Abstract
Air pollution is associated with hyperuricemia; however, its underlying mechanism remains poorly understood. In this retrospective analysis, 233 anonymous health data and urban air pollutants data were obtained. The mean daily exposure dose (DED) for combined air pollutants (CAPs) was 1.22 mg/day, which was defined as the threshold for dividing all individuals into two groups. The lower-exposure group (LEG) included those with a DED–CAPs less than or equal to 1.22 mg/day and the higher-exposure group (HEG) included those with a DED–CAPs that exceeded 1.22 mg/day. The peripheral blood cell counts of white blood cells, eosinophils, basophils, monocytes, and red blood cells were higher in the HEG than in the LEG, whereas peripheral platelet counts were lower in the HEG than in the LEG. In addition, serum uric acid (UA) levels were higher in the HEG than in the LEG. Multivariable-adjusted linear regression models suggested that with an increase in the daily exposure dose to air pollution, peripheral blood cells and serum UA levels increased. The results of mediation effect models further indicated that peripheral monocyte counts play a mediating role in the dose effect relationships between air pollutant exposures and serum UA levels. These results highlight that air pollution may increase serum UA levels by altering hematocytes inducing low-grade inflammation, which may ultimately increase the risk of kidney dysfunction.
Similar content being viewed by others
Introduction
Uric acid (UA) is an end product of purine metabolism, two-thirds of which is eliminated by the kidney1,2. Abnormally elevated UA levels can induce hyperuricemia (men: serum UA > 420 µmol/L; women: serum UA > 360 µmol/L), which is a critical factor for gout and nephrolithiasis and a risk factor for cardiovascular disease, cerebrovascular stroke, chronic kidney disease, hypertension, and metabolic syndrome1,3,4,5. Generally, serum UA levels can be increased in two ways. First, genetic, environmental and other exogenous factors disturb the balance of purine metabolism and promote UA accumulation. Second, UA excretion decreases due to weakened kidney function2. Recently, the critical role of environmental pollution in increasing serum UA levels has gained attention2,6.
Air pollution is closely related to public health, and accumulating evidence has revealed its toxic effects on kidney dysfunction6,7,8,9,10,11,12,13. The results of a retrospective analysis showed that combined exposure to air pollutants accelerated the risk of kidney impairment and increased serum UA concentrations in adult women10. In older men, exposure to fine particulate matter (PM2.5, aerodynamic diameter ≤ 2.5 μm) was positively related with serum UA levels and chronic kidney disease (CKD) risk14. A prospective cohort study conducted among healthy traffic police officers also suggested that ambient air pollution was associated with the incidence of hyperuricemia4. Exposure during pregnancy to air PM2.5 was associated with weakened kidney function and increased serum UA levels, consequently reducing newborn birth weight6,12. Additionally, in patients with IgA nephropathy, air PM2.5 exposure was found to be an independent risk factor for impaired kidney function9. Although the relationship between air pollution and increased serum UA concentrations has been highlighted, the potential mechanisms remain poorly understood.
Air pollution has been linked to alterations in peripheral blood cells13,15,16. Chronic exposure to air PM2.5 could increase total leukocyte, neutrophil, and monocyte counts in preschool children17. In Flemish adolescent boys, long-term exposure to PM2.5, PM10, and NO2 was positively associated with the total leukocyte, neutrophil, and lymphocyte counts18. The effects of short-term exposure also suggest that air CO, SO2, and NO2 pollution may be related to the modification of leukocyte counts19. Peripheral blood cells are also associated with kidney impairment20,21,22,23. Deng et al. found, patients with systemic lupus erythematosus (SLE) had significantly higher monocyte and granulocyte levels20. Kidney ischemia/reperfusion (IR) injury can rapidly induce monocyte and neutrophil infiltration22. A community-based cohort study showed that peripheral leukocytes and their subsets were negatively related to the estimated glomerular filtration rate (eGFR), and patients with CKD had higher counts of total leukocytes and their subsets23. Moreover, peripheral neutrophils are an independent risk factor for rapid renal progression, whereas an increased peripheral eosinophil count is an independent predictor of end-stage-kidney-disease21,23.
