Abstract
Previous studies have demonstrated that intermittent catheterization (IC) is an effective management strategy for neurogenic bladder (NB), but the knowledge of medical staff in this field remains under-researched. This cross-sectional study aimed to explore the profile of medical staff’s knowledge regarding IC in NB management and its associated factors. In August 2023, we conducted a convenience sampling survey involving 207 eligible medical staff from high-prevalence departments of NB at a tertiary general hospital in Nanchong, Southwest China. Data analysis was performed using latent class analysis (LCA) and logistic regression analysis. The results showed that respondents’ knowledge of IC in NB management scored 10.27 ± 2.89 (maximum possible score of 16). The LCA identified two distinct profiles: a high knowledge group (57.97%) and a low knowledge group (42.03%). Logistic regression revealed that individuals with a college degree or above (OR = 2.15, 95% CI 1.14–4.07), those focusing on NB management (OR = 4.07, 95% CI 2.21–7.49), and those who received relevant training (OR = 2.81, 95% CI 1.57–5.02) were more likely to be in the high level group. Additionally, variations in knowledge profiles were observed across different departments. These findings indicate a need to enhance medical staff’s understanding of IC in NB management in high-prevalence departments of NB, with targeted training programs as a potential solution. Notably, the use of convenience sampling and a single-center design in this study may constrain the generalizability of these findings, necessitating multicenter validation studies in the future.
Similar content being viewed by others
Introduction
Neurogenic bladder (NB) is a lower urinary tract dysfunction secondary to neurological compromise of central nervous system coordination, characterized by manifests as urinary retention, incontinence, and voiding difficulty1. It is a prevalent complication among patients with spinal cord injury, stroke, and multiple sclerosis2,3,4. In 2017, it was reported that 1009 individuals per million worldwide suffered from NB due to spinal cord injury alone5. The clinical course of NB is not limited to immediate urinary dysfunction but also predisposes patients to increasingly severe urological complications, such as recurrent urinary tract infections, vesicoureteral reflux, and hydronephrosis6. In severe cases, it even can lead to renal failure6. This pathophysiological cascade not only negatively impacts the quality of life of patients but also increases their risk of hospitalization and mortality6,7. From a health economics perspective, NB imposes a heavy socioeconomic burden, with a study on the global burden of NB showing annual per-patient costs ranging from €269 to €7068. Additionally, the total annual hospitalization costs for NB patients in China is still increasing at a rate of 36.66%9. Therefore, it is important to explore effective management strategies for NB. Intermittent catheterization (IC) is recognized as the preferred method for managing bladder dysfunction in NB patients10,11. It can effectively diminish post-void residual volume through regular bladder evacuation, thereby mitigating the risk of urinary tract infections and urolithiasis, as well as improving bladder function, sexual health, fertility, and overall quality of life for patients5,12,13,14.
Despite well-documented efficacy of IC, substantial evidence-practice gaps remain in healthcare workers’ understanding and implementation of this technique. Empirical evidence from a U.S.-based study (n = 210 nurses) revealed that approximately two-thirds (66%) of the nurses failed to adhere to the IC guidelines15, frequently culminating in regression to suboptimal bladder management modalities (e.g., chronic indwelling catheters)16. Globally, 17.6% to 25.6% of clinical workers erroneously associated IC with increased urinary tract infection risks and diminished quality of life in NB patients13,17. Similarly, most medical workers in China doubt the effectiveness of IC in NB management and lack knowledge in this area18,19. IC is typically performed by patients or their caregivers following training and rigorous competency verification from healthcare providers. Empirical evidence confirmed that healthcare providers’ comprehensive mastery of knowledge related to NB and IC is a key determinant for effectively imparting knowledge to trainees and sustaining procedural fidelity.20,21. Therefore, it is necessary to explore how to improve healthcare providers’ knowledge regarding NB and IC.
