Abstract
The use of Comprehensive Genomic Profiling (CGP) in clinical practice to detect broad-spectrum therapeutic, prognostic, and predictive biomarkers, including tumor mutational burden (TMB), microsatellite instability (MSI), somatic BRCA (sBRCA) and other homologous recombination repair genes (HRRs) provides a more cost-efficient and tissue-preserving approach than serial single-biomarker analysis. A total of 1000 biopsy-proven cancer patients at the HCG cancer center were profiled in an IRB-approved prospective study. The findings were discussed in the multidisciplinary molecular tumor board (MTB), and recommendations were documented in electronic medical records (EMRs) for clinical management and follow-up. A total of 1747 genomic alterations were detected (mean 1.7 mutations/sample), with 80% of patients having genetic alterations with therapeutic and prognostic implications (Tier I-32%, Tier II-50%). CGP revealed a greater number of druggable genes (47%) than did small panels (14%). Tumor-agnostic markers for immunotherapy (IO) were observed in 16% of the current cohort, based on which IO was initiated. In 13.5% of the cohort, alterations in the HRR pathway including sBRCA (5.5%) were detected providing an option for treatment with platinum or PARP inhibitors. Other significant alterations included those in EGFR, KRAS/BRAF, PIK3CA, cKIT, PDGFRA, ARID1A, ARID2, and FGFR. RNA sequencing revealed 55 + RNA alterations, including those in TMPRSS-ERG, RPS6KB1-VMP1, EML4-ALK, NTRK, PDGFRA and EWSR. Clinical outcome data were available via EMR for 618 patients (62%), out of whom 419 patients had druggable mutations (67%; 95% CI 88.9–93.9%) and 39 patients had 1 or more mutations with prognostic implications. However, only 200 patients (44%; 95% CI 39.1–48.1%) were included in the MTB discussion. Based on genomics reports, the treatment regimen was changed for 137 and 61 patients with and without clinical inputs from the MTB, respectively. The overall change in therapy based on CGP in the clinical cohort was 43%, which was greater in patients enrolled for MTB than in patients who had not undergone MTB. At the interim analysis, with a median follow-up of 18 months (range 12–24 months) after the change in therapy as per genomics report, 97 patients (71%) were found to be alive thus establishing the importance of CGP and MTB in personalized genomics-driven treatment.
Similar content being viewed by others

Introduction
Cancer is a multifactorial disease resulting from the synergistic influence of many genetic and environmental factors (e.g., ultraviolet radiation, cigarette smoke, and viruses). At the cellular level, the disesae is defined by key genetic alterations resulting in the upregulation of pro-oncogenic pathways or the downregulation of tumor suppressor pathways. The accumulation of multiple genetic alterations, including somatic mutations, copy‐number alterations (CNAs), structural variants (SVs), and epigenomic variations makes cancer a disease of the genome and results in disease progression, metastasis, and resistance to therapy. While most genetic alterations are acquired sporadically, approximately 5–10% of cancers have germline variants and are inherited.
With the advent of better diagnostic techniques and increased awareness of this disease, there has been significant development in the early diagnosis of cancer. In addition, remarkable progress has been made in terms of surgical expertise, radiotherapy techniques and chemotherapeutic advances in the past 10 years, which has changed cancer treatment protocols. However, the incidence and cancer-associated morbidity and mortality rates have not improved in the Indian subcontinent as described in global and Indian studies. Additionally, the survival outcomes and prognosis of patients with metastatic cancer have changed marginally. Institutional experience shows that many major drugs have an initial response, but the non-responder rates vary between 30 and 70%.
An important milestone in successful cancer treatment and management is early detection of the disease and understanding the genetic signature and molecular makeup of a specific cancer type. Most cancers present in advanced stages pose a major challenge for effective diagnosis and treatment. Additionally, it has been also known that tumor heterogeneity plays an important role in malignant tumors. Understanding inter- and intra tumoral heterogeneity can help categorize tumor biology and improve the design of diagnosis and treatment plans for cancer, thus benefiting patients1. Tumors with high levels of intratumoral heterogeneity might be a major cause of drug resistance and predispose patients to inferior clinical outcomes2. The identification and characterization of genomic alterations, introduction of FDA-approved biomarker-based companion diagnostics, increasing numbers of molecularly targeted therapies, and discovery of pan cancer biomarkers have facilitated the development of precision oncology for cancer patients3. This has strengthened the foundation of precision medicine/oncology and has resulted in a paradigm shift in treatment protocols from nonspecific chemotherapeutic regimens to targeted therapies that act on novel genomic alterations. Since June 2022, the FDA has approved companion diagnostic tests for 27 biomarkers that enable the selection of targeted therapies for more than 50 FDA-approved drugs indicated for the treatment of 16 solid tumor types. In addition, antibody–drug conjugates (ADCs) are evolving very rapidly and there are over a 100 new ADCs in clinical trials covering a wide variety of tumor types particularly in some highly treatment-refractory diseases4. ADC’s targeting HER2 like trastuzumab-emtansine and trastuzumab-deruxtecan have intensely changed the treatment landscape of breast cancer and improved the overall survival in the second and third-line settings with manageable adverse events5.
The approval of cancer immunotherapy(IO), i.e. immune checkpoint inhibition (ICI), for the treatment of many tumor types has drastically altered therapeutic strategies for cancer. However, not all patients benefit from this therapy to the same extent, and there is a critical need to test predictive biomarkers for neoadjuvant ICI treatment in patients to improve patient selection and develop more personalized immunotherapy strategies. Among these biomarkers, programmed death-ligand (PDL1), tumor-infiltrating lymphocyte (TILS), microsatellite instability (MSI), mismatch repair (MMR) and tumor mutational burden (TMB) have been widely investigated. There are currently multiple lines of evidence on the overall better response rates of TMB-high (TMB-H), MSI-high (MSI-H) and PD-L1-positive tumors treated with immunotherapy6,7. However, only a small fraction of biomarkers determines a patient’s response to IO. An in-depth understanding of other reliable biomarkers at the cellular and genomic levels including serum proteins, tumor-specific receptor expression patterns, factors in the tumor microenvironment, circulating immune and tumor cells, and host genomic factors, is needed to stratify patients into responders and non responders to IO8. An example of a complementary and/or surrogate biomarker is PTEN, which may also contribute to optimal patient selection9.