Therefore, we hypothesized that air pollutant increases serum UA levels by altering peripheral blood cells inducing low-grade inflammation, which may ultimately increase the risk of kidney dysfunction. We estimated the daily exposure dose (DED) of air pollution and the combined toxic effects of air pollutants (CAPs), measured the counts of peripheral blood cells (including total leukocytes and their subsets, red blood cells (RBCs), and platelets), and detected serum UA levels in a retrospective analysis. We also assessed the mediating effects of inflammation induced by peripheral blood cells’ alteration on the relationship between air pollution and serum UA levels.
Materials and methods
Study population
Individual electronic health data were extracted from the laboratory information system of the department of clinical laboratory medicine, Mianyang Central Hospital, September 2019. Firstly, the data collection was limited to individuals (20–67 years old) who underwent health examinations. Secondly, individuals with incomplete information were excluded. Thirdly, individuals with a history of gout, kidney impairment, or other chronic diseases were excluded. Fourthly, individuals who had lived at their current address in Mianyang City for less than 1 year were also excluded. At last, a total of 233 individuals were included in this retrospective analysis. Pan-informed consent was obtained at the time of each patient’s medical visit, and all data were handled anonymously. This retrospective study was approved by the Biomedical Ethics Committee of Mianyang Central Hospital, China. All procedures were complied with the principles of declaration of Helsinki.
Biological sampling and laboratory testing
All procedures for fasting vein blood sampling and biological measurements were performed according to the quality and management guidelines of the International Standardization Organization (ISO) 15,189. Trained nurses collected blood samples in vacuum tubes (Becton Dickinson, USA). Ethylene diamine tetraacetic acid (EDTA) anticoagulant blood (2 mL) was collected to determine the counts of peripheral blood cells using a Sysmex XE-2100 automatic hematology analyzer (Sysmex, Japan)13,24,25. Heparin sodium anticoagulant blood (5 mL) was used to separate serum by centrifugation (room temperature, 1000×g for 15 min), and serum UA levels were measured using a Roche Cobas c701automatic biochemical analyzer (Roche, Switzerland)5,10.
Exposure assessment
In Mianyang City, four stations monitored air quality, which ensured that the activity radius of all individuals was less than 40 km (the threshold of the monitoring station data could be applied to evaluate individual exposure) from the nearest monitoring station10,13,26,27. Air quality data between September 2018 and September 2019 were obtained from the National Air Quality Forecast Information Publishing System (https://air.cnemc.cn:18014/). The annual-mean of all stations for each air pollutant (PM2.5, PM10, SO2, CO, O3, and NO2) was calculated as the pollutant concentration, and then individual DED was assessed using the verified mathematical equation: DED-i = concentration-i × inhalation rate × individual weight/reference weight, in which the “i” is one pollutant among PM2.5, PM10, SO2, CO, O3, and NO2, and other methods for parameters estimation have been introduced as detailed in our previous studies10,13,17,27. The geometric mean of all six air pollutants was calculated to assess the DED–CAPs, and then all individuals were divided into two groups depending on the mean DED–CAPs value. Briefly, the lower-exposure group (LEG) was included those having a DED–CAPs less than or equal to 1.22 mg/day and the higher-exposure group (HEG) included those having a DED–CAPs exceeded 1.22 mg/day.
Statistical analysis
Data are reported as mean and standard deviation (SD) or median (interquartile range, IQR), depending on the distribution characteristics that were estimated with the Kolmogorov–Smirnov test. Group differences in peripheral blood cell counts and serum UA levels were identified using the independent-sample t-test and Mann–Whitney U test. Pearson correlation analyses were conducted to assess the relationships among air pollution, peripheral blood cell counts, and serum UA levels; dose effects were further estimated using multivariate-adjusted linear regression models. The covariates included age, alanine aminotransferase (ALT), aspartate aminotransferase (AST), glucose (GLU), total cholesterol (TC), and triglyceride (TG) levels5,10. To investigate whether peripheral blood cell counts play a mediating role in the relationship between air pollution and serum UA levels, we used mediation models with bootstrapping25,27,28. SPSS 22.0 (IBM, Armonk, NY, USA) and GraphPad Prism 8.0 (GraphPad, San Diego, CA, USA) were used for data analysis and figure generation, respectively. P < 0.05 was defined as the threshold of statistical significance in a two-tailed test.