Currently, research on IC in NB management mainly focuses on patients, with few studies addressing the perspectives of healthcare providers18,19,22. Existing literature investigated the knowledge levels of medical staff through homogenized conceptual frameworks that inadvertently lump diverse medical personnel into undifferentiated cohorts. This oversimplification can obscure important differences within medical workforce and overlook the unique educational needs of specialized subgroups, potentially undermining the effectiveness of educational interventions. Latent class analysis (LCA) provides a framework for classifying based on individual characteristics, which can effectively identify subgroups with similar characteristics and inform the development of more targeted interventions23. Therefore, this study used the LCA to examine the knowledge profiles of medical staff regarding IC in NB management and analyzed its associated factors, with the aim of establishing an evidence base for the development and implementation of targeted training programs.
Methods
Study design, setting and participants
This study was conducted as a single-center cross-sectional survey. We used a convenience sampling method to recruit medical staff from departments with a high prevalence of NB, including Rehabilitation, Neurology, Urology, Orthopedics, Gynecology, Pediatrics, and Endocrinology, in a tertiary general hospital. Eligibility criteria for participation included: (1) being at least 18 years of age; (2) possessing a valid medical or nursing license; (3) having a minimum of one year of work experience; and (4) providing informed consent for voluntarily participation. Medical staff who were absent due to sick leave, personal leave, or study abroad, or who were from other hospitals and enrolled in further educational programs within the departments, were excluded from the study. According to information obtained from the department heads, the total number of eligible medical staff was 278.
Measurements
Sociodemographic information form
The sociodemographic information form was developed to collect key demographic variables of participants, including gender, age, occupation, education level, professional title, years of work experience, and departmental affiliation. Additionally, dichotomous variables assessed clinical focus on NB management and the completion of related training.
Neurogenic bladder intermittent catheterization knowledge questionnaire
This questionnaire was developed by Du Yanhui18 informed by the guidelines on Neurogenic Bladder Dysfunction issued by the European Urology Association24, as well as the Neurogenic Bladder Nursing Guidelines formulated by the Rehabilitation Nursing Committee of the Chinese Association of Rehabilitation Medicine25. It addressed the etiology, clinical manifestations, examinations, treatment goals, follow-up, and medications related to NB, as well as prerequisites, hydration plans, fluid intake control, scheduling, operational precautions, contraindications, and the benefits of IC. The instrument consisted of 13 single-choice and 3 multiple-choice questions, totaling 16 items. Correct single-choice answers earned 1 point (incorrect/unknown responses scored as 0), while multiple-choice questions required all correct options to be selected for 1 point (any other response scored 0). The maximum score is 16, with a Cronbach’s α of 0.733.
Data collection
In August 2023, following departmental approval, we delivered an online questionnaire to charge nurses across departments, who subsequently circulated the questionnaire and accompanying instructions among the medical staff within their respective departments. The questionnaire’s homepage incorporated a series of questions designed to apply inclusion and exclusion criteria, thereby ensuring the eligibility of respondents. To prevent duplicate submissions and ensure data integrity, we implemented IP/WeChat ID restriction protocols permitting a single submission per unique identifier, coupled with forced-response validation requiring complete item responses for survey submission.
Ethical considerations
The study was approved by the Medical Ethics Committee of the Affiliated Hospital of North Sichuan Medical College (No.2022ER219-1). All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee, as well as the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All participants received a plain language statement prior to the survey, and the completion of a fully filled questionnaire implied their informed consent to participate in the study. Finally, informed consent was obtained from all subjects who were included in the analysis.
Statistical analysis
Data analyses were conducted in Mplus7.4 and Zstats1.0 (www.zstats.net). First, descriptive analyses were used to delineate the sociodemographic characteristics of the participants, with continuous variables presented as mean ± standard deviation and categorical variables expressed through frequency distributions with proportional representations. LCA was subsequently implemented in Mplus7.4 with items responses from the neurogenic bladder intermittent catheterization knowledge questionnaire as manifest indicators. Iterative model estimation evaluated through multiple fit indices: log-likelihood (LL), Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), adjusted BIC (aBIC), entropy, Vuong-Lo-Mendell-Rubin (VLMR), and Bootstrapped Likelihood Ratio Test (BLRT). Lower values of AIC, BIC, and aBIC indicated superior model fit. Additionally, higher entropy values reflected greater classification precision. Significant likelihood ratio tests (P < 0.05) supported the selection of the K-class model over the (K-1)-class solution26. Following subgroup identification through LCA, chi-square tests examined demographic differences across latent classes. Significant sociodemographic predictors were subsequently incorporated into multivariate logistic regression models with class membership as the outcome variable. The logistic regression analysis was conducted using Zstats1.0, which generated a logistic regression forest plot. A two-tailed P-value of 0.05 was applied for statistical significance throughout the analytical process.
