Abstract
Visual laryngoscope, as the most commonly used tracheal intubation tool in clinical practice, has a high intubation success rate and is quick to learn, but there are risks of over flexion of the neck, tooth loss, etc. The visual stylet helps to make up for these shortcomings. This study aimed to compare the effects of the visual stylet and visual laryngoscope on transoral single lumen tracheal intubation in non-difficult airways. The primary outcome was intubation time, and secondary outcomes included glottic exposure time, first success rates, hemodynamic indices, intubation-related complications. A total of 148 patients were included, with 75 in the visual stylet (VS) group and 73 in the visual laryngoscope (VL) group. The intubation time in the VS group was 35 (11) seconds, significantly shorter than the 41 (9) seconds in the VL group (P < 0.001). Immediately post-intubation, the MAP in the VS group was 80 (20.5) mmHg, lower than 87 (23) mmHg in the VL group (P < 0.01). Intubation-related complications are also lower in VS group compared to VL group. Other outcomes don’t have significant difference. Our study has demonstrated that the visual stylet significantly reduces intubation time and provides more stable hemodynamics. For patients with limited mouth opening, shorter thyromental distance, or higher Cormack-Lehane grades, the visual stylet may potentially be a better choice compared to video laryngoscopy for tracheal intubation.
Trial registration China Clinical Trial Registry (ChiCTR2100051812) (05/10/2021).
Similar content being viewed by others
Introduction
Endotracheal intubation is one of the basic techniques in clinical anesthesia, and exploring easier, faster, safer and more effective ways of intubation has always been the direction of clinical anesthesia efforts1,2. When performing tracheal intubation, anesthesiologists need to focus not only on how to improve the success rate of the first intubation, but should also pursue how to reduce the damage to the patient. Traditionally, tracheal intubation has mostly relied on exposure of the glottis through a laryngoscope, and in recent years, with the development of intubation tools such as light sticks, visual laryngoscopes, and fiberoptic bronchoscopes, the success rate of intubation has improved dramatically3,4. Currently, the most commonly used intubation tool in clinical practice is the visual laryngoscope, whose advantages of higher intubation success rate, lower learning difficulty and relatively low price make it the first choice for hospitals at all levels5. However, the use of video laryngoscopy still has drawbacks, such as the need for excessive neck flexion, the risk of tooth damage, potential pharyngeal injury, and significant hemodynamic fluctuations, and these disadvantages are notably correlated with the degree of difficult airway6,7. The disposable malleable visual stylet, with its adjustable tip curvature and reduced force required for glottic exposure, helps to address these limitations8,9.Our study investigates the clinical application effects of disposable malleable visual stylet compared to the visual laryngoscope in ordinary patients, exploring its feasibility as the preferred intubation tool.
Method
Study design
The study was a single center randomized controlled trial conducted at Sichuan Academy of Medical Sciences-Sichuan Provincial People’s Hospital. The trial was divided into 2 groups, the transoral single lumen tracheal intubation group using a disposable malleable visual stylet (Saixin Medical, SX-NK50A) (Visual stylet group, VS group), and the transoral single lumen tracheal intubation group using a visual laryngoscope (Zhejiang Youyi, VL300M) (Visual laryngoscope group, VL group). The study was approved by the Ethics Committee of Sichuan Academy of Medical Sciences-Sichuan Provincial People’s Hospital (No. 381, 2021), and registration was completed in the China Clinical Trial Registry (ChiCTR2100051812). Data reporting complied with the guidelines for reporting of randomized controlled trials (CONSORT). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants involved in the study.
Participants
The main observation in this study was the intubation time (the time from the beginning of the laryngoscope/stylet placement into the oral cavity to the appearance of 2 PETCO2 waveforms confirming successful tracheal intubation), which we derived from the preliminary experiment (n1 = n2 = 30 cases) that the intubation time for the VS group during single lumen endotracheal intubation was 37.4 ± 5.888 s, and that for the VL group was 40.533 ± 4.092 s. We set α = 0.05, β = 0.05, two-sided test, the sample size of the two groups was equal, and the means of the two independent samples were compared, and using the statistical software PASS 11.0, it was calculated that 71 subjects were needed for each group, N1 = N2 = 71. Considering the 10% fallout rate, the final sample size of the groups was about 78 cases, and the total sample size was 156 cases. Randomization was carried out using the random number generator method. None of the patients or postoperative followers were aware of the trial grouping.
