Abstract
Osteoporosis and osteopenia pose substantial public health challenges, particularly among postmenopausal women. Although various anthropometric measures have been proposed for risk assessment, their predictive performance and nonlinear relationships with bone outcomes remain unclear. We analyzed data from six consecutive cycles (2007–2018) of the National Health and Nutrition Examination Survey (NHANES). A total of 4473 postmenopausal women aged ≥ 50 years were included, each classified as having normal bone density, osteopenia, or osteoporosis based on dual-energy X-ray absorptiometry measurements. Ten anthropometric indices—waist-to-height ratio (WTHR), conicity index (CI), a body shape index (ABSI), body roundness index (BRI), lipid accumulation product, visceral adiposity index, cardiometabolic index, atherogenic index of plasma, weight-adjusted-waist index (WWI), and triglyceride–glucose (TyG) index—were examined using multiple logistic regression, restricted cubic spline curves, threshold-effect analyses, and SHAP (SHapley Additive exPlanations) analysis to assess their associations with osteoporosis and osteopenia. In fully adjusted models, individuals with higher WTHR, CI, BRI, WWI, and TyG tended to have a lower likelihood of osteoporosis or osteopenia (p < 0.01), whereas those with elevated ABSI were more likely to be diagnosed with these conditions (p < 0.01). Notably, several indices showed nonlinear effects on bone outcomes. Receiver operating characteristic (ROC) analyses indicated that WTHR and BRI had the highest discriminative capacity for differentiating osteoporosis from osteopenia. SHAP analysis further highlighted WTHR and BRI as the most influential predictors. WTHR and BRI demonstrated strong predictive utility for osteoporosis and osteopenia, suggesting their potential as noninvasive, cost-effective screening metrics for postmenopausal bone health. These findings provide insight into the varying roles of central and general obesity indicators in bone density and underscore the importance of incorporating novel anthropometric indices into early-stage risk assessment.
Similar content being viewed by others
Introduction
Osteoporosis and osteopenia occur at significantly higher rates among postmenopausal women in the United States. Studies indicate that approximately 30–50% of postmenopausal women develop osteopenia, and 15–20% ultimately progress to osteoporosis1. Furthermore, the risk of osteoporosis in this population is estimated to be two to three times higher than in men. The menopausal transition is associated with a decline in estrogen levels, neurodegenerative changes, and alterations in dietary habits2,3. Notably, reduced estrogen concentrations lead to an imbalance in bone remodeling, characterized by diminished osteoblast activity and heightened osteoclast activity. This phenomenon largely accounts for the difference in bone mineral density (BMD) observed before and after menopause. Indeed, the most rapid decline in femoral neck and lumbar spine BMD typically occurs within the first 1–2 years after menopause4,5. In a study by Liu and colleagues, the probability of osteoporosis in women over 50 years of age was 2.5 times greater than that in age-matched men; moreover, more than 55% of postmenopausal women with osteoporosis had sustained at least one fracture6.
Current intervention strategies predominantly emphasize pharmacological treatments for osteoporosis, whereas preventive measures have received comparatively less attention7. Most research to date has focused on menopausal hormone therapy (MHT), as well as calcium and vitamin D supplementation, to manage osteoporosis and osteopenia. Although MHT can increase bone mass and reduce fracture risk, its long-term use has been linked to elevated incidences of breast cancer and cardiovascular disease, thereby constraining its clinical applicability8,9. Consequently, preventing excessive bone loss from the outset may be more pragmatically beneficial. Previous studies have shown that increasing physical activity, maintaining an appropriate body weight, and optimizing nutritional intake can effectively attenuate bone loss and reduce fracture risk10,11. Nonetheless, non-pharmacological interventions often suffer from low adherence rates and considerable interindividual variability, limiting their broader impact12,13. Therefore, identifying simple, cost-effective early screening tools is crucial for enabling timely, targeted interventions during the early stages of disease progression and ultimately reducing fracture risk among postmenopausal women.
Anthropometric indices, which are noninvasive, cost-effective, and easily measured, have emerged as vital tools for screening health risks. Although body mass index (BMI) is widely used, it fails to capture individual variations in fat distribution or overall body composition. Hence, several novel indices—including the WTHR, CI, LAP, and TyG index—have been developed14,15,16,17. These indices demonstrate robust predictive value for various conditions, including cardiovascular disease, hip fractures, and metabolic syndrome. For instance, WTHR and CI can identify high-risk individuals for cardiovascular disease and hip fractures at an earlier stage, whereas the BRI exhibits high sensitivity in predicting cardiovascular mortality and overactive bladder18. LAP is used to assess hepatic steatosis, and TyG is strongly associated with both metabolic syndrome and insulin resistance. Additional indices—including ABSI, VAI, CMI, AIP, and WWI—are also gaining attention19. ABSI integrates waist circumference, BMI, and height to provide a more accurate predictor of mortality; VAI incorporates waist circumference, BMI, triglyceride, and high-density lipoprotein cholesterol levels to assess visceral fat accumulation and metabolic risk; and CMI combines waist circumference with lipid profiles to evaluate cardiovascular disease risk20. Collectively, these anthropometric measures can facilitate self-monitoring and early detection of obesity, osteoporosis, and metabolic disorders, which is particularly beneficial for postmenopausal women seeking to adopt lifestyle modifications and prevent adverse outcomes21. Nevertheless, no comprehensive study has yet confirmed the correlations between these emerging indices and osteopenia or osteoporosis in this specific population.
