Abstract
The Mediterranean diet (Med-Diet) is widely recognized for its protective effect in cardiovascular diseases (CVDs), less is known about the associations between health and adherence to the Prime Diet Quality Score (PDQS). This study investigates the relationship between adherence to the Med-Diet and PDQS with the risk of premature coronary artery disease (PCAD) in an Iranian population. A total of 3287 participants were included in this multicenter case-control study across various ethnic groups in Iran, categorized into PCAD cases (n = 2106) and controls (n = 1181). PCAD cases were defined as individuals with at least one coronary artery exhibiting ≥ 75% stenosis or a left main coronary artery with ≥ 50% stenosis, while controls had normal coronary arteries. Dietary intake was assessed using a semi-quantitative food frequency questionnaire (FFQ), previously validated for accuracy in the Iranian population Adherence to the Med-Diet was assessed using a standardized scoring system, awarding one point for higher consumption of beneficial food groups (such as vegetables, whole grains, legumes, fish, nuts, and a high monounsaturated-to-saturated fat ratio) and one point for lower consumption of less favorable foods (such as red and processed meats). The total score ranged from 0 to 9, with higher scores indicating greater adherence to the Med-Diet. The PDQS, a dietary quality index, evaluated adherence across 14 healthy and 7 unhealthy food groups, with higher scores reflecting better diet quality. Logistic regression models were employed to examine the association between dietary scores and PCAD risk. Participants with higher adherence to both the Med-Diet and PDQS had significantly lower odds of PCAD (OR = 0.30, 95% CI: 0.22, 0.40; P for trend < 0.001 for PDQS), with a stronger association observed for the Med-Diet (OR = 0.08, 95% CI: 0.06, 0.10; P for trend < 0.001). Additionally, higher adherence to the Med-Diet (OR = 0.04, 95% CI 0.03, 0.05) and PDQS (OR = 0.21, 95% CI: 0.17, 0.26) was inversely associated with PCAD severity in the fully adjusted model. This study showed a protective association of the Med-Diet and PDQS with reduced risk of PCAD in the Iranian population.
Similar content being viewed by others
Introduction
Worldwide, CVDs remain a leading cause of mortality, with deaths projected to rise to approximately 23.6 million by 2030. Low- and middle-income countries are experiencing a disproportionate increase in CVDs prevalence compared to high-income nations1. In Iran, data reveal a notably high prevalence of CVDs, with some studies reporting rates above 30%. These estimates are derived from population-based studies that use diagnostic criteria such as coronary angiography, which provides direct imaging of coronary artery stenosis. In our study, PCAD was defined by coronary angiography results, with cases identified as individuals with at least one coronary artery exhibiting ≥ 75% stenosis or a left main coronary artery with ≥ 50% stenosis2,3.
PCAD leads to significant morbidity, with approximately 50% of affected patients developing coronary atherosclerosis within a decade4. It also contributes to early mortality, with about 20% of PCAD patients experiencing premature death5. Generally, PCAD presents initially in men under 45 and women under 55, though age ranges can vary across studies. This condition results from complex genetic and environmental interactions6,7,8,9. More than 80% of individuals with PCAD have at least one modifiable cardiovascular risk factor, such as diabetes, hypertension, physical inactivity, excess body weight, psychosocial stress, smoking, or dyslipidemia10,11,12,13. Many of these risk factors are influenced by dietary habits14.
Med-Diet has been widely studied for its cardiovascular benefits and is recognized as a cardioprotective dietary pattern15. The Med-Diet emphasizes plant-based foods, whole grains, legumes, and healthy fats, particularly olive oil, while encouraging moderate fish and poultry intake and limiting red and processed meats. Numerous studies associate adherence to the Med-Diet with reduced risks of various chronic diseases16,17. However, adapting the Med-Diet for non-Mediterranean populations can be challenging due to differences in food availability and cultural preferences18,19. To address these challenges, food-based diet quality indices, such as the PDQS, offer a flexible framework that does not rely on complex nutrient analysis tools20,21,22,23. The PDQS evaluates adherence to dietary recommendations by scoring healthy and unhealthy food group intake24,25.
Adherence to the PDQS reflects how closely individuals follow a health-promoting dietary pattern designed to support cardiovascular and overall health. This score assesses diet quality by emphasizing foods with recognized health benefits, such as dark green leafy vegetables, whole grains, and fish, while reducing points for items like processed meats and sugary beverages26. As a dietary index, PDQS aims to capture the overall quality of diet patterns linked with reduced risks for chronic diseases, including CVD and certain metabolic conditions. It simultaneously discourages the consumption of less healthful foods, including processed meats, refined grains, sugar-sweetened beverages, and sweets. Higher PDQS scores indicate greater adherence to this balanced, health-oriented dietary pattern. This makes it particularly suitable for population studies seeking a pragmatic dietary assessment tool that is culturally adaptable and straightforward to implement25,26,27.
