Abstract
There are well-documented differences in idiopathic pulmonary fibrosis (IPF) between sexes. The sex-specific prevalence of interstitial lung disease (ILD) subtypes in patients who require a full diagnostic work-up, including transbronchial cryobiopsy (TCB), after initial multidisciplinary discussion (MDD) is still unknown. Retrospective analysis of sex dispareties in patients with ILD who received an interdisciplinary indication for lung biopsy and underwent bronchoalveolar lavage, TCB and, if necessary, surgical lung biopsy at our ILD centre in Heidelberg between 11/17 and 12/21. The analysis included clinical parameters, visual assessment of computed tomography (CT), automated histogram analyses of lung density by validated software and final MDD-ILD classifications. A total of 402 patients (248 men, 154 women; mean age 68 ± 12 years) were analysed. Smoking behaviour was similar between the sexes, but women were more exposed to environmental factors, whereas men were more exposed to occupational factors. Women had higher rates of thyroid disease (29.9% vs. 12.5%; p < 0.001) and extrathoracic malignancies (16.2% vs. 9.3%; p = 0.041), but lower rates of coronary heart disease (7.1% vs. 19.8%; p < 0.001), stroke (1.3% vs. 6.5%; p = 0.014) and sleep apnoea (5.8% vs. 17.7%; p < 0.001). There were no sex differences regarding CT lung density. On visual inspection, women were less likely to have reticular opacities (65% vs. 76%; p = 0.017) and features of usual interstitial pneumonia (17% vs. 34%; p < 0.001). Among final diagnoses, hypersensitivity pneumonitis was more common in women (34.4%) compared to men (21.8%; p = 0.007). In contrast, IPF was more common in men (22.6%) than in women (7.1%; p < 0.001), and unclassifiable interstitial lung disease was also more frequent in men (21.8%) compared to women (6.5%; p < 0.001). This study highlights significant sex-based differences in the prevalence and characteristics of ILD requiring comprehensive diagnostic work-up. These findings underscore the importance of considering sex-specific factors in the diagnosis and management of ILD.
Similar content being viewed by others
Introduction
The group of interstitial lung diseases (ILDs) comprises a large and very heterogeneous group of entities with different causes and pathophysiological backgrounds. In the case of ILDs with a known aetiology, such as connective tissue diseases (CTDs) and pneumoconiosis, it is known that sex and gender influence the disease, particularly with regard to different exposure and risk factors. Within the affected population, men were more likely to work in industrial and manual occupations and therefore have a higher risk of exposure to silica and asbestos which are associated with ILDs. Women, on the other hand, are much more likely to have autoimmune diseases and corresponding CTD ILDs. However, despite the higher prevalence of rheumatoid arthritis (RA) and systemic sclerosis (SSc) in women, male sex is a risk factor for developing ILDs when having one of these CTDs1,2.
There are significant sex differences in the prevalence of idiopathic interstitial pneumonias (IIPs), such as idiopathic pulmonary fibrosis (IPF), idiopathic non-specific interstitial pneumonitis (iNSIP) or smoking-related subtypes of ILD. These are best studied in IPF, a disease that occurs predominantly in older male smokers; approximately 70% of patients enrolled in large prospective cohorts are male3. Sex differences in granulomatous ILD are best studied in hypersensitivity pneumonitis (HP) and sarcoidosis. Sarcoidosis is more common in women, beyond which there are also sex differences in the prevalence of extrapulmonary phenotypes, including cardiac and cutaneous sarcoidosis4. Although the sex ratio in HP is probably balanced, the occupational exposure to certain aetiological antigens in particular is different in men and women, which can lead to different clinical manifestations and outcomes5. In the group of other rarer entities, the sex distribution in lymphangioleiomyomatosis (LAM), which almost exclusively affects women, is a classic example of the influence of sex in ILDs.