Results
Partcipants’ sociodemographic characteristics
A total of 207 medical staff participated in the survey, yielding a response rate of 74.5%. Demographics revealed a predominantly female cohort (79.7%), with clinical nurses comprising 75.8% of respondents. The majority were aged ≤ 40 years (81.6%) and held college degrees or lower qualifications (63.3%). Over half reported having ≤ 10 years of clinical experience (53.6%) and held a junior professional title (51.7%). While 66.2% of the participants expressed concerns regarding the management of NB, only 45.4% had received related training (Table 1). The average score for knowledge of IC in NB management among participants was 10.27 ± 2.89 (individual range: 2–16; theoretical maximum: 16).
LCA results of knowledge for IC in NB management
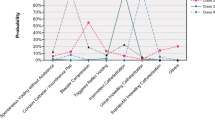
This study evaluated latent class models ranging from one to four categories, as summarized in Table 2. Models 1 through 3 demonstrated progressive improvements in model fit indices, evidenced by consistent decreases in the absolute LL values along with reductions in both AIC and aBIC. However, the BIC exhibited an inflection point at Model 4, showing an increased value compared to Model 3, thereby supporting the exclusion of the four-class solution. The likelihood ratio tests (BLRT and VLMR) for Model 3 revealed non-significant p-values (P > 0.05), statistically confirming that the three-class model did not provide superior fit relative to the two-class solution. Consequently, the two-class model was selected as the optimal model, with latent class probabilities of 57.97% for one category and 42.03% for the other. As shown in Fig. 1, the conditional probability distribution reflected the differences in response accuracy rates between the two latent classes across various knowledge items. One category exhibited a higher conditional probability of scoring on all items compared to the other, with a conditional probability of scoring on 11 items being ≥ 0.8, thus it was designated as the "high level group." In contrast, the other category demonstrated conditional probabilities of less than 0.6 for 13 items, resulting in its designation as the "low level group."
The conditional probability distribution of two latent classes (N = 207). Note: Q1-Q8: Question 1 to 8-the etiology, clinical manifestations, examinations, treatment goals, follow-up, and medications of neurogenic bladder; Q9-Q16: Question 9 to 16-the prerequisites, hydration plans, fluid intake control, scheduling, operational precautions, contraindications, and the benefits of IC.
Comparison of latent classes among participants with different sociodemographic characteristics
Statistically significant differences were observed among LCA-identified subgroups with respect to education level, departmental distribution, focus on NB management, and prior receipt of related training (Table 1).
Results of logistic regression analysis for latent classes
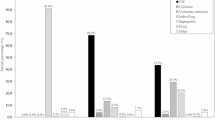
Figure 2 presents the logistic regression analysis results with the classification derived from LCA as the dependent variable. Individuals holding a degree above the college level were found to be 2.15 times more likely to be in the high level group compared to those with a college degree or lower (95% CI 1.14–4.07, P = 0.018). Furthermore, individuals who focused on NB management and received relevant training were 4.07 times (95% CI 2.21–7.49, P < 0.001) and 2.81 times (95% CI 1.57–5.02, P < 0.001) more likely to be in the high level group than those who did not concentrated on NB management and those who lacked relevant training, respectively. Compared with rehabilitation department, the likelihood of being classified in the high level group was significantly lower in orthopedics, gynecology, urology, pediatrics, and neurology, with odds ratios of 0.01, 0.02, 0.03, 0.04, and 0.06, respectively. In contrast, the likelihood in endocrinology was reduced to 0.27, although this finding was not statistical significant (P = 0.271).
