hospital 1 had 1.9% VRE bacteremia cases in patients with positive VRE culture, 11.3% in 2, 0.0% in 3 and 5.6% in 4.
At hospital 1, 40% of the cases with VRE bacteremia had no other positive culture for VRE, 20% had an infected bed sore with a positive culture for VRE, and 20% of the cases in hospital 1 had a positive urine culture for VRE, as well as 20% positive rectal surveillance culture. In hospital 2, 11% of bacteremia cases had no other positive culture for VRE, 11% positive stool culture and 78% positive rectal surveillance culture. In hospital 4 5% had no other positive culture, 5% positive wound culture, 60% positive urine culture and 30% positive rectal surveillance culture. The results was 0% bacteremia cases compared to other sites for hospital 3.
Positive rectal surveillance culture for VRE had the highest percentage in all hospitals, from highest to lowest was hospital 3, followed by 1, 2 and 4, respectively.
Discussion
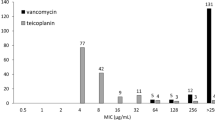
Infections due to VRE are considered one of the main burdens on healthcare facilities, as it can transfer its vancomycin resistance to Staphylococcus aureus, and it mostly affects patients in intensive care units, immunocompromised patients and leads to prolonged hospitalization and higher mortality rates4. It can also survive in the environment for more than one week on almost any surface. The percentage of infection has increased significantly in recent years with approximately 50% in Australia and over 20% in European countries. Xie et al. found in a large cohort study on hematology and oncology cases, that of patients who developed VRE BSI, 68% were found to be colonized and 79% were neutropenic and antibiotics were administered for a median of 17 days before diagnosis with a BSI. Patients included in this study who had, VRE VanB cases were treated with either Daptomycin, Linezolid, or Teicoplanin, and it was found that Teicoplanin had the lowest mortality rate4,5.
This retrospective study was used to assess risk among positive surveillance culture cases in developing VRE bloodstream infection (BSI) among four different health care facilities. Colonization is an asymptomatic condition, which might last for a long period with comparatively small numbers of documented infections. Active surveillance, however, is an important tracking monitoring process to prevent future transmissions and high-risk infections. In our study, all studied hospitals had the same infection control policies, however, adherence to these policies varied. To avoid any issues with hospitals in the region, we avoided disclosing names of the hospitals, as they will consider this research as an evaluation of the infection control measures in their institution, names can be disclosed privately to the reader upon request.
As seen in Fig. 1, hospital 2 had the highest risk of bacteremia due to overall positive culture for VRE, which might be explained by this same hospital having the highest percentage of positive rectal surveillance culture for VRE. 20% of patients with positive rectal surveillance cultures developed BSI in hospital 1, which serves mainly hemato-oncology patients and patients in need for long-term nursing, compared to 78% of patients from hospital 2, the specialized surgical hospital with a COVID-19 center, 0% from hospital 3, the pediatric center and 30% from the main district center. These variations can be attributed to a number of factors; with the population served being one of the major factors: patients with malignancy are at a considerably higher risk for VRE colonization and subsequently infection, especially those with leukemia or who were previously exposed to vancomycin12. Also, hematopoietic stem cell transplant patients are at an increased risk of infections due to multidrug resistant bacteria, including VRE because they rely on immediate administration of antibiotics to fight infections1. Oliver et al. found that long-term care facilities had an increased rate of VRE BSI, this risk increased with prior use of vancomycin or in the presence of another body site infection13. Matar et al. found that patients receiving chemotherapeutic agents that produce gastrointestinal mucositis and severe neutropenia are at increased risk for VRE infection secondary to colonization, which might explain the relatively high number of cases in hospital 1, which is an oncology-specialized center with a high number of such cases.