Results and discussion
Air pollution and exposure characteristics
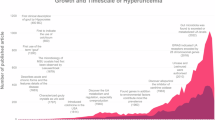
As shown in Fig. 1, the annual mean values were 39.04, 60.95, 5.41, 29.41, 95.76, and 659.60 µg/m3 for PM2.5, PM10, SO2, NO2, O3, and CO, respectively. The mean annual value of the calculated CAPs was 50.92 µg/m3. These results suggested that the air quality of Mianyang was worse than that of Suining but better than that of Chengdu, Chongqing, and Fuling13,27,29,30,31. Because these cities are all in the Sichuan Basin, where they share similar climatic conditions, the air quality differences may be attributed to differences in urbanization status, industrialization levels, traffic flow, and population density 13,31. In addition, all levels of air pollutants in Mianyang far exceeded the latest guideline thresholds issued by the World Health Organization (WHO), indicating that air pollution remains a severe challenge in Mianyang11,32,33. Concomitantly, the DED mean values were 0.89, 1.39, 0.12, 0.66, 2.16, 14.97, and 1.22 mg/day for PM2.5, PM10, SO2, NO2, O3, CO, and CAPs, respectively (Fig. 1).
Distribution characteristics of peripheral blood cells and serum UA levels
In total, 233 individuals who underwent health examinations were included in this retrospective study. According to the mean value of individual DED–CAPs, 109 people (mean-age: 39.53 years old) were categorized into LEG group and 124 (mean-age: 39.55 years old) into HEG group. The results of group differentiation analysis showed that, except for the neutrophil and lymphocyte counts, the distribution of peripheral blood cells between the LEG and HEG were statistically significantly different (Table 1). The peripheral counts of white blood cells (WBCs, 6.19 × 109/L vs. 5.78 × 109/L), eosinophils (0.12 × 109/L vs. 0.09 × 109/L), basophils (0.03 × 109/L vs. 0.02 × 109/L), monocytes (0.41 × 109/L vs. 0.35 × 109/L), and RBCs (5.11 × 1012/L vs. 4.44 × 1012/L) were higher in the HEG than in the LEG, whereas the platelet counts (180.49 × 109/L vs. 197.08 × 109/L) was lower in the HEG than in the LEG (all P < 0.05). In flemish adolescents exposed to PM2.5, PM10, and NO2, boys had higher counts of WBCs, neutrophils, and lymphocytes, whereas girls showed no significant differences18. In Kaohsiung adults, the counts of WBC, neutrophil, and monocyte increased in the peripheral blood after short-term exposure to CO but decreased when exposed to SO2 19. In an e-waste area, chronic exposure to PM2.5 increased the WBC, neutrophil, and monocyte counts in preschool children17. In healthcare workers, our previous studies suggested that long-term exposure to air pollution could elevate the peripheral counts of WBC, lymphocytes, and monocytes13,27. Although the results are inconsistent owing to population and geographical differences, these studies emphasize that air pollution may be related to peripheral blood cell distribution. These phenomena may be attributed to air pollution having adverse effects on progenitor cell differentiation and maturation directly through oxidative stress injury, resulting in hematotoxicity34,35,36.
The mean level of serum UA in the HEG was 424.76 µmol/L, which was higher than that in the LEG (mean level: 334.57 µmol/L, P < 0.001) (Fig. 2). This result showed that the mean serum UA level in the HEG exceeded the threshold for hyperuricemia in men3,5,37. Studies are increasingly indicating that exposure to air pollutants can elevate public serum UA levels and impair kidney function, especially exposure to air PM2.5, which plays an independent role in kidney failure risk in patients with IgA nephropathy4,9,10,12,14. In summary, our results are consistent with those of previous studies, which have highlighted that long-term exposure to air pollution may alter serum UA levels and ultimately increase the risk of hyperuricemia.