Discussion
This study provides unique insights into medical staff knowledge heterogeneity regarding IC in NB management through LCA. The results indicated that the participants’ average knowledge score was 10.27 ± 2.89 (individual range: 2–16; theoretical maximum: 16), marginally exceeding values reported by Niu (9.78)12 and Du (9.35)18. However, this aggregate score translates to merely 64.2% of the total possible points, revealing that the overall knowledge of healthcare workers in this domain remains insufficient. Unlike previous research, this study identified two distinct knowledge categories through LCA: the high-level group and the low-level group, comprising 57.97% and 42.03% of participants, respectively. These findings support Niu Mingming’s earlier research12, which highlighted significant differences in healthcare workers’ perceptions of NB management. In the low level group, the accuracy rate for most questions was below 60%, except for those pertaining to NB follow-up, IC hydration plans, and operational precautions, aligning with studies showing medical staff’s limited understanding of IC and NB management27. Notably, even in the high level group, the accuracy rate for questions pertaining to the etiology and treatment goals of NB, as well as prerequisites and contraindications of IC, remains below 50%. This finding highlights knowledge deficiencies even among those considered well-informed. Therefore, it is necessary to strengthen the training of medical staff on NB management in the future. Moreover, this study reveals that when developing training programs, the disparities in knowledge levels among different groups in specific aspects of NB management or IC procedures should be considered to improve the relevance and effectiveness of the training.
This study used logistic regression to identify determinants of latent class membership (derived via latent class analysis) in healthcare providers’ knowledge profiles regarding IC in NB management. The analysis revealed three significant predictors of classification into the high-knowledge group: attainment of a degree above the college level (OR = 2.15, 95% CI 1.14–4.07), focus on NB management (OR = 4.07, 95% CI 2.21–7.49), and completion of relevant training (OR = 2.81, 95% CI 1.57–5.02). These findings are consistent with the studies by Niu12 and Du18, which similarly identified that medical staff with higher knowledge scores were linked to these specific factors. This correlation may be attributed to the fact that medical staff with higher education levels usually receive more systematic medical education. Additionally, those who actively focus on NB management are more willing to engage in proactive learning and participate in relevant training, which has been shown to effectively enhance their knowledge27,28. In this study, while 66.2% of the participants expressed concern regarding NB management, only 45.4% had received relevant training. This gap underscores the need for enhanced NB management awareness and regular professional training, especially for those with lower education levels. Last but not least, compared to rehabilitation departments, medical staff in neurology, urology, pediatrics, orthopedics, and gynecology were more likely to be classified in the low level group, which may be attributed to the divergent clinical priorities of each department12,18. Patients admitted to the rehabilitation department are in a relatively stable condition, thus the primary focus is on patients’ functional recovery and self-care capacity, whereas other departments are preoccupied with the stabilization of patients’ acute medical conditions. This divergence in departmental focus may result in inadequate attention to NB management among medical staff in these departments. However, the NB prevalence remains substantial across these latter departments, and poor management of NB causes negative impacts on patients’ health outcomes6,7,8,9. To address these challenges, the implementation of specialty-tailored NB training modules and the establishment of cross-departmental knowledge-sharing protocols may be useful strategies. Such interventions could harmonize NB management standards while preserving specialty-specific workflows. Importantly, rehabilitation departments might serve as natural hubs for these knowledge-translation initiatives, given their demonstrated expertise. Future implementation research should evaluate the efficacy of these approaches in optimizing the management outcomes of NB while maintaining clinical efficiency.