The discovery of pan cancer biomarkers such as MSI-H, TMB-H, BRAF V600E, NTRK and RET fusions and next generation ADCs has enabled clinicians to adopt approved targeted therapies (TKIs) and surface protein directed ADCs irrespective of tumor histology and site of origin10,11,12. It’s now clear that many of them must be interrogated together so that we understand as much about the molecular makeup of a tumor as possible. The conventional diagnostic technologies such as immunohistochemistry (IHC), in situ hybridization (ISH), fluorescence in situ hybridization (FISH), and RT-PCR for single-gene testing remain the cost effective gold standard platforms for detection of potential predictive and therapeutic biomarkers in routine molecular pathology. However, with the growing number of genomic alterations, introduction of FDA-approved biomarker-based companion diagnostics, increasing numbers of molecularly targeted therapies, and discovery of pancancer biomarkers, there is an unmet need of comprehensive test which can provide detailed information of the cancer “at one go” using low-input, low-quality cancer specimens thus overcoming the “one-gene/one-drug” serial testing model. Given the decreasing costs and turnaround time of Next Generation Sequencing (NGS), improvement in bioinformatics analyses and management of knowledge bases to facilitate the clinical interpretation of genomic results, the move to comprehensive genomic profiling (CGP) is compelling in precision cancer medicine context. Clinical sequencing of tumor DNA to detect hotspot single nucleotide variants (SNVs), small insertions and deletions (INDELs), and copy number variants (CNVs) that confer sensitivity to targeted therapies and RNA sequencing to detect gene fusions have emerged an important class of biomarkers for precision medicine in tumors13. RNA sequencing has higher sensitivity for genes expressed either at low or very high level and can detect known and novel fusion partners, ISH allows for precise localization of a specific segment of nucleic acid within a histologic section.
CGP using TruSight™ Oncology 500, an NGS assay, analyzes 523 cancer-relevant genes from both DNA and RNA in one integrated workflow that includes SNVs, indels, splice variants, fusions, translocations, and emerging immunotherapy biomarkers that rely on analysis of multiple genomic loci, such as TMB and MSI. It therefore provides a more efficient, cost-saving and tissue-saving tumor analysis than serial single-biomarker analyses, particularly in the context of the genomic complexity that is known to exist within tumors.
Here, we describe an analysis of 1000 retrospective cases who underwent CGP at HealthCare Global (HCG), a speciality cancer institute in India, using the TruSight™ Oncology 500 Assay (TSO 500), of which approximately 80% of patients had advanced/metastatic disease and failed to respond to 1–2 lines of therapy. The results were presented to a tumor board, documented in patient records, and discussed in a multidisciplinary clinic with treating physicians. Among the 1000 patients, the most common were breast cancer, pulmonary malignancies, gastrointestinal, head and neck cancers, and female genital tract cancers.
Materials and methods
The study was approved by the Human Research Ethics Committee of the institute (HCG Central Ethics Committee/EC Registration No: ECR/386/Inst/KA/2013/RR‑19, a tertiary comprehensive cancer care hospital in Bangalore, India). The institutional ethics committee recommended the need for consent from patients to retrieve formalin‑fixed, paraffin‑embedded (FFPE) tumor samples obtained from the tumor tissue bank at the hospital’s Department of Pathology. All samples and medical data used in this study have been irreversibly anonymized. All methods were performed in accordance with the relevant guidelines and regulations.
Patient/study subjects and sample preparation
One thousand patients with different tumors aged 21–76 years (median age 55.7 years) diagnosed from September 2020 to September 2022 were counseled for CGP. All the patients underwent pathology review for stage, histological type, hormonal status, and Ki67. The H&E slides of the FFPE samples were examined for the presence of viable tumor cells and scored for the percentage of tumor nuclei by a pathologist who selected the areas of neoplastic cells. Specimens with estimated tumor nuclei ≥ 25% in the selected areas were considered for the study.
Histopathology and immunohistochemistry (IHC)
IHC for ER, PR and Her-2/neu for breast cancer cases; Her-2/neu for gastric cancer; and ALK D5F3 for lung cancer were performed on tissue sections using appropriate primary and secondary antibodies from Biocare, USA (ERSP1 clones for ER, PRSP2 clones for PR and EP3 clones for Her-2/neu, D5F3 clones for the Alk antibody and clone 22C3/SP263 for PDL1). The stained slides, along with the appropriate controls, were reviewed and interpreted by two pathologists as per the Allred Score for ER, PR and Her2 as per the American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) guidelines. Fluorescent in situ hybridization (FISH) was recommended for a score of 2 + (equivocal), where there was incomplete membrane staining in > 10% of the tumor cells.
Fluorescence in situ hybridization (FISH)
Her2/neu by FISH was tested via an FDA-approved PathVysion HER-2 DNA Probe Kit (Abbott PathVysion Kit Catalog number 06N46-03) according to the manufacturer’s protocol and visualized for signals. An epifluorescence microscope (Nikon Eclipse 80i) was used. The signals were enumerated in accordance with the manufacturer’s guidelines and interpreted on the basis of recent ASCO and CAP guidelines14.
ALK translocation by FISH was performed using Vysis ALK Break Apart FISH Probe Kit, and ROS1 translocation by FISH was performed using Vysis ROS1 Break Apart FISH Probe Kit. The signals were enumerated in accordance with the manufacturer’s guidelines and interpreted according to CAP guidelines14. IHC and FISH studies for appropriate markers were performed to confirm the NGS findings.
DNA and/or RNA extraction protocol and quality assessment
FFPE tissue samples were first deparaffinized in xylene, and 3–5-μm-thick sections were used for DNA and/or RNA extraction via a Covaris extraction kit according to the manufacturer’s protocol. The extracted nucleic acid was quantified via Nanodrop to check the 260/280 and 260/230 ratios for possible contamination by proteins, phenols, or other contaminants. The DNA/RNA samples were further quantified via fluorometric methods, such as the use of a Qubit DNA/RNA assay kit. The quality of the extracted DNA samples was assessed using an IlluminaR FFPE QC kit. The DNA integrity number (DIN) was used for accurate and objective assessments of genomic DNA degradation. FFPE samples with DIN values ≥ 4 were taken forward for NEBNext, FFPE repair. The repaired FFPE DNA samples were requantified via a Qubit before shearing and library preparation. To assess RNA quality, the integrity of the ribosomal RNA and RNA integrity number (RIN) values of the samples were examined using AgilentRNA screen tape. For highly degraded samples, the DV200 metric developed by Illumina (DV200 = % of RNA fragments in a sample that are larger than 200 nt) was checked. Purified RNA samples were primed with random hexamers in preparation for cDNA synthesis and reverse transcribed into first-strand cDNA via reverse transcriptase, followed by removal of the RNA template and synthesis of double-stranded cDNA. The purified cDNA fragments were taken forward directly for library preparation.