While some Med-Diet scoring tools incorporate a saturated-to-unsaturated fatty acid ratio, one of the most commonly used methods, as described by Martínez-González et al.28, does not require this calculation. This simplifies its application in both clinical and large-scale epidemiological studies. Calculating precise nutrient ratios requires detailed dietary data and specialized software for nutrient analysis, which may not be feasible in low-resource environments. In contrast, food-based scoring tools, such as the simplified 14-point Med-Diet scale or PDQS, offer more accessible alternatives for assessing adherence to healthy dietary patterns without needing complex nutrient breakdowns.
PDQS is a possible clinical tool for assessing diet health globally without elaborate dietary assessments20. The PDQS has been associated with lower risks of coronary heart disease and heart failure with reduced ejection fraction (HFrEF) in high-income populations, but there is limited research on its association with PCAD in low-income countries20,24. Fung et al., who first introduced the PDQS, reported that adherence to a healthful dietary pattern, as indicated by higher PDQS scores, is associated with a significantly lower risk of ischemic heart disease (IHD) in high-income countries20. Also, a recent study reported that higher scores of PDQS were associated with a lower risk of HFrEF24. Both studies recruited health professional participants in the United States (US), a high-income country. However, no studies have investigated the association between PDQS and PCAD in low-income countries.
In this study, we used both the Mediterranean dietary pattern scoring tool and the PDQS to assess diet quality and its association with PCAD. The Med-Diet scoring tool was chosen for its well-established associations with cardiovascular health and its ability to capture adherence to a dietary pattern linked with reduced risks of chronic diseases, particularly in Mediterranean populations. However, the Med-Diet scoring tool may have limitations in non-Mediterranean settings due to regional dietary differences. To address this, we also incorporated the PDQS, a flexible, food-based index that evaluates diet quality based on food group intake, making it adaptable to diverse cultural and dietary contexts. By using both the Med-Diet scoring tool and PDQS, our study provides a comprehensive assessment of dietary quality and its potential impact on PCAD risk, allowing for comparisons across different diet quality measures.
Therefore, this study aimed to explore the relationship between adherence to the Med-Diet and PDQS with the risk of PCAD, examining each dietary index independently.
Materials and methods
Study design and population
This study utilized data from the Iran Premature Coronary Artery Disease (IPAD) multicenter case-control study. Participants from various ethnic groups in 15 Iranian cities were recruited and underwent coronary angiography. Inclusion criteria included candidates for coronary angiography, aged ≤ 65 for women and ≤ 55 for men, who belonged to one of the studied ethnicities. Patients with at least one coronary artery with ≥ 75% occlusion or a left main coronary artery with ≥ 50% occlusion were classified as having PCAD and designated as the case group. In contrast, individuals with normal coronary arteries formed the control group. PCAD severity was classified based on the number of stenotic vessels (none, one, or two). Exclusion criteria included any history of documented PCAD, such as coronary artery bypass surgery (CABG) or percutaneous coronary intervention (PCI)29. In total, 3,287 individuals participated in this study. Further methodological details are available in previous publications29. All participants provided written informed consent, and the study was approved by the Ethics Committee of Isfahan University of Medical Sciences (IR.MUI.REC.1396.2.055).
Data collection
Main cardiac catheterization centers were selected based on the dominant ethnic group in each region. These centers enrolled participants who met the study criteria. Trained interviewers collected data on participant characteristics (e.g., age, gender, ethnicity, religion, education, marital status) and lifestyle habits (e.g., smoking, dietary intake, physical activity) through validated questionnaires. Physical activity was assessed using the International Physical Activity Questionnaire (IPAQ)30. Height was measured using a wall-mounted stadiometer (sensitivity of 0.1 cm), and weight was measured using a Seca 877 scale (sensitivity of 0.1 kg) with participants barefoot and in minimal clothing. Body mass index (BMI) was calculated as weight (kg) divided by height (m2). Waist circumference (WC) was measured to the nearest 0.1 cm at the midpoint between the lowest rib and the iliac crest31. Blood pressure was measured twice using a digital sphygmomanometer (BC 08, Beurer, Germany) after participants rested for at least 5 min; the average of these two measurements was recorded.
Biochemical measurements
Fasting blood samples were collected after a 12-hour fasting period to assess fasting serum glucose, triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) using enzymatic methods (Pars Azmoon, Tehran, Iran).
Dietary assessment
Dietary intake over the previous year was assessed using a semi-quantitative food frequency questionnaire (FFQ) comprising 110 items32. Participants reported their average consumption frequency for each item using nine response options, ranging from “never/almost never” to “six or more times per day32. Daily intake for each food item (in grams) was calculated by multiplying the frequency by the portion size32. Dietary intakes were analyzed using Nutritionist IV software, version X (Axxya Systems, Redmond, WA, USA; https://www.nutritionistpro.com/).
Med-Diet score was calculated following Trichopoulou et al.’s methodology33. Points were awarded if participants met the median intake criteria for vegetables, whole grains, fish, legumes, nuts, and the monounsaturated-to-saturated fatty acid ratio. Additionally, one point was awarded if meat (poultry, red meat, processed meats) and dairy intake fell below the median. The overall Med-Diet score ranged from 0 to 9 points, with higher scores indicating greater adherence to this dietary pattern.