This study has several limitations. Firstly, the convenience sampling method entails inherent selection bias risks, even though the proportional representation of staff in various departments approximated actual medical staff distributions in these departments in our study. Secondly, the single-center design and limited sample size constrain the generalizability of the findings across diverse healthcare systems and institutional contexts. Subsequent research should employ probability sampling frameworks and implement multicenter investigations spanning diverse geographic regions to elucidate systemic commonalities and context-specific variations, thereby providing a more comprehensive perspective for global health policy making. Despite these limitations, we used LCA to explore the latent classes of medical staff’s knowledge levels of IC in NB management, providing a fresh perspective on understanding their knowledge levels. We also analyzed the potential factors affecting the latent class grouping, laying a foundation for developing more targeted training programs. The optimization of training programs may enhance medical staff’s knowledge of NB management and collaboration within the healthcare system, thereby improving the quality of care for patients with NB at a system level and patients’ health outcomes. However, these potential effects need to be further verified in future research.
Conclusions
The overall knowledge score of medical staff regarding IC in the management of NB remains suboptimal, with two distinct profiles identified: a high level group and a low level group. Despite participants in the high level group generally perform well, there are still particular aspects of NB management or IC procedures that were less well-understood. Multivariate analysis identified attainment of a degree above the college level, focus on NB management, and completion of relevant training as significant predictors of classification into the high-knowledge group. Conversely, affiliation with high-NB prevalence departments, including orthopedics, gynecology, urology, neurology, and pediatrics, emerged as independent risk factors for low-knowledge categorization. These findings underscore the necessity for enhanced knowledge of IC in NB management among medical staff in high-prevalence departments of NB. Emphasizing the importance of focusing on NB management and implementing targeted training programs that address the varying knowledge levels across different groups in specific aspects of NB management and IC procedures could be effective. However, the potential impact of these interventions requires further validation in future research.
Data availability
The datasets used and analyzed in the study are available from the corresponding author upon reasonable request.
References
Panicker, J. N. Neurogenic bladder: epidemiology, diagnosis, and management. Semin. Neurol. 40, 569–579 (2020).
Ginsberg, D. The epidemiology and pathophysiology of neurogenic bladder. Am. J. Manag. Care 19, s191-196 (2013).
Hamid, R. et al. Epidemiology and pathophysiology of neurogenic bladder after spinal cord injury. World J. Urol. 36, 1517–1527 (2018).
Przydacz, M., Denys, P. & Corcos, J. What do we know about neurogenic bladder prevalence and management in developing countries and emerging regions of the world?. Ann. Phys. Rehabil. Med. 60, 341–346 (2017).
Wu, C. Q. & Franco, I. Management of vesicoureteral reflux in neurogenic bladder. Investig. Clin. Urol. 58, S54–S58 (2017).
Nseyo, U. & Santiago-Lastra, Y. Long-term complications of the neurogenic bladder. Urol. Clin. North Am. 44, 355–366 (2017).
Manack, A. et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol. Urodyn. 30, 395–401 (2011).
Flack, C. & Powell, C. R. The worldwide economic impact of neurogenic bladder. Curr. Bladder Dysfunct. Rep. 10, 350–354 (2015).
Palma-Zamora, I. D. & Atiemo, H. O. Understanding the economic impact of neurogenic lower urinary tract dysfunction. Urol. Clin. North Am. 44, 333–343 (2017).
Groen, J. et al. Summary of European association of urology (EAU) guidelines on neuro-urology. Eur. Uro. 69, 324–333 (2016).
Hu, Y. J. et al. Summary of the best evidences for risk management of urinary tract injury in neurogenic bladder. Chin. Nurs. Res. 33, 2367–2373 (2019).
Niu, M. M. Network meat-analysis and cognition investigation of the application effect of inermittent catheterization in patients with neurogenic bladder. Dissertation, Lanzhou University (2022).
Singh, N., McConnell, D. S. & Oligbo, N. Comparing clean intermittent catheterisation and transurethral indwelling catheterisation for incomplete voiding after vaginal prolapse surgery: A multicentre randomised trial. BJOG 119, 113 (2012).
Kinnear, N. et al. The impact of catheter-based bladder drainage method on urinary tract infection risk in spinal cord injury and neurogenic bladder: A systematic review. Neurourol. Urodyn. 39, 854–862 (2020).
