Abstract
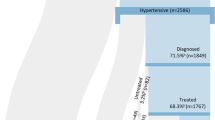
The high prevalence of hypertension in coastal regions poses a significant public health challenge due to factors such as high salt intake, air pollution, poor diets, limited healthcare access, and increased stress levels. However, disparities in diagnosed hypertension between coastal and non-coastal areas in Bangladesh remain underexplored. This study aims to investigate and address the prevalence of diagnosed hypertension among adults in both regions. In 2020–2021, a cross-sectional study was conducted in Bangladesh to assess hypertension prevalence in coastal and non-coastal regions. The study included 3917 adults from six districts, including non-coastal and coastal regions. Prevalence ratios (PRs) were determined using a modified Poisson regression model, to quantify the relationship between hypertension prevalence in the two regions. The study finds that 438 (11.2%) of the 3917 respondents [446 females [11.7%]; mean age 44.73 years] had been diagnosed with hypertension. Notably, adults residing in coastal areas had a higher prevalence of hypertension (13.4%, 95% confidence interval: 11.8%-15.0%) than their non-coastal counterparts (9.5%, 95% CI: 8.3%-10.7%). In coastal areas, the prevalence ranged from 7.8% in the 18–24 age group to 16.4% in the 55 + age group. In non-coastal areas, the prevalence ranged from 2.9% in the 18–24 age group to 15.8% in the 55 + age group. The results of the multivariable analysis revealed that adults from coastal areas were 29% more likely to have hypertension than those in non-coastal areas (aPR:1.29, 95% CI: 1.07–1.56). Moreover, age, physical activity, occupation, and body mass index (BMI) were identified as factors associated with the development of hypertension within these regions. Hypertension is a major health issue across Bangladesh, with coastal regions facing added challenges from high salinity in drinking water. While both coastal and non-coastal areas experience high rates of undiagnosed hypertension, environmental factors unique to coastal areas may intensify the issue. Targeted interventions that account for environmental and socioeconomic factors are essential to addressing this growing health concern in both regions.
Similar content being viewed by others
Introduction
Hypertension, a significant global health concern, exerts a widespread impact, particularly in coastal regions worldwide. This phenomenon is driven by a combination of factors, including increased salt intake, air pollution, unhealthy diets, restricted healthcare access, and elevated stress levels among coastal residents1,2. Associated with an estimated annual toll of 9.4 million premature deaths globally, hypertension serves as a major precursor to severe health risks such as stroke, cardiovascular diseases, and kidney failure1,2,3. Globally, hypertension is more prevalent and frequently treated among individuals with multimorbidity4. Additionally, long-term hypertension significantly diminishes the quality of life5.
While high-income countries witness a slight decline in hypertension prevalence, its relentless surge across low- and middle-income nations, especially in regions like South Asia and sub-Saharan Africa, casts a shadow on overachieving global health and sustainable development goals (SDG)−36,7,8. The geographical landscape plays a pivotal role, with disparities in prevalence linked to income levels and diverse risk factors—such as elevated salt content in local diets or water sources—significantly impacting susceptibility to hypertension9. The World Health Organization (WHO) stresses the importance of lowering the salt content in food to a recommended level below 5‒6 g per day10. Nevertheless, the salinity in water sources used for drinking and cooking has risen in numerous coastal regions worldwide, partly because of global climate change8. This heightened salinity in water for drinking and cooking purposes can amplify the likelihood of hypertension and related illnesses.
Bangladesh, a nation perched at the forefront of vulnerability to climate change, grapples with escalating saline water intrusion due to rising sea levels and intensified storms in the Bay of Bengal11,12,13. Coastal divisions like Khulna, Barishal, and Chattogram bear the brunt, hosting districts (such as Satkhira, Bagerhat, Khulna, and Barguna) highly prone to heightened water salinity, exposing inhabitants to increased hypertension risks14,15,16,17. Due to the infiltration of salty water triggered by environmental shifts, more than twenty million people in the Bangladesh region face a significant risk of developing high blood pressure18. Beyond climate change, local activities like intensive shrimp farming contribute to rising water salinity, further amplifying health hazards19. As a result, residents in these areas could be more vulnerable to the negative effects of heightened salinity in their drinking and cooking water.