The PDQS was calculated based on intake frequencies for specific food groups, scoring higher for increased consumption of health-promoting foods (e.g., leafy greens, whole grains) and lower for more frequent intake of foods linked with adverse health outcomes (e.g., refined grains, processed meats). This scoring system provides a comprehensive overview of diet quality by evaluating food group consumption rather than individual nutrients, offering a simplified yet robust assessment of dietary adherence to healthful patterns25. The PDQS is a validated food-based DQI20. It consists of 14 healthy food group components (e.g., dark green leafy vegetables, cruciferous vegetables, carrots, other vegetables, citrus fruits, other fruits, legumes, nuts, poultry, fish, eggs, whole grains, low-fat dairy, and liquid vegetable oils) and seven unhealthy food group (e.g., red meat, processed meats, potatoes, refined grains and baked goods, sugar-sweetened beverages, fried foods away from home, and sweets and ice cream)20. In the original validation study, the PDQS was shown to have an inverse association with several diseases, including coronary heart disease and heart failure with reduced ejection fraction (HFrEF), when higher scores indicated greater adherence to a healthful dietary pattern34. In contrast, the unhealthy food group was positively associated with disease risks and decreased PDQS scores. The PDQS score was calculated by the intake frequency of every food that was in the healthy/unhealthy group. For example, in the healthy group, based on the number of servings per week, 0, 1, and 2 points were assigned for intake of 0–1, 2–3, and ≥ 4 servings, respectively. However, grading was the opposite for the items in the unhealthy group: 2, 1, and 0 points were assigned for intake of 0–1, 2–3, and ≥ 4 servings, respectively. After summing over the component scores, the PDQS ranged from 0 to 42 points, with a higher PDQS score indicating a healthier diet.
Statistical analysis
The Med-diet score and PDQS were stratified into quartiles. Continuous variables were presented as mean ± standard deviations (SD), while the categorical variables were presented as numbers (percentages). In order to compare the mean quantitative variables between the quartiles of PDQS and the Med-Diet score in both the PCAD and control groups, a one-way analysis of variance (ANOVA) was utilized, and for the categorical variables among different groups, the chi-square test was utilized.
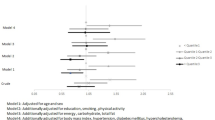
The associations between dietary scores (PDQS and Med-Diet) and PCAD were examined using logistic regression models. We categorized each variable as follows: age (in years), sex (male/female), ethnicity (specific ethnic groups in the study), energy intake (kcal/day), education (categorized by level attained), smoking status (yes/no), marital status (single/married), alcohol consumption (yes/no), physical activity (low/moderate/high based on IPAQ classification), BMI (kg/m²), and biochemical measures including HDL-C, LDL-C, total cholesterol, triglycerides, and fasting blood glucose. Additionally, aspirin use (yes/no) was included as it may influence cardiovascular risk factors.
Four models were applied to evaluate the robustness of associations. We included an unadjusted model to observe crude associations and a fully adjusted model that considers multiple demographic, lifestyle, and biochemical factors identified as PCAD risk factors in the literature. The other two models serve to illustrate stepwise adjustments: one minimally adjusted for age, sex, ethnicity, and energy intake, and another adjusted for additional lifestyle factors (education, smoking, marital status, alcohol consumption, and physical activity). This sequence highlights how various adjustments impact the associations between dietary scores and PCAD risk.
To assess trends across the quartiles of dietary scores, we assigned the median value of each quartile as a continuous variable and included it in the logistic regression models to calculate p-trend values. This analysis allowed us to evaluate whether the risk of PCAD changes progressively across increasing adherence levels to each dietary pattern. Statistical analysis was conducted using SPSS for Windows, version 23 (IBM Corp., Armonk, NY, USA; https://www.ibm.com/analytics/spss-statistics-software).
Results
A total of 3287 participants (2,106 cases and 1,181 control) were included, of which 44.7% were female, and the mean ± SD age was 53.74 ± 7.76. The characteristics of the study population at baseline in the PDQS and Med-Diet quartiles can be found in Table 1. In both PDQS and Med-Diet quartiles, participants with higher adherence were generally younger, had higher education levels, and were more likely to use aspirin. In the PDQS quartiles, individuals in the highest quartile were more likely to be smokers, engage in physical activity, and had lower systolic and diastolic blood pressure, as well as reduced waist circumference. Additionally, a higher Med-Diet score was associated with lower fasting blood glucose levels. Details of these associations are provided in Table 1.
A higher Med-Diet score, but not PDQS, was significantly associated with lower FBG (P < 0.001). The mean of BMI across the quartiles of the PDQS and age across the quartiles of the Med-Diet was significantly different (P = 0.011 and P = 0.014). No differences were reported in terms of marital status, alcohol drinking, TC, TG, and LDL-C and HDL-C across the quartiles of both PDQS and Med-Diet groups.