Associations among air pollutant DEDs, serum UA levels, and peripheral blood cells
The Pearson correlation models showed that individual air pollutant DEDs (PM2.5, PM10, SO2, NO2, O3, CO, and CAPs) were positively related to serum UA levels (rs = 0.460, rs = 0.460, rs = 0.457, rs = 0.458, rs = 0.457, rs = 0.460, and rs = 0.459, respectively, all P < 0.001) and the peripheral blood cell counts of monocytes (rs = 0.185, rs = 0.185, rs = 0.184, rs = 0.183, rs = 0.184, rs = 0.186, and rs = 0.185, respectively, all P < 0.01), eosinophils (rs = 0.267, rs = 0. 267, rs = 0. 267, rs = 0. 267, rs = 0. 267, rs = 0. 267, and rs = 0. 267, respectively, all P < 0.001), basophils (rs = 0.136, rs = 0.136, rs = 0.138, rs = 0.139, rs = 0.138, rs = 0.135, and rs = 0.137, respectively, all P < 0.05), and RBCs (rs = 0.574, rs = 0.574, rs = 0.572, rs = 0.571, rs = 0.573, rs = 0.575, and rs = 0.573, respectively, all P < 0.001) but negatively related to peripheral platelet counts (rs = − 0.188, rs = − 0.188, rs = − 0.189, rs = − 0.189, rs = − 0.188, rs = − 0.188, and rs = − 0.188, respectively, all P < 0.01) (Fig. 3). Serum UA levels were significantly associated with peripheral blood cell counts (all P < 0.05), including WBCs (rs = 0.151), monocytes (rs = 0.208), eosinophils (rs = 0.143), basophils (rs = 0.145), and RBCs (rs = 0.324) (Fig. 3).
Pearson correlations among air pollution, hematocyte, and serum UA levels. BA basophil, CAPs combined of air pollutants, DED daily exposure dose, EO eosinophil, LY lymphocyte, MO monocyte, NE neutrophil, PLT platelet, PM particulate matter, RBC red blood cell, UA uric acid, WBC white blood cell; *P < 0.05, **P < 0.01, ***P < 0.001.
To further assess the relationship between the toxic-effects of air pollutants on serum UA levels and peripheral blood cells, multivariate-adjusted linear regression models were used. Regardless of whether they were adjusted for covariates (age, ALT, AST, GLU, TC, and TG), we found significant correlations between air pollutant DEDs, serum UA levels, and peripheral blood cell counts (except for basophils) (Table 2). The unstandardized coefficient (B) and 95% confidence interval (CI) were (I) DED-PM2.5: 418.132 (284.068, 552.197) for serum UA levels, 0.223 (0.016, 0.430) for monocytes, 0.296 (0.132, 0.460) for eosinophils, 3.977 (3.174, 4.781) for RBCs and − 103.874 (− 201.266, − 6.483) for platelets, respectively (all P < 0.05); (II) DED-PM10: 268.301 (182.362, 354.241) for serum UA levels, 0.143 (0.010, 0.276) for monocytes, 0.190 (0.085, 0.295) for eosinophils, 2.550 (2.035, 3.066) for RBCs and − 66.605 (− 129.042, − 4.168) for platelets, respectively (all P < 0.05); (III) DED-SO2: 3019.736 (2043.370, 3996.101) for serum UA levels, 1.607 (0.100, 3.115) for monocytes, 2.158 (0.965, 3.351) for eosinophils, 28.868 (23.012, 34.723) for RBCs and − 753.129 (− 1461.879, − 44.379) for platelets, respectively (all P < 0.05); (IV) DED-NO2: 556.331 (376.591, 736.071) for serum UA levels, 0.295 (0.018, 0.573) for monocytes, 0.398 (0.178, 0.617) for eosinophils, 5.305 (4.226, 6.384) for RBCs and − 138.179 (− 268.656, − 7.701) for platelets, respectively (all P < 0.05); (V) DED-O3: 170.435 (115.191, 225.679) for serum UA levels, 0.091 (0.006, 0.176) for monocytes, 0.122 (0.055, 0.190) for eosinophils, 1.634 (1.303, 1.965) for RBCs and − 42.624 (− 82.718, − 2.530) for platelets, respectively (all P < 0.05); (VI) DED-CO: 24.827 (16.905, 32.749) for serum UA levels, 0.013 (0.001, 0.025) for monocytes, 0.017 (0.008, 0.027) for eosinophils, 0.236 (0.188, 0.283) for RBCs and − 6.165 (− 11.924, − 0.407) for platelets, respectively (all P < 0.05); (VII) DED–CAPs: 304.595 (206.603, 402.587) for serum UA levels, 0.162 (0.011, 0.314) for monocytes, 0.217 (0.097, 0.336) for eosinophils, 2.904 (2.316, 3.491) for RBCs and − 75.786 (− 146.953, − 4.619) for platelets, respectively (all P < 0.05).