In Bangladesh, evidence indicates a substantial variation in hypertension prevalence across regions20. A nationwide survey in Bangladesh (2017–2018) found that approximately 28% of the population had hypertension, including 16% undiagnosed cases and 12% diagnosed cases21. A study conducted in a rural district of Bangladesh found a prevalence of 6.9%, with a higher prevalence among women (8.9%) compared to men (4.5%)22. National surveys highlight this diversity, with rates fluctuating between urban and rural landscapes and regions like Khulna, Barisal, and Sylhet23,24,25. Studies reveal a higher prevalence in urban settings compared to rural areas, emphasizing the multifaceted influences shaping hypertension, including age, gender, education, employment status, body mass index, diabetes, socioeconomic status, and, notably, drinking water salinity24,26,27,28.
However, despite existing data, a critical gap persists in understanding the diagnosed hypertension disparities between coastal and non-coastal regions within rural Bangladesh. This research endeavors to bridge this gap, aiming to meticulously scrutinize and address the prevalence of diagnosed hypertension among adults dwelling in both coastal and non-coastal domains of rural Bangladesh. Such insights could pave the way for targeted interventions, enhance healthcare strategies, and fortify resilience against the burgeoning threat of hypertension in these regions.
Methods and materials
Study design and study area
Data collection for this cross-sectional study was conducted by the Center for Natural Resource Studies (CNRS) during 2020–2021. For the purposes of this study, the survey selected a total of 3917 households from six districts of Bangladesh, including coastal (Satkhira and Khulna) and non-coastal (Sherpur, Jamalpur, Sunamganj, and Pabna). The study protocol received approval from the Bangladesh Medical Research Council, and the authorized protocol is available in the public domain: https://osf.io/ka6sj/.
Calculation of sample size
The participants from rural areas were drawn from the 14 sub-districts of the selected districts. Within sub-districts, unions are the smallest geographic tier with precise and defined areas in rural areas. A total of at least 384 households were drawn from each sub-district and it was decided that the primary sampling units (PSUs) or clusters for the rural stratum were unions (each union consists of several villages- thus forming village-based communities). The sampling frame of the clusters is given in Supplementary Fig. S1. The sample size of total 7000 are collected for the study and the details are given in the Supplement. The sampling frame comprised a list of rural villages as developed by the Bangladesh Bureau of Statistics, based on the 2011 census of population and housing enumeration areas. The sample size calculation for project intervention areas is given in Supplementary Table S1. Figure 1 illustrates the study area in rural Bangladesh, along with a flow diagram outlining the participant selection process.
Outcome
We considered self-reported known hypertension among individuals in the study. A diagnosis of hypertension was made by a healthcare professional when systolic blood pressure measurements, taken on two separate occasions, are ≥ 140 mmHg and/or diastolic blood pressure measurements are ≥ 90 mmHg on both occasions. Here in this study, hypertension was considered to be present in individuals if they met one of the following criteria:
(1) Individuals who had a documented history of taking antihypertensive medication to control high blood pressure, or (2) Individuals who had received medical advice or recommendations for controlling high blood pressure, even if they were not currently taking antihypertensive medication.
This definition suggests that individuals who either had a history of taking medication for hypertension or had received medical advice for controlling high blood pressure were classified as having hypertension for the purposes of the study. This criterion allows for a broader inclusion of individuals who may be managing their hypertension through different means, including lifestyle modifications in addition to medication.
Exposure
Coastal residency in Bangladesh encompasses 19 districts that are directly or indirectly impacted by the Bay of Bengal. These regions are particularly vulnerable to natural hazards such as tidal surges, cyclones, saline water intrusion, and flooding. Key coastal districts include Chittagong, Cox’s Bazar, Khulna, Barisal, and Bhola. Characterized by their proximity to the sea and unique ecosystems like the Sundarbans, coastal areas are simultaneously blessed with abundant natural resources and challenged by climate-related risks.
Non-coastal Bangladesh, situated further inland, is less susceptible to the immediate threats posed by the Bay of Bengal, such as saline intrusion and tidal surges. Nevertheless, these regions may still experience flooding from riverine systems, especially during the monsoon season. Major non-coastal districts include Dhaka, Rajshahi, Sylhet, and Mymensingh.