The dietary intakes of the study participants in the PDQS and Med-Diet quartiles are demonstrated in Table 2. Higher adherence to both PDQS and Med-Diet scores was significantly associated with higher intake of energy (Kcal/day), protein (% of energy), low-fat dairy products, fiber, vegetables, fruits, legumes, whole grains, fishes and shrimps, and nuts and seed (P < 0.001). Also, higher PDQS and Med-Diet scores were significantly associated with lower intake of high-fat dairy products, refined grains, red and processed meats, processed meats, and fast foods (P < 0.001). Higher Med-Diet scores, but not PDQS, were significantly associated with higher total fat intake (P < 0.001).
Multivariable-adjusted ORs (95% CI) for PCAD across the PDQS and Med-Diet quartiles are illustrated in Table 3. In the fully adjusted models, higher adherence to the Med-Diet and the PDQS was associated with a substantially lower risk of PCAD. Participants in the highest quartile of Med-Diet adherence had approximately 92% lower odds of PCAD compared to those in the lowest quartile (OR = 0.08, 95% CI: 0.06, 0.1; P for trend < 0.001). Similarly, participants in the highest PDQS quartile had 70% lower odds of PCAD compared to those in the lowest quartile (OR = 0.30, 95% CI: 0.22, 0.40; P for trend < 0.001).
Table 4 shows ORs (95% CI) for PCAD severity across the PDQS and Med-Diet quartiles. In the fully adjusted model, participants in the highest quartile of PDQS had a 79% lower risk of severe PCAD compared to those in the lowest quartile (OR = 0.21, 95% CI: 0.17, 0.26; P for trend < 0.001). For the Med-Diet, the reduction in PCAD severity was even more substantial, with participants in the highest quartile showing a 96% lower risk compared to those in the lowest quartile (OR = 0.04, 95% CI: 0.0.3, 0.05; P for trend < 0.001).
Discussion
Cardiovascular diseases continue to pose a significant public health challenge globally, with escalating rates projected particularly in low- and middle-income countries35. Our study aimed to explore the relationship between adherence to the Med-Diet and PDQS with the risk of PCAD, examining each dietary index independently among Iranians, considering the rich ethnic diversity within the population. The results of this study showed that participants in the highest quartiles of PDQS and Med-Diet adherence had 70% and 92% lower odds of PCAD, respectively. Also, we found an inverse correlation between PDQS and Med-Diet scores with PCAD severity. Despite its effectiveness, the Med-Diet can be challenging to adopt in low-income countries due to the cost of certain foods and the need for detailed nutrient tracking, such as the specific ratios of saturated to unsaturated fats. These requirements make the Med-Diet less accessible and practical for widespread use in some populations.
The comparison between the Med-Diet and the PDQS in our study was driven by the recognition of the Med-Diet as one of several dietary patterns widely regarded for supporting heart health36. Although the Med-Diet scoring system incorporates a saturated-to-unsaturated fatty acid ratio, applying this measure can be challenging in routine clinical or large-scale epidemiological settings. This difficulty arises because calculating precise nutrient ratios often requires detailed dietary intake data and specialized nutritional analysis software, which may not be readily available, especially in low-resource settings. Alternatively, Med-Diet scoring tools based on food items rather than nutrient ratios, such as a simplified 14-point scale, offer a more feasible approach for assessing adherence to this dietary pattern37. In contrast, the PDQS offers a simpler and more accessible alternative for assessing diet quality. Its broader applicability and ease of use make it a valuable tool, especially in resource-constrained settings where the adoption of complex dietary patterns like the Med-Diet may be impractical38. Our findings highlight the effectiveness of both dietary indicators in reducing the risk of heart diseases, with the Med-Diet showing greater efficacy but the PDQS also showing substantial effectiveness.
It is important to note that while some Med-Diet scoring tools incorporate the calculation of saturated-to-unsaturated fat ratios, this is a limitation of the specific scoring tool chosen rather than a fundamental characteristic of all Med-Diet scoring systems. For instance, the validated 14-point Med-Diet scoring tool developed by Martínez-González et al.28 does not require nutrient composition analysis, making it more feasible for large-scale epidemiological studies.
Several studies have found an inverse correlation between PDQS and Med-Diet and odds of various chronic diseases such as coronary heart disease20, gestational diabetes mellitus39, short telomere length40 and cardiovascular risk factors41. However, to our knowledge, no study has investigated the association of PDQS with odds of PCAD.
Complex conditions arise from a combination of inherited susceptibility and various cardiometabolic risk factors contribute to the onset of PCAD. Dietary modifications through affecting cardiometabolic risk factors can modulate progression and trajectory of the disease8,41,42,43,44. Prior research underscored the importance of prevention during the initial stages of PCAD development45,46. In a case-control investigation, amongst diverse risk factors of myocardial infarction (MI) in young adults, dietary behaviors emerged as the most prominent factor47. Several meta-analysis studies have shown that adherence to the Med-Diet was inversely correlated with CVD and coronary heart disease risk48. Based on 29 observational studies, Rosato et al. concluded that the Med-Diet reduced the risk of CVD approximately 20–25%49.
