Abstract
Intracranial infection is one of the most common complications of microvascular decompression (MVD). However, the risk factors for intracranial infection after MVD remain unknown. The aim of this study was to identify the risk factors for the development of post-MVD intracranial infection and to provide a basis for the prevention and control of intracranial infection following MVD. The clinical data of 154 patients with cranial nerve diseases who underwent MVD from October 2010 to August 2024 were retrospectively analyzed. The risk factors of intracranial infection were subjected to univariate and multivariate analysis. Twenty-four cases of intracranial infection occurred in 154 patients in this study, for a total infection rate of 15.6%. Univariate analysis showed that gender, duration of operation, CSF leakage, mastoid air cells breach, implants and intra-operative use of antibiotics were the risk factors related to intracranial infection after MVD (P < 0.05). Multivariate logistic regression analysis showed that a duration of operation and mastoid air cells breach were independent risk factors of intracranial infection after MVD (P < 0.05). The ROC curve analysis revealed that duration of operation, mastoid air cells breach and combined prediction exhibited area under the curve (AUC) values of 0.675 (95% CI [0.562–0.788]), 0.713 (95% CI [0.586–0.840]), 0.807 (95% CI [0.712–0.903]), respectively, for predicting intracranial infection after MVD. Duration of operation and mastoid air cells breach were independent risk factors for postoperative intracranial infection after MVD. The combination of two factors has high value in predicting the risk of intracranial infection following MVD.
Similar content being viewed by others
Introduction
Microvascular decompression (MVD) has become the first surgical treatment for cranial nerve diseases such as trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia. Although MVD has made great progress in recent years, there are still some complications related to MVD. Intracranial infection is a common complication leading to a prolongation of the hospital stay and increases in pain and discomfort and the economic burden of health care on the patients, and it also worsens their prognosis and even endangers their lives1,2. Therefore, it is of great significance to understand the risk factors of intracranial infection after MVD and to evaluate, prevent and control these infections. Although intracranial infection after MVD has been reported in previous papers3,4,5, to our knowledge, there has been no systematic analysis of the risk factors of intracranial infection after MVD. The aim of this study was to retrospectively investigate the risk factors for the development of post-MVD intracranial infection and to evaluate their potential role in predicting the possibility of intracranial infection following MVD.
Materials and methods
Materials
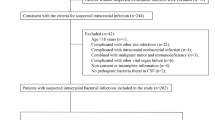
The clinical data of 154 patients with MVD from October 2010 to August 2024 treated in our hospital were analyzed, including 51 men and 103 women aged from 25 to 77, with an average age of 57.8 ± 9.8 years. There were 70 patients with trigeminal neuralgia, 82 with facial spasm and 2 with glossopharyngeal neuralgia.
Diagnostic criteria of intracranial infection
Referring to the diagnostic criteria of the American Advisory Committee for the implementation of nosocomial infection control6 and combined with the comprehensive analysis of conditions:1 The results of the postoperative cerebrospinal fluid (CSF) examination showed that the WBC > 100/UL and the sugar and chloride were decreased (CSF glucose level below 2.2 mmol/L or CSF-to-serum glucose ratio of less than 0.4, CSF chloride level below 120mmol/L)2. Blood routine examination showed that the WBC was more than 1.0 × 1010/L and the neutrophil percentage were more than 75%3. Postoperative temperature higher than 38 ℃ for more than 3 days was judged as intracranial infection after excluding the possibility of infection of other systems4. Meningeal irritation sign was positive5. CSF bacterial culture was positive with the same strain detected twice sequentially. The fifth criterion is an etiological diagnosis, the gold standard of diagnosis, and it can be diagnosed independently as an intracranial infection. However, due to the use of antibiotics after surgery, the positive rate of CSF cultures is relatively low, so a clinical comprehensive consideration is that patients with the first criterion and at least one of the second, third, or fourth criterion are identified as having an intracranial infection.
Statistical analysis
All statistical analyses were performed using SPSS version 16.0 for Windows (Chicago, IL). Chi square tests were used for the single factor analysis; the influencing factors with statistical significance in the univariate analysis were included in the binary logistic regression analysis. Evaluate the discriminative ability of factors using the area under the receiver operating characteristic (ROC) curve. A P-value less than 0.05 was considered to be statistically significant.