Next-generation sequencing-comprehensive multigene panel selection
NGS was performed using the TruSight Oncology 500 (Illumina, Inc.) (https://www.illumina.com/products/by-type/clinical-research-products/trusight-oncology-500.html), which analyzes cancer-relevant genes from both DNA and RNA in one integrated workflow. The assay profiles a patient’s tumor genotype to detect genetic alterations in key regions of 523 curated tumor-associated genes. The assay is designed to detect different classes of mutations, including single nucleotide variants (SNVs), copy number variants (CNVs), multinucleotide variants (< 3 bp), small insertions (1–18 bp)/deletions (1–27 bp), MSI and TMB, with an integrated workflow to detect fusions and splice variants in certain targeted genes from the same FFPE sample.
Library preparation
The qualified DNA samples were subjected to fragmentation using a Covaris™ E220 focused ultrasonicator. The purified cDNA fragments and sheared DNA samples were processed for library preparation via a targeted hybrid capture-based NGS assay utilizing a unique molecular index (UMI) to enable the detection of variants present in FFPE tumor samples or fresh tumor tissues at low VAFs with a high degree of sensitivity and specificity. The regions of interest for DNA and RNA were hybridized to biotinylated probes using the TruSight Oncology 500 (Illumina Inc.) and TruSight Tumor 170 (Illumina, Inc.) library prep kits, respectively. Libraries were normalized via a simple bead-based protocol and then pooled and sequenced on an IlluminaNextSeq™ 500/NextSeq 2000 instrument. The gDNA sample HD753 of the Structural Multiplex Reference Standard from Horizon Diagnostics (UK) was used as the DNA control. A Seraseq Fusion RNA Mix sample (Seraseq) with a list of known variants was used as an RNA sensitivity control.
Sequencing and analysis
The sequence data were processed via the analysis pipeline in the local app, as suggested in the vendor workflow (https://support.illumina.com/content/dam/illuminasupport/documents/documentation/software_documentation/trusight/trusight-oncology-500/trusight-oncology-500-local-app-v2.2-user-guide-1000000137777-01.pdf).
DNA analysis
The FASTQ files generated were put for DNA alignment and realignment followed by read collapsing, indel realignment and read stitching. The variant detection steps included small variant calling, small variant filtering, copy number variant calling, TMB, MSI status and contamination detection. Small variants were called on the entire manifest, whereas CNVs were called on 59 genes (https://www.illumina.com/products/by-type/clinical-research-products/trusight-oncology-500.html).
The quality control step outputs Run QC, DNA sample QC and RNA sample QC, which are used to perform sample QC on the basis of the guidelines specified by Illumina (https://supportdocs.illumina.com/SW/ClarityLIMS/ClarityIPP/Content/SW/FrontPages/ClarityLIMS_IPPs.htm).
TMB and MSI
TMB measurement of FFPE samples sequenced with this assay was performed via a vendor-provided tumor-only pipeline designed to call small nucleotide variants and indels while filtering germline variants and removing technical noise. The sequencing data were also used for MSI analysis. For comparison, the same samples were analysed by IHC. Additionally, MSI was assessed using a vendor-provided tumor-only algorithm examining 130 repeat loci covered by TSO 500. The samples were classified as TMB-High or TMB-Low using a cutoff value of 10 mut/Mb and as MSI-High or MSS/MSI-Low using a cutoff value of 20% unstable sites. (https://sapac.illumina.com/content/dam/illumina-marketing/documents/products/appnotes/trusight-oncology-500-tmb-analysis-1170-2018-009.pdf.
RNA analysis
The RNA analysis was performed by read trimming, alignment, duplicate marking, fusion calling, fusion filtering, splice variant calling, and fusion merging to generate gene fusions and splice variants.
As per the specifications of Illumina (https://emea.illumina.com/products/by-type/clinical-research-products/trusight-oncology-500.html), the limit of detection (LOD) for small variant calling was set at 5% and 5 copies per ng of RNA input for the fusions. The analytical validation in the laboratory achieved a sensitivity of 97.6%, a specificity of 100% for small variant calling, an accuracy (second method validation) of 100% and a precision/reproducibility (inter reagent lot, inter operator and inter run) of 98.2%. The analytical sensitivity of CNV calling was established at 100%.
Variant prioritization and interpretation
The sequence data were processed using the TruSight Oncology 500 Analysis Module from Illumina’s Local Run Manager (https://support.illumina.com/content/dam/illuminasupport/documents/documentation/software_documentation/trusight/trusight-oncology-500/trusight-oncology-500-local-app-v2-user-guide-1000000095997-02.pdf). A single merged VCF file including small variants, copy number variants, gene fusions and splice variants was created/generated on the basis of the output files from the DNA and RNA analyses and was uploaded into a proprietary clinical genomics interpretation and reporting platform called Strand Omics (https://clinical.strandomics.com), which includes algorithms to identify variant impact from both public content (ClinVar, HPO, dbSNP, 1000 Genomes, Exome Variant Server, COSMIC and dbNSFP) and proprietary content on genes, diseases, and therapeutic impact of somatic variants. Annotation and prioritization of variants were performed via automated pipelines in StrandOmics for identifying and reporting variants of interest. The therapeutic implications of the variants for a particular clinical diagnosis and relevant clinical information were determined on the basis of the analysis of up-to-date scientific literature from various databases, preclinical studies, and clinical studies. A mutation was considered actionable or significant if it could be linked to a potential response or resistance to a particular therapy or to the prognosis, diagnosis, or subtyping of the disease. The interpretation process employed a filtering strategy to identify and filter out germline polymorphisms using population databases. As per recommendations of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists, interpretation and reporting of sequence variants in cancer were followed and Tier II and Tier III variants were included in the report in addition to Tier I15.
Statistical analysis
The statistical analysis was performed via Jamovi 2.4.1 software. The comparison of proportions between two paired samples was performed via the nonparametric McNamara test. The proportions of patients with PD and without PD were compared via the chi-square test. The results are statistically significant when the p value < 0.05.