Recruitment
Cases that were excluded midway included excessive duration of the procedure, patients withdrawing consent before the procedure and slowing of heart rate during induction of intubation so using atropine to avoid adverse events. The inclusion and exclusion criteria were as follows, Inclusion criteria: (1) age 18–80 years old; (2) ASA: grade I-II; (3) elective surgery with proposed general anesthesia with transoral single lumen tracheal intubation, and the duration of the procedure was expected to be within two hours. Exclusion criteria: (1) patients with a definite history of difficult airway; (2) anticipated difficult airway (mouth opening < 3 cm; thyromental distance < 6 cm; head and neck mobility < 80°; Mallampati classification > II grade; BMI ≥ 30 kg/m2 and other factors suggesting a difficult airway); (3) patients with upper respiratory tract tumors, abscesses, foreign objects, or airway stenosis; (4) patients who could not communicate and the patient or his/her family members were unwilling to perform this test; (5) history of upper respiratory tract infection within two weeks and history of sore throat and hoarseness within one month; (6) history of ear, nose and throat, thyroid and cervical spine surgeries and related surgeries affecting postoperative observational indexes; and (7) primary cardiorespiratory disorders (e.g., asthma, pneumonia, and other oxygen saturation less than 95% of the patients).
Outcome indicators
The primary outcome was intubation time. Secondary outcomes included glottic exposure time, first success rate, hemodynamic indicators (patients’ blood pressure and heart rate at three minutes basal values after emotional stabilization in the operation room (T0), prior to intubation after induction (T1), immediately after intubation (T2), three minutes after intubation (T3), and five minutes after intubation (T4)), intubation-related complications including whether the tube was stained with blood after extubation, and the occurrence and grading of postoperative sore throat (PST) and postoperative hoarseness (PH) at one hour and 24 h postoperatively.
Research process
See Supplementary Material for details.
Data processing and analysis
SPSS 21.0 statistical software was applied for statistical analysis. All measurement data were first tested for normality, and data that met the normal distribution were expressed using the mean ± standard deviation and statistically analyzed using the two independent samples t-test. Data that did not meet the normal distribution were expressed using the median and interquartile range, and statistically analyzed using the Mann-Whitney rank-sum test. Comparisons of three or more groups of measurement data were analyzed by ANOVA. Post hoc pairwise comparisons of multiple measures were performed using the SNK test. Repeated measures data were analyzed using repeated measures ANOVA. Count data were expressed as rates and percentages using the chi-square test or Fisher’s exact probability method. A significance level of α = 0.05 two-sided was used for all tow-sided tests, with P < 0.05 indicating statistical significance.
Results
A total of 156 patients were screened into the randomized sequence according to the inclusion and exclusion criteria (Fig. 1), and ultimately a total of 148 patients were obtained with complete data results from October, 2021 to September, 2022. The data of VS (N1 = 75) and VL group (N2 = 73) were statistically analyzed. There were no statistical differences between the two groups in terms of demographics and airway condition, and they were comparable (Supplementary Table 2).
Main outcomes
The intubation time was 35 (11) seconds in the VS group and 41 (9) s in the VL group, and the intubation time was shorter in the VS group than in the VL group, and the difference between the two groups was statistically significant (P < 0.001).
Secondary outcomes
The time of glottic exposure was 10.59 ± 4.51 s in the VS group and 11.14 ± 4.12 s in the VL group, and the difference in the time of glottis exposure between the two groups was not statistically significant (P = 0.44). All patients in both groups successfully completed tracheal intubation. In the VS group, two patients were overdue in the first intubation attempt (more than one minute) due to secretion interference, and successfully intubated in the second attempt after suctioning. All patients in the VL group were successfully intubated for the first time, and two of these patients were intubated with assistance of external laryngeal pressure. The difference in the first success rate was not statistically significant between the two groups (P = 0.16).