The Med-Diet has gained substantial attention for its positive effects on cardiometabolic health and cardiovascular risk factors50. Higher adherence to the Med-Diet is inversely associated with obesity, as a main risk factors for PCAD51,52, lower levels of cholesterol, LDL-C, TG, and blood pressure and higher insulin sensitivity50,53,54,−55. Furthermore, higher amounts of olive oil in the Med-Diet, as a rich source of MUFA and polyphenols, contributes to its anti-inflammatory and antioxidant properties, lipid lowering and improving endothelial function, which altogether reduce cardiovascular risk56,57. The Med-Diet emphasizes fruits, vegetables, whole grains, legumes, and unsaturated fats, all associated with beneficial effects on cardiovascular health58. Fruits and vegetables contribute antioxidants and fiber, while whole grains provide complex carbohydrates and fiber, both impacting lipid profiles and glycemic control59. Legumes offer plant-based protein and fiber, further modulating cholesterol and blood sugar levels60,61. On the other hand, the Med-Diet contains small amounts of SFAs and trans-fatty acids (TFAs). Norouzian et al. in a cross-sectional study among Iranianians observed that daily consumption of hydrogenated fats and milk, as the sources of SFAs and TFAs, were significantly higher in obstructive PCAD patients compared to non-obstructive or non-PCAD patients62. Higher levels of LDL-C, related to higher consumption of SFAs, is associated with higher production of oxidized LDL-C particles which are removed by macrophages, leading to the onset of atherosclerosis63.
In line with our findings, a prospective cohort study among 44,525 men found an inverse association between PDQS and risk of heart failure24. This aligns with prior research findings that have recognized the PDQS as a marker of dietary quality, showing inverse associations with various health outcomes such as PCAD64, pregnancy39 and birth complications65, uterine fibroids66, and overall mortality across diverse geographic populations67,68. PDQS lessens the workload associated with dietary evaluation for clinicians and patients. In a recent investigation involving American women, the PDQS diet screeners demonstrated comparable validity and ease of use across versions assessing short-term or usual dietary patterns69. In contrast to a comprehensive FFQ typically comprising over 100 inquiries, the PDQS screeners are comprised of 22 questions regarding intake frequency, and their administration does not necessitate specialized nutritional training. Crucially, the PDQS derived from these screeners exhibited associations with the consumption levels of essential nutrients and Healthy Eating Index (HEI 2015)69. Hence, the PDQS emerges as a clinically relevant tool for dietary assessment, with the capability to pinpoint PCAD risk.
Despite its well-documented benefits, adherence to the Med-Diet was relatively low in our study population, even in the highest quartile. This can be attributed to the fact that the study was conducted in an Iranian population, where traditional dietary patterns are more prevalent. Many of the key components of the Mediterranean diet are less commonly consumed in this population, which may have contributed to the lower scores observed. The Med-Diet scores in our study ranged from 0 to 4 in the lowest quartile to 5 to 11 in the highest quartile out of a maximum of 14 points. Given that the highest quartile scores ranged from 5 to 11, this suggests that while some participants adhered closely to the Med-Diet, others in this group still had relatively moderate adherence, potentially reflecting dietary differences in this population. However, if scores ranged from 10 to 14, it would suggest the tool effectively captures a healthful dietary pattern despite differences in traditional diets.
The present study has several strengths including large sample size, multi-centric design, comprehensive data collection and simultaneous evaluation of Med-Diet and PDQS which increases the accuracy of the obtained results. However, the present study had some limitations that should be considered. First, the case-control nature of the study limits the ability to infer causality and assess temporal relationships between dietary patterns and PCAD risk. Second, the reliance on retrospective data collection, including self-reported dietary intake and lifestyle habits, may be prone to recall bias and may not accurately reflect long-term dietary patterns. Third, despite adjustment for various confounders, residual confounding from unmeasured factors, such as socioeconomic status or medication use, cannot be entirely ruled out.
Conclusion
In conclusion, our study provides compelling evidence supporting the protective role of both the Med-Diet and the PDQS against the development of PCAD in a multi-centric case-control study conducted in Iran. Participants with higher adherence to either the Med-Diet or PDQS showed significantly lower odds of PCAD, with a particularly pronounced association observed for the Med-Diet. Future prospective studies are warranted to validate our findings and elucidate the underlying mechanisms by which dietary factors influence the pathogenesis of PCAD.
Data availability
The data and all supporting materials used in the preparation of this manuscript are freely available from the corresponding author at reasonable request.
References
Bowry, A. D., Lewey, J., Dugani, S. B. & Choudhry, N. K. The burden of cardiovascular disease in low-and middle-income countries: epidemiology and management. Can. J. Cardiol. 31, 1151–1159 (2015).
Trevino, K. M. & McConnell, T. R. Religiosity and religious coping in patients with cardiovascular disease: change over time and associations with illness adjustment. J. Relig. Health 53, 1907–1917 (2014).