Results
Study cohort and patient characteristics
The following study is an analysis of clinical samples that underwent CGP over a 2-year period from September 2020 to September 2022. One thousand samples that matched the inclusion criteria of confirmed malignancy and an adequate tumor burden of > 25% were selected for sequencing. FFPE blocks and fresh tissue transported in RNA later™ were utilized for nucleic acid (DNA and/or RNA) extraction. Patient demographics and tumor spectrum characteristics are listed in Table 1. The most frequently studied cancer types were breast (n = 147, 15%), followed by lung (n = 168,17%), gastrointestinal tract (GIT) (n = 151,15%), female genital tract (FGT) (n = 123,12%), hepato-pancreaticobiliary (HPB) (n = 95,9.5%), head and neck (HN) (115,11%; squamous carcinoma, n = 78, non-squamous, n = 37), and genitourinary tract (GU) (n = 65, 6.5%) cancers. In 35 (3%) patients, the lesions were diagnosed as carcinomas of unknown primary origin. Other cancers (N = 101, 10%) tested included sarcoma (n = 68, 6.8%), tumors of the central nervous system (CNS), melanoma, and neuroendocrine tumors (NETs). The primary site of malignancy was analyzed in 486 cases, and 514 cases were analyzed from the metastatic site. The most common site of metastasis was the liver, followed by the lymph nodes. Approximately 655 (65%) patients had received 1 line of therapy, and 345 (35%) patients had received ≥ 2 lines of therapy prior to CGP. The primary endpoint of the study was to understand the proportion of patients with options for actionable and druggable genomic alterations tested after 1–2 lines of treatment failure.
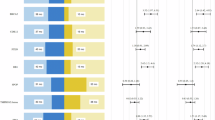
Genomic alterations detected by CGP
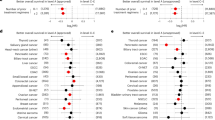
A total of 1747 clinically relevant genomic alterations were detected (1.74 genomic alterations/case) in the cohort. The most frequent genomic alterations detected were TP53 gene mutations (n = 287, 28.7%), homologous recombinant repair (HRR) gene mutations (n = 135, 13.5%), PIK3CA/AKT/mTOR pathway alterations (n = 216, 21.6%), and TMB (= / > 10 mut/Mb) (n = 163, 16%), followed by KRAS, EGFR, and ERBB2 alterations (n = 140, 14%; 100, 10%; 73,7%, respectively). MSI > 20% unstable sites was detected in 11 patients. The mutation spectrum of the cohort is shown in Fig. 1. In accordance with ACMG nomenclature, Tier I and II mutations were annotated in 822 cases, accounting for ~ 80% of the cases. Tier III/VUS were observed in 166 patients (~ 17%), and 12 patients (~ 2%) had no mutations (Tier I-III) (Fig. 2A). Tier I mutations were detected in 322 patients with a tumor-agnostic marker TMB (> 10 mutations/Mb) in 163 patients and MSI (> 20% MSIunstable sites) detected in 11 patients. Other tumor-related marker NTRK1-3 fusions were observed in 2 patients, and BRAF V600E was detected in 18 patients. TMB was the most frequently isolated type I mutation, followed by EGFR, which was observed in 163 patients; somatic alterations in sBRCA, which were detected in 55 patients; ERBB2 (HER2) amplification, which was detected in 73 patients; KRAS mutations, which were detected in 140 patients; and PIK3CA-AKT-mTOR alterations, which were detected in 216 patients. The clinical significance of the mutations found in the studied cohort is shown in Fig. 2B. Actionable targets were obtained in 600 patients, accounting for ~ 60% of the cases in the cohort, and 180 (18%) patients had both actionable and prognostic genetic alterations. Biomarkers with only prognostic indications were found in 43 patients (4%). CGP identified many more potential biomarkers in the cohort than single-gene testing or NGS via a small panel of genes.
sBRCA and HRR
Approximately 14% of patients in the studied cohort were found to have alterations in the sBRCA and HRR pathways. sBRCA1 and sBRCA2 mutations were found in 26 and 29 patients, respectively, accounting for 6% of the HRR pathway in the cohort. Other frequently identified HRR genes included ATM, RAD51, PTEN, ATRX, PALB2, MRE11A, RAD50, and NBN in 56 patients, accounting for 8% of the HRR pathway. The prevalence of the BRCA and HRR genes in different cancers is illustrated in Fig. 3A,B.
TMB and MSI
In the clinical cohort,160 (16%) patients had high TMB (≥ 10 mut/Mb), and 3 patients had borderline TMB (10 mut/Mb). The TMB varied from 10.1 to 656 mut/Mb in different cancers (Fig. 4A,B). Eleven patients had elevated MSI/MSI-H/MSI-unstable tumors. All eleven patients with elevated MSI/MSI-H/MSI-unstable tumors also had elevated TMB levels, reinforcing the findings that these patients would greatly benefit from ICI therapy. This group consisted of 4 patients with FGT (3 Ca endometrium + 1 Ca ovary), 4 patients with GIT (2 sigmoid colon + 2 esophagus), 1 patient with prostate cancer (GU), one patient with HPB and 1 pediatric patient with astrocytoma (CNS). The genomic data of 7 patients who underwent IO based on the report is shown (Table 2).
CGP has identified many biomarkers that could be potential tumour-agnostic markers in the future. Fibroblast growth factor receptors (FGFRs) were found to be aberrantly activated through copy number amplification in 69 patients (7%), of which FGFR1, FGFR19, and FGFR4 amplifications constituted 56%, 41%, and 33%, respectively. FGFR2 amplification was found in 11% of patients. FGFR1 translocation was found in one lung adenocarcinoma patient, one BC patient and one GIT patient, whereas 2 FGFR2 fusions were found in HPB cancers, one of which was cholangiocarcinoma. Among all the cancer types, FGFR alteration was found to be more prevalent in breast cancer (16%), followed by HNSCC (7%), GIT, lung and CUP (3–7%). The prevalence of FGFR alterations across different tumors is shown in Table 3.
Another interesting target identified in the cohort regardless of the type of tumor was the alteration in the AT-rich interaction domain (ARID) gene. The human SWI-SNF complex protein ARID1A was found to be altered in approximately 4.5% of cancers in the clinical cohort, comprising ovarian clear cell cancers (11%), uterine and endometrial cancers (28%) and other FGTs (6%). ARID1A gene alterations were also detected in breast (2%) HNSCC (4%), GIT (5%), and HPB (14%) samples, resulting in loss of function. The prevalence of ARIDA alterations along with the corresponding MSI and TMB across different tumors is shown in Table 4.
Fusions
RNA sequencing revealed 67 genomic alterations with 50 fusions and 17 splice variants (Fig. 5). Androgen receptor splice variants were detected in 15 patients with prostate carcinoma, and two MET splice variants were detected in patients with unknown primary and adenocarcinoma of the lung. Forty-nine fusions were reported with TMPRSS-ERG fusion (n = 7), EML4-ALK (n = 6), and RPS6KB1-VMP1 (n = 4), the most frequently isolated genomics alterations. Two patients had known NTRK fusions, which are predictive tumor markers. Three FGFR2 fusions, one RET fusion and two PDGFRA and EWSR1 fusions were also detected.