Covariates
The analysis includes several explanatory variables such as the respondent’s age (years), gender (male/female), schooling years (no/1–5 years/6–10 years/11–12 years/ ≥ 12 years), marital status (Married/ Divorced/ Widowed/ Unmarried), and occupation (Service/ Day labor/ Housewife/ Small Business/ Student/ Unemployed/ Retired). Body Mass Index (BMI), calculated from height and weight records, was categorized as normal (18.5–24.9 kg/m2), underweight (< 18.5 kg/m2), overweight (25–29.9 kg/m2), and obese (> = 30 kg/m2) (23). The World Health Organization’s Global Physical Activity Questionnaire (GPAQ) was used to assess physical activity levels29, measuring in three domains: work, transport, and leisure-time activities. It classifies physical activity by intensity using Metabolic Equivalent of Task (MET) values. Light (1–2.9 METs): Slightly increased breathing or heart rate (e.g., slow walking, light chores), Moderate (3–5.9 METs): Moderate increase in breathing or heart rate (e.g., brisk walking, leisurely cycling) and Vigorous (≥ 6 METs): Significant increase in breathing or heart rate (e.g., running, swimming). The location of residence is divided into coastal (Satkhira and Khulna) and non-coastal (Sherpur, Jamalpur, Sunamganj, and Pabna) regions. These variables are used to assess and explain various aspects of the study in relation to diagnosed hypertension.
Statistical analysis
The statistical analyses were conducted using R version 4.3.0. First, we conducted a bivariate analysis to assess the relationships between the outcome and the predictors by calculating the unadjusted prevalence ratio (PR) for each categorical predictor. The unadjusted PR is computed to assess the difference in hypertension prevalence between demographic groups. We used the robust standard errors to address potential overdispersion in the modified Poisson model and the sandwich package in R to compute robust standard errors. To preserve the statistical validity of our findings in adjusted analysis, cases with missing data were systematically excluded from the analytical process. The results of the multivariable regression analysis were presented as adjusted prevalence ratio (APR), and 95% confidence intervals (CI). To enhance our primary analysis, we conducted a sensitivity analysis using a machine learning approach, specifically the Random Forest (RF) method. RF offers key advantages, including the ability to model complex, nonlinear relationships and to identify important predictors even when variables are highly correlated. We implemented the RF model using the randomForest() function from the randomForest package in R. To assess the model’s accuracy, we used a 70/30 data split: 70% of the data for training and 30% for testing. This method enabled us to validate the model’s performance on unseen data, providing a more rigorous evaluation of its predictive capabilities.
Results
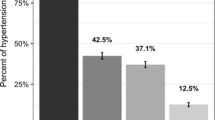
The unadjusted analysis in Table 1 reveals the relationship between socio-demographic characteristics and diagnosed hypertension in the study participants. Among the 3,917 adult participants, 438 (11.2%, 95% confidence interval, CI = 10.2%−12.1%) had been diagnosed with hypertension. The study had 2227 (56.8%) respondents from non-coastal regions, and the remaining 1690 (43.2%) were from coastal regions. Coastal adults had a higher prevalence of hypertension (13.4%, 95% CI = 11.8%−15.0%) compared to non-coastal adults (9.5%, 95% CI = 8.3%−10.7%). The unadjusted prevalence ratio indicated that coastal adults were 1.42 times more likely to have been diagnosed with hypertension than non-coastal adults (PR = 1.42, 95% CI = 1.19–1.69).
The study had 446 (11.4%) female respondents and 3471(88.6%) male respondents. Male respondents reported a 21% lower prevalence of diagnosed hypertension compared to female participants (PR = 0.79, 95% CI = 0.61–1.02), but this difference was not statistically significant in the unadjusted association analysis. Marital status did not show a significant association with hypertension prevalence.
The average age of the respondents was 44.73 years (standard deviation 13.53 years). The prevalence of diagnosed hypertension increased with age, ranging from 4.8% in the 18–24 age group to 16.1% in the 55 + age group. Approximately one-fifth of overweight or obese respondents (20.6%) were diagnosed with hypertension. Unemployed or retired participants had a higher prevalence of hypertension compared to those who were working.
The Table 2 compares various health-related characteristics between coastal residents and non-coastal residents. Coastal residents have a lower percentage of underweight individuals (17.4% vs 25.4%) and have a higher percentage of overweight (14.2% vs 8.5%) and obese (2.5% vs 1.5%) individuals. This suggests that coastal residents may have different lifestyle factors contributing to higher body mass. Coastal residents have a slightly higher rate of comorbid conditions with hypertension (11.1% vs 7.8%). Coastal residents have a lower smoking rate (34.3% vs 53.8%) but have a higher rate of chewing tobacco habit (33.8% vs 22.5%). This shift in substance use might reflect cultural preferences or availability of different tobacco forms in coastal areas. Coastal residents engage in more vigorous physical activity than non-coastal residents (19.1% vs 10.5%), possibly due to occupational demands (e.g., fishing, physical labor) or lifestyle choices influenced by their environment. Overall, the data suggests that coastal residents tend to have higher BMIs, slightly more hypertension-related comorbidities, and engage in more vigorous physical activity. They are less likely to smoke but more likely to chew tobacco compared to non-coastal residents.