Ebrahimi, M., Kazemi-Bajestani, S., Ghayour-Mobarhan, M. & Ferns, G. Coronary artery disease and its risk factors status in Iran: a review. Iran. Red Crescent Med. J. 13, 610 (2011).
Zeitouni, M. et al. Risk factor burden and long-term prognosis of patients with premature coronary artery disease. J. Am. Heart Assoc. 9, e017712 (2020).
Wilmot, K. A., O’Flaherty, M., Capewell, S., Ford, E. S. & Vaccarino, V. Coronary heart disease mortality declines in the united States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation 132, 997–1002 (2015).
Panwar, R. B. et al. Atherothrombotic risk factors & premature coronary heart disease in India: a case-control study. Indian J. Med. Res. 134, 26 (2011).
Virani, S. S. et al. Heart disease and stroke statistics—2020 update: a report from the American heart association. Circulation 141, e139–e596 (2020).
Mohammadifard, N. et al. The effect of ketogenic diet on shared risk factors of cardiovascular disease and cancer. Nutrients 14, 3499 (2022).
Hasanloei, M. A. V. et al. Effect of oral versus intramuscular vitamin D replacement on oxidative stress and outcomes in traumatic mechanical ventilated patients admitted to intensive care unit. Nutr. Clin. Pract. 35, 548–558 (2020).
Reibis, R. et al. Disparity in risk factor pattern in premature versus late-onset coronary artery disease: a survey of 15,381 patients. Vasc. Health Risk Manag. 473–481 (2012).
Pillay, A. & Naidoo, D. Atherosclerotic disease is the predominant aetiology of acute coronary syndrome in young adults. Cardiovasc. J. Afr. 29, 36–42 (2018).
Malakar, A. K. et al. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol. 234, 16812–16823 (2019).
Mannsverk, J. et al. Trends in modifiable risk factors are associated with declining incidence of hospitalized and nonhospitalized acute coronary heart disease in a population. Circulation 133, 74–81 (2016).
Engelfriet, P. et al. Food and vessels: the importance of a healthy diet to prevent cardiovascular disease. Eur. J. Prev. Cardiol. 17, 50–55 (2010).
Salas-Salvadó, J., Becerra-Tomás, N., García-Gavilán, J. F., Bullo, M. & Barrubes, L. Mediterranean diet and cardiovascular disease prevention: what do we know? Prog. Cardiovasc. Dis. 61, 62–67 (2018).
Dinu, M. et al. Effects of popular diets on anthropometric and cardiometabolic parameters: an umbrella review of meta-analyses of randomized controlled trials. Adv. Nutr. 11, 815–833 (2020).
USDA & U. (2015).
Bonaccio, M. et al. Low income is associated with poor adherence to a mediterranean diet and a higher prevalence of obesity: cross-sectional results from the Moli-sani study. BMJ Open 2, 1 (2012).
Obeid, C. A., Gubbels, J. S., Jaalouk, D., Kremers, S. P. & Oenema, A. Adherence to the mediterranean diet among adults in mediterranean countries: A systematic literature review. Eur. J. Nutr. 61, 3327–3344 (2022).
Fung, T. T., Isanaka, S., Hu, F. B. & Willett, W. C. International food group–based diet quality and risk of coronary heart disease in men and women. Am. J. Clin. Nutr. 107, 120–129 (2018).
Fanta, F. Developing and Validating Simple Indicators of Dietary Quality and Energy Intake of Infants and Young Children in Developing Countries: Summary of Findings from Analysis of 10 Data Sets (Academy for Educational Development, 2006).
Fung, T. T. et al. Food quality score and the risk of coronary artery disease: a prospective analysis in 3 cohorts. Am. J. Clin. Nutr. 104, 65–72 (2016).
Morshedzadeh, N. et al. The effects of flaxseed supplementation on metabolic syndrome parameters, insulin resistance and inflammation in ulcerative colitis patients: an open-labeled randomized controlled trial. Phytother. Res. 35, 3781–3791. https://doi.org/10.1002/ptr.7081 (2021).
Gu, X. et al. Dietary quality and risk of heart failure in men. Am. J. Clin. Nutr. 116, 378–385 (2022).
Cano-Ibáñez, N. et al. Association between the prime diet quality score and depressive symptoms in a mediterranean population with metabolic syndrome. Cross-sectional and 2-year follow-up assessment from PREDIMED-PLUS study. Br. J. Nutr. 128, 1170–1179 (2022).
Kronsteiner-Gicevic, S. et al. Validation of the rapid prime diet quality score screener (rPDQS), a brief dietary assessment tool with simple traffic light scoring. J. Acad. Nutr. Dietet. 123, 1541–1554. https://doi.org/10.1016/j.jand.2023.05.023 (2023).
Bakhtiary, M. et al. Effect of probiotic, prebiotic, and synbiotic supplementation on cardiometabolic and oxidative stress parameters in patients with chronic kidney disease: A systematic review and meta-analysis. Clin. Ther. 43, e71–e96. https://doi.org/10.1016/j.clinthera.2020.12.021 (2021).