CGP versus small-targeted panel
CGP revealed a greater number of druggable genetic alterations than small panels. In a pilot study, one hundred and twenty-five patients were tested for both targeted tissue-specific small panel and CGP. The proportion of patients with ≥ 1 actionable biomarker was significantly greater with CGP than with small panels (47% vs. 14%; p value < 0.05). The findings were discussed in the molecular tumor board (MTB), and recommendations from treating physicians were documented in patient records for changes in clinical management and follow-up. The average proportion of tested patients who received FDA-approved targeted therapy on the basis of the genomics report was greater in the CGP cohort than in the small panel cohort (30% vs. 2%; p value < 0.05) (Fig. 6).
CGP and clinical management
Among the 1000 patients, clinical and follow-up data were available for 618 patients (62%), which included patients with different cancer spectra, such as breast (n =105), lung (n =77), GI (n = 99), FGT (n = 62), HN (80), HPB (N = 59), GU (n = 43), and CUP (n = 18) cancer. Other cancers (n = 77) included sarcoma, melanoma, neuroendocrine tumors, etc. The cancer spectrum with clinical outcome data is shown in Fig. 7A,B. Actionable genetic alterations (Tier I + Tier II) were found in 458 patients (74%; 95% CI 70.6%-77.4%). Four hundred nineteen patients had druggable mutations (67%; 95% CI 88.9–93. 9%), and 39 patients had 1 or more mutations with prognostic implications.
In the present study, the highest proportion of actionable and druggable genetic alterations were found in patients with lung cancer (91%; 84%). The lung is the posterchild for precision oncology, with a myriad of approved targeted therapies for various genomic alterations, including tumor-specific and tumor-agnostic markers. The most frequently detected Tier I alterations were EGFR mutations observed in 72 patients followed by a TMB > 10, observed in 28 patients, and a KRAS mutation detected in 18 patients. Among the other patients with Tier I mutations, 6 had ALK-EML4 translocations, one with NTRK1 fusion and two with BRAF V600E. EGFR was found to be comutated with P53, MET amplification/mutation, RET amplification, KRAS, PIK3CA, and ERBB2 in 12 patients. Since these mutations are important de novo or acquired resistance mutations, the response to EGFR TKIs was determined from medical records. Three patients with EGFR and P53 comutations had a poor response to the first and second lines of EGFR tyrosine kinase inhibitors (TKIs). These findings corroborate earlier findings from other authors that P53 mutations can be associated with primary or acquired resistance to EGFR-TKIs16, highlighting the need to test the status or mutation of P53 in lung cancer in a larger cohort. This will not only improve the therapeutic effects of EGFR-TKIs in NSCLC but also prevent overtreatment with TKIs. Co-mutations of EGFR and KRAS were found in three patients. Based on the genomic data, all three patients were treated with combination therapy instead of TKIs alone and were followed up. An analysis of the data revealed that KRAS mutations were primarily detected in exon 2 (codon 12/13) of the KRAS gene. In addition, 3 cases of KRAS mutations were associated with elevated TMB, whereas all cases with actionable EGFR Tier I mutations were not associated with elevated TMB or the presence of ALK/ROS1 fusion. This is in contrast with a single-gene KRAS mutational study performed in-house, in which non exon 2 mutations in NSCLC were observed at higher frequencies than exon 2 mutations17. This discrepancy warrants further evaluation and may stem from the limited sample size of the current cohort. KRAS mutations were not the most common genomic alterations in the current cohort, as in the Caucasian population, where KRAS mutations are detected at higher frequencies18. Compared with WT KRAS, KRAS mutations were associated with higher TMB values, but the association was not statistically significant. A study on a larger clinical cohort would be necessary to clarify the true nature of KRAS mutations and their relationship with immunotherapy in Indian subpopulations19.
The second most common cancers with the greatest number of actionable and druggable genomic alterations were those with GI and HPB cancers (80% and 80%, respectively). However, the change in treatment based on genomics reports and MTB discussions was greater in patients with GI cancers (39%) than in patients with HPB (19%). In upper GI cases (esophagus and stomach), TMB was the most frequent actionable mutation, followed by HER2 amplification and cyclin-dependent kinases, whereas in lower GI cases, KRAS mutations were the most frequent actionable mutations, followed by PIK3CA and elevated TMB. In the GI cohort, 30 patients (20%) had high TMBs ranging from 10.2 to 656 mut/Mb. The incidence of elevated TMB was identical in upper and lower GI cases. Compound mutations of APC were observed in 45% of the patients. No actionable fusions or splice variants were observed in the GI cohort.
The most common druggable mutations in HPBs include KRAS mutations (n = 31), high TMB (n = 18), and mutations in the BRCA and HRR genes.
The CGP identified actionable (TierI + TierII) and druggable genomic alterations in 80% and 73% of patients, respectively, in the BC cohort. A previous study from the same author using a small hotspot panel reported actionable mutations in 46% of BC patients only20. Genetic aberrations were identified in the PI3KCA/AKT/PTEN signalling pathway in a substantial fraction (37%) of Indian BC patients. PI3KCA was found to be altered in 33% of patients, whereas mutations in AKT and deletions in PTEN were found in 2–3% of BC patients. The sBRCA and HRR pathways were altered in 22 patients (18%), among whom sBRCA1 and sBRCA2 were found in 9 (7%) and 7 (6%) patients, respectively. HRR genes such as PALB2, RAD51, ATM, and CHEK2 were found in 5 patients (4%). Twenty-seven patients (18%) had high TMB, and 9 patients had borderline high TMB.
Despite significant improvements in the outcomes of BC patients, many patients present intrinsic drug resistance, while others are initially drug sensitive but acquire resistance to anticancer drugs and frequently multidrug resistance, leading to recurrence and/or metastasis21,22,23,24. There is growing evidence that patients with the same BC molecular subtype can have different responses to treatment, strongly supporting high BC heterogeneity. Eight hormonal-positive BC patients (8%) in the cohort were found to have alterations in the ligand-binding domain (LBD) of estrogen receptor 1 (ESR1), encoding estrogen receptor α (ER), of which 9 were SNVs. A fusion of ESRI (ESR1: MTHFD1L) was also found in one BC patient and labeled VUS. The clinical outcomes of the 8 patients with ESR1 mutations who were treated with hormonal therapy are shown in Table 5. The clinical outcome data of 2 patients were not available in the electronic medical records. The FDA has recently approved blood-based companion diagnostics for ESR1 testing and a new drug called elacestrant (Orserdu™) for patients with HR + positive, HER2- MBC with an ESR1 gene mutation who have received at least one type of hormone therapy. This leads to reclassifying the ESR variant from Tier II to Tier I, establishing the importance of CGP.