In light of these gaps, the present study analyzed data from the NHANES to investigate associations between ten anthropometric indices—WTHR, CI, ABSI, BRI, LAP, VAI, CMI, AIP, WWI, and TyG—and the prevalence of osteoporosis and osteopenia among postmenopausal women. These findings will provide a valuable reference for future longitudinal investigations and inform the development of novel screening strategies aimed at early, targeted interventions in this high-risk demographic.
Methods
Participants
The NHANES, initiated in 1960, includes participants of all ages, sexes, races, and geographic regions across the United States. It provides extensive data on demographics, dietary intake, body weight, height, and biochemical parameters. Each survey cycle comprises approximately 260 subcomponents and more than 1,400 research variables. As of 2024, data from 11 cycles have been released22.
In this study, we included 4473 postmenopausal women aged 50 years or older from six consecutive NHANES cycles (2007–2008 through 2017–2018). Menopausal status was determined using two items from the reproductive health questionnaire: (1) “Have you had at least one menstrual period in the past 12 months?” and (2) “What is the main reason for not having a menstrual period in the past 12 months?” Participants were considered postmenopausal if they answered “No” to the first question and “Menopause/Hysterectomy” to the second. Those who answered “Yes” to the first question—or “No” to the first question but “Pregnancy,” “Breastfeeding,” “Medical condition/treatment,” or “Other” to the second—and were under 55 years of age were classified as premenopausal23,24. We excluded 3555 adults who did not undergo bone density examinations, 772 individuals with incomplete menstrual cycle data, 67 lacking anthropometric information, and 26 with missing covariates. Ultimately, 4473 postmenopausal women with osteoporosis or osteopenia were retained for the final analysis (Fig. 1).
Outcome
Dual-energy X-ray absorptiometry (DXA) was performed by NHANES-certified radiologic technologists. Individuals with metallic implants, severe cardiopulmonary conditions, or body weight exceeding the DXA scanner’s capacity were excluded25. Because questionnaire responses may be subject to recall bias, osteoporosis and osteopenia in women were defined according to BMD measurements and their standard deviations at multiple sites, including the total femur (TF), femoral neck (FN), and lumbar spine (LS)26. The mean BMD of female participants aged 20 to 29 years served as the reference value for diagnosing postmenopausal osteoporosis and osteopenia27. Osteopenia was defined as a BMD value 1.0 to 2.5 standard deviations (SD) below this young-adult mean, whereas osteoporosis was defined as a BMD value more than 2.5 SD below the same reference (Supplementary Table 1).
Exposures
Anthropometric data were collected using calibrated and standardized equipment to ensure accurate measurements. Each parameter was measured at least twice to minimize random error, and any questionable or anomalous values were rechecked and validated. We then calculated the WTHR, CI, ABSI, BRI, LAP, VAI, CMI, AIP, WWI, and TyG index using previously validated formulas28,29,30,31.
Covariates
In this study, we included and adjusted for multiple potential confounders to ensure the accuracy and reliability of our findings. We considered demographic variables, including age (categorized as middle-aged: 50–64 years, or older: ≥ 65 years), race (non-Hispanic White, non-Hispanic Black, Mexican American, and other), educational level (below high school, high school, or above high school), household income (determined by the ratio of family income to the poverty threshold [PIR]: low income [PIR ≤ 1.3], middle income [1.3 < PIR < 3.5], or high income [PIR ≥ 3.5]), and marital status (married or cohabiting, divorced/separated/widowed, or single). We also accounted for lifestyle factors, such as body mass index (BMI; normal or underweight < 25, overweight 25–29.9, or obese ≥ 30) and moderate physical activity (At least 150 min of moderate-intensity physical activity per week). In addition, we considered chronic noncommunicable diseases closely associated with BMD, including hypertension, cardiovascular disease (CVD), and diabetes. Hypertension was defined as an average systolic blood pressure (based on three measurements) ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or a self-reported history of hypertension. CVD encompassed physician-diagnosed congestive heart failure, coronary heart disease, angina, myocardial infarction, or stroke. Diabetes was defined by a fasting plasma glucose ≥ 7.0 mmol/L, a 2 h plasma glucose ≥ 11.0 mmol/L, a glycated hemoglobin A1c ≥ 6.5%, or a self-reported diabetes diagnosis. All covariates were defined and measured in accordance with standardized data collection procedures of the NHANES. Further details are provided in the official NHANES documentation (https://wwwn.cdc.gov/nchs/nhanes).
Statistical analysis
We consulted the NHANES analytical guidelines to properly account for sample weights, stratification, and clustering. In this study, categorical baseline characteristics are expressed as counts and percentages, whereas continuous variables are reported as means and standard deviations. To enhance model accuracy and efficiency, and to reduce the impact of varying measurement scales, we applied z-standardization to transform non-normally distributed data into a standard normal distribution with a mean of zero and a standard deviation of one.