Our prior study in healthy adult women indicated that the combined toxic effects of outdoor air pollution were positively associated with serum UA levels and CKD incidence risk10. Exposure to PM2.5 during pregnancy can increase serum UA levels and impair kidney function in both pregnant women and newborns6,12. In traffic officers, air pollution enhanced hyperuricemia risk; especially in men, PM (PM1, PM2.5, and PM1 − 2.5) exposure notably elevated serum UA levels4,37. In addition, long-term exposure to air PM (PM1, PM2.5, and PM10) increased the hyperuricemia odds ratio, whereas short-term exposure to PM2.5 increased serum UA levels and CKD risk14,38. In accordance with these above results, air pollution increasing serum UA levels and decreasing kidney function were further demonstrated in this present study. Our results also indicate that, consistent with previous studies, air pollution may induce alterations in peripheral blood cells13,15,16,17,18,19,27. Prior studies showed the similar results with the negative association between air pollution and platelets, which maybe linked with hypomethylation of platelet mitochondrial DNA39,40. In addition, platelets are the pivotal elements in hemostasis and thrombosis41,42. Therefore, we speculate that exposure to air pollution may increase bleeding risk by down-regulation platelets.
The results of further analysis showed that in the unadjusted model, increased counts of peripheral blood cells (including WBCs, monocytes, eosinophils, basophils, and RBCs) were significantly associated with increased serum UA levels (all P < 0.05) (Table 3). When adjusted for covariates (age, ALT, AST, GLU, TC, and TG), the correlation remained statistically significant (except for WBCs and eosinophils), although the correlation coefficient decreased (all P < 0.05) (Table 3). With a one unit increase in monocytes (109/L), basophils (109/L), and RBCs (1012/L), serum UA levels will increase 101.457, 657.386, and 43.590 µmol/L, accordingly. Previous studies have demonstrated a relationship between peripheral blood cells and kidney impairment20,21,22,23. Moreover, population-based studies have indicated that leukocytes and their subsets are negatively related to eGFR, peripheral neutrophil count is an independent risk factor for rapid renal progression, and an increased peripheral eosinophil count is an independent predictor of end-stage kidney disease21,23. Our results highlight the effect of dose between peripheral blood cells on serum UA levels, which may increase the risk of kidney impairment.