Results
All patients underwent retromastoid craniectomy. Twenty-four cases of intracranial infection occurred in 154 patients in this study, so the total infection rate was 15.6%. Univariate analysis showed that gender, duration of operation, CSF leakage, mastoid air cells breach, implants and intra-operative use of antibiotics were the related risk factors of intracranial infection after MVD (P < 0.05), as shown in Table 1. The risk factors related to intracranial infection obtained by the univariate analysis were included in the binary logistic regression analysis. The variable assignments are shown in Table 2. The results showed the duration of operation and mastoid air cells breach were independent risk factors of intracranial infection after MVD (P < 0.05), as shown in Table 3. The ROC curve analysis revealed that duration of operation, mastoid air cells breach and combined prediction exhibited area under the curve (AUC) values of 0.675 (95% CI [0.562–0.788]), 0.713 (95% CI [0.586–0.840]), 0.807 (95% CI [0.712–0.903]), respectively, for predicting intracranial infection after MVD. Combined prediction demonstrated the highest AUC in predicting intracranial infection after MVD (P < 0.001), as shown in Table 4; Fig. 1.
Discussion
The root cause of cranial nerve diseases such as trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia is the compression of ectopic small blood vessels twisted into loops at the root and the brain stem, resulting in nerve demyelination and a short circuit of the nerve conduction pathway, causing pain and convulsions. At present, MVD has become the preferred surgical method for the treatment of trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia. It can retain nerve function and normal facial sensation and function without affecting the quality of life, and achieve the purpose of establishing a radical cure, with an analgesic effect. Therefore, it is the safest and most effective method for the treatment of cranial nerve diseases7,8.
However, there are still some complications of MVD, among which intracranial infection is one of the more serious complications. Because MVD involves a craniotomy, intracranial infections can occur and are classified as a surgical site infection, which is an acute or chronic inflammatory disease caused by bacteria, viruses and other pathogens invading the brain parenchyma, capsule and blood vessels. Because MVD is a kind of functional minimally invasive surgery, methods to avoid complications are of paramount importance, allowing the postoperative patients to recover faster while reducing the incidence of surgical trauma and complications, including the incidence of intracranial infections. However, once an intracranial infection occurs, it delays the patient’s hospitalization discharge time, increases the patient’s treatment-related pain and increases the economic burden related to hospitalization expenses. In severe cases, brain abscesses, hydrocephalus, encephaledema and intracranial hypertension can develop, and additional surgery may be required, and permanent disability and even life-threatening complications may occur1,9. Therefore, understanding of the statistics and an analysis of the risk factors for intracranial infection after MVD is of great significance for the prevention and treatment of intracranial infection after MVD. The total postoperative intracranial infection rate of neurosurgical patients has been reported to be 1.5–6.85%9,10,11,12, and that of craniotomy patients is 3.6–9.5%13,14,15. Because MVD is a type of infratentorial posterior cranial fossa surgery, the incidence of intracranial infection in the posterior cranial fossa is 3 times that after cerebral hemisphere surgery. In our study of 154 cases of patients with cranial nerve diseases after MVD, 24 cases (15.6%) of intracranial infection occurred, much higher than the above reported range. Zhou et al. analyzed the complications of 308 patients with hemifacial spasm who underwent.
MVD. The results showed that the incidence of intracranial infection was 17.6%16, which was similar to our results, so we should pay more attention to taking the necessary measures to reduce the infection rate after MVD.
According to the clinical experience and related literature reports, the risk factors of intracranial infection after MVD were selected for univariate analysis and multivariate logistic regression analysis. The results showed that a duration of operation and mastoid air cells breach were independent risk factors for intracranial infection after craniotomy for a skull base tumor. The reasons for this may be as follows1: Duration of operation: many reports at home and abroad have shown that long operation time is a risk factor for intracranial infection after intracranial tumor surgery17,18,19. The longer the operation duration, the higher the risk of intracranial infection, the relationship between the operation time and an increased risk of intracranial infection can be explained by many factors, a long-duration operation may lead to more bacteria entering the wound from various sources, including the room air, the surgical tools and the patient’s skin. With the extension of the operation duration, the migration to the operation area increases, resulting in the operation area becoming infected. The dura mater and soft tissue contract due to the surgical exposure, resulting in decreased perfusion and time-dependent local immune defense. The soft tissue may also become dry due to the heat from the microscope light, and the local blood supply may be reduced, promoting infection. Therefore, prolonged exposure to the surgical area may affect the smooth closure of the dura mater and lead to more tissue damage, leading to a higher risk of infection2. Mastoid air cells breach: mastoid air cells breach was significantly correlated with the outcome of intracranial infection after MVD in our study (odds ratio (OR) = 9.349, p = 0.001). Multiple studies at home and abroad have shown that a mastoid air cells or sinus breach is a risk factor for intracranial infection after neurosurgical craniotomy16,20,21. The air cells of the sinus and mastoid are connected to the nasal cavity and external auditory canal, which are not sterile areas. Once opened, the mastoid air cells will pollute the operation area, leading to intracranial infection; such breaches may also cause cerebrospinal fluid leakage, allowing extracranial bacteria to migrate into the cranial space, again causing intracranial infection.