We used multiple logistic regression models to assess associations between various anthropometric indices and osteoporosis or osteopenia. Three models were developed. Model 1 was unadjusted. Model 2 controlled for demographic variables (age, race, education level, PIR, and marital status). Model 3 was fully adjusted by including hypertension, cardiovascular disease, diabetes, and moderate physical activity in addition to the demographic covariates. We then employed RCS curves and threshold-effect analyses to examine potential nonlinear associations between different anthropometric indices and osteoporosis or osteopenia. Discriminatory power was evaluated by comparing area under the curve (AUC) values and ROC curves for each index among postmenopausal individuals with osteoporosis or osteopenia. Finally, to quantify the relative importance of each anthropometric measure in predicting osteoporosis and osteopenia, we conducted SHAP (SHapley Additive exPlanations) analyses. All statistical procedures were performed using R (version 4.3.1) and Empower (version 4.2.0; www.empowerstats.com).
Results
Baseline characteristics
As shown in Supplementary Table 2, this study included 4,473 postmenopausal women, of whom 2274 (50.9%) had normal bone density, 199 (4.4%) had osteoporosis, and 2000 (44.7%) had osteopenia. Overall, the median age was approximately 64 years. However, among participants with osteoporosis, 75.4% were aged 65 years or older, a proportion significantly higher than that in both the normal bone density group (31.4%) and the osteopenia group (53.5%) (p < 0.001). In terms of educational attainment, the osteoporosis group had the highest percentage (35.2%) of individuals with less than a high school education, compared with 23.2% in the normal bone density group and 25.9% in the osteopenia group (p = 0.002). Regarding marital status, 60.8% of participants in the osteoporosis group were divorced, separated, or widowed, markedly exceeding the proportion observed in the other two groups (p < 0.001). From a lifestyle perspective, 79.4% of those in the osteoporosis group reported no moderate exercise, which was significantly higher than the 62.2% in the normal bone density group and 63.0% in the osteopenia group (p < 0.001).
When categorized according to body mass index (BMI), 62.3% of the osteoporosis group were classified as normal or underweight (BMI < 25). By contrast, 54.1% of the normal bone density group were obese (BMI ≥ 30), while 27.3% of the osteopenia group met the obesity criterion (p < 0.001). This distribution was also reflected in mean body weight: the osteoporosis group recorded the lowest average (56.98 ± 11.76 kg), followed by the osteopenia group (68.32 ± 14.03 kg) and the normal bone density group (81.41 ± 17.91 kg) (p < 0.001). Waist circumference showed a similar pattern (87.59 ± 12.67 cm vs. 94.86 ± 12.93 cm vs. 103.15 ± 14.14 cm, p < 0.001). Furthermore, key anthropometric indices such as waist-to-height ratio (WTHR; 56.75 ± 8.50) and the body roundness index (BRI; 4.86 ± 1.88) were significantly lower in the osteoporosis group than in the other two groups, whereas a body shape index (ABSI; 0.085 ± 0.005) was relatively higher (p < 0.001). By comparison, WTHR, BRI, and weight-adjusted-waist index (WWI) values were notably higher in both the osteopenia and normal bone density groups.
Associations between anthropometric parameters and osteoporosis and osteopenia in postmenopausal women
In this study, we used multiple logistic regression to evaluate the relationships between ten anthropometric indices and osteoporosis or osteopenia. Central obesity indicators included WTHR, LAP, VAI, ABSI, AIP, and CL. According to the regression results, WTHR showed a significant negative association with both osteoporosis and osteopenia (OR < 1, p < 0.01), (Supplementary Table 2). Specifically, higher WTHR was related to a lower prevalence of these conditions in all models. In Model III, the odds ratio for WTHR was 0.91 (95% CI 0.89–0.93, p < 0.01) in the osteoporosis group and 0.95 (95% CI 0.94–0.95, p < 0.01) in the osteopenia group. LAP demonstrated a similar trend, with an OR of 0.26 (95% CI 0.11–0.58, p < 0.01) for osteoporosis and 0.42 (95% CI 0.30–0.58, p < 0.01) for osteopenia in Model III. By contrast, ABSI differed from the other central obesity indices by showing a positive correlation (OR > 1, p < 0.01) with both osteoporosis and osteopenia. As ABSI increased, the prevalence of osteoporosis rose accordingly (Model III OR = 1.44, 95% CI 1.21–1.71, p < 0.01). CL also showed a significant negative association in some models. Although AIP exhibited a stronger inverse association with osteopenia (Model III OR = 0.57, 95% CI 0.39–0.82, p < 0.01), it was not significantly related to osteoporosis (p > 0.05). Finally, VAI did not reach statistical significance (p > 0.05), and its effect on osteoporosis or osteopenia remains unclear.