The mutational spectrum of sBRCA and HRR pathway alterations and TMB of TNBC patients revealed a distinctive mutational profile. A total of 140 actionable genomic alterations were detected in 63 patients (2.3 genomic alterations/case). The most frequent genomic alterations detected were TP53 mutations (81% of cases in the cohort), followed by TMB > 10 (28%), homologous recombination (HRR) gene mutations (26%), and PIK3CA pathway alterations (20%). sBRCA1 and sBRCA 2 were found in 13% and 11% of the patients, respectively. An MSI > 20% was not detected in TNBC.
Among 458 patients with ≥ 1 actionable genomic alterations, only 200 patients (44%; 95% CI 39.1%-48.1%) were enrolled for MTB discussion. The treatment planning data before and after genetic testing were obtained from EMR. With the multitude of clinical inputs from the multidisciplinary MTB, various modifications were made in the treatment paradigm in 137 patients (69%; 95% CI 62.4–74.6%). Sixty-three patients (31%; 95% CI 25.4–37.6%) underwent no change in therapy post-MTB despite possessing actionable genomic alterations. Notably, out of 258 patients (56%) who were not enrolled in the MTB, only 61 (24%) patients received therapy on the basis of genomics reports as per the recommendation of the referring doctor. Thus, the overall change in therapy based on CGP in the clinical cohort was 43% (n = 198), which was greater in patients enrolled for MTB (n = 137, 69%) than in patients who had not undergone MTB (n = 61. 24%), thus establishing the importance of MTB in personalized genomics-driven treatment. The clinical management of patients across different cancer types based on the CGP report is shown in Fig. 7C. A summary flow chart of patients after receipt of the CGP report is shown in Fig. 8. Among the 137 patients enrolled in MTB, and received genomics-matched treatment, the most recommended therapy was immune checkpoint inhibitors (ICIs) (n = 44) with MSI-H and/or TMB > 10 mu/Mb. Platinum agents and PARP inhibitors were used in 22 patients for mutations in one of 19 HRR genes, including sBRCA. The other recommended therapies by the MTB were anti-EGFR tyrosine kinase inhibitors (TKIs) (n = 21), other TKIs (n = 15), anti-Her2 therapy for Her2 amplification (n = 17), mTOR inhibitors for PIK3CA/AKT/mTOR alterations (n = 5), and ALK inhibitors for ALK translocation (n = 4). Based on a genomics report showing the KRASG12C mutation, 3 lung adenocarcinoma patients were treated with sotorasib. The number of patients assigned to tumor-agnostic therapy post-MTB (n = 137) is shown in Fig. 9.
At the interim analysis, with a median follow-up of 18 months (range 12–24 months) after a change in therapy, 97/137 patients (70%) were found to be alive. The number of patients per tumor type assigned to each tumor-agnostic therapy post- MTB is shown in Fig. 10. The clinical outcome of the patients is shown in Table 6.
Discussion
The CGP approach using NGS is emerging as an important diagnostic tool to find novel and well-known targets for genomic-based therapies, particularly in patients with a limited response to the standard of care (SOC)25. However, comprehensive genomic reports need to be interpreted, translated into potential clinical recommendations based on the evaluation of the clinical indication, actionability of the detected molecular target, tumor type, and patient characteristics.
In this retrospective analysis of approximately 1000 cases, we highlight the importance of CGP in understanding the clinical utility of genetic testing. To our knowledge, this is the first comprehensive analysis from India to understand the clinical utility of the CGP in patients. More than 80% of patients had actionable genomic alterations, of which about 67% were druggable and potentially had the ability to access/receive molecularly targeted therapy on the basis of CGP before starting SOC or after failure of SOC. The overall change in therapy based on CGP in the clinical cohort was 43%, which was greater in patients enrolled for MTB (69%) than in patients who had not undergone MTB (24%), thus establishing the importance of MTB in personalized genomics-driven treatment. The proportion of actionable, druggable mutations and MTB-driven therapy changes has also been reported in a recent study by Matsubara et al. in a cohort of 183 Japanese patients. The study revealed 100% and 63% actionable and druggable genomic alterations, respectively, of which 61% of patients had undergone MTB-based therapy recommendation26. The importance of CGP and MTB in therapy recommendations has been established in many other previous studies26,27,28,29. Tamborero et al. also established the role of the MTB portal in supporting clinical decisions and automated reporting for precision oncology26. Carolina SR et al. established an MTB strategy with demographic, clinical and genomic information from 146 Hispanic patients with one or more genomic alterations and characterized them as benefitting from the recommended treatment option. The current study revealed that the genomics results discussed by the MTB prompted a change in therapeutic decisions in 60% of patients, with the most prevalent malignancy being non-small cell lung cancer30. This study corroborates our finding that the highest proportion of actionable and druggable genetic alterations were found in patients with lung cancer (91%; 84%).
In the present study, genomics-matched therapy based on reports targeting genes included in the CGP list in a tumor-agnostic setting was recommended for 137 patients. The most recommended therapy was immune checkpoint inhibitors (ICIs) for patients (n = 44) with either MSI-H or TMB > 10 and patients with both MSI-H and TMB > 10 followed by platinum agents and PARP inhibitors (n = 22) for patients with deleterious alterations in one of 19 genes, including sBRCA involved in homologous recombination repair. The other recommended therapies by the MTB were anti-EGFR tyrosine kinase inhibitors (TKIs) (n = 21), other TKIs (n = 15), anti-Her2 therapy for Her2 amplification (n = 17), mTOR inhibitors for PIK3CA/AKT/mTOR alterations (n = 5), ALK inhibitors for ALK translocation (n = 4) and sotorasib (n = 1) for the KRASG12C mutation. Previous studies have shown that molecular targeted therapy accompanied by companion diagnostics that included tropomyosin receptor kinase for TRK fusion-positive tumors31,32 and pembrolizumab for MSI-high and/or TMB-high patients33,34,35 is highly effective in a tumor-agnostic setting.