In view of the above analysis of the risk factors of intracranial infection after MVD, patients with these risk factors should be paid more attention to prevent intracranial infections. The corresponding measures should be taken to minimize the probability of intracranial infection. The dura mater should be covered with water during the operation. The degree of mastoid gas room pneumatization should be understood by referring to the imaging data, especially thin-layer CT of the mastoid process before the operation. Opening of the mastoid air chamber and frontal sinus should be avoided as much as possible. If this does occur, the mucosa in the sinus or mastoid air cells should be scraped off, and then the opening should be filled with sufficient bone wax and sealed tightly. If necessary, medical glue, muscle fat, gentamicin and iodovox should be used. The operation area needs to be rinsed with hydrogen peroxide and the incision needs to be bandaged under pressure. If the operation time is long, prophylactic application of antibiotics during the operation is necessary. Surgeons should improve their study of anatomical knowledge, undergo training in microsurgery operations, improve their operation proficiency, use advanced surgical tools, and shorten the operation time as much as possible to ensure the safety of the operation. During the operation, the retractor should be released intermittently to prevent pulling the soft tissue and muscle around the incision for a long time, which weakens the local anti-infection ability. During the operation, the surgeon should be gentle, and the tissue should be treated with care. Especially during the process of craniotomy, careful hemostasis should be undertaken to prevent unnecessary bleeding. Intermittent irrigation of the operation area during the operation can moisten the muscle tissue, enhance the anti-infection ability of the local tissue, and wash away any bacteria, preventing bacterial colonization and reproduction.
It is worth mentioning that there was no correlation between the extent of hair shaving and postoperative intracranial infection. Bekar et al.22compared the incidence of postoperative intracranial infection in 980 patients with preoperative shaving and 1038 patients without shaving, the results showed that there was no difference in the infection rate between the two groups. According to The Asia Pacific Society of Infection Control (APSIC) guidelines for the prevention of surgical site infections, the hair on the surgical site should be removed only when it interferes with the operation. Shaving the hair may cause small incisions and abrasions that may damage the skin barrier, and it is not conducive to the prevention and control of infection23. Therefore, it is not necessary to shave all of the hair before the operation. Implementing local shaving only can prevent the psychological anxiety and stress caused by full head shaving. In addition, it is recommended to use scissors to remove hair in the operating room, so as to avoid any infections that could be caused by scraping the scalp with an electric shaver or a razor blade24.
This study comprehensively analyzed the risk factors related to intracranial infection after MVD and provided a clinical reference basis for preoperative evaluation, the control of infection risk factors and the prevention of intracranial infections after MVD, which has certain clinical significance. However, there are some limitations of this study that should be noted. Because this study is a retrospective single-center study, and it is a specific study of intracranial infection after MVD, the number of cases is relatively small, which may affect the accuracy of the results. A prospective, multi-center, large sample study is needed to further confirm the risk factors of intracranial infection after MVD.
Data availability
All datasets generated or analyzed during the present study are available from the corresponding author upon reasonable request.
References
Hweidi, I. M., Barbarawi, M. A., Tawalbeh, L. I., Al-Hassan, M. A. & Al-Ibraheem, S. W. Surgical site infections after craniotomy: a matched health-care cost and length of stay study. J. Wound Care. 27, 885–890 (2018).
Piednoir, E., Robert-Yap, J., Baillet, P., Lermite, E. & Christou, N. The socioeconomic impact of surgical site infections. Front. Public. Health. 9, 712461 (2021).
Yu, R. et al. Study on the therapeutic effects of trigeminal neuralgia with microvascular decompression and stereotactic gamma knife surgery in the elderly. J. Craniofac. Surg. 30, e77–e80 (2019).
Zheng, X. et al. Fully endoscopic microvascular decompression for hemifacial spasm: a clinical study and analysis. Neurosurg. Rev. 47, 83 (2024).
Shi, H. et al. Application value of calcium phosphate cement in complete cranial reconstructions of microvascular decompression craniectomies. J. Plast. Reconstr. Aesthet. Surg. 85, 210–216 (2023).
Mangram, A. J., Horan, T. C., Pearson, M. L., Silver, L. C. & Jarvis, W. R. Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect. Control Hosp. Epidemiol. 20, 250–278 (1999). quiz 279–280.