General obesity indicators included BRI, WWI, TyG, and CMI. BRI showed a significant negative correlation (OR < 1, p < 0.01). In Model III, its OR for osteoporosis was 0.67 (95% CI 0.61–0.75, p < 0.01), while for osteopenia it was 0.81 (95% CI 0.78–0.84, p < 0.01). WWI displayed a similar negative trend, with an OR of 0.77 (95% CI 0.67–0.89, p < 0.01) for osteoporosis and 0.84 (95% CI 0.79–0.89, p < 0.01) for osteopenia in Model III. However, TyG and CMI showed inconsistent associations across models. TyG only exhibited a negative correlation with osteoporosis in the Q4 subgroup of Model III (OR = 0.46, 95% CI 0.19–1.10, p = 0.08), which did not meet the conventional threshold for statistical significance. Meanwhile, CMI was inversely related to osteopenia (Model III OR = 0.66, 95% CI 0.54–0.82, p < 0.01), but it was not significantly associated with osteoporosis.
Overall, central obesity indices had a more pronounced impact on osteoporosis and osteopenia than general obesity indicators. WTHR, LAP, BRI, and WWI all displayed consistent negative correlations (OR < 1, p < 0.01). In contrast, ABSI and CL were positively associated (OR > 1) in selected models. VAI, TyG, and CMI yielded variable results across different analyses.
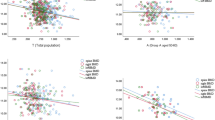
Nonlinear associations and threshold effects of anthropometric indices with osteoporosis and osteopenia
We applied RCS curves and threshold-effect analyses to explore nonlinear relationships between ten anthropometric indices and osteoporosis or osteopenia, (Supplementary Table 3). In the osteoporosis group, seven indices—all except ABSI, WWI, and TyG—exhibited significant nonlinear associations with osteoporosis, (Figs. 2, 3). In contrast, only the BRI, LAP, VAI, and CMI demonstrated nonlinear relationships with osteopenia. The key turning points for WTHR, CL, BRI, ABSI, LAP, VAI, CMI, AIP, WWI, and TyG in the osteoporosis group were 53.57, 1.29, 4.43, 0.09, 45.50, 2.22, 0.63, 0.15, 17.55, and 8.44, respectively. The corresponding cut-offs in the osteopenia group were 58.45, 1.30, 5.39, 0.09, 56.11, 2.48, 0.73, 0.26, 17.95, and 8.68. Among individuals with osteoporosis, WTHR, BRI, LAP, WWI, and TyG remained negatively correlated with the disease across the full range of values. In contrast, although CL, ABSI, VAI, CMI, and AIP became positively correlated with osteoporosis once they exceeded their respective thresholds, these relationships did not reach statistical significance. Finally, in the osteopenia group, increases in VAI and CMI exhibited a robust U-shaped association with osteopenia (p for non-linearity < 0.05).
Diagnostic performance of different anthropometric indicators
In this study, we used ROC curves to assess the performance of several anthropometric indices for distinguishing osteoporosis from osteopenia, (Supplementary Table 5). Our findings revealed that the WTHR and the BRI achieved higher areas under the curve (AUCs) than the other indices in both conditions, (Fig. 4). Moreover, the optimal cut-off values for WTHR and BRI in the osteoporosis group were − 0.16 and − 0.22, respectively, whereas in the osteopenia group, these values were − 0.91 and − 0.89.
Model decision of SHAP
We used SHAP analysis to determine the relative importance of various anthropometric indices in predicting osteoporosis and osteopenia, (Fig. 5). First, we compared multiple machine learning models by evaluating their performance using ROC curves, confusion matrices, Youden’s index, area under the curve (AUC), accuracy, and F1 scores, (Supplementary Table 6). Based on these criteria, the neural network model (AUC = 0.898) and the logistic regression model (AUC = 0.823) were identified as the most effective classifiers for osteoporosis and osteopenia, respectively. We then conducted SHAP analyses, which included swarm plots and feature-importance rankings, to identify the most influential predictors. Our results indicate that, for osteoporosis, the BRI has the strongest predictive influence, followed by the WWI. In contrast, for osteopenia, the WTHR emerged as the most significant predictor, with WWI and BRI ranking second and third, respectively.
SHAP Analysis of Anthropometric Indicators in Predicting Osteoporosis and Osteopenia. (A, D) ROC curves comparing the performance of different machine learning models for predicting osteoporosis (A) and osteopenia (D). (B, E) Mean absolute SHAP values ranking the most influential features in the neural network (B) and logistic regression (E) models. (C, F) SHAP summary plots showing the distribution of SHAP values for each feature in the neural network (C) and logistic regression (F) models.
Discussion
We used data from six consecutive cycles (2007–2018) of the NHANES to investigate associations between ten anthropometric indices—WTHR, CI, ABSI, BRI, LAP, VAI, CMI, AIP, WWI, and TyG index—and the prevalence of osteoporosis and osteopenia in postmenopausal women. In fully adjusted models, most indices (WTHR, CI, BRI, WWI, and TyG) were negatively and significantly associated with these conditions, whereas ABSI displayed a positive correlation with osteoporosis and osteopenia. Among the ten indices, BRI and WTHR demonstrated the highest discriminative capacity. Notably, several indices exhibited nonlinear relationships with bone outcomes. For example, when BRI fell below 4.44, even a minor increase was linked to a substantial rise in osteopenia risk. Furthermore, SHAP analysis confirmed that WTHR and BRI were among the most influential predictors of osteoporosis and osteopenia, underscoring the importance of these anthropometric measures in clinical assessments of bone health.