Mediating role of peripheral blood cells between air pollution and serum UA levels
To identify the mediating role of peripheral blood cells in air pollution and serum UA levels, mediation models were constructed by bootstrapping25,27,28. The results suggest that only peripheral monocyte counts had a partial mediating role between air pollution and serum UA levels after further controlling for age, ALT, AST, GLU, and TC levels (Fig. 4). The indirect effect of peripheral monocyte counts on exposure to air pollutants (PM2.5, PM10, SO2, NO2, O3, CO, and CAPs) increasing serum UA levels was 23.580 (3.467, 68.527), 15.112 (1.883, 42.938), 172.153 (22.104, 501.359), 31.689 (3.531, 91.643), 9.742 (1.058, 27.769), 1.391 (0.190, 4.201), and 17.251 (2.510, 51.574), with a mediated proportion (Mppt) of 4.105%, 4.101%, 4.138%, 4.138%, 4.144%, 4.083%, and 4.118%, respectively (all P < 0.05) (Table S1 and Fig. 4). Although only peripheral monocyte counts were significant mediators of the relationship between air pollution and serum UA levels, our results highlight that exposure to air pollutants can elevate serum UA levels by increasing hematocyte counts advancing low-grade inflammation, consequently increasing the risk of kidney injury.
Mediating role of monocyte in dose-effect relationships among air pollution on serum uric acid. B unstandardized coefficient, CI confidence interval, CAPs combined of air pollutants, DED daily exposure dose, Mppt mediated proportion, PM particulate matter; Analyses were controlled by age, alanine aminotransferase, aspartate aminotransferase, glucose, and total cholesterol; Number of bootstrap samples for bias corrected bootstrap confidence intervals: 5000; *P < 0.05.
This study has several limitations. Firstly, this retrospective analysis does not allow determination of causality, which requires further investigation in future studies. Secondly, the geometric means assessing the combined effect for six air pollutants were based on the assumption that each pollutant has equal toxic effects, which may be overestimated the grouping differences, but the associations among air pollution, hematocytes, and kidney dysfunction were not changed. Thirdly, the small sample size of 233 participants limits the statistical power and generalizability of the findings, particularly in diverse populations with varying environmental and genetic backgrounds. In addition, there are some potential confounders such as dietary habits, socioeconomic status, physical activity, and pre-existing health conditions which did not record in the laboratory information system of the department of clinical laboratory medicine, Mianyang Central Hospital. Last but not least, personal wearable equipment was not applied to accurately monitor air pollutant exposure levels because the study was limited by retrospective analysis; however, a mathematical equation was employed to assess individual exposure doses with monitoring station air pollution data, which has been proven to be reliable10,13,26,27.
Conclusion
With this retrospective analysis, we are the first to evaluate the relationship between air pollution, inflammation based on peripheral blood cells, and serum UA levels. The results showed that air pollution remains a severe challenge in Mianyang, with high daily exposure doses and peripheral blood cells and serum UA levels being elevated in the public. In addition, peripheral monocyte count played a mediating role in the dose-dependent relationship between air pollutant exposure and serum UA levels. In summary, the results suggest that air pollution may increase serum UA levels by altering hematocytes inducing low-grade inflammation, which may ultimately enhance the risk of kidney dysfunction. Air quality has improved in recent decades because the “Air Pollution Prevention and Control Action” was implemented. However, to improve living spaces and public health, ecological and environmental protection policies must be implemented.
Data availability
All data generated or analysed during this study are included in this published article.
References
Lee, Y. J. et al. Relationship between bisphenol A, bisphenol S, and bisphenol F and serum uric acid concentrations among school-aged children. PloS One 17, e0268503 (2022).
Wu, Z. D. et al. Environmental factors and risk of gout. Environ. Res. 212, 113377 (2022).
Dong, X. et al. Residential greenness associated with lower serum uric acid levels and hyperuricemia prevalence in a large Chinese rural population. Sci. Total Environ. 770, 145300 (2021).
Tang, Y. X. et al. Association between ambient air pollution and hyperuricemia in traffic Police officers in China: A cohort study. Int. J. Environ. Health Res. 31, 54–62 (2021).
Wang, H. et al. Purine-induced IFN-γ promotes uric acid production by upregulating Xanthine oxidoreductase expression. Front. Immunol. 13, 773001 (2022).
Zhao, Y. et al. Fine particulate matter exposure and renal function: A population-based study among pregnant women in China. Environ. Int. 141, 105805 (2020).
Bouza, E. et al. Air pollution and health prevention: A document of reflection. Revista Espanola de Quimioterapia—Publicacion oficial de La. Sociedad Esp. De Quimioterapia 35, 307–332 (2022).