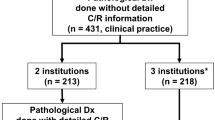
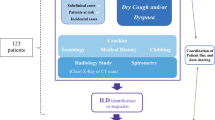
The careful categorisation of ILDs requires a thorough anamnestic and clinical examination and comprehensive expertise in this area6. In view of the complexity of the underlying diseases and their broad differential diagnosis, the diagnosis is made in a multidisciplinary ILD board (MDD) after demonstration of all relevant clinical and radiological findings. Primary unclassifiable ILDs represent a minority group in multidisciplinary discussions, with the need for further invasive diagnostic procedures, such as transbronchial lung cryobiopsy (TCB) or surgical lung biopsy (SLB)7, indicated in less than 30% of cases, as reported in the literature. We chose to focus on this cohort due to the complexity and uncertainty surrounding their diagnosis. The aim of this monocentric retrospective observational study was to investigate sex-specific aspects regarding prevalence and characteristics of different ILD entities in such a cohort of patients with yet undiagnosed ILD with the indication for further invasive work-up. For this purpose, the data of patients presenting to our centre for bronchoscopy with TCB were systematically analysed.
Methods
Study design and participants
This is a retrospective analysis of consecutive patients with suspected ILD evaluated at the Thorax Clinic of the University of Heidelberg, a tertiary referral centre for interstitial lung disease. All patients who underwent transbronchial lung cryobiopsy between November 2017 and December 2021 were included. In case of inconclusive histological findings, the patients were offered a surgical lung biopsy by video-assisted thoracoscopic surgery (VATS) for further classification after MDD. The study was approved by the institutional review board (S-382/2023) and conducted in accordance with the principles of the Declaration of Helsinki. Due to its retrospective design, the requirement for informed consent was waived by the Ethics Committee of the University of Heidelberg.
Pulmonary function tests
Pulmonary function tests were performed using a Jaeger MasterScreen Body System (CareFusion, Rolle, Switzerland). Lung volumes were assessed by whole-body plethysmography and diffusion capacity for carbon monoxide (DLCO) by the single breath technique. All measurements were performed according to the American Thoracic Society (ATS) and the European Respiratory Society (ERS) guidelines8,9,10, using Global Lung Function Initiative (GLI) equations to express the results as % predicted11,12.
Imaging
A standardised non-contrast thin-section computed tomography (SOMATOM Definition AS, Siemens Healthineers AG) was used for diagnosis if no external imaging of comparable quality was available. The CT images of all patients were presented and evaluated in an interdisciplinary case discussion involving one of three different radiologists, each with several years of experience in chest imaging. Moreover, CT datasets (i40f kernel) were post-processed using the validated in-house software YACTA (version v2.9.4.65) as previously described13,14,15,16. The segmentation of the airway tree and lung lobes was performed using a fully automated process. The segmentation results were then visually checked for inconsistencies by a reader (J.R.). The houndsfield units (HU) value of the range 10th-90th percentile in 5th percentiles steps was derived from the histogram recording the densities of all lung voxels for each Modified Discrete Cosine Transformation (MDCT). The analyses included the density values of the 40th and 80th percentiles of the MDCT attenuation frequency histogram, as these have been identified in previous studies as parameters of disease extent15,17.
Multidisciplinary board discussion
The multidisciplinary discussion (MDD) team consisted of two experienced pulmonologists, a thoracic radiologist, a thoracic pathologist, and, in the case of suspected systemic disease, a rheumatologist. All cases were discussed at least twice to ensure a thorough evaluation. At the MDD, each patient’s detailed medical history, including exposures and signs of systemic disease, pulmonary function tests, laboratory values, 6-min walk test, echocardiography and high-resolution computed tomography were reviewed according to current national and international guidelines7,18,19. Further invasive diagnostic procedures including transbronchial cryobiopsy were also indicated in the multidisciplinary discussions. Finally, all data including histology were discussed again in a second MDD and the final diagnosis was again made according to national and international guidelines7,18,19.
Bronchoscopy
Bronchoscopy and periprocedural preparations were performed according to an institutional standard as previously described20. Endoscopists were instructed to collect samples from both the upper and lower lobes of the most affected lung side, utilizing fluoroscopic guidance for precision. They were further advised to obtain samples from the distal part of the lung parenchyma, ensuring a distance of at least 1 cm from the pleura to ensure representation of the peripheral lung areas, as recommended21. The commercially available 1.7 or 1.9-mm cryoprobe (ERBE, Solingen, Germany) were used. Two hours after the end of the procedure, a chest x-ray was performed to rule out a pneumothorax.