Based on the results of this study, the WTHR and the BRI demonstrated strong predictive value for osteoporosis and osteopenia, along with evidence of a nonlinear relationship32,33. In recent years, both indices have been increasingly examined in metabolic disorders, cardiovascular diseases, and bone health. WTHR captures waist circumference relative to height and effectively reflects central adiposity, whereas BRI incorporates waist circumference and height into a mathematically optimized model, making it more sensitive to overall body shape and fat distribution34,35,36. In the context of bone health, previous research indicates that central obesity may promote bone loss through chronic inflammation, abnormal adipose metabolism, and insulin resistance, thereby elevating osteoporosis risk37,38. These mechanisms could explain the significant associations between WTHR, BRI, and reduced BMD observed in our study39. Published evidence further highlights the potential role of WTHR and BRI as clinical tools for assessing bone health. For example, Lin et al.40 reported that WTHR not only predicted sarcopenia but also effectively forecasted osteoporosis, thereby emphasizing its promise as a clinical screening approach. However, that study did not explore possible nonlinear effects of WTHR or its applicability across diverse populations41,42. Likewise, Chen et al.43 identified a U-shaped relationship between WTHR-defined obesity and osteoporosis in postmenopausal women, suggesting that both extremely low body weight and excessive adiposity may increase the risk of osteoporosis. Nevertheless, their findings were limited by a lack of covariate adjustments, restricting the generalizability of the conclusions. Ding et al.44 further demonstrated a key threshold for BRI in predicting osteoporosis risk: once BRI exceeded 9.5229, BMD declined significantly (− 0.0363 g/cm2 per unit increase), suggesting that higher BRI values may serve as a risk factor for osteoporosis45. These data align with our findings and underscore the importance of BRI in monitoring bone health. In conjunction with our study, the collected evidence suggests that WTHR and BRI could serve as valuable, noninvasive, and cost-effective screening metrics for identifying osteoporosis and osteopenia in postmenopausal women46,47. Future research should validate these indices across diverse ethnicities, age cohorts, and health statuses.
WTHR and BRI, which emerged as the most robust anthropometric predictors of bone density in our analysis, may influence bone health through distinct physiological pathways. As a measure of central obesity, WTHR primarily reflects abdominal fat accumulation, which has been linked to osteoporosis via chronic inflammation, endocrine imbalances, and insulin resistance40. Excess visceral adipose tissue secretes pro-inflammatory cytokines, including tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6). These mediators can activate the RANK/RANKL/OPG signaling cascade, increasing osteoclast activity while inhibiting osteoblast differentiation and thus accelerating bone loss48. Moreover, a cohort study revealed that each incremental rise in WTHR was associated with a 1.47-fold increase in fracture risk (95% CI 1.20–1.81, p < 0.01) in postmenopausal women, lending further support to WTHR as a tool for early osteoporosis screening44. By contrast, BRI reflects general (overall) obesity by integrating weight and waist circumference, allowing it to capture comprehensive fat distribution and body composition. In this study, a higher BRI was significantly and inversely correlated with osteoporosis and osteopenia (OR < 1, p < 0.01), suggesting that elevated BRI values might confer a protective effect on bone25. One plausible explanation lies in the dual role of adipose tissue: subcutaneous fat may enhance bone formation, whereas visceral fat can be harmful to bone integrity. Furthermore, reduced muscle mass often accompanies obesity and may diminish mechanical loading on bone, aggravating bone loss. Indeed, one investigation reported that each 1 kg increase in muscle mass lowered the risk of low bone density by 7% (p = 0.03) in postmenopausal women49. Since an elevated BRI typically corresponds to reduced muscle mass, this interplay could partly explain the paradoxical relationship between adiposity and bone status in obese populations.
Despite the strong predictive performance of WTHR and BRI for osteoporosis, controversies persist concerning the effects of different obesity phenotypes on bone metabolism50. For instance, the LAP showed promising predictive utility in this study, yet its association with osteoporosis remains inconsistent across the literature. Some investigations have noted a positive correlation between LAP and BMD, whereas others propose that higher LAP could amplify fracture risk. Similarly, although the WWI demonstrated a protective influence on BMD in certain scenarios, it exhibited weaker predictive power here (OR = 0.84, 95% CI 0.79–0.89, p < 0.01). A systematic review also demonstrated that people with a higher TyG index tend to have lower BMD, which is consistent with our conclusion51. The AIP was significantly and inversely associated with low bone density in our sample but did not reach statistical significance in the osteoporosis subgroup, suggesting it may be more sensitive to mild bone loss52,53. Collectively, these findings indicate that both central and overall obesity indices exert varied effects on osteoporosis and osteopenia via distinct physiological pathways. In our analysis, WTHR and BRI demonstrated the highest discriminatory capacity, likely owing to their links with inflammatory pathways, fat distribution, and muscle mass changes.