Although multidisciplinary molecular tumor boards are becoming integral part of oncology practice globally, this strategy needs to be explored more, made accessible to all hospitals and executed as a mandatory guideline for cancer treatment and management in all hospitals. Continuous efforts to standardize and update the MTB discussion is warranted, as reported in a previous study36.
In summary, within this Indian cohort, we have shown the valuable utility of using CGP in early stages to advise on treatment options to provide better survival outcomes. The outcomes of the current study have not only reinforced the utility of CGP in the clinic but also helped to add more data of clinical relevance by identifying genetic alterations/genomic signatures as valuable tools for correct diagnosis, prognosis and clinical intervention. CGP, in addition to the detection of predictive genes, allows the identification of genes associated with therapy resistance, prognosis and early recurrence and additionally provides information on key cancer-agnostic biomarkers. As stated by the author in a previous study on the genomic landscape of breast cancer using small panels20, the current study further emphasized the importance and advantage of CGP over a limited gene panel. About 35% of patients have been enrolled in genome-specific, investigator-initiated clinical trials. This study will enable the clinicians to develop a large-scale Indian population-specific cancer database to achieve better therapeutic and clinical outcomes. The findings from the current study establishes a foundation for introducing precision oncology in clinical practice to reduce treatment costs and improve clinical outcomes. This has a considerable effect on healthcare costs in emerging economic countries such as India, where the availability of and access to cancer drugs, rational combination therapies, and enriched clinical trials have been additional challenges in the adoption of genomic medicine.
However, this study has several limitations. A major limitation is referral for CGP for all patients registered in the hospital, and only 50% of all patients counselled opted for CGP within the study period. The reasons for fewer referrals and low adoption of these tests in clinical practice could be manifold. Comparatively higher cost of genetic tests than other conventional diagnostic tests (IHC, FISH), and the limited awareness and accessibility of these tests are major hindrances. A collaborative approach of researchers and laboratories with clinicians to initiate large-scale prospective studies to confirm the independent prognostic and therapeutic value of the CGP in a larger cohort of the Indian population might help to overcome the hindrances.
Data availability
We are not permitted to share the sequence data publicly since they belong to cancer patients coming to the hospital for treatment and we need to protect study participant’s privacy. As suggested by editorial office, we agree to share the sequence data upon other researcher’s request if they have obtained the required ethics approval and patients’ consent. Please contact mithuaghosh@hcgel.com if any data is required from the study.
References
Gilson, P., Merlin, J.-L. & Harlé, A. Deciphering tumor heterogeneity: From tissue to liquid biopsy. Cancers 14, 1384. https://doi.org/10.3390/cancers14061384 (2022).
Dagogo-Jack, I. & Shaw, A. T. Tumor heterogeneity and resistance to cancer therapies. Nat. Rev. Clin. Oncol. 15, 81–94. https://doi.org/10.1038/nrclinonc.2017.166 (2018).
Schilsky, R. L. & Longo, D. L. Closing the gap in cancer genomic testing. N. Engl. J. Med. 387, 2107–2110. https://doi.org/10.1056/NEJMp2210638 (2022).
Shastry, M., Gupta, A., Chandarlapaty, S., Young, M., Powles, T. & Hamilton, E. Rise of antibody-drug conjugates: The present and future. In: Developmental therapeutics—molecularly targeted agents and tumor biology. (ASCO Educational Book, 2023).
Rassy, E., Rached, L. & Pistilli, B. Antibody drug conjugates targeting HER2: Clinical development in metastatic breast cancer. The Breast 66, 217–226 (2022).
Samstein, R. M. et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat. Genet. 51, 202–206. https://doi.org/10.1038/s41588-018-0312-8 (2019).
Salmaninejad, A. et al. PD-1/PD-L1 pathway: Basic biology and role in cancer immunotherapy. J. Cell. Physiol. 234, 16824–16837. https://doi.org/10.1002/jcp.28358 (2019).
Spencer, K. R. et al. Biomarkers for immunotherapy: Current developments and challenges. Am. Soc. Clin. Oncol. Educ. Book 35, e493-503. https://doi.org/10.1200/EDBK_160766 (2016).
Fusco, N. et al. PTEN alterations and their role in cancer management: Are we making headway on precision medicine?. Genes 11, 719. https://doi.org/10.3390/genes11070719 (2020).
El-Deiry, W. S. et al. The current state of molecular testing in the treatment of patients with solid tumors. CA A Cancer J. Clin. 69(4), 305–343. https://doi.org/10.3322/caac.21560 (2019).
Malone, E. R., Oliva, M., Sabatini, P. J. B., Stockley, T. L. & Siu, L. L. Molecular profiling for precision cancer therapies. Genome Med. 12, 8. https://doi.org/10.1186/s13073-019-0703-1 (2020).
Bosi, C. et al. Pan-cancer analysis of antibody-drug conjugate targets and putative predictors of treatment response. Eur. J. Cancer 195, 113379. https://doi.org/10.1016/j.ejca.2023.113379 (2023).
Haynes, B. C. et al. An integrated next-generation sequencing system for analyzing DNA mutations gene fusions, and RNA expression in lung cancer. Translational Oncol. 12(6), 836–845. https://doi.org/10.1016/j.tranon.2019.02.012 (2019).
Wolff, A. C. et al. Human epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/college of American pathologists clinical practice guideline focused update. Arch. Pathol. Lab. Med. 142, 1364–1382. https://doi.org/10.5858/arpa.2018-0902-SA (2018).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424. https://doi.org/10.1038/gim.2015.30 (2015).
Liu, S., Yu, J., Zhang, H. & Liu, J. TP53 co-mutations in advanced EGFR-mutated non-small cell lung cancer: Prognosis and therapeutic strategy for cancer therapy. Front. Oncol. 12, 860563. https://doi.org/10.3389/fonc.2022.860563 (2022).
Balaram, G. et al. Kirsten rat sarcoma mutation in South Indians with non-small lung cancer: A cause for concern?. J. Precis. Oncol. 2(1), 3–8. https://doi.org/10.4103/jpo.jpo_7_22 (2022).
Hsu, J. et al. Molecular signatures of KRAS-mutated lung adenocarcinoma: Analysis of concomitant EGFR, ALK, STK11, and PD-L1 status. Clin. Pathol. 15, 1–8. https://doi.org/10.1177/2632010X221102054 (2022).
Sciortino, C. et al. Response to immunotherapy in KRAS G12C mutated NSCLC: A single-center retrospective observational study. Oncotarget 13, 686–693. https://doi.org/10.18632/oncotarget.28230 (2022).
Ghosh, M. et al. Landscape of clinically actionable mutations in breast cancer ‘A cohort study’. Translational Oncol. 14, 100877. https://doi.org/10.1016/j.tranon.2020.100877 (2021).