Han, C. et al. Mortality burden due to long-term exposure to ambient PM(2.5) above the new WHO air quality guideline based on 296 cities in China. Environ. Int. 166, 107331 (2022).
Luo, C. et al. Particulate matter of air pollution may increase risk of kidney failure in IgA nephropathy. Kidney Int. 102, 1382–1391 (2022).
Wang, H. H. et al. Combined toxicity of outdoor air pollution on kidney function among adult women in Mianyang City, Southwest China. Chemosphere 238, 124603 (2020).
World Health Organization. WHO Global Air Quality Guidelines. Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. World Health Organization, (2021). https://apps.who.int/iris/handle/10665/345329. Permission: CC BY-NC-SA 3.0 IGO.
Xie, G. et al. Associations among prenatal PM(2.5), birth weight, and renal function. Chemosphere 301, 134668 (2022).
Zhang, S. et al. The associations between air pollutant exposure and neutralizing antibody titers of an inactivated SARS-CoV-2 vaccine. Environ. Sci. Pollut. Res. Int. 29, 13720–13728 (2022).
Gao, X. et al. Short-term exposure to PM(2.5) components and renal health: Findings from the veterans affairs normative aging study. J. Hazard. Mater. 420, 126557 (2021).
Gao, X. et al. Impacts of air pollution, temperature, and relative humidity on leukocyte distribution: An epigenetic perspective. Environ. Int. 126, 395–405 (2019).
Gondalia, R. et al. Leukocyte traits and exposure to ambient particulate matter air pollution in the women’s health initiative and atherosclerosis risk in communities study. Environ. Health Perspect. 128, 17004 (2020).
Zhang, S. et al. Ambient fine particulate matter inhibits innate airway antimicrobial activity in preschool children in e-waste areas. Environ. Int. 123, 535–542 (2019).
Verheyen, V. J. et al. Long-term residential exposure to air pollution is associated with hair cortisol concentration and differential leucocyte count in Flemish adolescent boys. Environ. Res. 201, 111595 (2021).
Hung, S. C. et al. The association of white blood cells and air pollutants-A population-based study. Int. J. Environ. Res. Public Health 18, 2370 (2021).
Deng, Y. et al. Expression characteristics of interferon-stimulated genes and possible regulatory mechanisms in lupus patients using transcriptomics analyses. EBioMedicine 70, 103477 (2021).
Tariq, A. et al. Eosinophilia and risk of incident end stage kidney disease. BMC Nephrol. 21, 14 (2020).
Williams, T. M., Wise, A. F., Layton, D. S. & Ricardo, S. D. Phenotype and influx kinetics of leukocytes and inflammatory cytokine production in kidney ischemia/reperfusion injury. Nephrol. (Carlton Vic). 23, 75–85 (2018).
Yen, C. H. et al. The prognostic value of peripheral total and differential leukocyte count in renal progression: A community-based study. PloS One 16, e0258210 (2021).
Hu, J. et al. Increased body mass index linked to decreased neutralizing antibody titers of inactivated SARS-CoV-2 vaccine in healthcare workers. Obes. Sci. Pract. 9 (1), 23–29 (2022).
Zhang, S. et al. Oral antimicrobial activity weakened in children with electronic waste lead exposure. Environ. Sci. Pollut. Res. Int. 27, 14763–14770 (2020).
Bowe, B. et al. Associations of ambient coarse particulate matter, nitrogen dioxide, and carbon monoxide with the risk of kidney disease: A cohort study. Lancet Planet. Health. 1, e267–e276 (2017).
Zhang, S., Hu, J., Xiao, G., Chen, S. & Wang, H. Urban particulate air pollution linked to dyslipidemia by modification innate immune cells. Chemosphere 319, 138040 (2023).
Preacher, K. J. & Hayes, A. F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 40, 879–891 (2008).
Huang, Y. et al. Source apportionment and health risk assessment of air pollution particles in Eastern district of Chengdu. Environ. Geochem. Health 42, 2251–2263 (2020).