Categorisation of ILD
ILDs were categorised into four categories according to the national German ILD guideline6,22: Category I: ILDs associated with known causes, Category II: idiopathic forms, Category III: granulomatous ILDs, Category IV: others.
Statistical analysis
Data in the tables are presented as numbers and percentages or means and standard deviations (SD). Data were analysed with Fisher’s exact test for categorical variables or a two-tailed t test for independent samples in the case of continuous variables. All analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY, USA); p < 0.05 was considered statistically significant.
Results
Medical history, clinical and functional characteristics
A total of 402 patient cases, including 145 women and 248 men, were included in the analysies. There were no differences between men and women with regards to age or duration of symptoms before presentation to the centre. Men had a significantly higher body mass index than women (29.3 ± 4.7 vs. 27.8 ± 6.1; p = 0.016). Smoking status and pack-years did not differ between men and women. In the cohort, women reported significantly more environmental (55.8% vs. 41.9%; p = 0.008) and men more occupational (9.3% vs. 1.9%, p = 0.003) exposures, as well as more frequent dust exposures in both areas (19.8% vs. 6.5%, p < 0.001). There were no differences between the sexes in the results of the autoimmune serologies performed. Overall, women had lower values for static and dynamic lung function parameters and diffusion capacity, but there were no differences compared to the corresponding reference values. In a total of 18 patients (4.5%), a surgical lung biopsy was indicated following a transbronchial cryobiopsy (TCB) because the TCB did not yield conclusive results, as determined by the multidisciplinary discussion (MDD). Patient characteristics, stratified by sex, are shown in Table 1.
Comorbidities
Several comorbidities were systematically analysed and differences were found between the sexes: Men were significantly more likely to have coronary heart disease (3.6% vs. 0.6%, p < 0.001), sleep apnoea (1.3% vs. 0.4%, p < 0.001) and a history of stroke (6.5% vs. 1.3%, p = 0.014). Women were significantly more likely to have malignancies (16.2% vs. 9.3%, p = 0.041) and thyroid disease (29.9% vs. 12.5%; p < 0.001). The distribution of comorbidities by sex is shown in Table 2.
Imaging
CT was assessed visually by experienced thoracic radiologists as part of the radiological findings and during MDD. Reticular opacities were described more frequently in male patients (76.2 vs. 64.9%; p = 0.017), while there were no differences between the sexes with regard to ground-glass opacities or honeycombing. In the evaluation of the radiological patterns, a UIP pattern (either probable or indeterminate) was described more frequently in men (33.9% vs. 16.9%; p < 0.001). Table 3 shows radiological findings and results of lung density histogram analyses.
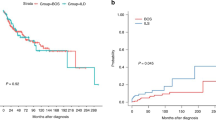
Final diagnoses
Including the diagnosis of unclassifiable ILD, which was assigned to category II, all but 11 cases that were ultimately not diagnosed with ILD after final assessment, could be assigned to the 4 categories. These were interstitial lung disease with known causes in 12.4% of cases, idiopathic interstitial lung disease in 52.2% of cases, granulomatous interstitial lung disease in 29.9% of cases and others in 2.7% of cases. There were relevant sex-specific differences with regard to ILD categories. The most common diagnostic category, category II, was significantly more common in male patients (60.9% vs. 39%; p < 0.001). The most common diagnosis in this category was IPF, which was diagnosed in 21.8% of men and 7.1% of women (p < 0.001). The second most common diagnosis in this category unclassifiable ILD was also more common in men and was diagnosed in 21.8% of men and 6.5% of women (p < 0.001). In addition, 10.1% of men and 12.3% of women were diagnosed with NSIP, with no differences between the sexes. In contrast, the second most common category, category III, was diagnosed significantly more frequently in women (37% vs. 25.4%; p = 0.007). In terms of the most common diagnoses in this category, HP was more frequent in women (34.4% vs. 21.8%; P = 0.007). There was no sex difference for sarcoidosis, which was diagnosed in 3.2% of men and 1.9% of women. In the third most common diagnostic category, Category I (known causes), the sex prevalences were balanced and there were no sex differences for the individual entities, CTD RA-ILD or drug-induced ILD. Of the category IV diagnoses, lympangioleyomyomatosis was the most common diagnosis, diagnosed in women. Figure 1 provides an overview of the diagnosis categories; an overview of the categories with the most common individual entities is shown in Table 4.