Masoud, V. & Pagès, G. Targeted therapies in breast cancer: New challenges to fight against resistance. WJCO 8, 120. https://doi.org/10.5306/WJCO.V8.I2.120 (2017).
Abad, E., Graifer, D. & Lyakhovich, A. DNA damage response and resistance of cancer stem cells. Cancer Lett. 474, 106–117. https://doi.org/10.1016/j.canlet.2020.01.008 (2020).
Marquette, C. & Nabell, L. Chemotherapy-resistant metastatic breast cancer. Curr. Treat Options Oncol. 13, 263–275. https://doi.org/10.1007/s11864-012-0184-6 (2012).
Brown, K. A., Andreopoulou, E. & Andreopoulou, P. Endocrine therapy-related endocrinopathies—Biology, prevalence, and implications for the management of breast cancer. Oncol. Hematol. Rev. (US) 16, 17. https://doi.org/10.17925/OHR.2020.16.1.17 (2020).
Larson, K. L. et al. Clinical outcomes of molecular tumor boards: A systematic review. JCO Precis. Oncol. 5, 1122–1132. https://doi.org/10.1200/PO.20.00495 (2021).
Matsubara, J. et al. First-line genomic profiling in previously untreated advanced solid tumors for identification of targeted therapy opportunities. JAMA Netw. Open 6(7), e2323336. https://doi.org/10.1001/jamanetworkopen.2023.23336 (2023).
Sunami, K. et al. Feasibility and utility of a panel testing for 114 cancer-associated genes in a clinical setting: A hospital-based study. Cancer Sci. 110(4), 1480–1490. https://doi.org/10.1111/cas.13969 (2019).
Kondo, T. et al. Comprehensive genomic profiling for patients with chemotherapy-naïve advanced cancer. Cancer Sci. 112(1), 296–304. https://doi.org/10.1111/cas.14674 (2021).
Aoyagi, Y. et al. Clinical utility of comprehensive genomic profiling in Japan: Result of PROFILE-F study. PLoS One 17(3), e0266112. https://doi.org/10.1371/journal.pone.0266112 (2022).
Tamborero, D. et al. The molecular tumor board portal supports clinical decisions and automated reporting for precision oncology. Nat. Cancer 3, 251–261. https://doi.org/10.1038/s43018-022-00332-x (2022).
Rodriguez, C. S. et al. Molecular tumor board improves outcomes for hispanic patients with advanced solid tumors. JCO Global Oncol. 10, e2300011. https://doi.org/10.1200/GO.23.00011 (2024).
Drilon, A. et al. Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. N. Engl. J. Med. 378(8), 731–739. https://doi.org/10.1056/NEJMoa171444836 (2018).
Doebele, R. C. et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumors: integrated analysis of three phase 1–2 trials. Lancet Oncol. 21(2), 271–282. https://doi.org/10.1016/S1470-2045(19)30691-6 (2020).
Marabelle, A. et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient cancer: Results from the phase II KEYNOTE-158 study. J. Clin. Oncol. 38(1), 1–10. https://doi.org/10.1200/JCO.19.02105 (2020).
Marabelle, A. et al. Association of tumor mutational burden with outcomes in patients with advanced solid tumors treated with pembrolizumab: Prospective biomarker analysis of the multicohort, openlabel, phase 2 KEYNOTE-158 study. Lancet Oncol. 21(10), 1353–1365. https://doi.org/10.1016/S1470-2045(20)30445-9 (2020).
Tamborero, D. et al. Support systems to guide clinical decision-making in precision oncology: The cancer core Europe molecular tumor board portal. Nat. Med. 26(7), 992–994. https://doi.org/10.1038/s41591-020-0969-2 (2020).
Acknowledgements
We express our sincere gratitude to the oncologists Dr. Ramesh Billimaga, Dr. Naresh Somani, Dr. Kaustuv Patel, Dr Jagdish Kothari, Dr. Jagannath Dixit, Dr.Prabhu N, Dr Abhilasha, Dr.Raghunath, Dr. Ravi Diwakar; Dr Sashidhar, Dr. Indoo Ambolkar, Dr. Jitendra P, Dr. Satish S, Dr Sachin Trivedi for providing clinical recommendations. Strand Life Sciences- Dr.Shanmukh Katragadda, and Swetha N.S.N for data analysis. Godina P, Department of Biostatistics, HCG for statistical analysis
Funding
No funding was received from any external source. Institutional Support.
Author information
Authors and Affiliations
Contributions
Mithua Ghosh (Corresponding Author): Conceptualization, Methodology, Writing—Original Draft, Review & Editing Visualization, Investigation, Project administration, Supervision. Sheela Mysore Lingaraju: Conceptualization, Methodology, Project administration, review and editing, Data curation Krishna CR: Methodology, Validation, Gautam Balaram: Methodology, review and editing, Data curation; Ramya Kodandapani: Methodology, Validation; Vijay E: Methodology, Vijay K: Methodology, Suhas N—Methodology, Devika H: Methodology (Genetic Counselling), Shekar Patil: Investigation, Satheesh Chiradoni Thungappa: Investigation; Somorat Bhattacharjee: Investigation; Sridhar PS: Investigation ;Roshni Dasgupta: Investigation; Mohammed Naseer Investigation; Srinivas BJ: Investigation; Vishal Rao: Investigation; Veena Ramaswamy: Methodology; Radheshyam Naik: Investigation Govind Babu K: Investigation; Aarthi Ravichandran: Software, Formal Validation, Investigation; Urvashi Bahadur: Software, Formal Validation, Investigation Krithika Murugan: Investigation, Mahesh B: Investigation; Lohith Reddy: Investigation; Basavalinga S. Ajaikumar: Conceptualization, Investigation, Resources.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
EC Name: HCG Central Ethics Committee. EC Registration No: ECR/386/Inst/KA/2013/RR-19. This article does not contain any studies with human participants or animals performed by any of the authors. All methods were performed in accordance with the relevant guidelines and regulations with the retrospective FFPE blocks available in the Pathology lab.
Informed consent
Informed consent was obtained from all individual participants included in the study. All the subjects of the cohort have been anonymized.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ghosh, M., Lingaraju, S.M., C.R, K. et al. Comprehensive genomic profiling reveals a unique genomic landscape in solid tumors in an Indian cancer cohort of 1000 patients: a single institutional experience. Sci Rep 15, 12455 (2025). https://doi.org/10.1038/s41598-025-94762-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94762-z