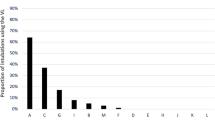
Meanwhile, for intubation time and glottic exposure time, we also performed subgroup analysis under different Cormork-Lehane classification (C-L classifications), and the detailed results are shown in Table 1. For different C-L classifications (except for Grade IIa), the intubation time of the VS group was smaller than that of the VL group, with a statistically significant difference. For the glottic exposure time, the difference between the two groups was statistically significant only in Grade III (P = 0.02), and there was no statistical difference in the rest of the classifications. Within-group comparisons revealed that in the VL group, the glottic exposure time (P = 0.001) and intubation time (P = 0.002) increased with higher C-L grading. In the VS group, the differences in glottic exposure time and intubation time were not statistically significant across different C-L grading.
The hemodynamics of the two groups of patients at different time points suggested that the visual stylet had less influence on the circulatory fluctuations of the patients (Table 2; Fig. 2). The SBP and MAP of the VS group at the moment of T2 were lower than those of the VL group (P = 0.02 and P < 0.01), and there was no statistically significant difference between the two groups for the rest of the moments and indicators.
We performed subgroup analyses of patients’ hemodynamic data at different time points based on some preoperative airway assessment (Supplementary Table 3). Grouped according to degree of mouth opening, we found that when mouth opening was 3–3.9 cm, both MAP and HR were lower in VS group than in the VL group at T2 (P = 0.04 and P = 0.03). HR in VS group at T3 was still lower than that in VL group (P = 0.02). When the mouth opening was ≥ 4 cm, the difference in hemodynamic data between the VS group and VL group was not statistically significant, which indicated that visual laryngoscopy has a greater effect on the circulation when the mouth opening is small. Grouping patients according to different thyromental distances, we found that VS group was more advantageous than VL group in patients with smaller thyromental distances. When the thyromental distance was 7–7.9 cm, the MAP of VS group was lower than that of VL group at T2 (P = 0.01). In the remaining three subgroups with a thyromental distance of ≥ 8 cm, there was no statistically significant difference in hemodynamic data comparisons between the two groups. Comparison of hemodynamics between the two groups of patients with different C-L grades revealed that the higher the C-L grade, the smaller the circulatory impact of the visual stylet compared with the visual laryngoscope. When the C-L grading was I, there was no statistically significant difference in hemodynamics data between the two groups. When the C-L classification was IIa, MAP and HR were lower in VS group than in the VL group at T2 (P = 0.04 and P = 0.03, respectively), and SBP and HR were lower in VS group than in the VL group at T3 (P = 0.04 and P = 0.02, respectively). When the two groups of patients were compared within groups separately, the higher the C-L grading, the more dramatic the circulatory fluctuations of the two groups of patients, such as VS group at the moment of T2, the MAP of the patients with C-L grading I was lower than the MAP of the patients with C-L grading IIb (P < 0.01). VL group in the intra-group comparisons of the patients in the different C-L grading, although the difference was not statistically significant, it still was trend of higher heart rate and blood pressure after intubation as C-L grading increased (Supplementary Table 4).
For intubation-related complications (Table 3), the incidence of blood staining of the tracheal tube was higher in VL group compared to VS group, with a statistical difference between the two groups (P = 0.03). There was no statistical difference in PST and PH between the two groups at one hour and 24 h postoperatively, and the patients in the two groups with PST and PH recovered within 48 h postoperatively. There were no anesthesia adverse events such as paralysis of the vocal cord or dislocation of cricoarytenoid joints. Both intubation tools were clinically safe to use.