Discussion
The objective of the present study was to investigate sex differences in a group of patients with interstitial lung disease with the indication for an extended work-up, including histological confirmation, at a tertiary centre for ILDs with further expert status in interventional endoscopy and thoracic surgery. By focusing on this certain subgroup ILDs where further investigation is indicated, typically a minority in most centres, we aim to explore potential sex-specific differences that could provide valuable insights into the management and diagnostic approach for these patients, particularly those who may not be suitable candidates for invasive diagnostic procedures. Our findings highlight significant sex-based disparities in various aspects of the disease, including risk factors, comorbidities, radiological patterns, and final diagnoses. Notably, idiopathic pulmonary fibrosis (IPF) emerged as the most prevalent diagnosis among men, while hypersensitivity pneumonitis was more frequently diagnosed in women. Additionally, men were more likely to be diagnosed with unclassifiable interstitial lung disease compared to women.
With regard to risk factors, men were more frequently exposed to occupational exposure, while women reported higher exposure to household antigens. Smoking behavior was similar across genders, and CT analyses corroborated the medical history data, showing no differences in the emphysema index between men and women. Comorbidity patterns also differed, with men more likely to have cardiovascular disease such as coronary heart disease and stroke, as well as sleep apnoea. In IPF, the prevalence of coronary heart disease (CHD) was generally high (60%), potentially being a consequence of smoking, which is associated with poorer survival; but an unrecognised comorbid condition in 20% of cases23. In our cohort, the prevalence of CHD and IPF was higher in men compared to women, with no differences in smoking behavior between the sexes. We found a high burden of previous malignancies, with 3 cases of lung cancer diagnosed and a total of 48 patients having a history of another malignancy. With 16.2% of women having a previous extrathoracic malignancy, it is also striking that women in this cohort were particularly affected by malignancy. Women were also more likely to have thyroid disease. We observed a significant burden of previous malignancies, including 3 cases of lung cancer and a total of 48 patients with a history of other malignancies. Comorbidities in interstitial lung disease (ILD) may reflect shared risk factors such as smoking but can also represent manifestations of systemic diseases like sarcoidosis or rheumatoid arthritis-related ILD. Furthermore, systemic inflammation is an important factor linking various comorbidities with ILD24. In our study, the higher prevalence of thyroid disease in women may be related to the generally increased risk of autoimmune disorders in females25. The notable rate of malignancies in women is surprising and deserves further investigation. One potential explanation could be systemic inflammation, which is known to be involved in tumorigenesis26.
We observed no sex differences in the severity of lung disease among our patients, as indicated by static and dynamic lung volumes, diffusion capacity, and histogram analyses of lung density. The qualitative differences became evident only through the analysis by an experienced thoracic radiologist, with reticular opacities and UIP features being more prevalent in men. These radiological indicators of IPF corresponded with the final diagnoses. There were no gender-specific differences in the systematically conducted autoantibody screenings. It is important to note that patients with ILD associated with RA, CTD, or SSc typically do not require histological confirmation of the diagnosis. Therefore, those with autoimmune diseases might represent a specific subset of cases. It is also noteworthy that although a diagnosis could be made in nearly all cases after the second multidisciplinary discussion (MDD), a diagnosis of ‘unclassifiable ILD’ was notably more frequent in men. It is important to critically assess that our MDD process is not gender-blind, which could potentially introduce biases in the final diagnoses. Research by Assayag et al. indicates that patient sex independently influences the diagnosis of IPF. Their study found that pulmonologists were more likely to diagnose idiopathic pulmonary fibrosis in male patients, even after adjusting for factors such as age, smoking history, exposures, and autoantibodies. This suggests that clinicians may place significant emphasis on male sex when assessing the pre-test diagnostic probability of this disease27. This could ultimately lead to underdiagnosis of IPF in women and overdiagnosis in men. The relatively low proportion of women in IPF cohorts has resulted in a significant gender bias in the existing literature on IPF, with the majority of studies focusing on male subjects. Consequently, there is a dearth of research that explicitly examines the characteristics and outcomes of women with IPF. Data from the French ILD cohort "COhorte Fibrose (COFI)" show that IPF looks different in women than in men, the majority of women in the COFI cohort were neversmokers in 65% of cases, compared to a rate of 21% in men28. They were also less likely to present with honeycombing or concomitant emphysema. These findings are supported by data from the French Rare Disease Cohort—Interstitial Lung Disease (RaDiCo-ILD), where comorbid emphysema, and honeycombing on HRCT are more common characteristics of males than females with IPF29. Although histological characteristics of IPF may vary between sexes, we assume that women with IPF, potentially underdiagnosed due to distinct clinical phenotypes and possible investigator bias, would particularly benefit from invasive diagnostic methods for accurate diagnosis. The higher prevalence of HP in women in our study was surprising. Although there are data from some registries, such as the Danish one, where men have a slightly higher prevalence (57%) than women30, it is generally assumed that the gender-specific prevalence of this entity is relatively balanced31. However, antigen-indeterminate cases are reported more often in older women with lower lung function, less alveolar lymphocytosis and greater fibrosis on imaging32. The fact that histological clarification may be indicated in these cases in particular may explain the higher prevalence of the disease in our collective.