The study’s findings, as shown in Fig. 2, indicate a consistent pattern of higher diagnosed hypertension prevalence among respondents in coastal areas compared to those in non-coastal areas across different age groups. For instance, within the age group of 45–54 years, the prevalence of diagnosed hypertension was notably higher in coastal regions, at 16.2%, compared to 10.1% in non-coastal regions. In general, younger adults from coastal areas exhibited a higher likelihood of hypertension compared to those in non-coastal regions. A significant difference in the prevalence of diagnosed hypertension was observed between coastal and non-coastal residents in the 35–54 age group. However, as the age category increases to 55 years and above, the difference in diagnosed HTN prevalence between coastal and non-coastal adults becomes less pronounced.
To account for potential factors influencing the associations between our exposures and diagnosed hypertension, we employed a modified Poisson regression model to estimate adjusted prevalence ratios (aPRs). We previously utilized a directed acyclic graph (DAG) – a visual representation of hypothesized causal relationships – to identify confounders in these relationships. In this DAG (see Supplementary Fig. S2, constructed with DAGitty: http://www.dagitty.net/dags.html#), diagnosed hypertension was considered the outcome, while coastal residency was the main exposure. For the association between exposures and diagnosed hypertension, a minimal sufficient adjustment set including age, sex, BMI, physical activity and coastal residency was determined. The mosaik plot, given in Supplementary Fig. S3, is also investigated to understand the relationship with coastal residency and confounders.
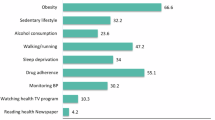
The adjusted analysis, using a Poisson regression model with robust standard errors, revealed several significant associations between hypertension and various variables. The adjusted prevalence ratios from the multivariable analysis are given in Fig. 3.
The PR for coastal residents (compared to non-coastal residents) is 1.29, indicating that coastal residents have a 29% higher prevalence of the outcome. This association was statistically significant, with a 95% confidence interval of 1.07–1.56. Male adults were 12% less likely to be diagnosed with hypertension compared to female participants (aPR = 0.88, 95% CI = 0.51–1.51). Overweight or obese individuals were 1.69 times more likely to have been diagnosed with hypertension than those with a normal weight (aPR = 1.69, 95% CI = 1.35–2.11). The PR for the retirement group in occupation category (compared to day labor) is 1.73, indicating that individuals in this category have a 73% higher prevalence of the outcome compared to day labor (aPR = 1.73, 95% CI = 1.19–2.52). Adults in the 35–44 age group were 1.91 times more likely to have hypertension compared to those in the 18–24 age group (aPR = 1.91, 95% CI = 0.86–4.21). Additionally, individuals aged 55 years and above were 3.52 times more likely to be diagnosed with hypertension than those in the 18–24 age group. These age-related associations were statistically significant, with 95% confidence intervals of 1.62–7.66. This indicates that older individuals have a significantly higher prevalence of the outcome compared to younger individuals.
We used a random forest model to identify the top five important variables on defining diagnosed hypertension among the adult Bangladeshis in a sensitivity analysis. The values of mean decrease accuracy estimate the prediction measure of significance. If a particular variable is removed from the model, the higher it is for a predictor, the more the precision will decrease. The overall precision of the test data is 88.2 percent (see Supplementary Fig. S4). The supplementary figure shows that, according to the measure of importance, the top 5 potential predictors are: age, sex, employment status, coastal residency, and physical activity. We also have conducted a sensitivity analysis by incorporating additional variables into the Poisson regression model to explore potential counterintuitive findings and identify aspects that may warrant further investigation. The results are given in Supplementary Table S2. Coastal residency was consistently found to be significant across all models, even after adjusting for confounders, highlighting its robust association with the outcome.
Discussion
The study’s investigation of hypertension prevalence in adults residing in coastal and non-coastal regions provides insightful observations regarding geographic disparities. The descriptive analysis revealed a significantly elevated prevalence of diagnosed hypertension among adults in coastal areas compared to their non-coastal counterparts. This pattern persisted across diverse age groups, indicating a consistent trend of higher hypertension prevalence in coastal regions, albeit with a diminishing gap in older age brackets. These findings align with previous studies in Bangladesh, reporting hypertension prevalence ranging from 6.2% to 26.2% across different regions and demographics30,31. A comprehensive nationwide survey in Bangladesh conducted in 2017–2018 revealed that approximately 28% of the population had hypertension, with 16% of cases being undiagnosed and 12% diagnosed21. Another study with one rural district in Bangladesh, the prevalence was 6.9%, with higher rates among women (8.9%) compared to men (4.5%)22. Similar trends in hypertension prevalence have been observed internationally, including in regions such as China, and India32,33. The low prevalence of diagnosed hypertension also indicate that undiagnosed hypertension is a significant issue in Bangladesh, affecting both coastal and non-coastal rural regions. The high rates of undiagnosed cases suggest a need for improved screening and awareness programs, especially in rural and lower socioeconomic areas.