Martínez-González, M. A. et al. A 14-item mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS ONE 7, e43134. https://doi.org/10.1371/journal.pone.0043134 (2012).
Zarepur, E. et al. Rationale, design, and preliminary results of the Iran-premature coronary artery disease study (I-PAD): A multi-center case-control study of different Iranian ethnicities. ARYA Atheroscler. 16, 295 (2020).
Moghaddam, M. B. et al. The Iranian version of international physical activity questionnaire (IPAQ) in Iran: content and construct validity, factor structure, internal consistency and stability. World Appl. Sci. J. 18, 1073–1080 (2012).
Organization, W. H. Measuring Obesity—Classification and Description of Anthropometric Data. Report on a WHO Consultation of the Epidemiology of Obesity. Warsaw 21–23 October 1987. Copenhagen: WHO, 1989. Nutrition Unit Document, EUR/ICP/NUT, Vol. 123 (1987).
Mohammadifard, N. et al. Validation of simplified tools for assessment of sodium intake in Iranian population: rationale, design and initial findings. Arch. Iran. Med. 19, 1 (2016).
Trichopoulou, A., Costacou, T., Bamia, C. & Trichopoulos, D. Adherence to a mediterranean diet and survival in a Greek population. N. Engl. J. Med. 348, 2599–2608 (2003).
Brennan, S. F. et al. Validity and reproducibility of the prime diet quality score (PDQS) against a four-day food diary in adults at risk of cardiovascular disease on the Island of Ireland. J. Nutr. Sci. 13, e29 (2024).
Yun, J. S. & Ko, S. H. Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes. Metabolism 123, 154838 (2021).
Martinez-Lacoba, R., Pardo-Garcia, I., Amo-Saus, E. & Escribano-Sotos, F. Mediterranean diet and health outcomes: a systematic meta-review. Eur. J. Pub. Health 28, 955–961 (2018).
Milano, A., Kabbaha, S. & Thorlund, K. Effects of the mediterranean diet versus low-fat diet on metabolic syndrome outcomes: A systematic review and meta-analysis of randomized controlled trials. Hum. Nutr. Metab. 30, 200175 (2022).
Kronsteiner-Gicevic, S. et al. Validation of the rapid prime diet quality score screener (rPDQS), a brief dietary assessment tool with simple traffic light scoring. J. Acad. Nutr. Dietet. 123, 1541–1554 (2023).
Gicevic, S. et al. Evaluating pre-pregnancy dietary diversity vs. dietary quality scores as predictors of gestational diabetes and hypertensive disorders of pregnancy. PLoS ONE 13, e0195103 (2018).
Ojeda-Rodríguez, A. et al. Association between diet quality indexes and the risk of short telomeres in an elderly population of the SUN project. Clin. Nutr. 39, 2487–2494 (2020).
Alvarez-Alvarez, I. et al. Adherence to a priori dietary indexes and baseline prevalence of cardiovascular risk factors in the PREDIMED-Plus randomised trial. Eur. J. Nutr. 59, 1219–1232 (2020).
Wang, H. et al. Pathogenesis of premature coronary artery disease: focus on risk factors and genetic variants. Genes Dis. 9, 370–380 (2022).
Poorzand, H. et al. Risk factors of premature coronary artery disease in Iran: A systematic review and meta-analysis. Eur. J. Clin. Investig. 49, e13124 (2019).
Rahimlu, M., Shab-Bidar, S. & Djafarian, K. Body mass index and all-cause mortality in chronic kidney disease: a dose–response meta-analysis of observational studies. J. Ren. Nutr. 27, 225–232 (2017).
Charakida, M., Deanfield, J. E. & Halcox, J. P. Childhood origins of arterial disease. Curr. Opin. Pediatr. 19, 538–545 (2007).
Collet, J. P. et al. Long-term evolution of premature coronary artery disease. J. Am. Coll. Cardiol. 74, 1868–1878 (2019).
Panagiotakos, D. B. et al. Background dietary habits are strongly associated with the development of myocardial infarction at young ages: A case–control study. Eur. E-J. Clin. Nutr. Metab. 3, e328–e334 (2008).
Becerra-Tomás, N. et al. Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit. Rev. Food Sci. Nutr. 60, 1207–1227. https://doi.org/10.1080/10408398.2019.1565281 (2020).
Rosato, V. et al. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur. J. Nutr. 58, 173–191 (2019).
Schwingshackl, L., Missbach, B., König, J. & Hoffmann, G. Adherence to a mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health. Nutr. 18, 1292–1299 (2015).
Khoja, A. et al. Risk factors for premature coronary artery disease (PCAD) in adults: a systematic review protocol. F1000Research 10, 1 (2021).
Beunza, J. J. et al. Adherence to the mediterranean diet, long-term weight change, and incident overweight or obesity: the Seguimiento Universidad de Navarra (SUN) cohort. Am. J. Clin. Nutr. 92, 1484–1493 (2010).
Tong, T. Y. et al. A combination of metabolites predicts adherence to the mediterranean diet pattern and its associations with insulin sensitivity and lipid homeostasis in the general population: the Fenland study, united Kingdom. J. Nutr. 150, 568–578 (2020).