Limitations
This study has several limitations. First, the sex data are based on patient self-report, which may introduce potential biases. While all patients were examined according to internal center standards, the quality of the data cannot be compared with that of a controlled study. CT scans were interpreted by experienced radiologists, who, like other members of the MDD team, may have been influenced by potential bias. Additionally, diagnoses of comorbidities were primarily based on pre-existing medical records, which were not consistently reviewed at the center. The monocentric nature of the study and the absence of a control group or matched cohorts limit the generalizability of the findings. Furthermore, 62% of the patients were male, and patients deemed ineligible for transbronchial cryobiopsy due to comorbidities, disease severity, or refusal were not included. The monocentric nature of the study and the absence of a control group or matched cohorts limit the generalizability of the findings. Furthermore, 62% of the patients were male, and patients deemed ineligible for transbronchial cryobiopsy (TCB) due to comorbidities, disease severity, or refusal were not included. Finally, prospective, multicentric studies are needed to validate these findings and explore the role of sex-specific differences in ILD diagnosis and outcomes.
Conclusion
This work offers a preliminary overview of sex differences in a well- characterised real-world cohort investigated at a single centre using transbronchial cryobiopsy. The high prevalence of IPF among men and, conversely, the more frequent diagnosis of hypersensitivity pneumonitis (among women had therapeutic consequences, making invasive diagnostic work-up helpful for these patients. Overall, it is possible that men and women may require different therapeutic approaches. However, it is important to emphasize that treatment decisions must be made based on the individual diagnosis, considering the unique characteristics of each patient and their response to therapy. The study emphasizes the importance of understanding these disparities to improve patient outcomes and guide future research directions in the field of interstitial lung disease.
Data availability
The full data set supporting the conclusions of this article is available upon request from Franziska C. Trudzinski.
Abbreviations
- ATS:
-
American Thoracic Society
- BAL:
-
Bronchoalveolar lavage
- BMI:
-
Body Mass Index
- CHD:
-
Coronary heart disease
- COFI:
-
Cohorte Fibrose
- CTD:
-
Connective tissue diseases
- DLCO:
-
Diffusion capacity for carbon monoxide
- ERS:
-
European Respiratory Society
- FEV1:
-
Forced expiratory volume in the first second
- FVC:
-
Forced vital capacity
- GLI:
-
Global Lung Function Initiative
- HP:
-
Hypersensitivity Pneumonitis
- HU:
-
Hounsfield-Unit
- IIPs:
-
Idiopathic Interstitial pneumonias
- ILD:
-
Interstitial lung disease
- iNSIP:
-
Idiopathic non-specific interstitial pneumonitis
- IPF:
-
Idiopathic pulmonary fibrosis
- LAM:
-
Lymphangioleiomyomatosis
- MDCT:
-
Multidetector computed tomography
- MDD:
-
Multidisciplinary discussion
- RA:
-
Rheumatoid arthritis
- RaDiCo-ILD:
-
Rare Disease Cohor-Interstitial Lung Disease
- SD:
-
Standard deviations
- SLB:
-
Surgical lung biopsy
- SSc:
-
Systemic sclerosis
- TCB:
-
Transbronchial cryobiopsy
- UIP:
-
Usual interstitial pneumonia
- VATS:
-
Video-assisted thoracoscopic surgery
References
Ozaki, M. et al. Sexual dimorphism in interstitial lung disease. Biomedicines 10, 12 (2022).