While hospital 2 had the highest percentage of anal colonization among patients developing BSI, it had the smallest crude number of colonization cases among the four studied hospitals, this might be reflective of strict surveillance policy rather than major differences in patient characteristics. While hospital three had 114 cases of VRE colonization, it had zero cases of infection. While the characteristics of pediatric age group patients at risk for VRE colonization and infection do not differ from that of adult patients, that is, patients with malignancies or organ transplant, the lack of these two specific groups among the population served by hospital 3 explains our findings1. Regarding hospital 4, it had the highest number of colonization and infection. As an acute care hospital that serves an entire district, various factors were identified as possible factors contributing for VRE colonization, including an increase in the number of beds per room, a phenomenon observed in the district hospital in comparison to the three other specialized centers. In addition, the lack of good antimicrobial stewardship due to the lack of an independent infection control unit14. Also, the percentage of positive VRE rectal surveillance cultures can’t be as reflective of the true percentage as in the other three hospitals, as their criteria for screening patients is not identical. On the other hand, hospitals 1, 2 and 3 had similar screening protocols in addition to infection prevention and control strategies. Molecular detection was not performed in this study.
Infection control strategies employed to detect multidrug resistant (MDR) organisms in the studied hospitals were the same: patients referred from other hospitals directly, patients who had a history of admission the last 6 months, and patients who are known to have a multidrug resistant organism in the past underwent surveillance via nasal and rectal surveillance cultures. All patients who underwent screening swabs and met the criteria for active surveillance screening were kept in contact isolation until the final results of pending swabs., Those who tested positive for VRE continued to be isolated in a contact mode isolation, if available in a single room, if not in a cohort room with patients who are colonized with the same organism. While those who were known to harbor a resistant organism were put in contact isolation from the start, pending the result of their surveillance swab. These methods do not only aim at identifying patients who acquired an MDR organism during their journey between hospitals, but also aim at identifying community cases colonized with VRE with no history of prior hospitalization, as a Czech study published in 2006 found that 0.4% of people in the community are colonized by VRE15.
Zirakzadeh et al. found that VRE bacteremia secondary to colonization is dependent on the population affected. In kidney and pancreas transplant patients, bacteremia is usually secondary to VRE wound or UTI, while neutropenic patients are at risk of VRE bacteremia as a result of gut translocation, central line infection or UTI16. In our study, the highest percentage of other VRE sites that might potentially be the source of VRE BSI was highly variable from one center to another (Fig. 2). In Fig. 3, in all 4 hospitals most of rectal surveillance swabs had a positive result of VRE, followed by blood, urine, wound and stool, respectively. On the other hand, skin swab culture, sputum, CSF and other sites results were negligible. However, the cumulative average of other site infection causing BSI showed that the most common origin was the urinary tract, followed by wound infection, and then gastrointestinal tract (GIT) as shown in Fig. 4.
While anal colonization had the lowest percentage for BSI among the aforementioned sites, it had the highest incidence of positive VRE culture among them. In principle, infection with VRE is usually seen in those colonized with the bacteria. The ratio in infected-to-colonized patients is dependent on the population affected, with the ratio in hematology and organ transplant patients being the highest16. In our study, the underlying medical condition of the studied subjects was not included, which might be counted as a limitation of this study.
Conclusion
Patients at risk for VRE colonization including ICU patients, and patients with altered bowel habits should be identified for screening, so infection control measures can be taken in order to reduce the risk of nosocomial transmission. In addition, the use of vancomycin as part of empiric therapy should be controlled because it is identified as a risk factor for VRE BSI. Also, in some cases of septic patients with VRE colonization or VRE infection, it might be needed to cover VRE empirically based on clinical judgement.
Data availability
Data is provided within supplementary information files.
References
Vancomycin-resistant enterococcus. colonization and infection in children: six-year follow-up - PubMed n.d. accessed August 22, (2024). https://pubmed.ncbi.nlm.nih.gov/26388592/
WHO publishes list of bacteria for which new antibiotics. are urgently needed n.d. accessed July 29, (2024). https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed
Sakka, V. et al. Risk-factors and predictors of mortality in patients colonised with vancomycin-resistant enterococci. Clin. Microbiol. Infect. 14, 14–21. https://doi.org/10.1111/J.1469-0691.2007.01840.X (2008).