As this trial was mostly short surgeries with more laparoscopic surgeries, and previous studies suggested that the incidence of PST and PH was higher in laparoscopic surgeries. We counted the incidence of PST and PH in these patients, and the differences in the general information and airway assessment between the two groups were not statistically significant, so they were comparable. The postoperative one hour and 24 h PST and PH of the two groups is shown in Supplementary Table 5, the incidence of postoperative one hour PH in VS group was lower than that in VL group (46.48% vs. 63.23%, P = 0.047), and the rest of the differences were not statistically significant. At the same time, we conducted a within-group comparison of PST and PH between the two groups according to different thyromental distances. The within-group comparison of VS group at different thyromental distances revealed (Supplementary Table 6) that the incidence of postoperative one hour PST was lower in the thyromental distance 8–8.9 cm group than in the 7–7.9 cm (0% vs. 20%, P < 0.05), and lower than in the > 9 cm group (0% vs. 20.69%, P < 0.01). The incidence of PH was higher in the thyromental distance > 9 cm group than in the 8–8.9 cm group (58.62% vs. 29.0%, P < 0.05). In VL group, there was no statistically significant difference in the incidence of one hour PST and PH at different thyromental distances.
Discussion
Our study found that the intubation time in VS group was lower than that in VL group, and there was no statistically significant difference between the two groups in terms of first success rate and duration of glottic exposure. Intubation time is often an important indicator of the usefulness of clinical intubation tools. The airway is open during intubation, and the longer the intubation time, the higher the risk of aspiration, which is especially critical in emergency and obstetric patients10,11. However, for non-emergency patients, the clinical significance of a significantly reduced intubation time may need to be explored by investigating complications such as hypoxemia. Since there was no significant difference in the duration of glottic exposure between the two intubation tools, it was hypothesized that the reduction in intubation time was due to the fact that when intubating with a visual stylet, the stylet could enter the glottis in a smooth manner after exposing the vocal cord, and then the tracheal tube was pushed directly into the airway, which reduced the time spent on delivering the tracheal tube from the oral cavity to the glottis, resulting in a more consistent intubation, and thus a shorter intubation time.
In this study, it was found that when the patient’s C-L classification was higher, the time of glottic exposure and intubation in VS group tended to be significantly lower than that in VL group. Because C-L classification is one of the indicators for assessing the degree of obstruction in the hypopharyngeal cavity and the relationship between the epiglottis and the vocal cord, patients with high C-L classification often need to adjust the position of the epiglottis several times to find the most appropriate angle of exposure when intubating with the visual laryngoscope, so the time for exposing the glottis was prolonged. However, visual stylet can bypass the epiglottis from the piriform sinus using the esophageal withdrawal method, making it less dependent on patient anatomy while still providing adequate exposure of the glottis. Therefore, visual stylet may be more suitable as a routine intubation tool, as it could offer an advantage over the visual laryngoscope in unanticipated difficult airways12,13.
During tracheal intubation, the stress response comes from mechanical stimulation of the vocal cord and airway. This activates the sympathetic-adrenomedullary and renin-angiotensin system, which causes a large release of catecholamine transmitters and transient, but noticeable, hemodynamics fluctuations14,15. In our study, we found that SBP and MAP at the T2 were lower in VS group than in VL group, which may be beneficial for certain patients who need to avoid dramatic hemodynamic fluctuations16. When performing subgroup analyses, we found that the hemodynamic differences between the two groups were more pronounced when the mouth opening was smaller, the thyromental distance was smaller, and the C-L grading was higher. This may be related to the fact that the visual laryngoscope uses more force for better exposure of the glottis and pharyngeal view in more challenging airway intubation, which laterally confirms the advantages of disposable malleable visual stylet over visual laryngoscopes in cases of relatively difficult airway intubation.