Khanna, D. et al. Etiology, risk factors, and biomarkers in systemic sclerosis with interstitial lung disease. Am. J. Respir. Crit. Care Med. 201(6), 650–660 (2020).
Jo, H. E. et al. Baseline characteristics of idiopathic pulmonary fibrosis: analysis from the Australian Idiopathic Pulmonary Fibrosis Registry. Eur. Respir. J. 49, 2 (2017).
Xiong, Y. et al. Sex differences in the genetics of sarcoidosis across European and African ancestry populations. Front. Med. (Lausanne) 10, 1132799 (2023).
Lacasse, Y. & Cormier, Y. Hypersensitivity pneumonitis. Orphanet. J. Rare Dis. 1, 25 (2006).
Kreuter, M. et al. Consensus guideline on the interdisciplinary diagnosis of interstitial lung diseases. Pneumologie 77(5), 269–302 (2023).
Raghu, G. et al. Idiopathic pulmonary fibrosis (an update) and progressive pulmonary fibrosis in adults: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am. J. Respir. Crit. Care Med. 205(9), e18–e47 (2022).
Macintyre, N. et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur. Respir. J. 26(4), 720–735 (2005).
Miller, M. R. et al. Standardisation of spirometry. Eur. Respir. J. 26(2), 319–338 (2005).
Wanger, J. et al. Standardisation of the measurement of lung volumes. Eur. Respir. J. 26(3), 511–522 (2005).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur. Respir. J. 40(6), 1324–1343 (2012).
Stanojevic, S. et al. Official ERS technical standards: global lung function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur. Respir. J. 50, 3 (2017).
Weinheimer, O. et al. About objective 3-d analysis of airway geometry in computerized tomography. IEEE Trans. Med. Imaging 27(1), 64–74 (2008).
Lim, H. J. et al. Fully automated pulmonary lobar segmentation: influence of different prototype software programs onto quantitative evaluation of chronic obstructive lung disease. PLoS One. 11(3), e0151498 (2016).
Colombi, D. et al. Visual vs fully automatic histogram-based assessment of idiopathic pulmonary fibrosis (IPF) progression using sequential multidetector computed tomography (MDCT). PLoS One 10(6), e0130653 (2015).
Heussel, C. P. et al. Fully automatic quantitative assessment of emphysema in computed tomography: comparison with pulmonary function testing and normal values. Eur. Radiol. 19(10), 2391–2402 (2009).
Ley-Zaporozhan, J. et al. Fully automated segmentation of pulmonary fibrosis using different software tools. Respiration 100(7), 580–587 (2021).
Travis, W. D. et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 188(6), 733–748 (2013).
Raghu, G. et al. Diagnosis of idiopathic pulmonary fibrosis an official ATS/ERS/JRS/ALAT clinical practice guideline. Am. J. Respir. Crit. Care Med. 198(5), e44–e68 (2018).
Walscher, J. et al. Transbronchial cryobiopsies for diagnosing interstitial lung disease: real-life experience from a tertiary referral center for interstitial lung disease. Respiration 97(4), 348–354 (2019).
Hetzel, J. et al. Transbronchial cryobiopsies for the diagnosis of diffuse parenchymal lung diseases: expert statement from the cryobiopsy working group on safety and utility and a call for standardization of the procedure. Respiration 95(3), 188–200 (2018).
Kreuter, M., Ladner, U. M., Costabel, U., Jonigk, D. & Heussel, C. P. The diagnosis and treatment of pulmonary fibrosis. Dtsch Arztebl Int. 118, 152–162 (2021).
Kizer, J. R. et al. Association between pulmonary fibrosis and coronary artery disease. Arch. Intern. Med. 164(5), 551–556 (2004).
Margaritopoulos, G. A., Antoniou, K. M. & Wells, A. U. Comorbidities in interstitial lung diseases. Eur. Respir. Rev. 26, 143 (2017).
Kronzer, V. L., Bridges, S. L. Jr. & Davis, J. M. 3rd. Why women have more autoimmune diseases than men: an evolutionary perspective. Evol. Appl. 14(3), 629–633 (2021).