The adjusted analysis, utilizing modified Poisson regression, reaffirmed key associations in hypertension prevalence and living in coastal regions. Coastal residency emerged as a significant predictor, indicating that adults in coastal areas were more likely to have hypertension compared to their non-coastal counterparts. Gender differences were notable, with males having a lower likelihood of hypertension diagnosis than females but the difference is not independently significant. Hypertension is generally more common in males, especially in younger age groups. However, females experience a sharper increase in blood pressure from the third decade of life, leading to a higher prevalence in older age groups and it is also found in another study34.
Factors such as BMI and age also exerted substantial influences, with overweight or obese individuals and older adults exhibiting a higher likelihood of hypertension. These findings resonate with existing research that identifies water salinity, gender, age, and lifestyle habits as substantial contributors to hypertension rates35,36,37. While both BMI and physical activity independently affect hypertension risk, they may also interact. Physical activity can help mitigate some of the hypertension risk associated with higher BMI38. Individuals with more schooling tend to have less active lifestyles and higher BMIs, both of which contribute to elevated blood pressure. Coastal living may further amplify these risks.
A Study has linked saline water consumption to elevated blood pressure, underscoring the potential impact of environmental factors on public health24. Coastal populations have a higher risk of hypertension due to the tradition of salting and drying fish, which increases salt intake in these populations. The high amount of salt used for salting fish can have an undesirable effect on blood pressure.
Our study reveals that younger adults residing in coastal regions exhibit a higher susceptibility to hypertension compared to their non-coastal counterparts. This aligns with findings from a study conducted in coastal villages of Udupi district in southern India, which observed a substantial proportion of pre-hypertensives and identified a moderate to high risk of pre-hypertensives progressing to hypertension among younger adults39. Certain coastal occupations, particularly those involving strenuous physical labor, can have complex effects on hypertension risk. Fish farming is considered a physically demanding occupation, with high workloads and awkward work positions for prolonged periods. Fishery workers were found to have a higher incidence of cardiometabolic diseases, which may include hypertension40. Younger individuals in our study may be more biologically susceptible to the effects of a high-salt diet, resulting in a more immediate impact on their health. Additionally, they may engage in other lifestyle behaviors, such as physical inactivity or poor dietary habits, that further intensify the effects of high salt intake. In contrast, older individuals might have developed a degree of adaptation or resilience over time due to prolonged exposure, making them less affected by acute changes in salt consumption.
Studies conducted in different time frames and regions consistently highlight the multifaceted nature of hypertension prevalence, underscoring the intricate interplay between geographical, environmental, cultural, and individual factors in shaping public health outcomes38,39,40,41,42,43. In our study, we found hypertension is influenced by lifestyle factors like smoking, tobacco use, and physical inactivity. Managing these behaviors through lifestyle modifications can be essential for both preventing and controlling high blood pressure. A study conducted among a Bangladeshi population explored the use of telemedicine as a strategy to alleviate the burden of hypertension44. These findings not only enhance our understanding of regional variations in hypertension but also highlight the significance of implementing tailored interventions that account for the diverse factors influencing health within specific geographic settings.
The strength of this study indicates a notably higher prevalence of diagnosed hypertension among adults in coastal areas, a pattern consistent across age groups. This disparity may be attributed to environmental factors, particularly the increased salt consumption common in coastal regions. Lifestyle elements such as physical inactivity and unhealthy habits like chewing tobacco further compound the risk of hypertension in these areas. The study also highlights the alarming issue of undiagnosed hypertension, especially in rural and low-income communities. This finding emphasizes the critical need for enhanced screening and awareness initiatives to effectively identify and manage hypertension. By comprehending the intricate relationship between geographical, environmental, and lifestyle factors, we can craft targeted interventions tailored to the specific needs of both coastal and non-coastal populations. Future studies should investigate the long-term effects of climate change on hypertension prevalence and evaluate the efficacy of various interventions in reducing the risks associated with this chronic condition.