Intubation-related complications such as PST and PH are primarily due to mechanical stimulation during intubation and prolonged compression of the pharyngeal mucosa by the cuff and tube. This can lead to local detachment of the mucosal epithelium, mucosal oedema, and clinical manifestations including tube-related bleeding, sore throat and hoarseness. In this study, in order to avoid the influence of cuff pressure on the outcomes, the cuff were pressure-measured with a VBM manometer after successful intubation. In our study, we found that although there was no statistically significant difference in the incidence of PH between VS group and VL group, the difference was statistically significant in patients undergoing laparoscopic surgery. This difference could be attributed to the establishment of the pneumoperitoneum and the head-down-foot-up position, which can exacerbate mucosal edema and amplify patients’ perception of hoarseness and sore throat16. Our study suggests that the rate of blood staining on the tracheal tube after extubation in VS group was lower than that in VL group. This may be due to the real-time visualization capabilities of the visual stylet, which allows for smoother entry into the mouth without causing significant trauma to the lips, teeth, and tongue. Moreover, it facilitates observation of the catheter’s position relative to the vocal cords during intubation, resulting in less overall damage17,18.
Overall, the visual stylet for tracheal intubation, compared to the visual laryngoscope, demonstrates shorter intubation times, less hemodynamic fluctuation. For patients with limited mouth opening, shorter thyromental distance, or higher C-L grades, the visual stylet may potentially be a better choice compared to video laryngoscopy for tracheal intubation. However, whether visual stylet intubation can provide significant clinical benefits for non-emergency patients remains worthy of further investigation.
Our study also has other limitations. Firstly, some subgroups in our study’s subgroup analyses may have insufficient sample sizes, and future research will need to further expand the sample size for validation. Additionally, for the assessment of postoperative sore throat, future studies will need to strictly control the use of postoperative analgesic regimens to avoid interference from analgesic medications on the severity of sore throat pain. Finally, all patients were from the same center, which may introduce selection bias.
Data availability
All data are available upon request from the corresponding author.
References
Driver, B. E. et al. Effect of use of a Bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: A randomized clinical trial. Jama 319, 2179–2189. https://doi.org/10.1001/jama.2018.6496 (2018).
Klabusayová, E. et al. Videolaryngoscopy vs. Direct laryngoscopy for elective airway management in paediatric anaesthesia: A prospective randomised controlled trial. Eur. J. Anaesthesiol. 38, 1187–1193. https://doi.org/10.1097/eja.0000000000001595 (2021).
Apfelbaum, J. L. et al. American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 136, 31–81, (2022). https://doi.org/10.1097/aln.0000000000004002 (2022).
Rosenstock, C. V. et al. Awake fiberoptic or awake video laryngoscopic tracheal intubation in patients with anticipated difficult airway management: A randomized clinical trial. Anesthesiology 116, 1210–1216. https://doi.org/10.1097/ALN.0b013e318254d085 (2012).
Aziz, M. F. et al. First-Attempt intubation success of video laryngoscopy in patients with anticipated difficult direct laryngoscopy: A multicenter randomized controlled trial comparing the C-MAC D-Blade versus the glidescope in a mixed provider and diverse patient population. Anesth. Analg. 122, 740–750. https://doi.org/10.1213/ane.0000000000001084 (2016).
McCoy, E. P., Mirakhur, R. K. & McCloskey, B. V. A comparison of the stress response to laryngoscopy. The macintosh versus the McCoy blade. Anaesthesia 50, 943–946. https://doi.org/10.1111/j.1365-2044.1995.tb05924.x (1995).
Seo, K. H. et al. Comparison of C-MAC D-blade videolaryngoscope and McCoy laryngoscope efficacy for nasotracheal intubation in simulated cervical spinal injury: a prospective randomized comparative study. BMC Anesthesiol. 20, 114. https://doi.org/10.1186/s12871-020-01021-x (2020).
Nowakowski, M., Williams, S., Gallant, J., Ruel, M. & Robitaille, A. Predictors of difficult intubation with the Bonfils rigid fiberscope. Anesth. Analg. 122, 1901–1906. https://doi.org/10.1213/ane.0000000000001258 (2016).
Park, S. O. et al. Efficacy of the disposcope endoscope, a new video laryngoscope, for endotracheal intubation in patients with cervical spine immobilisation by semirigid neck collar: comparison with the macintosh laryngoscope using a simulation study on a manikin. Emerg. Med. J. 30, 270–274. https://doi.org/10.1136/emermed-2011-200899 (2013).