O’Byrne, K. J. & Dalgleish, A. G. Chronic immune activation and inflammation as the cause of malignancy. Br. J. Cancer 85(4), 473–483 (2001).
Assayag, D., Morisset, J., Johannson, K. A., Wells, A. U. & Walsh, S. L. F. Patient gender bias on the diagnosis of idiopathic pulmonary fibrosis. Thorax 75(5), 407–412 (2020).
Sese, L. et al. Gender differences in idiopathic pulmonary fibrosis: are men and women equal?. Front. Med. (Lausanne) 8, 713698 (2021).
Cottin, V. et al. Impact of gender on the characteristics of patients with idiopathic pulmonary fibrosis included in the RaDiCo-ILD cohort. Respiration 101(1), 34–45 (2022).
Rittig, A. H., Hilberg, O., Ibsen, R. & Lokke, A. Incidence, comorbidity and survival rate of hypersensitivity pneumonitis: a national population-based study. ERJ Open Res. 5, 4 (2019).
Kawano-Dourado, L., Glassberg, M. K., Assayag, D., Borie, R. & Johannson, K. A. Sex and gender in interstitial lung diseases. Eur. Respir. Rev. 30, 162 (2021).
Walters, G. I. et al. Characteristics of hypersensitivity pneumonitis diagnosed by interstitial and occupational lung disease multi-disciplinary team consensus. Respir. Med. 155, 19–25 (2019).
Funding
Open Access funding enabled and organized by Projekt DEAL.
The study was funded by the E&H Knorr Stiftung, Weinheim, Germany. The funder had no influence on the conception, design, data collection, analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
JR, MP and FCTandwere involved in the design of the study, the interpretation of the data, drafting and finalisation of the manuscript, approved the final submitted version and agreed to be accountable for all aspects of the work. KB, ME, CPH, MG, JDMZ, MOW, KK, KKo, LVK, MA, FJH, RE and MK were involved in the interpretation of the data, drafting and finalisation of the manuscript, approved the final submitted version, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
MP received lecture fees from AstraZeneca, Boehringer Ingelheim and Novartis. FCT received payment lectures, or reimbursement of travel expenses from Novartis AG, GlaxoSmithKline, Chiesi, Boehringer Ingelheim GmbH, Grifols and AstraZeneca, CSL Behring and Grifols Deutschland GmbH. MOW reports study grants by Vertex Pharmaceuticals, and advisory board membership at Boehringer Ingelheim and Vertex Pharmaceuticals, KK received lecture fees from AstraZeneca, Boehringer Ingelheim, GSK, Insmed, GlaxoSmithKLine and Chiesi. JDMZ is a board member of the E&H Knorr Stiftung and reports funding by the innovation fund of the G-BA as well as payment or honoraria for lectures from AstraZeneca and reimbursement of travel expenses from CSL Behring. FJH received lecture fees from CSL Behring and Grifols Deutschland GmbH. KKo has received honoraria for lectures from Berlin-Chemie, Astra Zeneca and Boston Scientific, outside the submitted work. MA received lecture fees from Boehringer Ingelheim. KB reports on financial support from the Sarcoidosis Network e.V., consultancy fees from Boehringer-Ingelheim and Astra Zeneca as well as fees for lectures from Boehringer-Ingelheim, Astra Zeneca and Chiesi. CPH has stock ownership in GSK and is a co-inventor of a patent for a method and device for representing the microstructure of the lungs.Dr. Heussel has received consultation and fees from Boehringer Ingelheim, Pfizer, and Exscientia. His research has been funded by Boehringer Ingelheim and Exscientia. He has also received lecture fees from Boehringer Ingelheim and Pfizer. All the remaining authors declare no conflict of interest.
Ethics approval and consent to participate
The study was approved by the Institutional Review Board Ethics Committee of the Medical Faculty of Heidelberg University (S-382/2023). Informed consent was waived by the Ethics Committee due to the retrospective nature of the study. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reinhard, J., Polke, M., Buschulte, K. et al. Sex-specific aspects in a population of patients undergoing evaluation for interstitial lung disease with transbronchial cryobiopsy. Sci Rep 15, 11730 (2025). https://doi.org/10.1038/s41598-025-94575-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94575-0