This study has several limitations. First, as a cross-sectional investigation, it can only establish associations between anthropometric indices and osteoporosis or osteopenia, without inferring causality or underlying mechanisms. Longitudinal cohort studies are needed to track changes in bone mineral density over time and clarify the progression from osteopenia to osteoporosis. Second, although we adjusted for common chronic noncommunicable diseases such as hypertension, cardiovascular disease, and diabetes, we did not explicitly exclude conditions that directly affect bone health, such as fractures and bone tumors. Finally, this study did not address the key factor of postmenopausal osteoporosis—estrogen levels—and did not explore in detail how endocrine changes in older women might influence anthropometric indices and osteoporosis.
Conclusion
WTHR and BRI demonstrated strong predictive utility for osteoporosis and osteopenia, suggesting their potential as noninvasive, cost-effective screening metrics for postmenopausal bone health. These findings provide insight into the varying roles of central and general obesity indicators in bone density and underscore the importance of incorporating novel anthropometric indices into early-stage risk assessment. Future studies should validate these measures across diverse populations and clinical settings to enhance osteoporosis prevention strategies.
Data availability
The survey data are publicly available on the internet for data users and researchers throughout the world (https://www.cdc.gov/nchs/nhanes/index.htm).
References
Gilbert, L. et al. How diet, physical activity and psychosocial well-being interact in women with gestational diabetes mellitus: An integrative review. BMC Pregnancy Childbirth 19, 60. https://doi.org/10.1186/s12884-019-2185-y (2019).
Dello Russo, M. et al. Gestational weight gain and adiposity, fat distribution, metabolic profile, and blood pressure in offspring: The IDEFICS project. Int. J. Obes. (Lond.) 37, 914–919. https://doi.org/10.1038/ijo.2013.35 (2013).
Shevroja, E., Cafarelli, F. P., Guglielmi, G. & Hans, D. DXA parameters, trabecular bone score (TBS) and bone mineral density (BMD), in fracture risk prediction in endocrine-mediated secondary osteoporosis. Endocrine 74, 20–28. https://doi.org/10.1007/s12020-021-02806-x (2021).
Wang, L. et al. Association between glycosylated hemoglobin A1c and bone biochemical markers in type 2 diabetic postmenopausal women: A cross-sectional study. BMC Endocr. Disord. 19, 31. https://doi.org/10.1186/s12902-019-0357-4 (2019).
Méndez, J. P. et al. Bone mineral density in postmenopausal Mexican-Mestizo women with normal body mass index, overweight, or obesity. Menopause 20, 568–572. https://doi.org/10.1097/GME.0b013e318277694f (2013).
Hallfrisch, J., Powell, A., Carafelli, C., Reiser, S. & Prather, E. S. Mineral balances of men and women consuming high fiber diets with complex or simple carbohydrate. J. Nutr. 117, 48–55. https://doi.org/10.1093/jn/117.1.48 (1987).
Black, D. M. & Rosen, C. J. Clinical practice. Postmenopausal osteoporosis. N. Engl. J. Med. 374, 254–262. https://doi.org/10.1056/NEJMcp1513724 (2016).
Piqueras, P. et al. Anthropometric indicators as a tool for diagnosis of obesity and other health risk factors: A literature review. Front. Psychol. 12, 631179. https://doi.org/10.3389/fpsyg.2021.631179 (2021).
Islam, M. R., Moinuddin, M., Saqib, S. M. & Rahman, S. M. Relationship of anthropometric indicators of general and abdominal obesity with hypertension and their predictive performance among albanians: A nationwide cross-sectional study. Nutrients https://doi.org/10.3390/nu13103373 (2021).
Valdez, R. A simple model-based index of abdominal adiposity. J. Clin. Epidemiol. 44, 955–956. https://doi.org/10.1016/0895-4356(91)90059-i (1991).
Flegal, K. M. BMI and obesity trends in Chinese national survey data. Lancet 398, 5–7. https://doi.org/10.1016/s0140-6736(21)00892-8 (2021).
Dhawan, D. & Sharma, S. Abdominal obesity, adipokines and non-communicable diseases. J. Steroid. Biochem. Mol. Biol. 203, 105737. https://doi.org/10.1016/j.jsbmb.2020.105737 (2020).
Ragino, Y. I., Stakhneva, E. M., Polonskaya, Y. V. & Kashtanova, E. V. The role of secretory activity molecules of visceral adipocytes in abdominal obesity in the development of cardiovascular disease: A review. Biomolecules https://doi.org/10.3390/biom10030374 (2020).
Xia, C. et al. Lipid accumulation product is a powerful index for recognizing insulin resistance in non-diabetic individuals. Eur. J. Clin. Nutr. 66, 1035–1038. https://doi.org/10.1038/ejcn.2012.83 (2012).
Sun, J. Y. et al. Association between waist circumference and the prevalence of (Pre) hypertension among 27,894 US adults. Front. Cardiovasc. Med. 8, 717257. https://doi.org/10.3389/fcvm.2021.717257 (2021).
Krakauer, N. Y. & Krakauer, J. C. A new body shape index predicts mortality hazard independently of body mass index. PLoS One 7, e39504. https://doi.org/10.1371/journal.pone.0039504 (2012).