Limitations of the study
It is crucial to recognize and address the limitations inherent in this study. Firstly, the participants were exclusively drawn from two coastal areas, which inherently restricts the generalizability of the findings to encompass all coastal regions. Consequently, caution should be exercised when extrapolating these results into a broader context. Moreover, the study refrains from endorsing the testing of causal relationships. The nature of the research design precludes the establishment of direct cause-and-effect associations, emphasizing the need for prudence in interpreting the observed correlations. The data on lifestyle factors and medical history were self-reported, which may be subject to bias. Additionally, dietary factors should be considered to better understand the complex factors contributing to developing hypertension in coastal and non-coastal regions.
Conclusion
The research indicates an increased risk of hypertension in coastal populations compared to non-coastal areas. The low prevalence of diagnosed hypertension suggests undiagnosed hypertension is a significant issue in both coastal and non-coastal rural areas of Bangladesh, highlighting the need for better screening and awareness programs, especially in rural, low-income regions. The study has highlighted the multifaceted nature of hypertension’s determinants, revealing that geographical location, gender, BMI, and age all have significant impacts on the high prevalence of diagnosed hypertension among adults. Addressing these factors, particularly among younger adults in coastal regions, requires targeted interventions, including the promotion of healthy lifestyles, enhanced healthcare access, and heightened awareness of hypertension risks. These findings stress the importance of continued research into the complex interplay of these factors in hypertension to refine our understanding and improve healthcare approaches.
Data availability
The protocol, data, and questionnaire are accessible in the public domain at https://osf.io/ka6sj/.
References
World Health Organization. A global brief on hypertension: Silent killer, global public health crisis. WHO, Geneva. Available from https://www.who.int/publications/i/item/a-global-brief-on-hypertension-silent-killer-global-public-health-crisis-world-health-day-2013#. Accessed 11 Dec 2023 (2013).
Lim, S. S. et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England) 380(9859), 2224–2260. https://doi.org/10.1016/S0140-6736(12)61766-8 (2012).
World Health Organization. The top 10 causes of death. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 24 November 2023.
Chowdhury, S. R., Chandra Das, D., Sunna, T. C., Beyene, J. & Hossain, A. Global and regional prevalence of multimorbidity in the adult population in community settings: A systematic review and meta-analysis. EClinicalMedicine 16(57), 101860. https://doi.org/10.1016/j.eclinm.2023.101860 (2023).
Hossain, A. et al. Chronic illness and quality of life 5 years after displacement among rohingya refugees in Bangladesh. JAMA Netw. Open. 7(9), e2433809. https://doi.org/10.1001/jamanetworkopen.2024.33809 (2024).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet (London, England) 389(10064), 37–55. https://doi.org/10.1016/S0140-6736(16)31919-5 (2017).
Mills, K. T. et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 134(6), 441–450. https://doi.org/10.1161/CIRCULATIONAHA.115.018912 (2016).
World Health Organization. Sustainable development goal 3: health. https://www.who.int/topics/sustainable-development-goals/targets/en/. Accessed 30 November 2023.
Rust, P. & Ekmekcioglu, C. Impact of salt intake on the pathogenesis and treatment of hypertension. Adv. Exp.Med. Boil. 956, 61–84. https://doi.org/10.1007/5584_2016_147 (2017).
Khalesi, S. et al. Reducing salt intake: A systematic review and meta-analysis of behavior change interventions in adults. Nutr. Rev. 80(4), 723–740. https://doi.org/10.1093/nutrit/nuab110 (2022).
Hossain, A. et al. Natural disasters, livelihood, and healthcare challenges of the people of a riverine island in Bangladesh: A mixed-method exploration. PLoS One. 19(3), e0298854. https://doi.org/10.1371/journal.pone.0298854 (2024).
Benneyworth, L. et al. Drinking water insecurity: Water quality and access in coastal south-western Bangladesh. Int. J. Environ. Health Res. 26(5–6), 508–524. https://doi.org/10.1080/09603123.2016.1194383 (2016).
Bhalachandran, S. et al. On the processes influencing rapid intensity changes of tropical cyclones over the Bay of Bengal. Sci. Rep. 9(1), 3382. https://doi.org/10.1038/s41598-019-40332-z (2019).
Scheelbeek, P. F. D. et al. Drinking water salinity and raised blood pressure: Evidence from a cohort study in coastal Bangladesh. Environ. Health Perspect. 125(5), 057007. https://doi.org/10.1289/EHP659 (2017).
Rashid, M. B. et al. Human exposures to multiple water sources in the southwestern coastal region of Bangladesh: Water quality, pollution sources, and preliminary health risks appraisals. Environ. Sci. Pollut. Res. Int. 30(37), 88132–88154. https://doi.org/10.1007/s11356-023-28108-5 (2023).