López-Luis, B. A. et al. Risk factors and outcomes associated with vancomycin-resistant Enterococcus faecium and ampicillin-resistant Enterococcus faecalis bacteraemia: A 10-year study in a tertiary-care centre in Mexico City. J. Glob Antimicrob. Resist. 24, 198–204. https://doi.org/10.1016/J.JGAR.2020.12.005 (2021).
Morgan, D. J. et al. The effect of contact precautions on healthcare worker activity in acute care hospitals. Infect. Control Hosp. Epidemiol. 34, 69–73. https://doi.org/10.1086/668775 (2013).
Billington, E. O. et al. Incidence, risk factors, and outcomes for Enterococcus spp. Blood stream infections: a population-based study. Int. J. Infect. Dis. 26. https://doi.org/10.1016/J.IJID.2014.02.012 (2014).
Kampmeier, S. et al. Hospital acquired Vancomycin resistant enterococci in surgical intensive care patients - a prospective longitudinal study. Antimicrob. Resist. Infect. Control 2018;7. https://doi.org/10.1186/S13756-018-0394-1
Weinstock, D. M. et al. Colonization, bloodstream infection, and mortality caused by vancomycin-resistant Enterococcus early after allogeneic hematopoietic stem cell transplant. Biol. Blood Marrow Transpl. 13, 615–621. https://doi.org/10.1016/J.BBMT.2007.01.078 (2007).
Johnstone, J. et al. Rates of blood cultures positive for vancomycin-resistant Enterococcus in Ontario: a quasi-experimental study. CMAJ Open. 5, E273. https://doi.org/10.9778/CMAJO.20160121 (2017).
Zaas, A. K., Song, X., Tucker, P. & Perl, T. M. Risk factors for development of vancomycin-resistant enterococcal bloodstream infection in patients with cancer who are colonized with vancomycin-resistant enterococci. Clin. Infect. Dis. 35, 1139–1146. https://doi.org/10.1086/342904 (2002).
Matar, M. J., Tarrand, J., Raad, I. & Rolston, K. V. I. Colonization and infection with vancomycin-resistant Enterococcus among patients with cancer. Am. J. Infect. Control. 34, 534–536. https://doi.org/10.1016/J.AJIC.2006.04.205 (2006).
Alevizakos, M. et al. Colonization with Vancomycin-Resistant enterococci and risk for bloodstream infection among patients with malignancy: A systematic review and Meta-Analysis. Open. Forum Infect. Dis. 4. https://doi.org/10.1093/OFID/OFW246 (2016).
Olivier, C. N., Blake, R. K., Steed, L. L. & Salgado, C. D. Risk of vancomycin-resistant Enterococcus (VRE) bloodstream infection among patients colonized with VRE. Infect. Control Hosp. Epidemiol. 29, 404–409. https://doi.org/10.1086/587647 (2008).
Tan, D. et al. Comparative epidemiology of Vancomycin-Resistant enterococci colonization in an Acute-Care hospital and its affiliated Intermediate- and Long-Term care facilities in Singapore. Antimicrob. Agents Chemother. 62. https://doi.org/10.1128/AAC.01507-18 (2018).
(PDF) Prevalence of vancomycin-resistant enterococci in hospitalized patients and those living in the community in the Czech Republic n.d. accessed August 22, (2024). https://www.researchgate.net/publication/6943271_Prevalence_of_vancomycin-resistant_enterococci_in_hospitalized_patients_and_those_living_in_the_community_in_the_Czech_Republic
Zirakzadeh, A. & Patel, R. Vancomycin-resistant Enterococci: colonization, infection, detection, and treatment. Mayo Clin. Proc. 81, 529–536. https://doi.org/10.4065/81.4.529 (2006).
Author information
Authors and Affiliations
Contributions
DS wrote the manuscript, HR extracted and analyzed the data, HA wrote the manuscript, A.Sh reviewed the manuscript, MH wrote the manuscript, AS supervised the research. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sadaqa, D., Rjoup, H., Arafat, H. et al. Risk for development of vancomycin resistant enterococci bacteremia among colonized or infected patients, a multiple center, retrospective study in Palestine. Sci Rep 15, 13182 (2025). https://doi.org/10.1038/s41598-025-93956-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93956-9