Bouchi, R. et al. Indirect measure of visceral adiposity ‘A Body Shape Index’ (ABSI) is associated with arterial stiffness in patients with type 2 diabetes. BMJ Open Diabetes Res. Care 4, e000188. https://doi.org/10.1136/bmjdrc-2015-000188 (2016).
Nkwana, M. R., Monyeki, K. D. & Lebelo, S. L. Body roundness index, a body shape index, conicity index, and their association with nutritional status and cardiovascular risk factors in South African rural young adults. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18010281 (2021).
Thomas, D. M. et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring) 21, 2264–2271. https://doi.org/10.1002/oby.20408 (2013).
Huang, Q. et al. Lipid accumulation product is a valid predictor of hepatic steatosis and nonalcoholic fatty liver disease. Biomark. Med. 18, 123–135. https://doi.org/10.2217/bmm-2023-0725 (2024).
Mirr, M., Skrypnik, D., Bogdański, P. & Owecki, M. Newly proposed insulin resistance indexes called TyG-NC and TyG-NHtR show efficacy in diagnosing the metabolic syndrome. J. Endocrinol. Invest. 44, 2831–2843. https://doi.org/10.1007/s40618-021-01608-2 (2021).
Wu, W. T. et al. Data mining in clinical big data: The frequently used databases, steps, and methodological models. Mil. Med. Res. 8, 44. https://doi.org/10.1186/s40779-021-00338-z (2021).
Wang, K. et al. Associations of healthy eating index-2015 with osteoporosis and low bone mass density in postmenopausal women: A population-based study from NHANES 2007–2018. Front. Nutr. 11, 1388647. https://doi.org/10.3389/fnut.2024.1388647 (2024).
Wang, J., Xing, F., Sheng, N. & Xiang, Z. Associations of dietary oxidative balance score with femur osteoporosis in postmenopausal women: Data from the national health and nutrition examination survey. Osteoporos Int 34, 2087–2100. https://doi.org/10.1007/s00198-023-06896-3 (2023).
Tang, Y. et al. Systemic immune-inflammation index and bone mineral density in postmenopausal women: A cross-sectional study of the national health and nutrition examination survey (NHANES) 2007–2018. Front. Immunol. 13, 975400. https://doi.org/10.3389/fimmu.2022.975400 (2022).
Looker, A. C. et al. Prevalence of low femoral bone density in older U.S. adults from NHANES III. J. Bone. Miner. Res. 12, 1761–1768. https://doi.org/10.1359/jbmr.1997.12.11.1761 (1997).
Watson, S. L. et al. High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: The LIFTMOR randomized controlled trial. J. Bone Miner. Res. 33, 211–220. https://doi.org/10.1002/jbmr.3284 (2018).
Zwierzchowska, A., Kantyka, J., Rosołek, B., Nawrat-Szołtysik, A. & Małecki, A. Sensitivity and specificity of anthropometric indices in identifying obesity in women over 40 years of age and their variability in subsequent decades of life. Biology (Basel) https://doi.org/10.3390/biology11121804 (2022).
Zhang, J. et al. Associations between novel anthropometric indices and the prevalence of gallstones among 6848 adults: A cross-sectional study. Front. Nutr. 11, 1428488. https://doi.org/10.3389/fnut.2024.1428488 (2024).
Tang, L. & Zeng, L. Comparative efficacy of anthropometric indices in predicting 10-year ASCVD risk: Insights from NHANES data. Front. Cardiovasc. Med. 11, 1341476. https://doi.org/10.3389/fcvm.2024.1341476 (2024).
Kahn, H. S. The, “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disord. 5, 26. https://doi.org/10.1186/1471-2261-5-26 (2005).
Xiao, P. L. et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: A systematic review and meta-analysis. Osteoporos. Int. 33, 2137–2153. https://doi.org/10.1007/s00198-022-06454-3 (2022).
Rachner, T. D., Khosla, S. & Hofbauer, L. C. Osteoporosis: Now and the future. Lancet 377, 1276–1287. https://doi.org/10.1016/s0140-6736(10)62349-5 (2011).
Schmitt, N. M., Schmitt, J. & Dören, M. The role of physical activity in the prevention of osteoporosis in postmenopausal women-An update. Maturitas 63, 34–38. https://doi.org/10.1016/j.maturitas.2009.03.002 (2009).
Management of Postmenopausal Osteoporosis. ACOG clinical practice guideline No. 2. Obstet. Gynecol. 139, 698–717. https://doi.org/10.1097/aog.0000000000004730 (2022).
Liu, C. et al. Effects of combined calcium and vitamin D supplementation on osteoporosis in postmenopausal women: A systematic review and meta-analysis of randomized controlled trials. Food Funct. 11, 10817–10827. https://doi.org/10.1039/d0fo00787k (2020).
Clynes, M. A. et al. The epidemiology of osteoporosis. Br. Med. Bull. 133, 105–117. https://doi.org/10.1093/bmb/ldaa005 (2020).
Howe, T. E. et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Datab. Syst. Rev. https://doi.org/10.1002/14651858.CD000333.pub2 (2011).
Sridharan, K. et al. Utility of anthropometric indicators in predicting osteoporosis in ambulant community dwelling rural postmenopausal women from southern India. Trop. Dr. 50, 228–232. https://doi.org/10.1177/0049475520922769 (2020).