Naser, A. M. et al. Drinking water salinity, urinary macro-mineral excretions, and blood pressure in the southwest coastal population of Bangladesh. J. Am. Heart Assoc. 8(9), e012007. https://doi.org/10.1161/JAHA.119.012007 (2019).
Shammi, M., Rahman, M. M., Bondad, S. E. & Bodrud-Doza, M. Impacts of salinity intrusion in community health: A review of experiences on drinking water sodium from coastal areas of Bangladesh. Healthc. (Basel, Switz.) 7(1), 50. https://doi.org/10.3390/healthcare7010050 (2019).
Akter, T. et al. Water quality index for measuring drinking water quality in rural Bangladesh: A cross-sectional study. J. Health Popul. Nutr. 35, 4. https://doi.org/10.1186/s41043-016-0041-5 (2016).
Schmidt, C. W. Another side of a low-salt diet: Reductions in the salinity of drinking water may lower blood pressure. Environ. Health Perspect. 125(6), 064002. https://doi.org/10.1289/EHP2099 (2017).
National Institute of Population Research and Training, Mitra and Associates, ICF International. Bangladesh demographic and health survey 2011. NIPORT, Mitra and Associates, and ICF International Dhaka, Bangladesh- Calverton, Maryland, USA. Available from https://dhsprogram.com/publications/publication-fr265-dhs-final-reports.cfm (2013)
Hossain, A. et al. Hypertension and undiagnosed hypertension among Bangladeshi adults: Identifying prevalence and associated factors using a nationwide survey. Front. Publ. health 10, 1066449. https://doi.org/10.3389/fpubh.2022.1066449 (2022).
Islam, J. Y. et al. Sex differences in prevalence and determinants of hypertension among adults: A cross-sectional survey of one rural village in Bangladesh. BMJ Open. 10(9), e037546. https://doi.org/10.1136/bmjopen-2020-037546 (2020).
Zaman, M. M. et al. Clustering of non-communicable diseases risk factors in Bangladeshi adults: An analysis of STEPS survey 2013. BMC publ. Health 15, 659. https://doi.org/10.1186/s12889-015-1938-4 (2015).
Country Office for Bangladesh of World Health Organization. Non-Communicable Disease Risk Factor Survey Bangladesh 2010 (Country Office for Bangladesh of WHO, 2011).
Sayeed, M. A. et al. Prevalence of hypertension in people living in coastal areas of Bangladesh. Ibrahim Med. Coll. J. 9(1), 11–17 (2016).
Chowdhury, M. A., Uddin, M. J., Haque, M. R. & Ibrahimou, B. Hypertension among adults in Bangladesh: Evidence from a national cross-sectional survey. BMC Cardiovasc. Disord. 16, 22 (2016).
Talukder, M. R. R., Rutherford, S., Phung, D., Islam, M. Z. & Chu, C. The effect of drinking water salinity on blood pressure in young adults of coastal Bangladesh. Environ. Pollut. 214, 248–254. https://doi.org/10.1016/j.envpol.2016.03.074 (2016).
Chowdhury, S. R., Islam, M. N., Sheekha, T. A., Kader, S. B. & Hossain, A. Prevalence and determinants of non-communicable diseases risk factors among reproductive-aged women: Findings from a nationwide survey in Bangladesh. PloS one 18(6), e0273128. https://doi.org/10.1371/journal.pone.0273128 (2023).
WHO Technical document. Global physical activity questionnaire (GPAQ), Available from https://www.who.int/publications/m/item/global-physical-activity-questionnaire. Accessed 15 Oct 2024 (2021).
World Health Organization. Country office for Bangladesh. National STEPS survey for non-communicable diseases risk factors in Bangladesh 2018. World Health Organization. Country Office for Bangladesh. https://apps.who.int/iris/handle/10665/332886 (2018).
Khan, M. N. et al. Prevalence, awareness, treatment, and control of hypertension in Bangladesh: Findings from national demographic and health survey, 2017–2018. J. Clin. Hypertens. 23(10), 1830–1842. https://doi.org/10.1111/jch.14363 (2021).
Lin, H. et al. Prevalence of hypertension and 10-year cardiovascular disease risk among older adults living in Quanzhou, a coastal region of southeast China. Risk Manag. Healthc. Policy 15, 1045–1053. https://doi.org/10.2147/RMHP.S341148 (2022).