Shaji, I. M. et al. Efficacy of Metoclopramide for prevention of gastric regurgitation during endotracheal intubation in the emergency department: A randomized controlled trial. Int. J. Crit. Illn. Inj. Sci. 13, 92–96. https://doi.org/10.4103/ijciis.ijciis_80_22 (2023).
Arzola, C., Cubillos, J., Perlas, A., Downey, K. & Carvalho, J. C. Interrater reliability of qualitative ultrasound assessment of gastric content in the third trimester of pregnancy. Br. J. Anaesth. 113, 1018–1023. https://doi.org/10.1093/bja/aeu257 (2014).
Mahrous, R. S. S. & Ahmed, A. M. M. The Shikani optical stylet as an alternative to awake fiberoptic intubation in patients at risk of secondary cervical spine injury: A randomized controlled trial. J. Neurosurg. Anesthesiol. 30, 354–358. https://doi.org/10.1097/ana.0000000000000454 (2018).
Cheng, T. et al. Shikani optical stylet for awake nasal intubation in patients undergoing head and neck surgery. Laryngoscope 131, 319–325. https://doi.org/10.1002/lary.28763 (2021).
El-Shmaa, N. S. & El-Baradey, G. F. The efficacy of labetalol vs Dexmedetomidine for Attenuation of hemodynamic stress response to laryngoscopy and endotracheal intubation. J. Clin. Anesth. 31, 267–273. https://doi.org/10.1016/j.jclinane.2016.01.037 (2016).
Sivilotti, M., Ducharme, J. & Randomized Double-Blind study on sedatives and hemodynamics during Rapid-Sequence intubation in the emergency department: The SHRED study. Ann. Emerg. Med. 31, 313–324. https://doi.org/10.1016/s0196-0644(98)70341-5 (1998).
Siddiqui, N., Katznelson, R. & Friedman, Z. Heart rate/blood pressure response and airway morbidity following tracheal intubation with direct laryngoscopy, glidescope and trachlight: A randomized control trial. Eur. J. Anaesthesiol. 26, 740–745. https://doi.org/10.1097/EJA.0b013e32832b138d (2009).
Chen, P. T. et al. A randomised trial comparing real-time double-lumen endobronchial tube placement with the Disposcope(®) with conventional blind placement. Anaesthesia 72, 1097–1106. https://doi.org/10.1111/anae.13984 (2017).
Yu, J., Hu, R., Wu, L., Sun, P. & Zhang, Z. A comparison between the disposcope endoscope and fibreoptic bronchoscope for nasotracheal intubation: A randomized controlled trial. BMC Anesthesiol. 19, 163. https://doi.org/10.1186/s12871-019-0834-3 (2019).
Funding
This work is supported by the Science and Technology Plan Project of Sichuan Province, China (2023YFS0137), Sichuan Provincial People’s Hospital Youth Talent Fund (2023QN13) and Sichuan Provincial People’s Hospital Lateral Fund (2021HX042).
Author information
Authors and Affiliations
Contributions
CHM, GJQ and LQ were responsible for the study conceptualization and design, GJQ, ZYQ, MSK, LYQ, CL and YY recruited participants and collected the data, CHM and GJQ processed and analyzed the data and prepared the figures, CHM, GJQ and LQ wrote the manuscript, HH and LP supervised the project, all authors read and approved the final manuscript, offering critical feedback.
Corresponding authors
Ethics declarations
Competing interest
The authors declare no competing interests. Each participant obtained his or her own informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Haoming Chen, Jiaqi Gan and Qian Liu have equally contributed to this work as first author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, H., Gan, J., Liu, Q. et al. A randomized controlled trail comparing the visual stylet and visual laryngoscope for transoral single lumen tracheal intubation. Sci Rep 15, 10733 (2025). https://doi.org/10.1038/s41598-025-95298-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95298-y