Lin, Y. A. et al. The effectiveness of a group kickboxing training program on sarcopenia and osteoporosis parameters in community-dwelling adults aged 50–85 years. Front. Med. (Lausanne) 9, 815342. https://doi.org/10.3389/fmed.2022.815342 (2022).
Aspray, T. J. & Hill, T. R. Osteoporosis and the ageing skeleton. Subcell. Biochem. 91, 453–476. https://doi.org/10.1007/978-981-13-3681-2_16 (2019).
Warensjö, E. et al. Dietary calcium intake and risk of fracture and osteoporosis: Prospective longitudinal cohort study. BMJ 342, d1473. https://doi.org/10.1136/bmj.d1473 (2011).
Chen, P. J., Lu, Y. C., Lu, S. N., Liang, F. W. & Chuang, H. Y. Association between osteoporosis and adiposity index reveals nonlinearity among postmenopausal women and linearity among men aged over 50 years. J. Epidemiol. Glob. Health 14, 1202–1218. https://doi.org/10.1007/s44197-024-00275-9 (2024).
Ding, Z. et al. Negative association between Body Roundness Index and bone mineral density: Insights from NHANES. Front Nutr 11, 1448938. https://doi.org/10.3389/fnut.2024.1448938 (2024).
Huang, Y. & Ye, J. Association between hypertension and osteoporosis: A population-based cross-sectional study. BMC Musculoskelet. Disord. 25, 434. https://doi.org/10.1186/s12891-024-07553-4 (2024).
Litwin, M. & Kułaga, Z. Obesity, metabolic syndrome, and primary hypertension. Pediatr. Nephrol. 36, 825–837. https://doi.org/10.1007/s00467-020-04579-3 (2021).
Wang, K., Xia, F., Li, Q., Luo, X. & Wu, J. The associations of weekend warrior activity patterns with the visceral adiposity index in US adults: Repeated cross-sectional study. JMIR Public Health Surveill. 9, e41973. https://doi.org/10.2196/41973 (2023).
Chen, P. J., Lu, Y. C., Lu, S. N., Liang, F. W. & Chuang, H. Y. Association between osteoporosis and adiposity index reveals nonlinearity among postmenopausal women and linearity among men aged over 50 years. J. Epidemiol. Glob. Health https://doi.org/10.1007/s44197-024-00275-9 (2024).
Xia, P., Jiang, Y., Cai, F., Peng, S. & Xu, Z. Construction and verification of risk prediction model of osteoporotic fractures in patients with osteoporosis in China. Front. Public Health 12, 1380218. https://doi.org/10.3389/fpubh.2024.1380218 (2024).
Hung, T. N. K. et al. An AI-based prediction model for drug-drug interactions in osteoporosis and paget’s diseases from SMILES. Mol. Inform. 41, e2100264. https://doi.org/10.1002/minf.202100264 (2022).
Shirinezhad, A. et al. A systematic review of the association between insulin resistance surrogate indices and bone mineral density. Front. Endocrinol. (Lausanne) 15, 1499479. https://doi.org/10.3389/fendo.2024.1499479 (2024).
Du, D. et al. TNF-α suppresses osteogenic differentiation of MSCs by accelerating P2Y(2) receptor in estrogen-deficiency induced osteoporosis. Bone 117, 161–170. https://doi.org/10.1016/j.bone.2018.09.012 (2018).
Yuan, S. & Shen, J. Bacteroides vulgatus diminishes colonic microbiota dysbiosis ameliorating lumbar bone loss in ovariectomized mice. Bone 142, 115710. https://doi.org/10.1016/j.bone.2020.115710 (2021).
Author information
Authors and Affiliations
Contributions
J.Z., Y.W., and J.G. contributed equally to the conceptualization and design of the study. H.L. performed the majority of experiments and collected data. D.T. prepared Figs. 1, 2, and 3 and contributed to data interpretation. Z.S. performed data analysis and contributed to manuscript revision. Z.J. assisted with data validation and literature review. H.C. supervised the project and provided critical feedback on the final manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The ethics review board of the National Center for Health Statistics approved all NHANES protocols. All procedures performed in this study involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
The data used in this study were obtained from the publicly accessible National Health and Nutrition Examination Survey (NHANES) database, which is maintained by the Centers for Disease Control and Prevention (CDC). The NHANES data can be accessed via the following link: https://www.cdc.gov/nchs/nhanes/index.htm. NHANES data are available for public use and do not require special access permissions. No additional original data were generated during this study. All data supporting the findings of this research are based on secondary analysis of NHANES data. Data privacy and confidentiality are maintained by NHANES, and all identifying information has been removed to ensure participant anonymity. Therefore, no restrictions apply to the sharing of this data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, J., Wang, Y., Guo, J. et al. The association between ten anthropometric measures and osteoporosis and osteopenia among postmenopausal women. Sci Rep 15, 10994 (2025). https://doi.org/10.1038/s41598-025-94218-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94218-4
This article is cited by
-
miR-629-3p affects postmenopausal osteoporosis through targeted regulation of BACH1
Journal of Orthopaedic Surgery and Research (2025)