Alizadeh, Y., Hayak, H. & Khoshnevisan, A. Microvascular decompression versus gamma knife surgery in patients with Drug-Resistant trigeminal neuralgia: A systematic review and Meta-Analysis. World Neurosurg. 167, 67–73 (2022).
Peng, W. et al. Fully endoscopic microvascular decompression for the treatment of hemifacial spasm, trigeminal neuralgia, and glossopharyngeal neuralgia: a retrospective study. BMC Surg. 23, 331 (2023).
Bekelis, K., Coy, S. & Simmons, N. Operative duration and risk of surgical site infection in neurosurgery. World Neurosurg. 94, 551–555.e556 (2016).
López Pereira, P. et al. Epidemiology of surgical site infection in a neurosurgery department. Br. J. Neurosurg. 31, 10–15 (2017).
Adapa, A. R. et al. Risk factors and morbidity associated with surgical site infection subtypes following adult neurosurgical procedures. Br. J. Neurosurg. 1–7 (2021).
Zhu, H., Liu, X. & Wang, Z. Infection rate in 1033 elective neurosurgical procedures at a university hospital in South China. J. Neurol. Surg. Cent. Eur. Neurosurg. 78, 467–471 (2017).
Lepski, G., Reis, B., de Oliveira, A. & Neville, I. Recursive partitioning analysis of factors determining infection after intracranial tumor surgery. Clin. Neurol. Neurosurg. 205, 106599 (2021).
Wang, L. Y. et al. Risk factors for intracranial infection after craniotomy: A case-control study. Brain Behav. 10, e01658 (2020).
Joerger, A. K. et al. The impact of intraoperative MRI on cranial surgical site infections-a single-center analysis. Acta Neurochir. (Wien). 165, 3593–3599 (2023).
Zhou, J. et al. Association study of the pneumatization degree of mastoid air cells and postoperative complications after microvascular decompression in hemifacial spasm. Acta Neurochir. (Wien). 164, 1543–1550 (2022).
Patel, S. et al. Risk factors for surgical site infections in neurosurgery. Ann. R Coll. Surg. Engl. 101, 220–225 (2019).
Huang, X. et al. Analysis of risk factors and preventive strategies for intracranial infection after neuroendoscopic transnasal pituitary adenoma resection. BMC Neurosci. 23(1), 1 (2022).
Kurdyumova, N. V. et al. [Risk factors of nosocomial meningitis in neurological intensive care unit. Results of a five-year prospective study]. Zh Vopr Neirokhir Im N N Burdenko. 85, 83–91 (2021).
Belzberg, M., Shalom, N. B., Wolff, A., Huang, J. & Gordon, C. Bilateral versus unilateral cranialization in the management of a breached frontal sinus. J. Craniofac. Surg. 31, 261–264 (2020).
Lin, J. et al. Preoperative imaging and microscopic navigation during surgery can avoid unnecessarily opening the mastoid air cells through craniotomy using the retrosigmoid approach. World Neurosurg. 121, e15–e21 (2019).
Bekar, A. et al. The effect of hair on infection after cranial surgery. Acta Neurochir. (Wien). 143, 533–536 (2001). discussion 537.
Ling, M. L. et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob. Resist. Infect. Control. 8, 174 (2019).
Matsuda, S. et al. Questionnaire survey regarding prevention of surgical site infection after neurosurgery in Japan: focus on perioperative management and administration of surgical antibiotic prophylaxis. Neurol. Med. Chir. (Tokyo). 59, 197–203 (2019).
Acknowledgements
The authors thank Zhihua Zhang (Department of epidemiology and health statistics, The Anhui Medical University) for technical assistance of statistics.
Funding
This work was supported by the Cooperative research promotion plan of basic medicine and clinical medicine of Anhui Medical University under Grant [2020xkjT044] and the National Natural Science Foundation Incubation Project of the Second Affiliated Hospital of Anhui Medical University (Grant No. 2024GMFY04).
Author information
Authors and Affiliations
Contributions
“Zhifei Guo wrote the main manuscript text and prepared figures 1 and Tables 1-4. Xiangyu Zhang carried out data collection. B ing Zhao performed design of the work and critical revision of the article. All authors reviewed the manuscript.”
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The experimental protocol and procedures were approved by the ethical committee of the Second Affiliated Hospital of Anhui Medical University under Grant [YX2023-152]. All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, Z., Zhang, X. & Zhao, B. Analysis of risk factors of intracranial infection after microvascular decompression. Sci Rep 15, 11540 (2025). https://doi.org/10.1038/s41598-025-96431-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96431-7