Gray, M., Wasner, M. & Nichols, T. Nursing practice related to intermittent catheterization: A cross-sectional survey. J. Wound Ostomy Continence Nurs. 46, 418–423 (2019).
Patel, D. P. et al. Reasons for cessation of clean intermittent catheterization after spinal cord injury: Results from the Neurogenic Bladder Research Group spinal cord injury registry. Neurourol. Urodyn. 39, 211–219 (2020).
Nazarko, L. Intermittent self-catheterisation: Past, present and future. Br. J. Commun. Nurs. 17(408), 410–412 (2012).
Du, Y. H. Cognition status of medical staffs in a third-grade class-A hospital in Chong Qing on intermittent catheterization used in the neurogenic bladder and the countermeasure. Dissertation, Chongqing Medical University (2015).
Zhou, J. G., Zhou, M., Pang, F., Liu, Y. & Guo, M. M. Survey of rehabilitation nursing management of neurogenic bladder and clinical application of intermittent catheterization in Guangdong, China. Chin. J. Rehabil. Theory Pract. 27, 1233–1240 (2021).
Hayes, L. C. et al. Facilitators and challenges to transitioning to self-catheterization: Patient and caregiver perspectives. Neurourol. Urodyn. 42, 1399–1410 (2023).
Fitzpatrick, M. A. et al. Perceptions, experiences, and beliefs regarding urinary tract infections in patients with neurogenic bladder: A qualitative study. PLoS ONE 18, e0293743 (2023).
Fan, F. & Ma, X. X. Qualitative study on the cognition of medical staff bladder function rehabilitation training in patients with spinal cord injury. Chin. Evid. -Based Nurs. 6, 1087–1092 (2020).
Yang, Q. et al. Latent profile/class analysis identifying differentiated intervention effects. Nurs. Res. 71, 394–403 (2022).
Stöhrer, M. et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur. Urol. 56, 81–88 (2009).
Rehabilitation Nursing Committee of the Chinese Association of Rehabilitation Medicine Neurogenic bladder nursing guidelines (2011 Edition) (Part 2). Chin. J. Nurs. 46, 210–216 (2011).
Sinha, P., Calfee, C. S. & Delucchi, K. L. Practitioner’s guide to latent class analysis: Methodological considerations and common pitfalls. Crit Care Med 49, e63–e79 (2021).
Xiang, L. et al. Rehabilitation care of patients with neurogenic bladder after spinal cord injury: A literature review. World J. Clin. Cases 11, 57–64 (2023).
Kumar, S. J. & Biswas, D. A. Anatomical aspects of neurogenic bladder and the approach in its management: A narrative review. Cureus. 14, e31165 (2022).
Wong, B. T. H., Kan, S. C. F., Lo Alex, H. K., Ho Lap, Y. & Kan, R. W. M. Asian guidelines for UTIs & STIs UTI section: Complicated UTIs with neurogenic bladder. J. Infect. Chemother. 28, 6–9 (2022).
Acknowledgements
First of all, we would like to thank the Affiliated Hospital of North Sichuan Medical College for its approval and support for this study. Secondly, we would like to express our gratitude to the head nurses of the investigated departments for their support and assistance in the data collection process, as well as to the medical staff who participated in the survey for their valuable time.
Funding
This work was supported by Nanchong Federation of Social Science Associations (Grant numbers: NC2018B058).
Author information
Authors and Affiliations
Contributions
Conceptualization, W.L., X.S., and L.W.; Data curation, J.H., X.D., and X.X.; Formal analysis, J.H., and X.X.; Funding acquisition, W.L., X.S., L.W., and X.D.; Investigation, W.L., X.S., L.W., X.D., and Y.L.; Supervision, X.X.; Writing-original draft, W.L., X.S., and L.W.; All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Luo, W., Sun, X., Wang, L. et al. Latent classes analysis and associated factors of knowledge of intermittent catheterization in neurogenic bladder management among medical staff. Sci Rep 15, 11319 (2025). https://doi.org/10.1038/s41598-025-96362-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96362-3