Qiao, B. et al. Characterization of water soluble inorganic ions and their evolution processes during PM(2.5) pollution episodes in a small City in Southwest China. Sci. Total Environ. 650, 2605–2613 (2019).
Wang, H. et al. Seasonal characteristics, formation mechanisms and source origins of PM2.5 in two megacities in Sichuan basin, China. Atmos. Chem. Phys. 18, 865–881 (2018).
Zhang, S., Chen, X., Dai, C., Wang, J. & Wang, H. Associations between air pollutants and risk of respiratory infection: Patient-based bacterial culture in sputum. Environ. Geochem. Health 44, 4007–4016 (2022).
Zhang, S. et al. Particulate air pollution and respiratory haemophilus influenzae infection in Mianyang, Southwest China. Environ. Sci. Pollut. Res. Int. 28, 33158–33164 (2021).
Scharf, P., Broering, M. F., Oliveira da Rocha, G. H. & Farsky, S. H. P. Cellular and molecular mechanisms of environmental pollutants on hematopoiesis. Int. J. Mol. Sci. 21, 6996 (2020).
Sun, R. et al. Ferroptosis is involved in the benzene-induced hematotoxicity in mice via iron metabolism, oxidative stress and NRF2 signaling pathway. Chem. Biol. Interact. 362, 110004 (2022).
Suzuki, T., Hidaka, T., Kumagai, Y. & Yamamoto, M. Environmental pollutants and the immune response. Nat. Immunol. 21, 1486–1495 (2020).
Tang, Y. X. et al. Exposure to ambient particulate matter and hyperuricemia: An 8-year prospective cohort study on male traffic officers in China. Ecotoxicol. Environ. Saf. 249, 114354 (2023).
Zeng, C. et al. The role of lipid profile in the relationship between particulate matters and hyperuricemia: A prospective population study. Environ. Res. 214, 113865 (2022).
Liu, Q. et al. Effects of short-term personal exposure to air pollution on platelet mitochondrial DNA methylation levels and the potential mitigation by L-arginine supplementation. J. Hazard. Mater. 417, 125963 (2021).
Qiu, W. et al. Short-term impacts of air pollution on the platelet-lymphocyte ratio and neutrophil-lymphocyte ratio among urban adults in China. J. Environ. Sci. (China) 125, 101–111 (2023).
Dai, Y. et al. Alterations in platelet indices link polycyclic aromatic hydrocarbons toxicity to low-grade inflammation in preschool children. Environ. Int. 131, 105043 (2019).
Zeng, Z. et al. Lead exposure is associated with risk of impaired coagulation in preschool children from an e-waste recycling area. Environ. Sci. Pollut Res. 25, 20670–20679 (2018).
Acknowledgements
We thank Editage (www.editage.cn) for English language editing during the preparation of this manuscript.
Funding
This work was supported by the High-level Talent Cultivation Project of Chengdu Medical College, China (KYPY22-08) and the Talent Introduction Research foundation of the Second Affiliated Hospital of Chengdu Medical College (Nuclear Industry 416 Hospital), China (SYL2024RCYJ003).
Author information
Authors and Affiliations
Contributions
Conceptualization, S.Z. and H.W.; methodology, S.Z. and H.W.; software, S.Z., J.W., Z.L., and Y.L.; validation, S.Z. and H.W.; formal analysis, H.W., J.W., Z.L., Y.L., H.Q. and G.X.; investigation, J.W. and X.C; resources, J.W.; data curation, S.Z. and H.W.; writing-original draft preparation, H.W.; writing-review and editing, S.Z.; visualization, S.Z. and H.W.; supervision, S.Z.; project administration, S.Z., H.W. and J.W.; funded, H.W. and S.Z.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, H., Li, Z., Wang, J. et al. Independent and joint air pollutants exposure associated with kidney dysfunction mediating by hematocyte. Sci Rep 15, 10033 (2025). https://doi.org/10.1038/s41598-025-95204-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95204-6