Deo, M. G., Pawar, P. V., Kanetkar, S. R. & Kakade, S. V. Prevalence and risk factors of hypertension and diabetes in the Katkari tribe of coastal Maharashtra. J. Postgrad. Med. 63(2), 106–113. https://doi.org/10.4103/0022-3859.194204 (2017).
Connelly, P. J., Currie, G. & Delles, C. Sex differences in the prevalence outcomes and management of hypertension. Curr. Hypertens. Rep. 24(6), 185–192. https://doi.org/10.1007/s11906-022-01183-8 (2022).
Al Nahian, M. et al. Drinking water salinity associated health crisis in coastal Bangladesh. Elementa https://doi.org/10.1525/elementa.143 (2018).
Khan, J. R., Awan, N., Archie, R. J., Sultana, N. & Muurlink, O. The association between drinking water salinity and hypertension in coastal Bangladesh. Glob. Health J. 4(4), 153–158. https://doi.org/10.1016/j.glohj.2020.11.001 (2020).
Scheelbeek, P. F. D., Khan, A. E., Mojumder, S., Elliott, P. & Vineis, P. Drinking water sodium and elevated blood pressure of healthy pregnant women in salinity-affected coastal areas. Hypertension 68(2), 464–470. https://doi.org/10.1161/HYPERTENSIONAHA.116.07743 (2016).
Dun, Q. et al. Physical activity, obesity, and hypertension among adults in a rapidly urbanised city. Int. J. Hypertens. 11(2021), 9982562. https://doi.org/10.1155/2021/9982562 (2021).
Kini, S., Kamath, V. G., Kulkarni, M. M., Kamath, A. & Shivalli, S. Pre-hypertension among young adults (20–30 Years) in coastal villages of Udupi district in Southern India: An alarming scenario. PLoS One. 11(4), e0154538. https://doi.org/10.1371/journal.pone.0154538 (2016).
Lin, M. S., Lin, Y. C., Huang, T. J. & Chen, M. Y. Health inequality among fishery workers during climate change: A national population-based and retrospective longitudinal cohort study. Int. J. Environ. Res. Pub. Health. 19(16), 10281. https://doi.org/10.3390/ijerph191610281 (2022).
Rasheed, S. et al. Salt intake and health risk in climate change vulnerable coastal Bangladesh: What role do beliefs and practices play?. PLoS ONE 11, e0152783 (2016).
Hossain, A. et al. Medication adherence and blood pressure control in treated hypertensive patients: first follow-up findings from the PREDIcT-HTN study in Northern Bangladesh. BMC Pub. Health. 25(1), 250. https://doi.org/10.1186/s12889-025-21409-z (2025).
Hossain, A. et al. Palliative care needs and quality of life among adults with advanced chronic illnesses in low-income communities of Bangladesh. BMC Palliat Care. 24(1), 18. https://doi.org/10.1186/s12904-024-01643-9 (2025).
A. Hossain et al. Assessing the efficacy of telephone telemedicine in enhancing follow-up visits for non-adherence hypertensive patients: A cross-sectional study in Northern Bangladesh. In 2024 IEEE 48th Annual Computers, Software, and Applications Conference (COMPSAC) 1929–1933 https://doi.org/10.1109/COMPSAC61105.2024.00306 (Osaka, Japan, 2024)
Funding
This research did not receive funding from any public, commercial, or not-for-profit agency.
Author information
Authors and Affiliations
Contributions
AH, GUA and SRS formulated and planned the experiments. AH devised the analytical approach and conducted the data analysis. AH, SRS, MJS, and MZH drafted the manuscript. AH, SRS, MJS, GUA, MZH, MAH, HH, RC and AS participated in editing, reviewing, and contributing to the acquisition and interpretation of data for the work. AH is accountable for the overall content as the guarantor. All authors contributed to the critical revision and endorsed the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study received ethical clearance from the National Research Ethics Committee, adhering to the ethical guidelines of the Bangladesh Medical Research Council (BMRC) with the reference number 25003092020. The respondents and/or their legal representatives provided written informed consent, acknowledging the study’s objectives, procedures, associated risks and benefits, voluntary participation rights, the option to withdraw, and the assurance of data anonymity and confidentiality.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hossain, A., Sultana, S.R., Sujan, M.J. et al. Coastal residency and its association with diagnosed hypertension based on findings from a cross-sectional study in rural Bangladesh. Sci Rep 15, 10278 (2025). https://doi.org/10.1038/s41598-025-94983-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94983-2
Keywords
This article is cited by
-
Social-ecological-technological drivers of freshwater salinization in the Occoquan Reservoir, United States
Communications Earth & Environment (2026)