Cowell, O. R. et al. Effects of a mediterranean diet on blood pressure: a systematic review and meta-analysis of randomized controlled trials and observational studies. J. Hypertens. 39, 729–739 (2021).
Sánchez-Sánchez, M. L. et al. Mediterranean diet and health: A systematic review of epidemiological studies and intervention trials. Maturitas 136, 25–37 (2020).
Gantenbein, K. V. & Kanaka-Gantenbein, C. Mediterranean diet as an antioxidant: the impact on metabolic health and overall wellbeing. Nutrients 13, 1951 (2021).
Morshedzadeh, N. et al. The effects of flaxseed supplementation on metabolic syndrome parameters, insulin resistance and inflammation in ulcerative colitis patients: an open-labeled randomized controlled trial. Phytother. Res. 35, 3781–3791 (2021).
Estruch, R. et al. Primary prevention of cardiovascular disease with a mediterranean diet. N. Engl. J. Med. 368, 1279–1290 (2013).
Martínez-González, M. A., Gea, A. & Ruiz-Canela, M. The mediterranean diet and cardiovascular health: A critical review. Circ. Res. 124, 779–798 (2019).
Angeles, J. G. C. et al. Legumes as functional food for cardiovascular disease. Appl. Sci. 11, 5475 (2021).
Rahimlou, M. et al. Effects of ginger supplementation on anthropometric, glycemic and metabolic parameters in subjects with metabolic syndrome: A randomized, double-blind, placebo-controlled study. J. Diabetes Metab. Disord. 18, 119–125. https://doi.org/10.1007/s40200-019-00397-z (2019).
Ostad, A. N. et al. Food intake pattern and cardiovascular risk factors in patients with premature coronary artery disease in Iran. J. Nutr. Food Secur. 1, 1 (2022).
Libby, P. Changing concepts of atherogenesis. J. Intern. Med. 247, 349–358 (2000).
Fung, T. T., Isanaka, S., Hu, F. B. & Willett, W. C. International food group-based diet quality and risk of coronary heart disease in men and women. Am. J. Clin. Nutr. 107, 120–129. https://doi.org/10.1093/ajcn/nqx015 (2018).
Madzorera, I. et al. Maternal dietary diversity and dietary quality scores in relation to adverse birth outcomes in Tanzanian women. Am. J. Clin. Nutr. 112, 695–706. https://doi.org/10.1093/ajcn/nqaa172 (2020).
Zhou, M., Zhai, Y., Wang, C., Liu, T. & Tian, S. Association of dietary diversity with uterine fibroids among urban premenopausal women in Shijiazhuang, China: A cross-sectional study. Asia Pac. J. Clin. Nutr. 29, 771–781. https://doi.org/10.6133/apjcn.202012_29(4).0012 (2020).
Gicevic, S., Tahirovic, E., Bromage, S. & Willett, W. Diet quality and all-cause mortality among US adults, estimated from National health and nutrition examination survey (NHANES), 2003–2008. Public. Health Nutr. 24, 2777–2787. https://doi.org/10.1017/s1368980021000859 (2021).
Morshedzadeh, N. et al. Association between adipokines levels with inflammatory bowel disease (IBD): systematic reviews. Dig. Dis. Sci. 62, 3280–3286 (2017).
Kronsteiner-Gicevic, S., Mou, Y., Bromage, S., Fung, T. T. & Willett, W. Development of a diet quality screener for global use: evaluation in a sample of US women. J. Acad. Nutr. Dietetics 121, 854–871 (2021).
Acknowledgements
The authors greatly appreciate the help of all staff in different study centers with their assistance in data collection and conducting intervention activities.
Funding
This study was funded by the Research and Technology Department, Iran Ministry of Health and Medical Education, and Iranian Network of Cardiovascular Research (Grant number: 96110).
Author information
Authors and Affiliations
Contributions
NM conceived the study, MR, RAB, BD, EZ, SGh, AS, MD, AA, FH, SNH and NA collected and analyzed the data. NS and ML interpreted the statistical analyses and NS wrote the first draft of the manuscript. MR contributed to the manuscript revising and editing. All of the authors critically revised the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the ethical committee of the Isfahan University of Medical Sciences (IR.MUI.REC.1396.2.055). All patients were provided with written and verbal information about the study and informed consent was obtained from all subjects.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mohammadifard, N., Rahimlou, M., Amani-Beni, R. et al. Mediterranean diet and prime diet quality score are associated with reduced risk of premature coronary artery disease in Iran: a multi-centric case-control study. Sci Rep 15, 11385 (2025). https://doi.org/10.1038/s41598-025-95719-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95719-y
Keywords
This article is cited by
-
The correlation between PURE healthy diet and premature coronary artery disease: Iran premature coronary artery disease (IPAD) study
BMC Cardiovascular Disorders (2025)
-
Dietary inflammatory index and mortality in middle-aged and elderly patients with metabolic syndrome
Diabetology & Metabolic Syndrome (2025)